Содержание
- 2. Supported by: Blue Cross and Blue Shield of North Carolina Foundation Collaborating Organizations: NC Department of
- 3. Introduction Thank you for being a participant in the DATA Program!! Your participation demonstrates your interest
- 4. Introduction continued… When a student with diabetes is part of the school system, the school staff
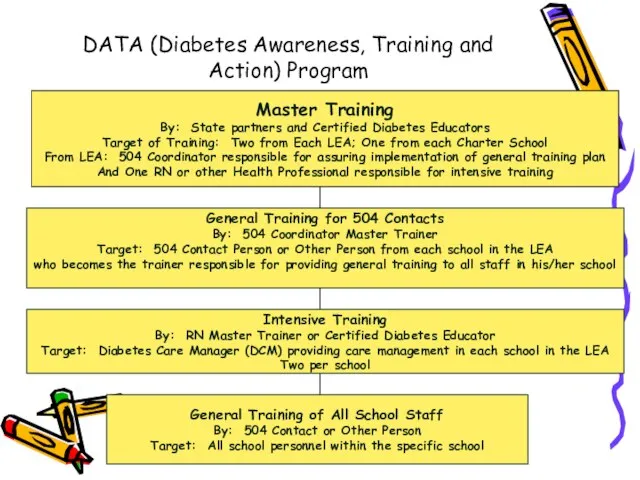
- 5. DATA (Diabetes Awareness, Training and Action) Program Master Training By: State partners and Certified Diabetes Educators
- 6. Part 1 Overview of SB 911 Care of School Children With Diabetes
- 7. Part 1: Overview of SB 911: Care of School Children with Diabetes Federal & State Support
- 8. Overview of SB 911 continued… State Board of Education Policy # 04A107 Special Health Care Services
- 9. Overview of SB 911 continued… The bill passed unanimously in the House and Senate in August,
- 10. Overview of SB 911 continued… Implications for NC Schools Guidelines adopted in every school in the
- 11. Overview of SB 911 continued… Section 1 of SB 911 Procedures for the development of a
- 12. Overview of SB 911 continued… Section 2 of SB 911 Local Boards of Education must ensure
- 13. Section 3 of SB 911 The NC State Board of Education delivered a progress report in
- 14. Overview of SB 911 continued… Please refer to your copy of the ADA Standards. An Individual
- 15. Overview of SB 911 continued… Children should have immediate access to diabetes supplies and diabetes treatments
- 16. G.S. 115C-375.3 April 28, 2005 House Bill 496 states that local boards of education shall ensure
- 17. Forms to Facilitate Implementation of the Law Diabetes Care Plan Request Diabetes Care Plan Responsibilities of
- 18. Role of the Master Trainer (One RN and One 504 Coordinator from each LEA) Participate in
- 19. Communication- Role of Nurse With student, parent & school staff SB-911 Diabetes School Act Provide forms
- 20. Communication With student and parent before school year begins By phone, meeting at the library, by
- 21. Communicate: Self Care Procedures done at school Equipment kept at school Diabetes care recommendations may change
- 22. Communicate: Parent Responsibilities Phone numbers Home, work, cell, pager Supplies Snacks School absences Care Plan request
- 23. Customize: Parent Request Form No MD signature required Request for Care Plan to be implemented Consent
- 24. Communicate: Parent Responsibilities Student, parent or 9-1-1 may have to assume responsibility for diabetes care until
- 25. Role of the DCM Diabetes Care Managers in Each School Participate in the Intensive training session.
