- Главная
- Английский язык
- Tissue parasites

Содержание
- 3. LEISHMANIA 4/9/2020 prof. Mahi Ghobashy
- 4. 4/9/2020 prof. Mahi Ghobashy
- 6. دورة حياة الليشمانيا 4/9/2020 prof. Mahi Ghobashy
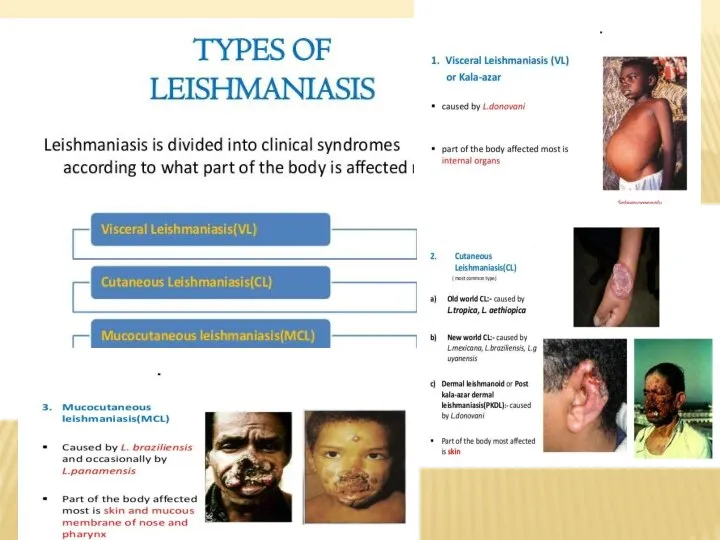
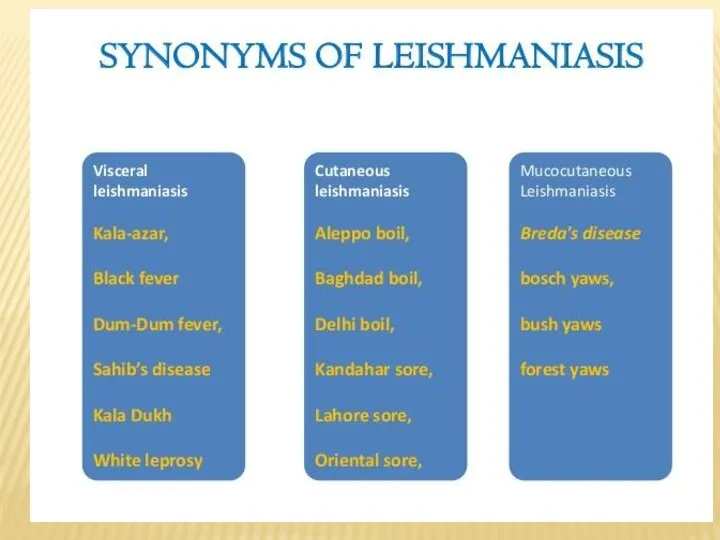
- 8. Clinical Features: Human leishmanial infections can result in 2 main forms of disease, cutaneous leishmaniasis and
- 9. TOXOPLASMA GONDII Causal Agent: Toxoplasma gondii that infects most species of warm blooded animals, including humans,
- 10. Definitive hosts for Toxoplasma gondii are members of family Felidae (domestic cats and their relatives). Unsporulated
- 12. 4/9/2020 prof. Mahi Ghobashy
- 13. In the human host, the parasites form tissue cysts, most commonly in skeletal muscle, myocardium, brain,
- 14. Laboratory Diagnosis: The diagnosis of toxoplasmosis may be documented by: Observation of parasites in patient specimens,
