Слайд 2Definition
DDCT (collagen diseases)- are characterized by systemic inflammation of connective tissue
and its appendages. This group includes four major collagen diseases: systemic lupus erythematosus, systemic scleroderma, polyarteritis (periarteritis) nodosa, dermatomyositis.
Слайд 3Common features of diseases:
1. common pathogenesis, which is manifested by disordered
immune homeostasis and hyperplasia of immunocompetent organs with signs of dysproteinosis. The autoimmune processes play the leading role. Own cells and tissues are assessed by the body as foreign and autoantibodies are produced
Слайд 42. similarity of morphological changes: fibrinoid changes in connective tissue, vasculitis, lymphoid
and plasma cell infiltrates
3. undulant and chronic course
4. exacerbations due to non-specific factors
Слайд 55. involvement of many systems: joints, skin, heart, kidneys, serous membranes
6.
corticosteroids are effective; other anti-inflammatory and immunosuppressive preparations are less efficacious.
Слайд 6Risk or predisposing factors
Heredity or genetic factors
Immunological factors
Sex hormone status
Environment triggers: ultraviolet
light; a viral agents; drags ( hydralazine, methildopa, procaiamide, D-penicillamine)
Слайд 7Pathogenesis
In the presence of hereditary predisposition the virus upset the immune
response which causes hyper-reactivity of the humoral immunity. Antibodies to various tissues, cells, proteins are produced uncontrolled in patient’s body.
Слайд 8 The next stage is formation of immune complexes and their deposition
in various organs. Then, the processes connected with elimination of fixed immune complexes occur, as a result of which lysosome enzymes are released, organs an tissues are affected, and immune inflammation develops.
Слайд 9 During inflammation and distruction of connective tissue, new antigents are released,
in response to which antibodies and new immune complexes are formed.
A vicious circle is closed and the disease becomes chronic.
Слайд 10Systemic lupus erythematosus (SLE)
SLE is an inflammatory, multisystem disorder with arthralgia
and rashes as the most common clinical features, and cerebral and renal diseases as the most serious problems.
Слайд 11General features
Fever is common in exacerbations occurring in up to 50%
of cases. Patients complain of marked malaise and tiredness.
Слайд 12The joints (90%)
Patients have symptoms that sound like RA with
small joints being involved in a symmetrical fashion. Joints are painful, sometimes there is slight soft-tissue swelling surrounding the joint. Deformity due to joint capsule and tendon contraction, bony erosions and aseptic necrosis - are rare.
Myalgia is present in up to 50% of patients, but a true myositis in< 5%.
Слайд 13The skin (75% of cases)
Erythema in "butterfly" distribution on the cheeks of
the face
Vasculitic lesion of the fingertips and around nail-folds, purpura, urticaria
Photosensitivity
Livedo reticularis, palmar and plantar rashes pigmentation
Alopecia
Слайд 14The lungs (50%)
Reccurrent pleurisy and pleural effusions (exudates) are bilaterial.
Pneumonitis
Atelectasis
Restrictive
lung defect develops with loss of lung volumes.
Pulmonary fibrosis
Слайд 15Heart (25%)
Pericarditis, with small pericardial effusions
A mild myocarditis giving rise to
arrhythmias.
Aortic valve lesions
Cardiomyopathy
Non-infective endocarditis involving the mitral valve (Libman-Sacks syndrome)
Vasculitis, arterial and venous thromboses
Слайд 16The kidneys (40%)
Most types of glomerulonephritis occur: mesangial, focal, diffuse and membranous.
Hypertension
Nephrotic syndrome
Renal failure.
Слайд 17The nervous system (60%)
There may be a mild depression
Psychiatric disturbunces
Epilepsy
Cerebellar ataxia
Aseptic
meningitis
Cranial nerve lesions
Cerebrovascular accidents
Polyneuropathy
Слайд 18The eyes
Retinal vasculitis can cause infarcts, hard exudates and haemorrhages.
Episcleritis,
Conjunctivitis
Optic

neuritis,blindness is uncommon.
Secondary Sjogren's syndrome (15% of cases).
Слайд 19The gastrointestinal system
Mesenteric vasculitis can produce inflammatory lesions involving the small bowel
(infarction or perforation)
Liver involvement is unusual
Pancreatitis is uncommon
Слайд 20LUPUS variants
Chronic discoid lupus is a benign variant. The rash is characteristic
and appears on the face as well-defined erythematous plaques that progress to scarring and pigmentation.
Subacute cutaneous lupus erythematosus is a rare variant
Слайд 21Drug-induced SLE
Drug-induced SLE is characterized by arthralgia and mild systemic features, rashes
and pericarditis, but seldom renal or cerebral disease. It usually disappears when the drug is stopped. Hydralazine, procianamide are the most likely causes.
Слайд 22Findings of direct diagnostic importance:
LE-cells are mature neutrophils that have phagocytized nuclear
protein of cells destroyed by the antinuclear factor (AF)
AF a complex of antinuclear antibodies circulating in the blood in high titres ≥1: 32
Antibodies to native (whole) DNA
The rosette phenomenon: free-lying lyised nuclei in tissues (bodies of acute phase).
Слайд 23Non-specific sings of acute phase:
Dysproteinemia with high alpha2 and gamma - globulin
content
Appearance of C-reactive protein
High fibrinogen content
Accelerated ESR
The rheumatoid factor (antibody to the Fc fragment of class G immune globulin)
Слайд 24Peripheral blood and changes in urine
Leucopenia with a shift in the leucocytic
formula
Lymphopenia
Moderate hypochromic or haemolitic anaemia
Thrombocytopenia combined with Werlhof syndrome
Proteinuria
Mild leucocyturia due to urinary tract infection.