- 26. DCM Roles continued… Communicate with teachers/substitute teachers/student/parents/health care team as indicated or as necessary. Assist the
- 27. Role of the 504 Contact in Each School Attend general information session instructed by the 504
- 28. Guidelines for PE Teacher and Coach Encourage exercise and participation in sports and physical activities for
- 29. Guidelines for Bus Drivers At the beginning of the school year, identify any students on the
- 30. Actions for Food Service Staff or Lunchroom Monitor Provide a lunch menu and lunch schedule in
- 31. Role of School Administration Work with the LEA Master Trainers to identify at least 2 school
- 32. Role of School Administration continued… Notify the Master Trainers for the school when such turnovers occur
- 33. Liability Concerns and Issues for DCMs How do I prevent liability situations from occurring? Be very
- 34. Liability Concerns and Issues Remember, a vial of insulin kept at room temperature is discarded 30
- 35. Liability Concerns and Issues continued… What happens if there is an occurrence? Most incidents occur when
- 36. Liability Concerns and Issues continued… If you give too much insulin Notify the student’s health care
- 37. Liability Concerns and Issues continued… If you give too little insulin, an additional shot can be
- 38. Liability Concerns and Issues continued… But how am I protected from litigation? The State of NC
- 39. Liability Concerns and Issues continued… Do I have any other protections? NC General Statute 90-21.14 adopted
- 40. Liability Concerns and Issues continued… So what needs to happen in my school? You as DCM,
- 41. Liability Concerns and Issues continued… So what about sharps, blood, carrying medication around the school? Self-monitoring
- 42. Continued Glucose Tabs are not medication. Some students with diabetes should be monitored at all times
- 43. Questions ??
- 44. Part 2: Diabetes Overview Diabetes Defined: “Diabetes Mellitus is a group of metabolic diseases characterized by
- 45. Diabetes Overview continued… Insulin is a hormone produced in the beta or islet cells of the
- 46. Diabetes Overview continued… Type 1: *Has been called Juvenile-Onset or Insulin Dependent Diabetes in the past.
- 47. Diabetes Overview continued… Type 2: * Has been called Adult-Onset or Non-Insulin-Dependent Diabetes. * Characterized by