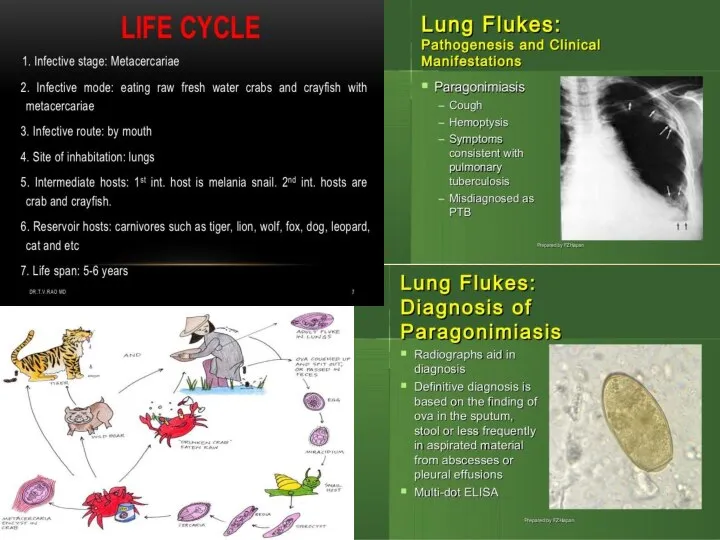
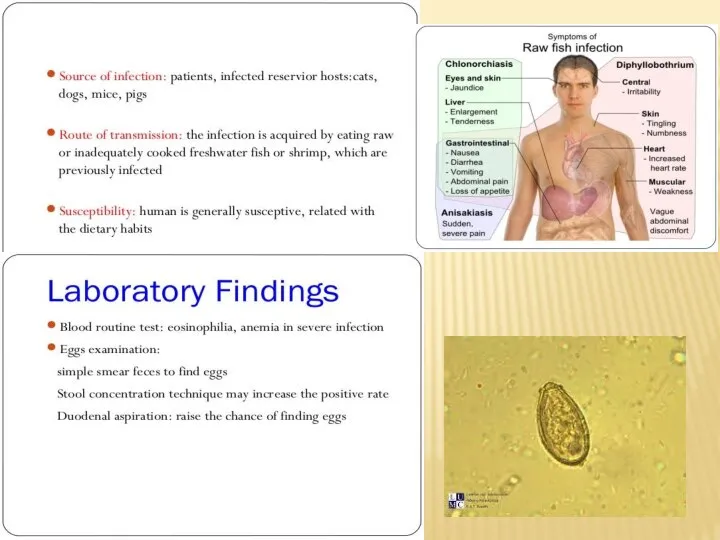
- 15. Paragonimus westermani is the major species of lung fluke that infects humans, causing paragonimiasis. The species
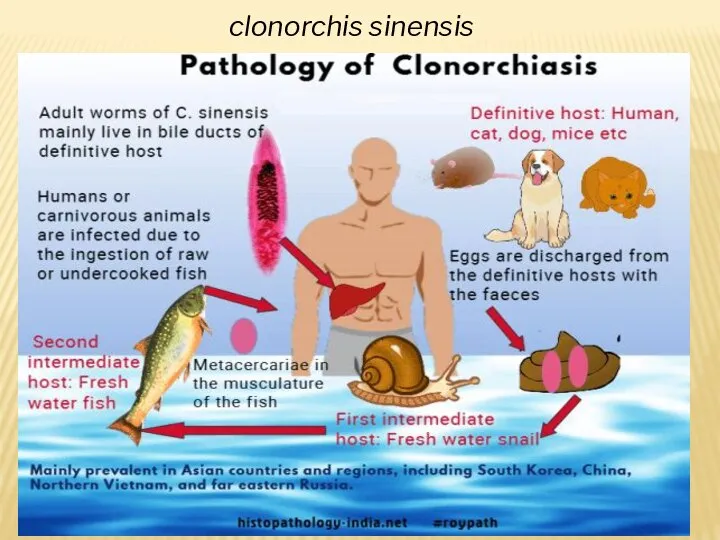
- 17. clonorchis sinensis
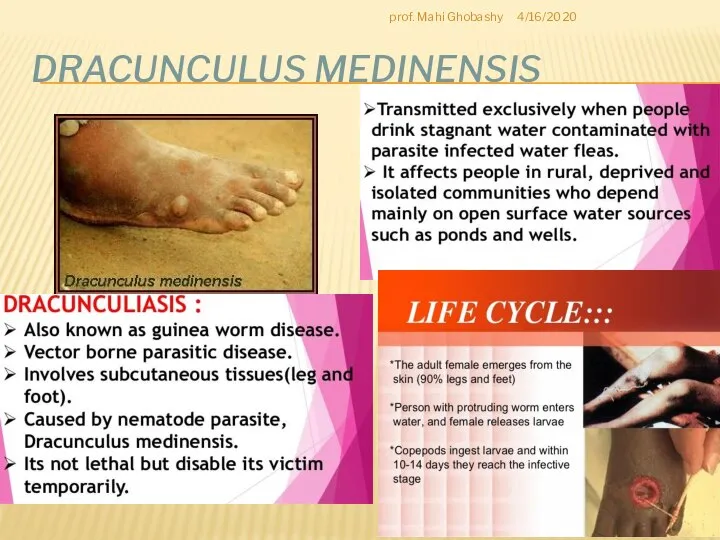
- 19. DRACUNCULUS MEDINENSIS 4/16/2020 prof. Mahi Ghobashy
- 23. Скачать презентацию
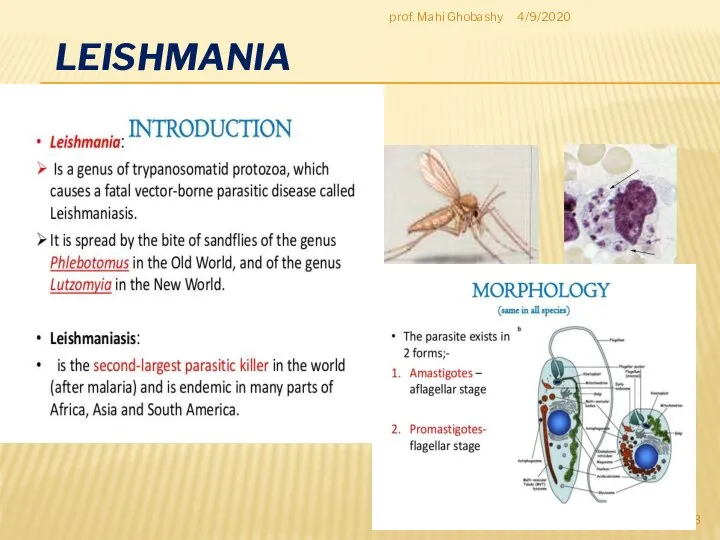
Слайд 3LEISHMANIA
4/9/2020
prof. Mahi Ghobashy
LEISHMANIA
4/9/2020
prof. Mahi Ghobashy
Слайд 44/9/2020
prof. Mahi Ghobashy
4/9/2020
prof. Mahi Ghobashy

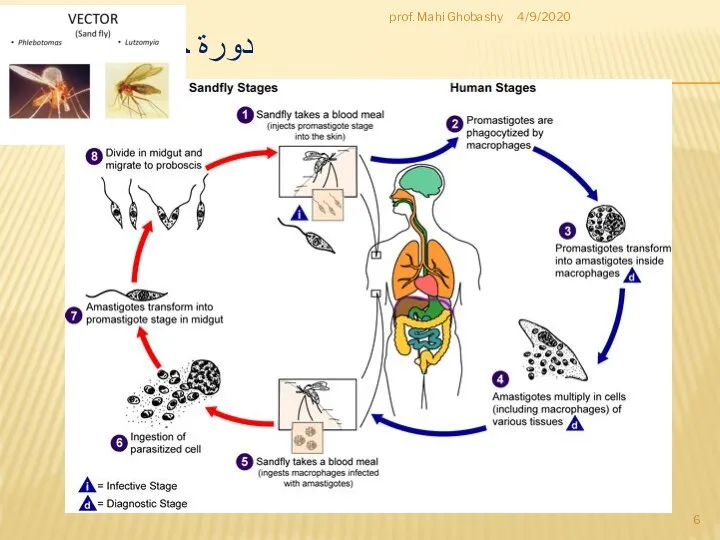
Слайд 6دورة حياة الليشمانيا
4/9/2020
prof. Mahi Ghobashy
دورة حياة الليشمانيا
4/9/2020
prof. Mahi Ghobashy
Слайд 8Clinical Features:
Human leishmanial infections can result in 2 main forms of disease,
