Содержание
- 2. The bleeding disorders is a group of diseases with increased bleeding, which is based on disorders
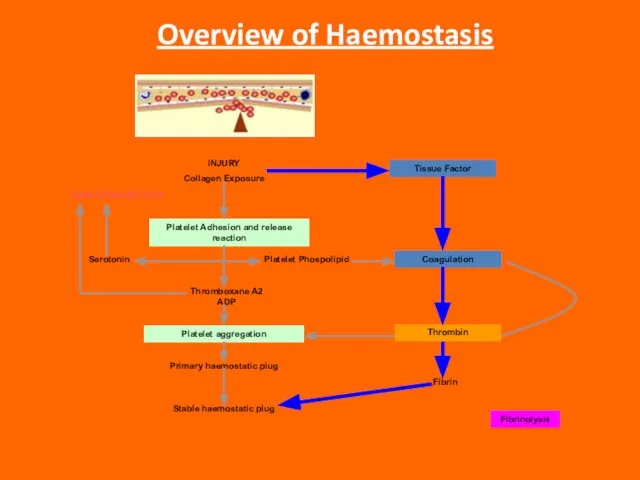
- 3. Overview of Haemostasis INJURY Collagen Exposure Platelet Adhesion and release reaction Platelet aggregation VASOCONSTRICTION Serotonin Platelet
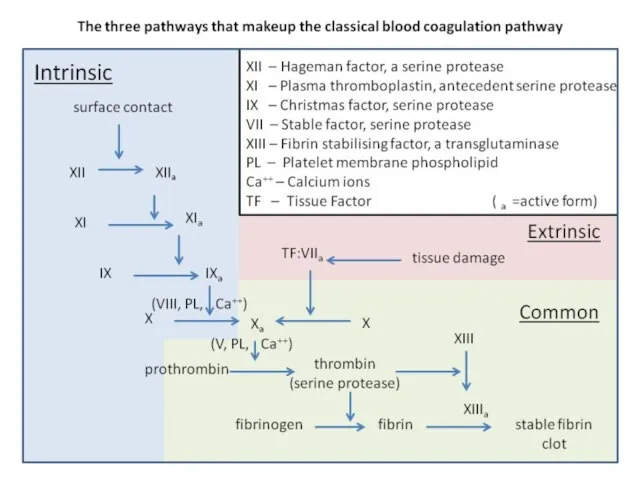
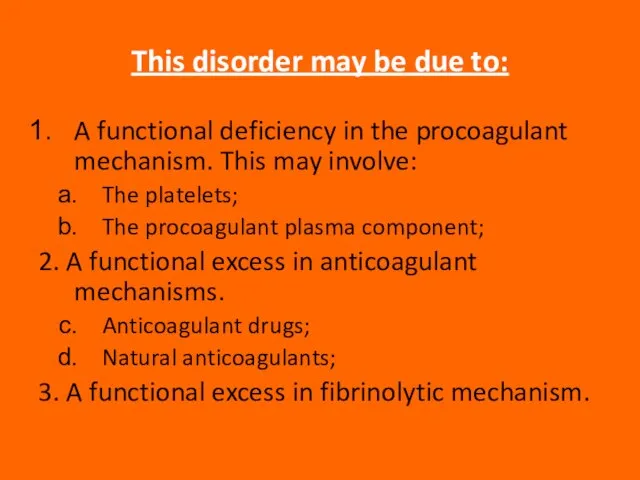
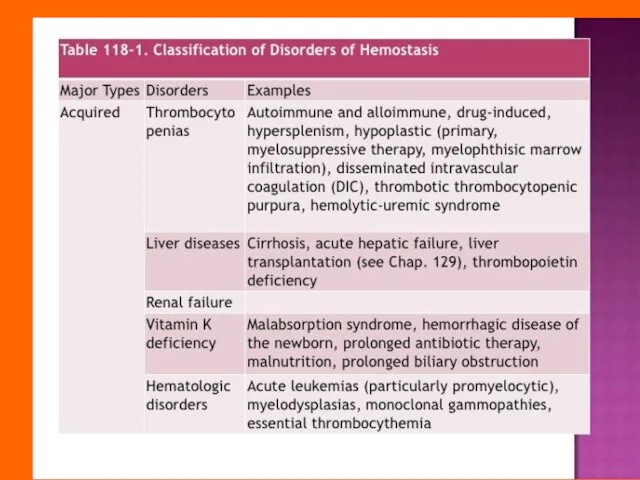
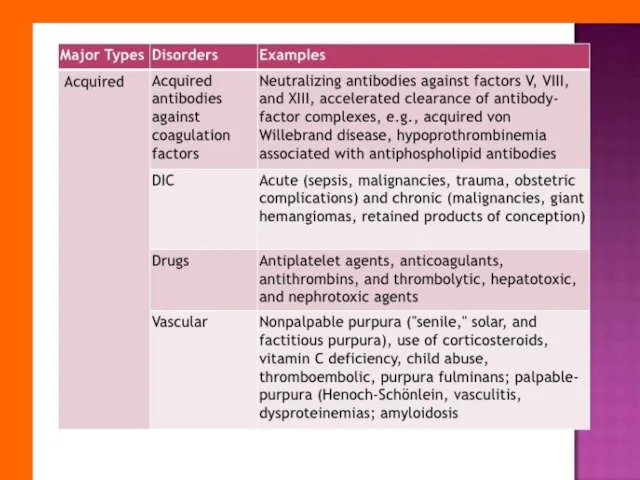
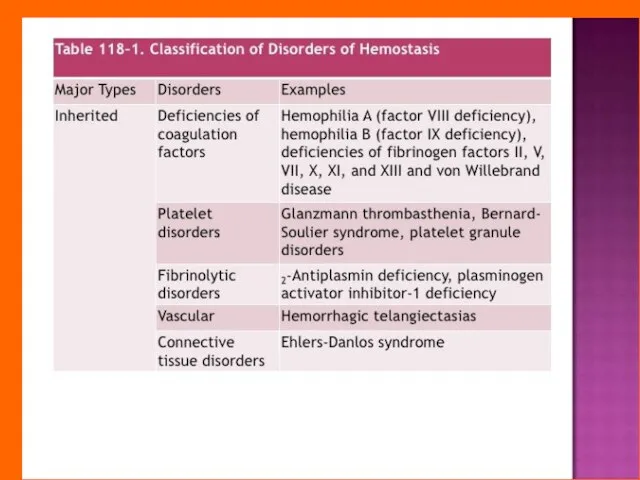
- 7. This disorder may be due to: A functional deficiency in the procoagulant mechanism. This may involve:
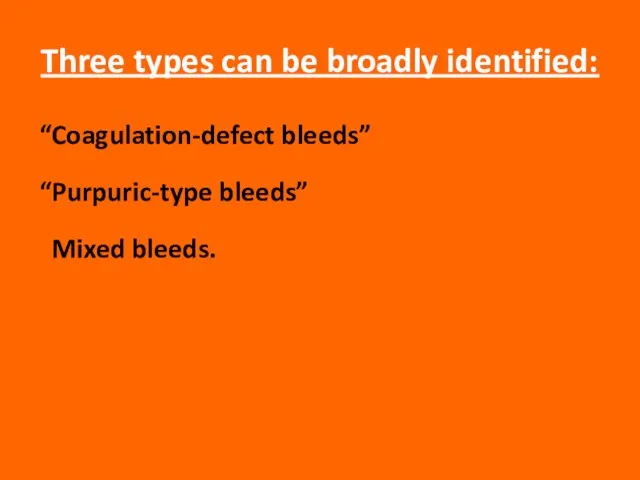
- 8. Three types can be broadly identified: “Coagulation-defect bleeds” “Purpuric-type bleeds” Mixed bleeds.
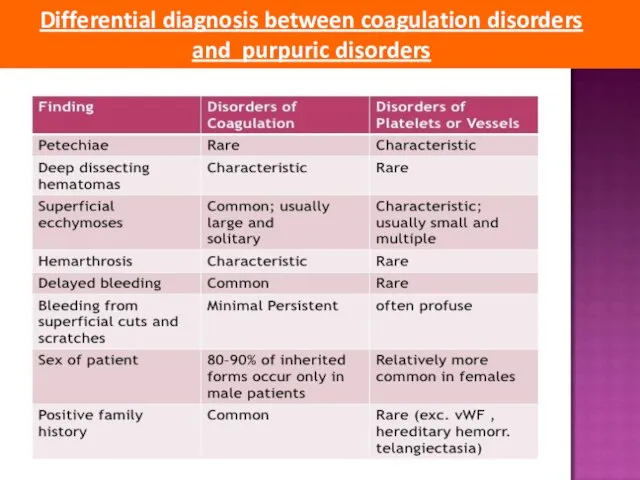
- 9. Differential diagnosis between coagulation disorders and purpuric disorders
- 13. Bleeding history The bleeding history forms the basis of the laboratory tests and therapy. Asking patients