- 48. Diabetes Overview continued… Insulin resistance means that insulin is produced, but the body is not using
- 49. Diabetes Overview continued… Reasons for Control: Diabetes is the 7th leading cause of death in the
- 50. Diabetes Overview continued… The goal of effective diabetes management is to control blood glucose levels by
- 51. Diabetes Overview continued… Diabetes management means monitoring or checking blood glucose levels throughout the day. Planning
- 52. Diabetes Overview continued… The Good News: The “Diabetes Control And Complications Trial” (DCCT) of 1993, clearly
- 53. Treatment Foundations: Type 1 diabetes: Occurs in approximately 1:400 children (10% of the diabetes population.) Often
- 54. Treatment Foundations: Currently, most students are taking insulin by syringe, pen device, or insulin pump. The
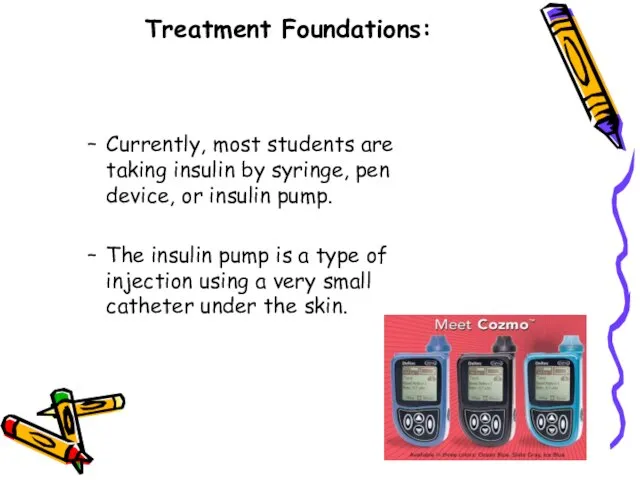
- 55. Treatment Foundations: The amount of insulin taken has to be balanced with food intake (specifically carbohydrates)
- 56. Treatment Foundations: Type 2 diabetes: Most often occurs in the adult population. Accounts for 90% of
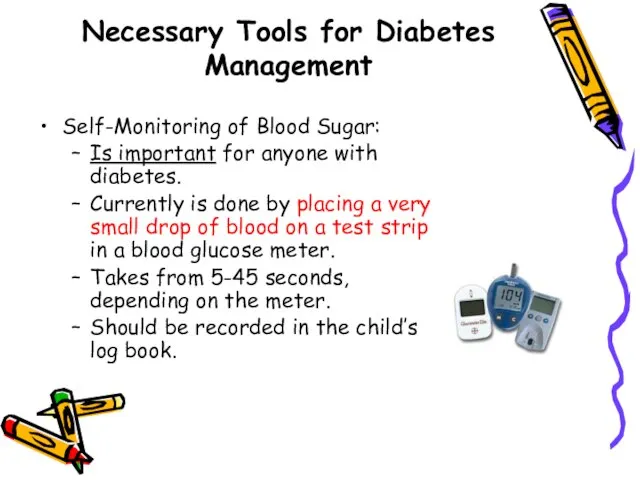
- 57. Necessary Tools for Diabetes Management Self-Monitoring of Blood Sugar: Is important for anyone with diabetes. Currently
- 58. Necessary Tools continued… Blood Sugar Monitoring If you need to assist a child with blood sugar
- 59. Blood Sugar Monitoring continued… Prick the fleshy part on the side of the fingertip (may use
- 60. Blood Sugar Monitoring continued… If the school has a meter that is kept in the office
- 61. Necessary Tools continued… Carbohydrate Counting and the Meal Plan Students with Type 1 diabetes may practice
- 63. Insulin Action and Administration Most students take at least two injections of insulin a day. Some
- 64. What is an insulin pump? A battery operated device about the size of a pager
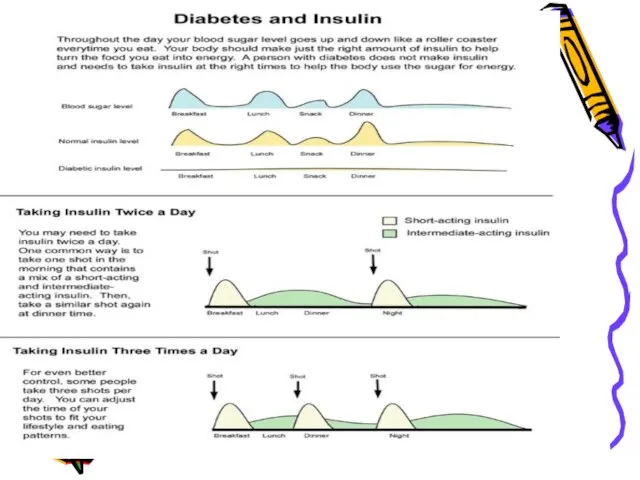
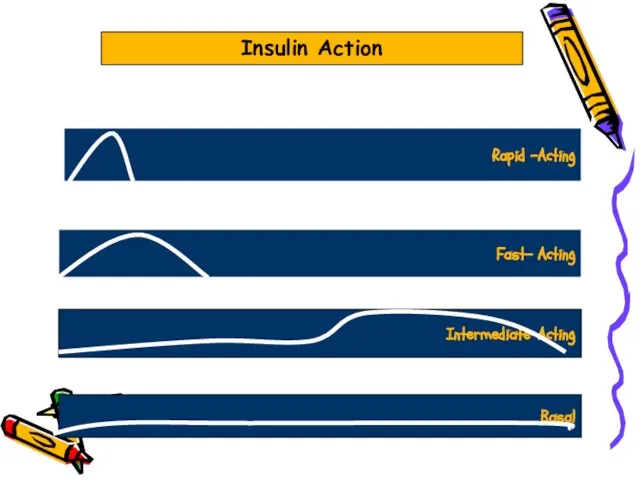
- 65. Insulin Action Insulin types are categorized as rapid-acting, fast-acting, intermediate-acting, long-acting or basal. Each type has
- 66. Rapid -Acting Fast- Acting Intermediate-Acting Basal Insulin Action
- 67. Insulin Administration After carefully drawing up the correct amount of insulin, cleanse the injection site with