Clinical Features: Human leishmanial infections can result in 2 main forms of disease,
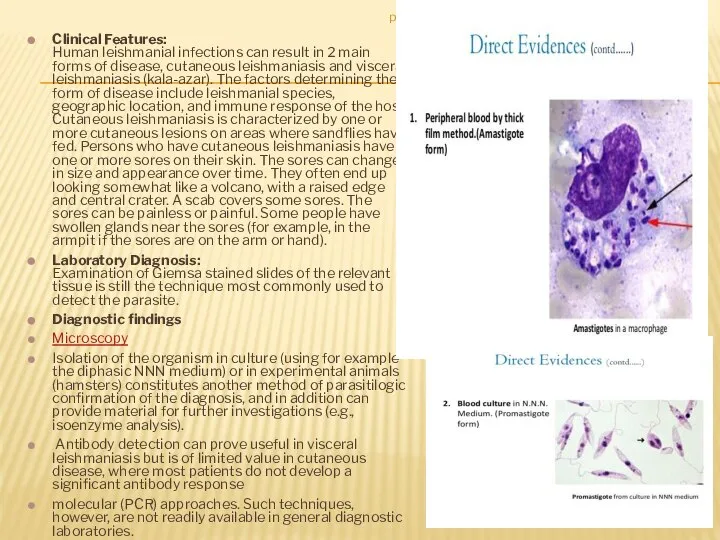
Laboratory Diagnosis: Examination of Giemsa stained slides of the relevant tissue is still the technique most commonly used to detect the parasite.
Diagnostic findings
Microscopy
Isolation of the organism in culture (using for example the diphasic NNN medium) or in experimental animals (hamsters) constitutes another method of parasitilogic confirmation of the diagnosis, and in addition can provide material for further investigations (e.g., isoenzyme analysis).
Antibody detection can prove useful in visceral leishmaniasis but is of limited value in cutaneous disease, where most patients do not develop a significant antibody response
molecular (PCR) approaches. Such techniques, however, are not readily available in general diagnostic laboratories.