- 14. Physical Examination Several clinical as well as laboratory features help differentiate clinical disorders associated with qualitative
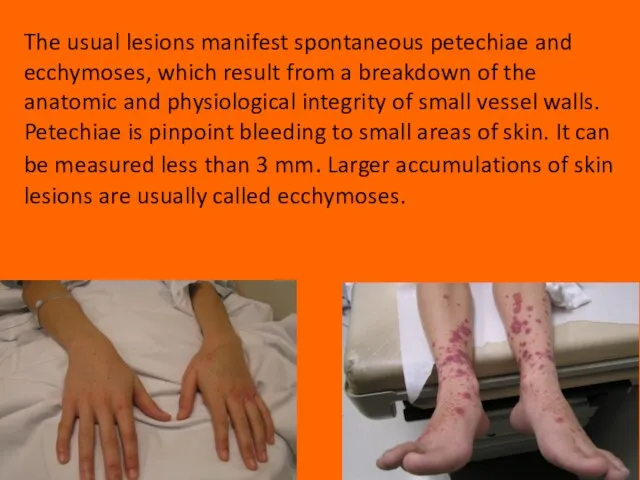
- 15. The usual lesions manifest spontaneous petechiae and ecchymoses, which result from a breakdown of the anatomic
- 16. Gastrointestinal and genitourinary bleeding may occur spontaneously with abnormalities of platelets and/or coagulation factors. Deep hematomas,
- 17. LABORATORY EVALUATION OF HEMOSTATIC DISORDERS Understanding of the physiology of primary and secondary hemostasis is important
- 18. The platelet count is performed to detect thrombocytopenia, which is defined as a platelet count of
- 19. The bleeding time is defined as the time between the infliction of a small standard cut
- 20. The various methods for performing the bleeding time are basically modifications of two techniques: the bleeding
- 21. The prothrombin time (PT) The prothrombin time may be prolonged because of a deficiency of a
- 22. The aPTT (activated partial thromboplastin time) In the old “cascade” theory of coagulation, the aPTT involves