- 68. Insulin Administration-Continued After pushing the plunger on the syringe, count slowly to five and remove the
- 69. Carb Counting, Insulin to Carb Ratios Many students are now using an algorithm instead of a
- 70. Insulin to Carb Ratio In an effort to match insulin to carbohydrate eaten, an insulin to
- 71. Combining the Two In order to correctly determine the amount of insulin needed before a meal,
- 72. Insulin to Carb Ratios and the Insulin Pump Most insulin pumps today are far more sophisticated
- 73. Oral Meds for Kids With Type 2 Diabetes The preferred method of treating Type 2 diabetes
- 74. Oral Meds The most frequently used medication for increasing insulin sensitivity in Type 2 diabetes in
- 75. Oral Meds It is important to note that some kids with Type 2 diabetes may at
- 76. Part 3 Acute Complications of Diabetes Hyperglycemia (High Blood Sugar) Hypoglycemia (Low Blood Sugar)
- 77. High Blood Sugar “Hyperglycemia”
- 78. Hyperglycemia High blood glucose (hyperglycemia) occurs when the body gets too little insulin, too much food,
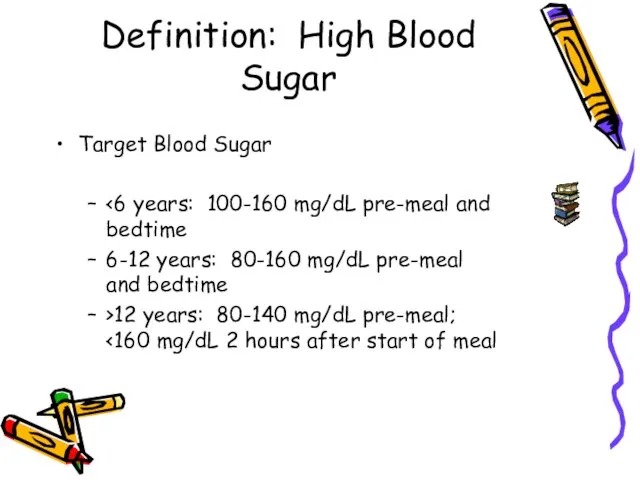
- 79. Definition: High Blood Sugar Target Blood Sugar 6-12 years: 80-160 mg/dL pre-meal and bedtime >12 years:
- 80. Definition: High Blood Sugar Most health professionals view a blood sugar greater than 240 as “hyperglycemia.”
- 81. Signs & Symptoms of Hyperglycemia Frequent Urination Extreme Hunger Extreme Fatigue Unusual Thirst Irritability Blurred Vision
- 82. High Blood Sugar “Hyperglycemia” For the school age child, a blood sugar greater than 240 mg/dL
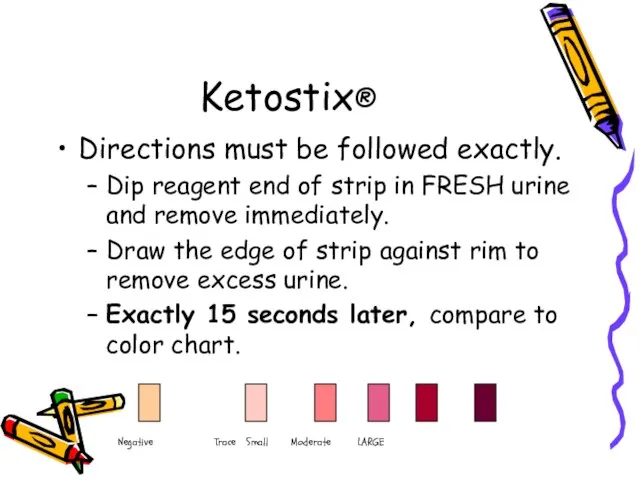
- 83. Ketostix® Directions must be followed exactly. Dip reagent end of strip in FRESH urine and remove
- 84. If a student’s ketone level is greater than “trace” but less than “large”, refer to that
- 85. In the event of moderate to large ketones, treat as an emergency situation according to the
- 86. In all cases of high blood sugar, if the student is able, he should drink calorie-free,
- 87. Diabetic Ketoacidosis-DKA If untreated over a period of time, high blood sugar can cause a serious
- 88. Diabetic Ketoacidosis For students using insulin infusion pumps, lack of insulin supply may lead to DKA
- 89. Diabetic Ketoacidosis Ketones in the bloodstream cause the pH of the blood and body fluids to
- 90. Any Questions???