4/9/2020
prof. Mahi Ghobashy
Слайд 9TOXOPLASMA GONDII
Causal Agent:
Toxoplasma gondii that infects most species of warm blooded animals,
TOXOPLASMA GONDII
Causal Agent: Toxoplasma gondii that infects most species of warm blooded animals,
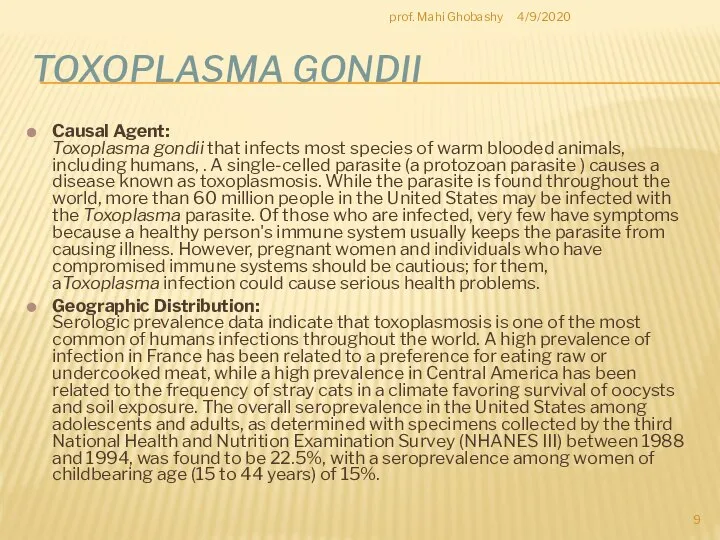
Geographic Distribution: Serologic prevalence data indicate that toxoplasmosis is one of the most common of humans infections throughout the world. A high prevalence of infection in France has been related to a preference for eating raw or undercooked meat, while a high prevalence in Central America has been related to the frequency of stray cats in a climate favoring survival of oocysts and soil exposure. The overall seroprevalence in the United States among adolescents and adults, as determined with specimens collected by the third National Health and Nutrition Examination Survey (NHANES III) between 1988 and 1994, was found to be 22.5%, with a seroprevalence among women of childbearing age (15 to 44 years) of 15%.
4/9/2020
prof. Mahi Ghobashy
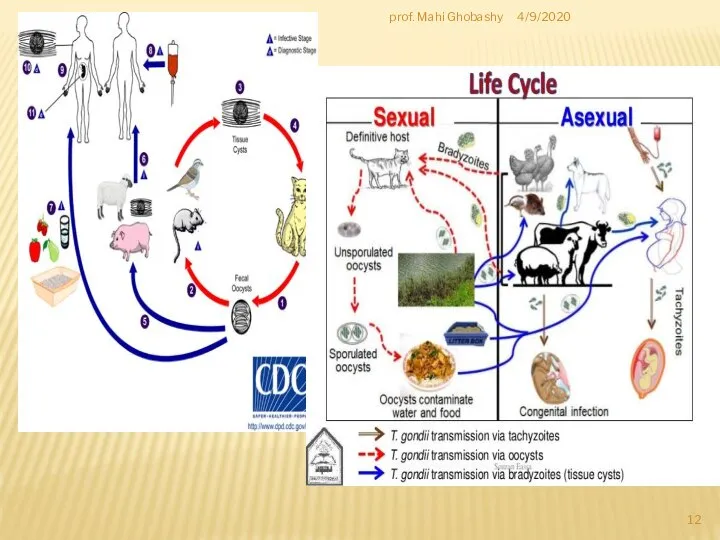
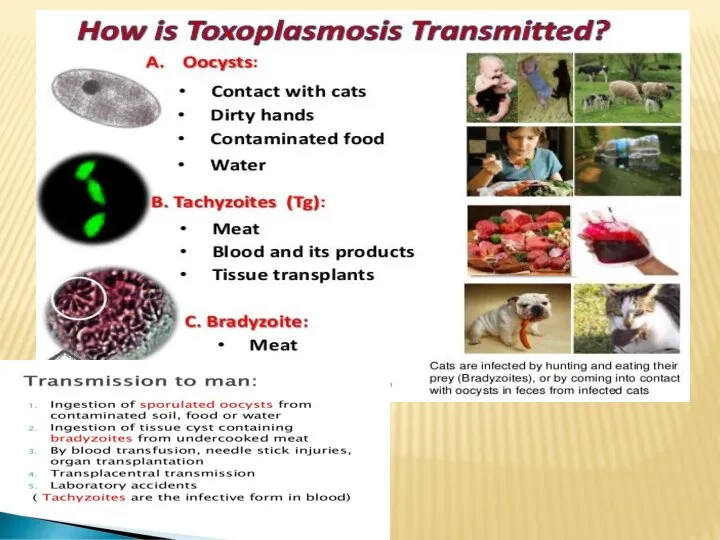
Слайд 10Definitive hosts for Toxoplasma gondii are members of family Felidae (domestic cats
Definitive hosts for Toxoplasma gondii are members of family Felidae (domestic cats
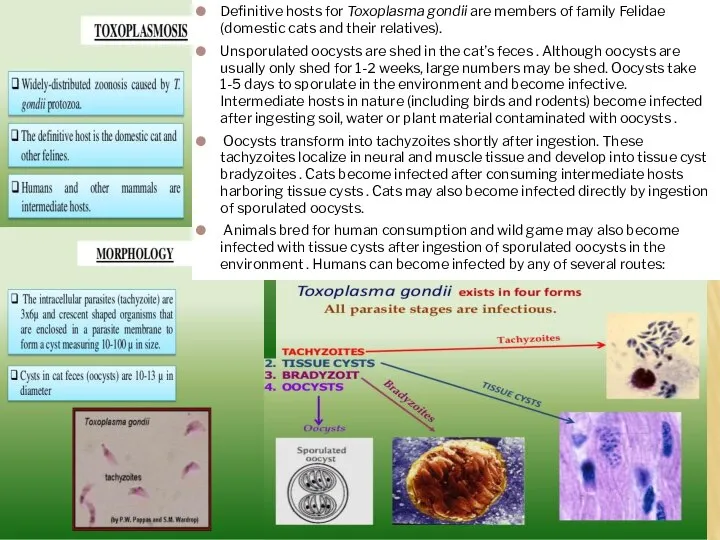
Unsporulated oocysts are shed in the cat’s feces . Although oocysts are usually only shed for 1-2 weeks, large numbers may be shed. Oocysts take 1-5 days to sporulate in the environment and become infective. Intermediate hosts in nature (including birds and rodents) become infected after ingesting soil, water or plant material contaminated with oocysts .