- 23. The thrombin time (TT) as part of the screening procedures. The thrombin time will be prolonged
- 24. Interpretation of the Screening Tests of Hemostasis Discrimination of the majority of the inherited and acquired
- 25. A prolonged PT and a normal aPTT and TT may indicate a factor VII deficiency. Inherited
- 26. Most congenital deficiencies are single, whereas acquired abnormalities caused by vitamin K deficiency, liver disease, disseminated
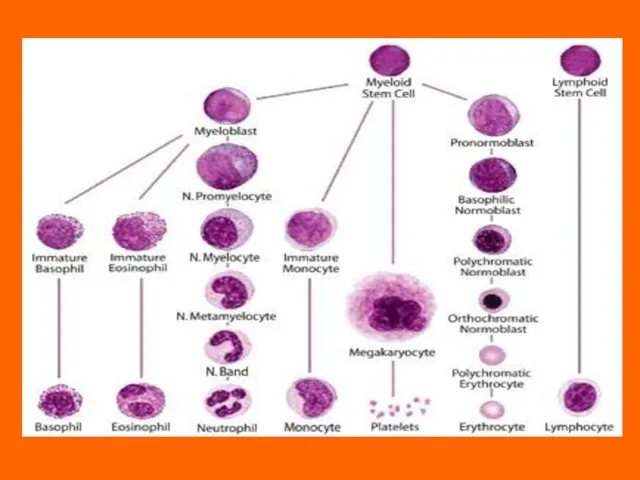
- 27. PLATELET DISORDERS Though platelets are classified as cells, they are actually cytoplasmatic fragments derived from megakaryocytes
- 28. Thrombocytopenia thrombocytopenia occurs when the platelet amount drops below 150,000/μL. The bleeding usually occurs when the
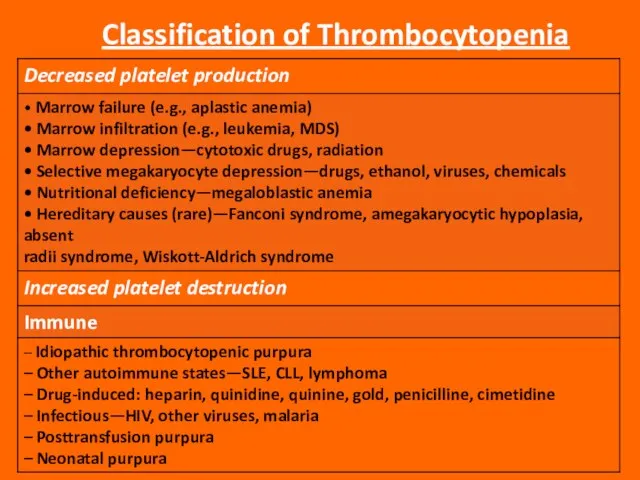
- 29. Classification of Thrombocytopenia
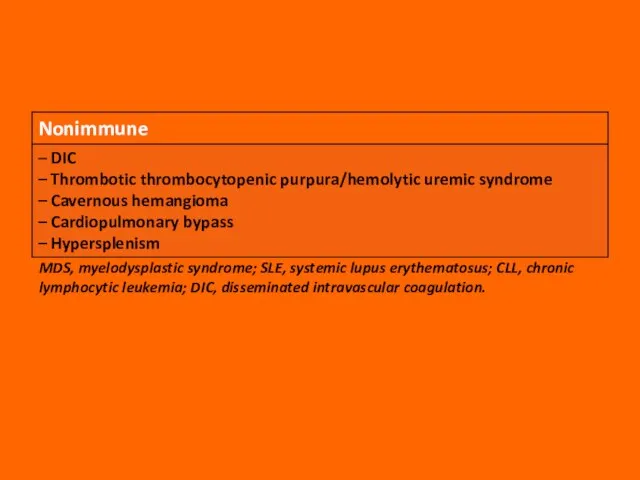
- 30. MDS, myelodysplastic syndrome; SLE, systemic lupus erythematosus; CLL, chronic lymphocytic leukemia; DIC, disseminated intravascular coagulation.