- 91. Low Blood Sugar “Hypoglycemia”
- 92. What Is Hypoglycemia or Low Blood Sugar? Sometimes called an insulin reaction Occurs when blood sugar
- 93. Lows happen when insulin and blood sugar are out of balance. People without diabetes do not
- 94. Low blood glucose levels, which can be life-threatening, present the greatest immediate danger to people with
- 95. Signs and Symptoms of Low Blood Sugar Hunger Shakiness Dizziness Sweatiness Fast heartbeat Drowsiness Feeling irritable,
- 96. More Signs and Symptoms of Low Blood Sugars Feeling sleepy Being stubborn Lack of coordination Tingling
- 97. Recognizing Low Blood Sugar It is important to recognize a low blood sugar as soon as
- 98. Frequent Causes of Low Blood Sugar Meals that are late or missed Extra exercise or activity
- 99. What To Do When Hypoglycemia Occurs If possible always do a blood sugar check first. If
- 100. Hypoglycemia Busters 2-4 glucose tablets 4 ounces of apple or orange juice 4-6 ounces of regular
- 101. Catch Low Blood Sugar Early Be alert for any symptoms and times when a low blood
- 102. Treating Severe Hypoglycemia When severe hypoglycemia occurs, not enough sugar is in the brain. The student
- 103. What Happens when the Child is Unconscious? Drinking soda or eating glucose tablets is not possible
- 104. Using Glucagon Glucagon should be administered promptly if the person is unable to swallow, loses consciousness
- 105. In order for school staff to use Glucagon, orders for its use must be included on
- 107. Скачать презентацию


 Тестовый контроль
Тестовый контроль Чумная палочка
Чумная палочка Инциденталома надпочечника, синдромы, связанные с ней
Инциденталома надпочечника, синдромы, связанные с ней Таргетная терапия у онкологических больных
Таргетная терапия у онкологических больных Гигиена опорно-двигательной системы
Гигиена опорно-двигательной системы Кисты почек
Кисты почек Біорітми
Біорітми Правовое регулирование трансплантологии
Правовое регулирование трансплантологии дезінфекція2
дезінфекція2 Защитно-приспособительные реакции при гипоксии
Защитно-приспособительные реакции при гипоксии Биологиялық белсенді нүктелер және рефлексотерапия принциптері
Биологиялық белсенді нүктелер және рефлексотерапия принциптері Гастроэнтерит. дДифференциальная диагностика с ОКИ и инвазия
Гастроэнтерит. дДифференциальная диагностика с ОКИ и инвазия Эндокринология. Диагностика Анамнез, осмотр БХК, глюкоза-экспресс, ОАК, УЗИ, рентген
Эндокринология. Диагностика Анамнез, осмотр БХК, глюкоза-экспресс, ОАК, УЗИ, рентген Правила наложения повязок
Правила наложения повязок Report on EEE disease
Report on EEE disease Индекс пострефлюксной глоток-индуцированной перистальтической волны – метод оценки эффективности пищеводного клиренса
Индекс пострефлюксной глоток-индуцированной перистальтической волны – метод оценки эффективности пищеводного клиренса Цистит. Виды цистита. Лечение цистита
Цистит. Виды цистита. Лечение цистита Физиология сердечно-сосудистой системы
Физиология сердечно-сосудистой системы Доврачебная помощь пострадавшим
Доврачебная помощь пострадавшим Первая медицинская помощь ОБЖ. Лекция 1. Искусственное дыхание и непрямой массаж сердца
Первая медицинская помощь ОБЖ. Лекция 1. Искусственное дыхание и непрямой массаж сердца Скоропостижная смерть в структуре смертности как важный индикатор демографических процессов
Скоропостижная смерть в структуре смертности как важный индикатор демографических процессов Безопасная больничная среда
Безопасная больничная среда Диуретики
Диуретики Туристический маршрут в музей-заповедник Прохоровское поле
Туристический маршрут в музей-заповедник Прохоровское поле Влияние различных забол. на беремен.5-6Доврачебная
Влияние различных забол. на беремен.5-6Доврачебная Эндометриоз: болезнь работающих женщин?! Взгляд с позиций психосоматики
Эндометриоз: болезнь работающих женщин?! Взгляд с позиций психосоматики Значение жидкости для организма
Значение жидкости для организма Повышение стрессоустойчивости с новым набором от НСП Антистресс
Повышение стрессоустойчивости с новым набором от НСП Антистресс