Oocysts transform into tachyzoites shortly after ingestion. These tachyzoites localize in neural and muscle tissue and develop into tissue cyst bradyzoites . Cats become infected after consuming intermediate hosts harboring tissue cysts . Cats may also become infected directly by ingestion of sporulated oocysts.
Animals bred for human consumption and wild game may also become infected with tissue cysts after ingestion of sporulated oocysts in the environment . Humans can become infected by any of several routes:
Слайд 124/9/2020
prof. Mahi Ghobashy
4/9/2020
prof. Mahi Ghobashy
Слайд 13
In the human host, the parasites form tissue cysts, most commonly
In the human host, the parasites form tissue cysts, most commonly
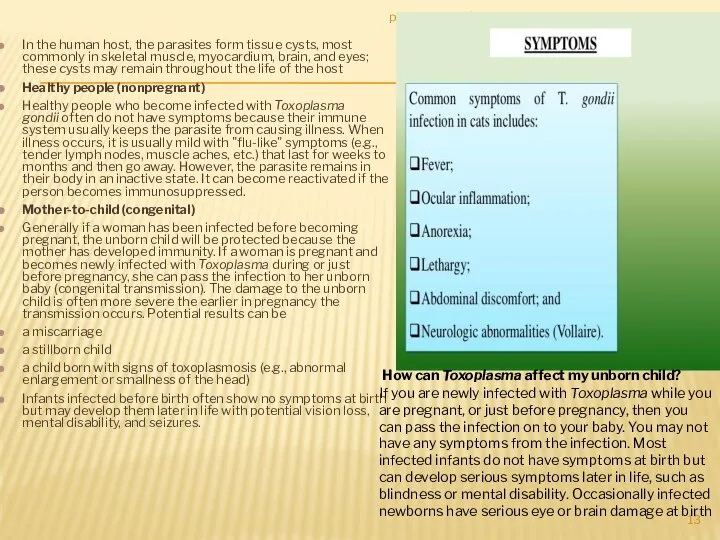
Healthy people (nonpregnant)
Healthy people who become infected with Toxoplasma gondii often do not have symptoms because their immune system usually keeps the parasite from causing illness. When illness occurs, it is usually mild with "flu-like" symptoms (e.g., tender lymph nodes, muscle aches, etc.) that last for weeks to months and then go away. However, the parasite remains in their body in an inactive state. It can become reactivated if the person becomes immunosuppressed.
Mother-to-child (congenital)
Generally if a woman has been infected before becoming pregnant, the unborn child will be protected because the mother has developed immunity. If a woman is pregnant and becomes newly infected with Toxoplasma during or just before pregnancy, she can pass the infection to her unborn baby (congenital transmission). The damage to the unborn child is often more severe the earlier in pregnancy the transmission occurs. Potential results can be
a miscarriage
a stillborn child
a child born with signs of toxoplasmosis (e.g., abnormal enlargement or smallness of the head)
Infants infected before birth often show no symptoms at birth but may develop them later in life with potential vision loss, mental disability, and seizures.