- 31. Thrombocytopenia Due to Decreased Platelet Production Thrombocytopenia due to decreased platelet production means that the bone
- 33. Thrombocytopenia Due to Increased Platelet Destruction Isolated thrombocytopenia is caused by increased platelet destruction. In these
- 34. Immune Thrombocytopenia Immune thrombocytopenia is an increase of platelet destruction caused by immunological mechanisms. The sensitization
- 35. Idiopathic Thrombocytopenic Purpura Acute ITP in children is equally common in boys and girls, has its
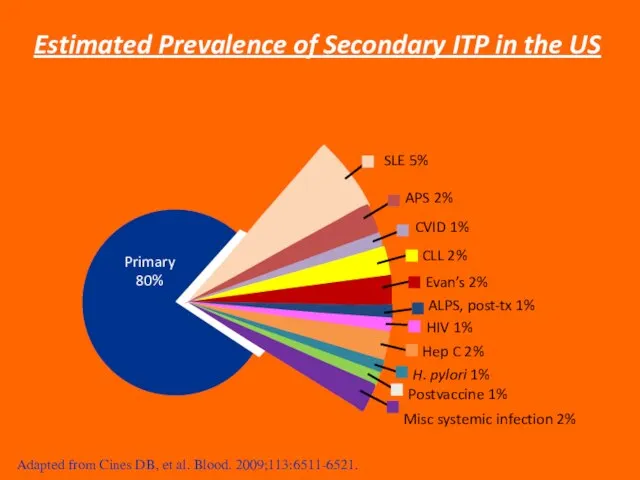
- 36. SLE 5% APS 2% CVID 1% CLL 2% Evan’s 2% ALPS, post-tx 1% HIV 1% Hep
- 37. Causes The exact causes of ITP are yet unknown, but there is currently research going on
- 38. Theories Three most common theories for ITP are: The Microbial Trigger Theory The Molecular Mimicry Theory
- 39. The Microbial Trigger Theory Related to the destruction of platelets to a chemical called interleuken 12
- 40. The Molecular Mimicry Theory This theory says that someone can develop ITP when the bodies T-helper
- 41. Free Radical Damage Theory DNA is damaged by “free radicals”. Free radicals are compounds that build
- 42. Pathophysiology ITP is caused by an autoantibody - in generally IgG - that binds to specific
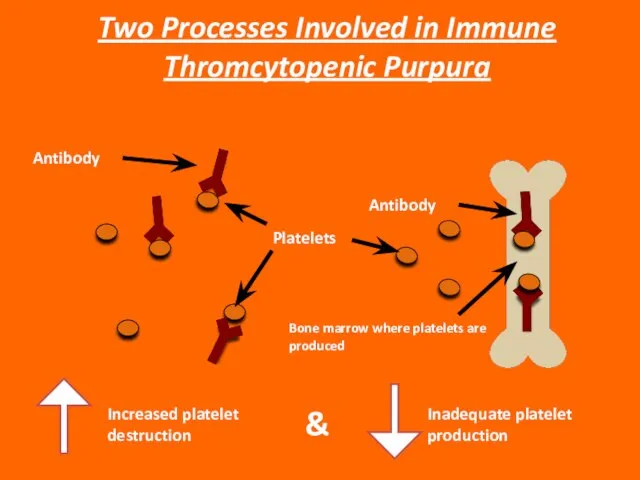
- 43. Increased platelet destruction & Inadequate platelet production Two Processes Involved in Immune Thromcytopenic Purpura Platelets Antibody
- 44. Classification of ITP Primary ITP: Idiopathic - etiology is unknown; No clinically evident secondary form. Secondary
- 45. Classification of ITP Secondary ITP Antiphospholipid syndrome; Autoimmune thrombocytopenia (e.g., Evans syndrome); Common variable immune deficiency;
- 46. Newly diagnosed (acute) ITP: Less than 6 months; Chronic ITP: More than 6-12 months; Refractory ITP:
- 47. Symptoms of ITP Excessive bleeding after minor injuries; Spontaneous bleeding from the mouth and nose; Unexplainable
- 48. Depression and ITP ITP is accompanied by short term or more permanent depression. This is because
- 49. Diagnosis of ITP Platelet count: Less than 100 x 109/L (rather than 150 x 109/L) Medical
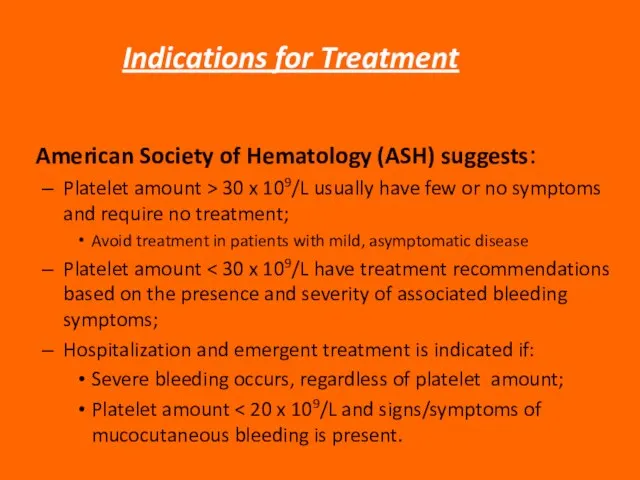
- 50. Indications for Treatment American Society of Hematology (ASH) suggests: Platelet amount > 30 x 109/L usually
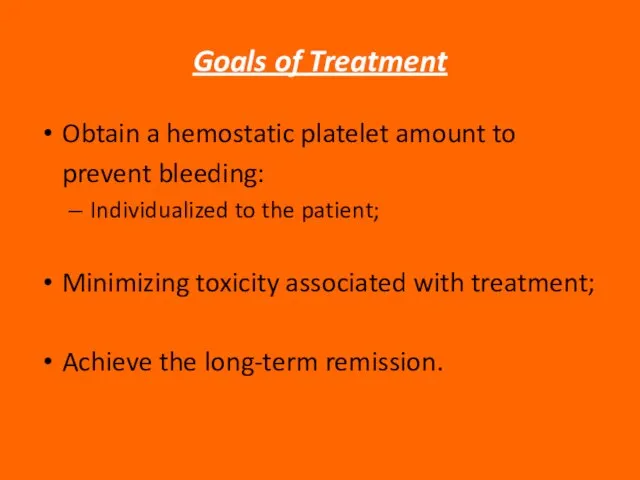
- 51. Goals of Treatment Obtain a hemostatic platelet amount to prevent bleeding: Individualized to the patient; Minimizing
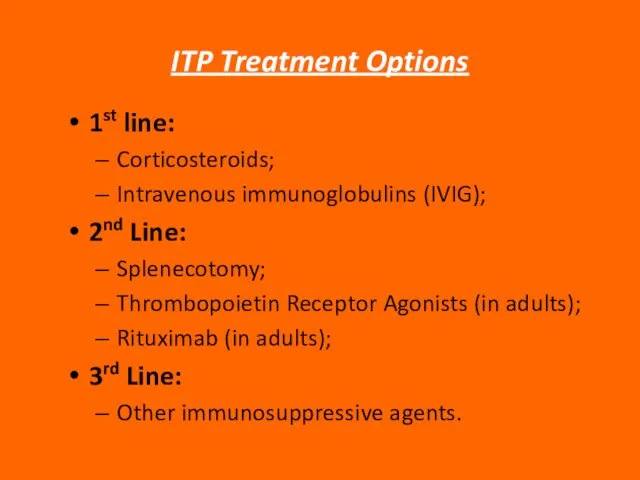
- 52. ITP Treatment Options 1st line: Corticosteroids; Intravenous immunoglobulins (IVIG); 2nd Line: Splenecotomy; Thrombopoietin Receptor Agonists (in
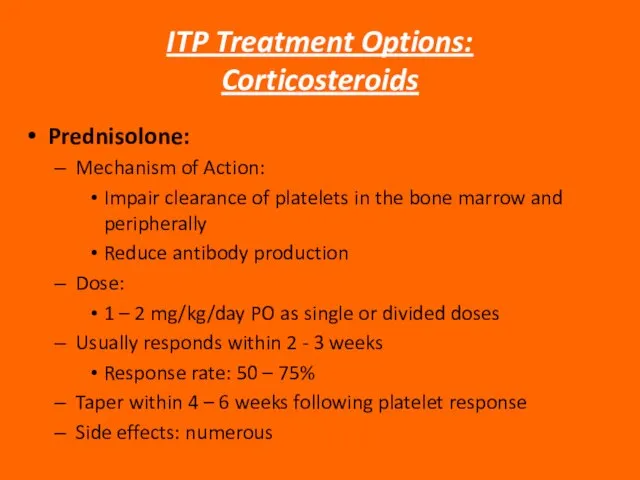
- 53. ITP Treatment Options: Corticosteroids Prednisolone: Mechanism of Action: Impair clearance of platelets in the bone marrow
- 54. ITP Treatment Options: IVIG IVIG: Mechanism of action: Undefined and potentially multifactorial Dose: Variable regimen Dose:
- 55. ITP Treatment Options: Splenectomy Splenectomy: Mechanism of action: Removes a primary site of platelet destruction and
- 56. EMERGENCY TREATMENT OF ITP Platelet transfusion + high dose steroids Platelet transfusion + continuous IVIG Antifibrinolytics
- 57. Neonatal Purpura Neonatal thrombocytopenia may develop due to isoimmunization of the mother against fetal platelets with
- 58. INHERITED DISORDERS OF COAGULATION There is a large number of inherited disorders of coagulation; however, only
- 59. von Willebrand’s Disease (vWD) von Willebrand disease is the most common inherited disorder of primary hemostasis.