4/9/2020
prof. Mahi Ghobashy
How can Toxoplasma affect my unborn child?
If you are newly infected with Toxoplasma while you are pregnant, or just before pregnancy, then you can pass the infection on to your baby. You may not have any symptoms from the infection. Most infected infants do not have symptoms at birth but can develop serious symptoms later in life, such as blindness or mental disability. Occasionally infected newborns have serious eye or brain damage at birth
Слайд 14Laboratory Diagnosis:
The diagnosis of toxoplasmosis may be documented by:
Observation of parasites in
Laboratory Diagnosis:
The diagnosis of toxoplasmosis may be documented by:
Observation of parasites in
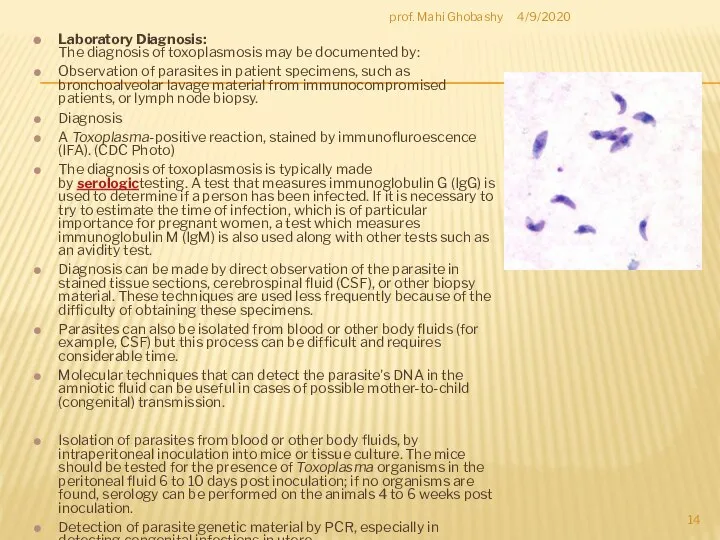
Diagnosis
A Toxoplasma-positive reaction, stained by immunofluroescence (IFA). (CDC Photo)
The diagnosis of toxoplasmosis is typically made by serologictesting. A test that measures immunoglobulin G (IgG) is used to determine if a person has been infected. If it is necessary to try to estimate the time of infection, which is of particular importance for pregnant women, a test which measures immunoglobulin M (IgM) is also used along with other tests such as an avidity test.
Diagnosis can be made by direct observation of the parasite in stained tissue sections, cerebrospinal fluid (CSF), or other biopsy material. These techniques are used less frequently because of the difficulty of obtaining these specimens.
Parasites can also be isolated from blood or other body fluids (for example, CSF) but this process can be difficult and requires considerable time.
Molecular techniques that can detect the parasite's DNA in the amniotic fluid can be useful in cases of possible mother-to-child (congenital) transmission.
Isolation of parasites from blood or other body fluids, by intraperitoneal inoculation into mice or tissue culture. The mice should be tested for the presence of Toxoplasma organisms in the peritoneal fluid 6 to 10 days post inoculation; if no organisms are found, serology can be performed on the animals 4 to 6 weeks post inoculation.
Detection of parasite genetic material by PCR, especially in detecting congenital infections in utero.
Serologic testing is the routine method of diagnosis.
Diagnostic findings Microscopy
Antibody detection
4/9/2020
prof. Mahi Ghobashy
Слайд 15Paragonimus westermani is the major species of lung fluke that infects humans, causing paragonimiasis.
Paragonimus westermani is the major species of lung fluke that infects humans, causing paragonimiasis.
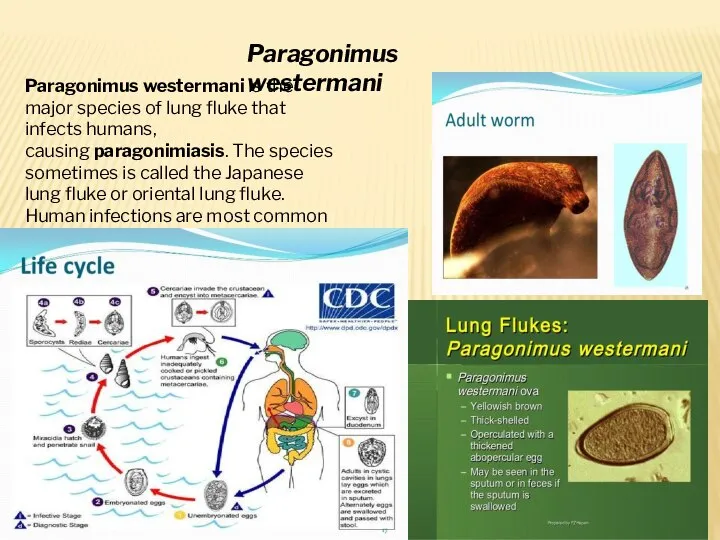
Paragonimus westermani
Слайд 17clonorchis sinensis
clonorchis sinensis
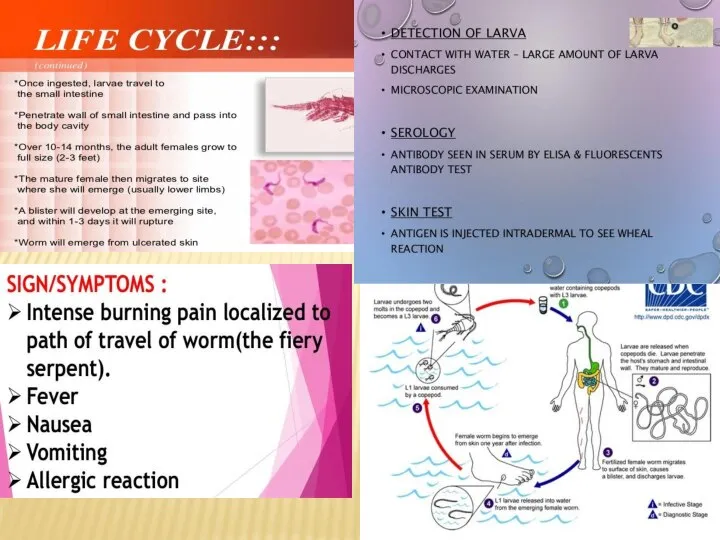
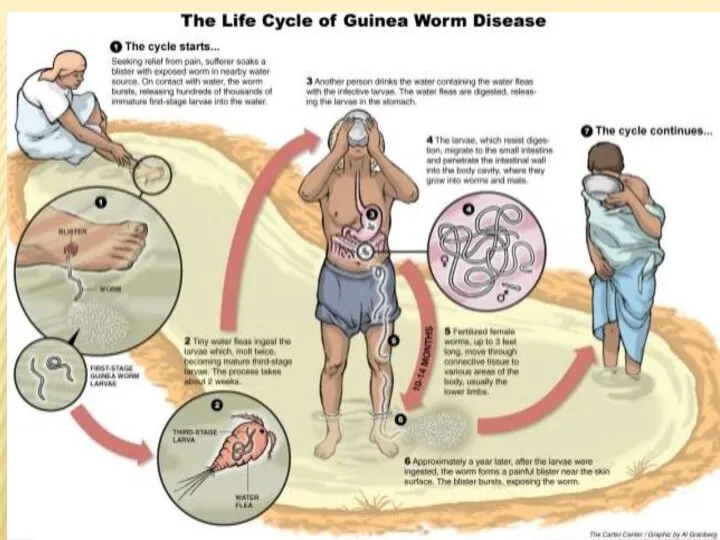
Слайд 19DRACUNCULUS MEDINENSIS
4/16/2020
prof. Mahi Ghobashy
DRACUNCULUS MEDINENSIS
4/16/2020
prof. Mahi Ghobashy
 Moscow is the largest and one of the most beautiful cities in Russia
Moscow is the largest and one of the most beautiful cities in Russia Past Simple. Test
Past Simple. Test What can you see?
What can you see?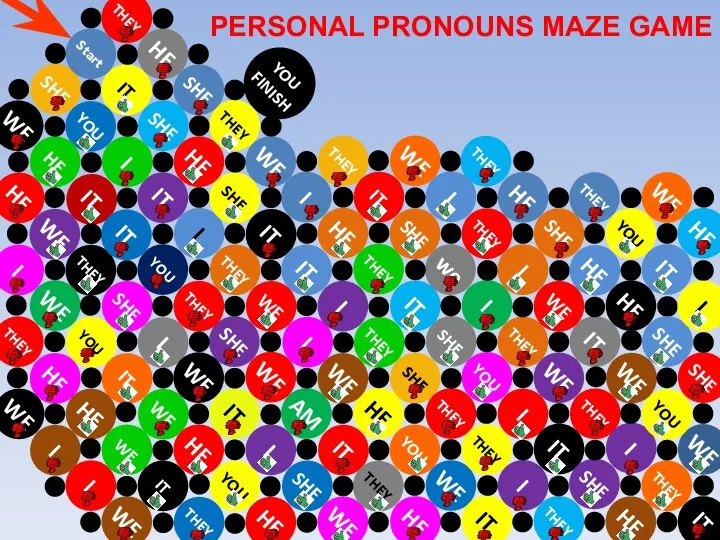 Personal pronoun game
Personal pronoun game Present Simple & Continuous sentences
Present Simple & Continuous sentences There is no place like home
There is no place like home Ghost-busters
Ghost-busters My hero is Leonidas — king of Sparta
My hero is Leonidas — king of Sparta Инфинитив. The Infinitive
Инфинитив. The Infinitive Max’s family
Max’s family Which one of the five is least like the other four
Which one of the five is least like the other four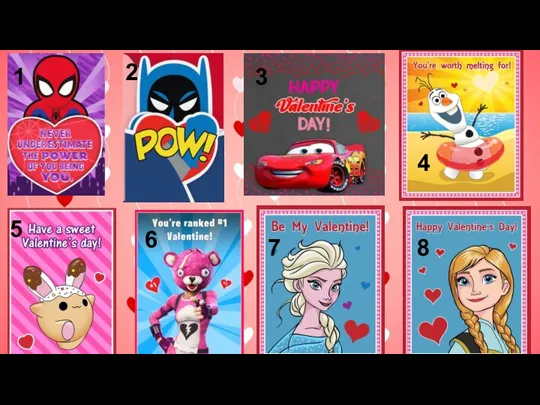 Interactive english valentine's day. Cards and bags