- 60. Three main subtypes of vWD have been defined: Type 1: the most common (≥70% of cases
- 61. Type 2: In Type 2 vWD, there is a qualitative defect in vWF. Several different subtypes
- 62. Type 3: In Type 3 vWD, there is a total or near-total absence of vWF in
- 63. Clinical Manifestations of von Willebrand’s Disease Most cases of vWD present with the typical picture of
- 64. The laboratory manifestations of vWD can also be highly variable; sometimes laboratory tests must be repeated
- 65. Laboratory Diagnosis of von Willebrand’s Disease The most important diagnostic tests for vWD are the bleeding
- 66. In vWD Type 1, the BT will usually be prolonged. The PTT may also be slightly
- 67. Type 2A is diagnosed by demonstrating an absence of the high-molecular-weight multimers by agarose gel electrophoresis.
- 68. Diagnosis of Type 2M requires sophisticated techniques, which are not widely available; therefore, specimens must usually
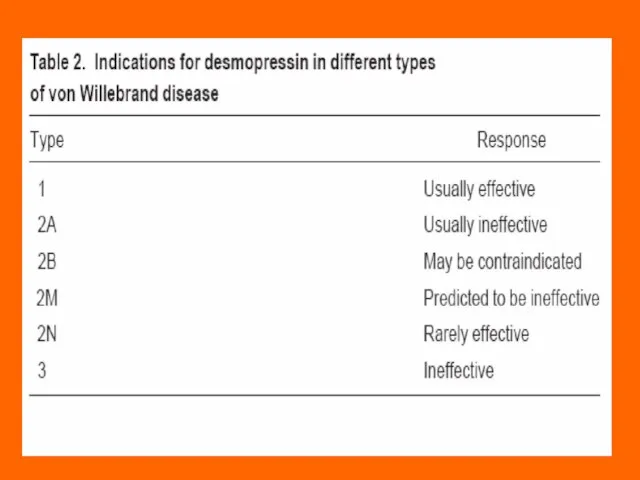
- 69. Treatment of von Willebrand’s Disease Most cases of vWD Type 1 can be very successfully treated
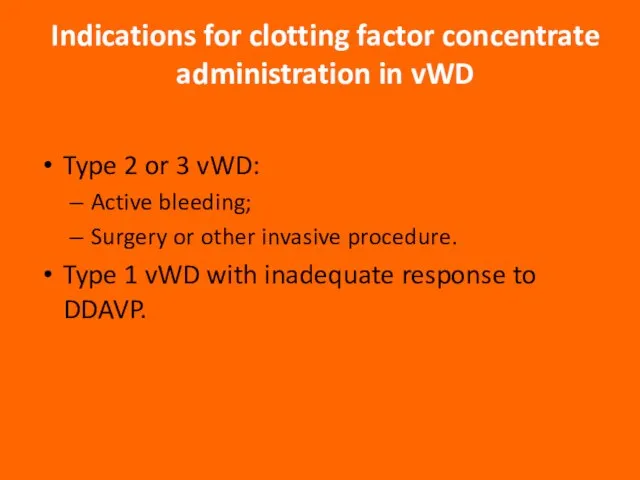
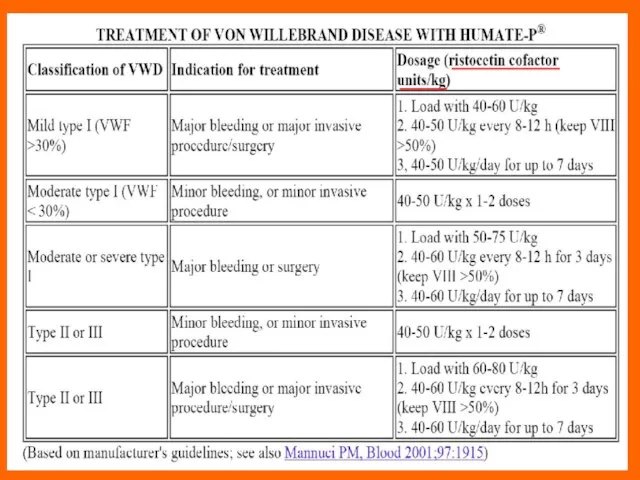
- 71. Indications for clotting factor concentrate administration in vWD Type 2 or 3 vWD: Active bleeding; Surgery
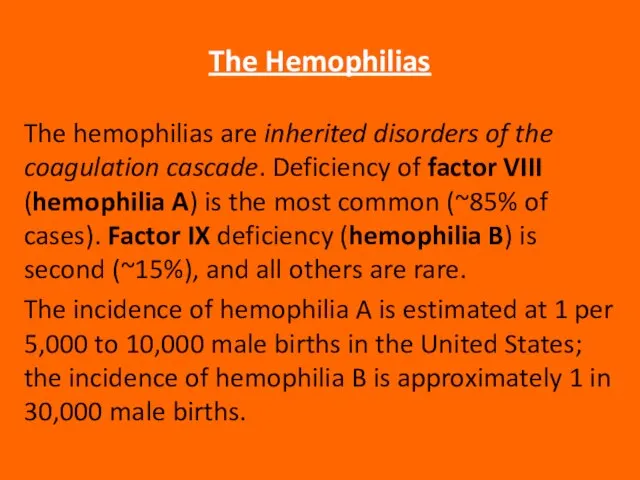
- 73. The Hemophilias The hemophilias are inherited disorders of the coagulation cascade. Deficiency of factor VIII (hemophilia
- 74. Hemophilia A and B are both inherited as X-linked recessive: women are carriers, men develop the
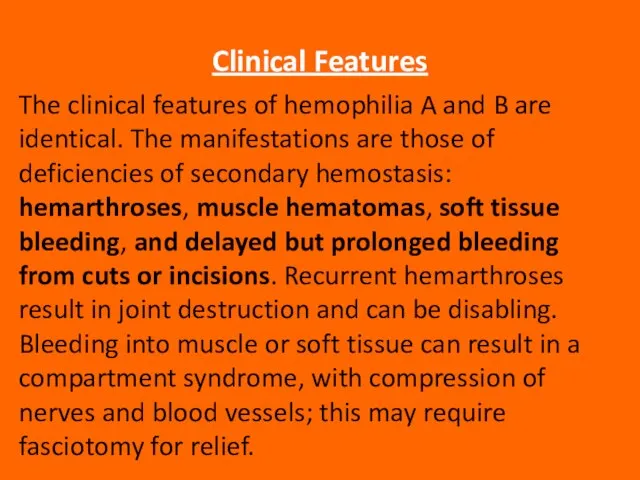
- 75. Clinical Features The clinical features of hemophilia A and B are identical. The manifestations are those
- 76. Muscle hematoma (pseudotumor) Hemarthrosis (joint bleeding)
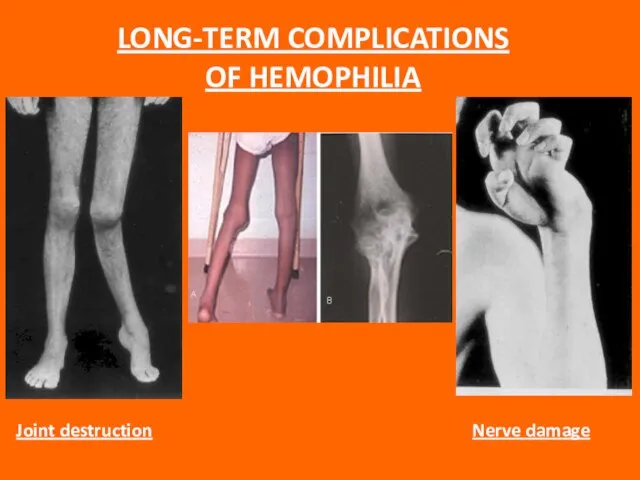
- 77. LONG-TERM COMPLICATIONS OF HEMOPHILIA
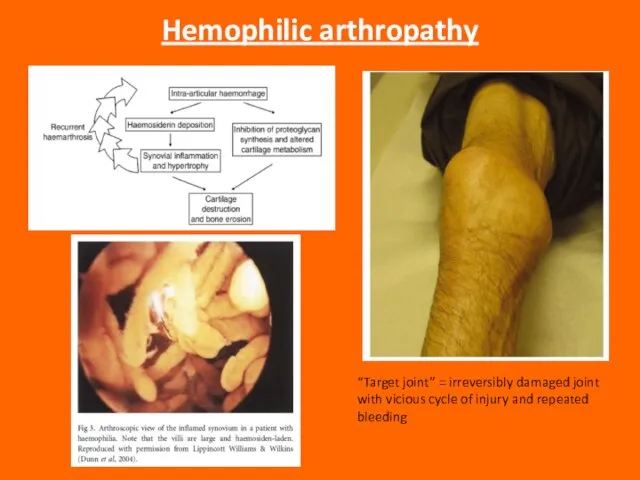
- 78. Hemophilic arthropathy “Target joint” = irreversibly damaged joint with vicious cycle of injury and repeated bleeding
- 79. Intracranial bleeding is anespecially serious complication, and even minor head trauma in a severe hemophiliac should
- 80. Children with severe hemophilia usually begin to have problems at about 9 to 12 months of
- 81. Most patients will have a family history of pathologic bleeding on the maternal side, including maternal
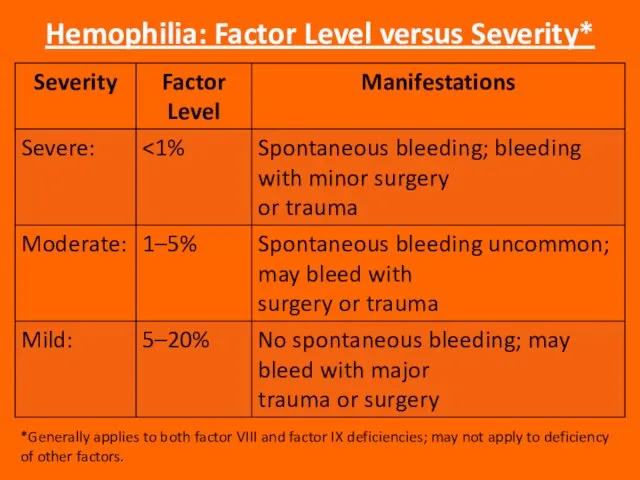
- 82. Hemophilia: Factor Level versus Severity* *Generally applies to both factor VIII and factor IX deficiencies; may
- 83. Laboratory Diagnosis The PTT is prolonged; the PT is normal. Mixing studies show correction of the
- 84. Treatment Treatment depends on which factor is deficient, the severity of the deficiency, and the nature
- 85. Always be sure to determine which factor the patient is deficient in before you start replacement
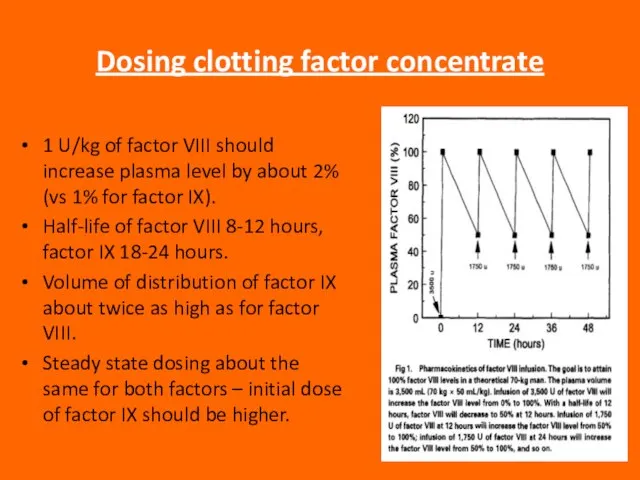
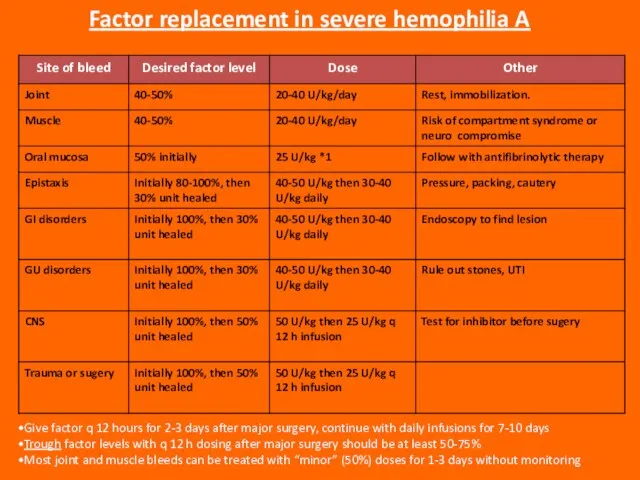
- 86. Dosing clotting factor concentrate 1 U/kg of factor VIII should increase plasma level by about 2%
- 87. Give factor q 12 hours for 2-3 days after major surgery, continue with daily infusions for
- 88. Liver disease in hemophilia Hepatitis C is still a problem, though incidence is falling with safer
- 89. ACQUIRED FACTOR VIII DEFICIENCY Due to antibody to factor VIII (most common autoimmune factor deficiency) Most
- 91. Скачать презентацию

 Техника мраморирования в дизайне
Техника мраморирования в дизайне Индийская культура
Индийская культура Цветок - генеративный орган
Цветок - генеративный орган Экономическая