Interactive english valentine's day. Cards and bags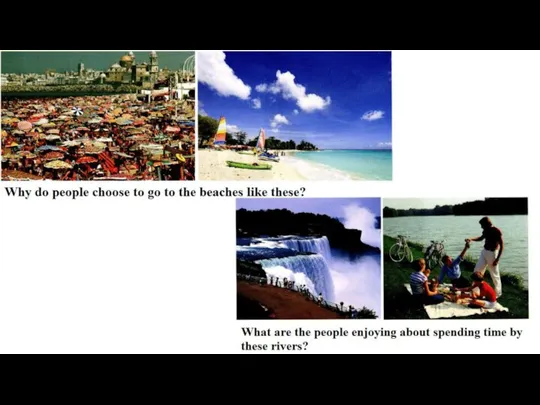 Discuss pics
Discuss pics My favourite gymnast
My favourite gymnast Present Perfect-Past Simple
Present Perfect-Past Simple My family's favorite dish
My family's favorite dish Breaking the ice. Present simple or present continuous
Breaking the ice. Present simple or present continuous 4 stars of the Moulin Rouge
4 stars of the Moulin Rouge Eyes for seeing, legs for walking, Tongue for tasting and for talking
Eyes for seeing, legs for walking, Tongue for tasting and for talking Презентация на тему Canada
Презентация на тему Canada  Holiday story. Jack's Christmas present
Holiday story. Jack's Christmas present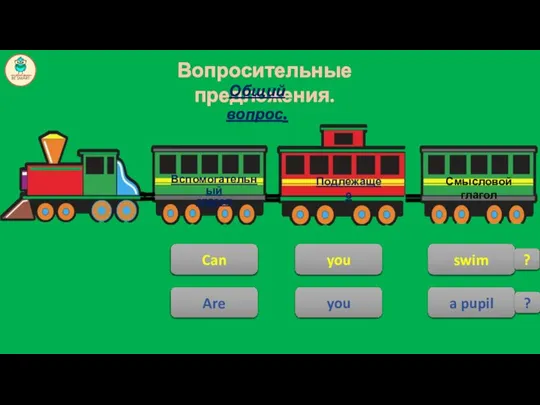 Структура английского предложения
Структура английского предложения Семья, родственники. Familу
Семья, родственники. Familу Integrating Sources. Week 2. Lesson 2
Integrating Sources. Week 2. Lesson 2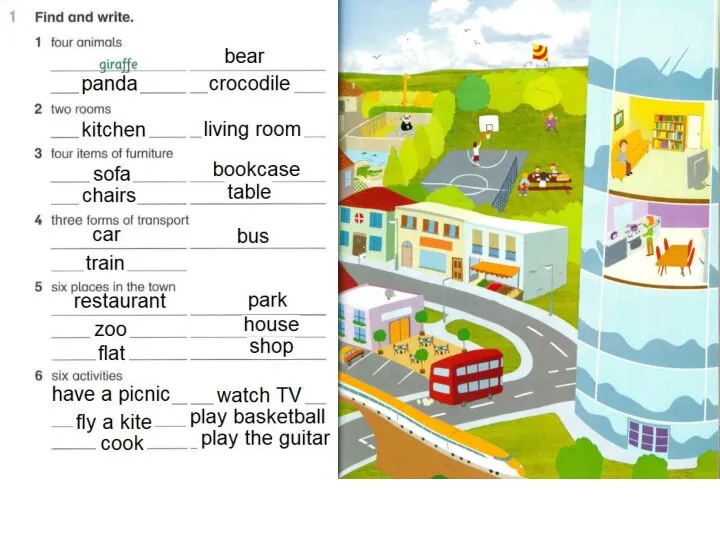 Город. Английский язык
Город. Английский язык Present Simple
Present Simple Automobile
Automobile Opposites
Opposites