Экономическая Городской пейзаж. Картины художников
Городской пейзаж. Картины художников Управленческие циклы
Управленческие циклы Роль лидера в совершенствовании педагогического корпуса
Роль лидера в совершенствовании педагогического корпуса Методические рекомендации по подготовке к выполнению части "С" ЕГЭ по русскому языку
Методические рекомендации по подготовке к выполнению части "С" ЕГЭ по русскому языку Александр Иванович Куприн
Александр Иванович Куприн Экстрасенсорное общение
Экстрасенсорное общение Использование проектной методики на уроках английского языка.
Использование проектной методики на уроках английского языка. Животноводство России
Животноводство России «Они должны жить»
«Они должны жить» Мудрая княгиня Ольга
Мудрая княгиня Ольга Ориентирование
Ориентирование Человек и его здоровье 3 класс
Человек и его здоровье 3 класс Взаимодействие ТОС и СМИ
Взаимодействие ТОС и СМИ Иван-царевич
Иван-царевич Композиция фигуры человека
Композиция фигуры человека Профилактика делинквентного поведения в школьной среде
Профилактика делинквентного поведения в школьной среде Барто «В театре»
Барто «В театре» Индустрия фильмов
Индустрия фильмов Игра по финансовой грамотности Копейка к копейке – проживет семейка
Игра по финансовой грамотности Копейка к копейке – проживет семейка Загадки Джоконды
Загадки Джоконды Роль социально-бытовой ориентировки в адекватной интеграции обучающихся, воспитанников школы-интерната в системе современных
Роль социально-бытовой ориентировки в адекватной интеграции обучающихся, воспитанников школы-интерната в системе современных Intelli Corder
Intelli Corder ОБЩАЯ ТЕОРИЯ ДИНАМИЧЕСКИХ СИСТЕМ
ОБЩАЯ ТЕОРИЯ ДИНАМИЧЕСКИХ СИСТЕМ Подарки, которые я бы хотела получить на день рождения
Подарки, которые я бы хотела получить на день рождения