Erythrocyturia
Слайд 25X-ray studies, ECG
X – ray studies reveal: changes in the joints with
articular syndrome; epiphysel osteoporosis; changes in the lungs associated with pneumonitis or chronic interstitial changes; changes in the heart.
ECG reveal non-speciphic changes (the T wave and S-T segment), which are similar to those in myocarditis and pericarditis.
Слайд 26Management
Complex pathogenetic therapy is indicated:
(1) suppression of immune inflammation and immune complex
pathology
(2) action on separate pronounced syndrom.
(3) prevention of side effects of immunosup- pressive therapy
(4) treatment of complications of therapy.
Слайд 27Duration of treatment
Duration of treatment, particular preparati- ons and their doses (and
also maintenance doses) are selected depending on:
(1) activity of the disease;
(2) acuity of the process;
(3) involvement of the internal organs;
(4) tolerance of corticosteroids or cytostatics and the presence (or absence) of complications of the immunosuppressor therapy
Слайд 28In subacute and chronic course:
non-steroid anti-inflammatory preparati- ons: salicylates – aspirin 1-
4 times a day;
derivatives of pyrozoloni (amidopyrini 0,25 4 times a day, analgini 0,5 4 times a day);
derivatives of indoli (indomethacin 25 – 60 mg 3 times a day);
brufen 2 dr 3 times a day.
Слайд 29In chronic course:
In chronic course with predominant involment of the skin:
delagil,
chloroquine 0,25 – 0,5g 3 times a day for 2 weeks, then 0,25 1 times a day for many months.
Слайд 30In acute and subacute course or if the sings of generalization
should
be given prednisolone: in acute course and third degree 40-60 mg; in the activity of the second degree 30-40 mg; and in first degree 15-20 mg. Maintenance doses are 5 or 10 mg daily.
Слайд 31Cortiteroids
Cortiteroids are the main remedy against SLE. They produce a high therapeutic
effect and their administration during many years produces comparatively mild side effects. Duration of the corticosteroid therapy for suppression of the process activity depends on the dynamics of the clinico-laboratory signs of activity.
Слайд 32In nephrotic syndrome and in the presence of cerebral symptoms
the preparation is
given until a clinical improvement is attained (not less than for 3 months, or for 6 months and longer, whenever necessary).
Слайд 33As soon as the desired effect is attained, the prednisolone dose is
reduced very slowly;
first by 5 mg weekly for 3-4 weeks,
then by 2.5 mg for 1-3 months, with observation of the patient's condition and analysis.
Maintenance dose of prednisolone (5-10 g/day) is given for years.
Слайд 34Side effects are corrected by:
(1) potassium preparations and anabolics ;
(2) diuretics and
hypotensives
(3) antacids, antiulcer therapy.
(4) antibiotics (in secondary infections);
(5) antituberculosis preparations
(6) insulin preparations and dietary restrictions for diabetes mellitus;
(7) antifungal preparations for candidomycosis;
Слайд 35Administration of superhigh doses of prednisolone (1000 mg for 3 days, i/v).
(1)
abrupt intensification of the process activity despite adequate therapy;
(2) in cases where the patient develops resistance to the doses.
It is believed that such “pulse” therapy stops formation of immune complexes due to inhibited synthesis of antibodies to DNA.
Слайд 36This becomes necessary in following conditions:
(1) abrupt intensification of the activity despite
therapy;
(2) in cases where the patient develops resistance.
Pulse therapy stops formation of immune complexes due to inhibited synthesis of antibodies to DNA.
The pulse therapy is most effective in young patients with a short history of SLE.
Слайд 37Corticosteroid therapy is not always effective.
It is explained by:
(1) the necessity to
decrease the dose, if complications develop (despite efficacy of the therapy in a given patient);
(2) intolerance of corticosteroids;
(3) resistance to corticosteroid therapy (usually developing very soon).
Слайд 38Cytostatics
Cyclophosphane or azathioprine, 1-3 mg/ kg, in combination with 10-30 mg
of prednisolone, for 4-6 months. The maintenance dose is continued for 1/2-3 years. Corticosteroids can later be given because resistance to them usually disappears with time.
Слайд 39Criteria of cytostatic efficacy:
(1) lessening or disappearance of clinical signs;
(2) disappearance of
resistance to steroids;
(3) stable reduction of process activity and absence of relapses;
(4) prevention of progress of lupus nephritis.
Слайд 40The complications of cytostatic therapy
(1) leucopenia;
(2) anaemia and thrombocytopenia;
(3) dyspepsia;
(4) infective complications
Слайд 41The complications of cytostatic therapy
If leucocyte count drops below 2000/mm3, the
dose should be decreased to 1 mg/kg; If leucopenia intensifies, the administration of the cytostatic should be suspended and the prednisolone dose increased by 50%.
Слайд 42Prognosis.
Effective methods of treatment have been developed during recent years and
the prognosis has improved significantly: remission is attained in about 90% of patients. The prognosis remains bad in 10 %, especially if the kidneys are involved.

 Правила перевозок железнодорожным транспортом подкарантинных грузов
Правила перевозок железнодорожным транспортом подкарантинных грузов Компетентностный подход в обучении
Компетентностный подход в обучении Равновесие реакции
Равновесие реакции Одна из достопримечательностей нашего города
Одна из достопримечательностей нашего города Презентация на тему Климат России Климатообразующие факторы
Презентация на тему Климат России Климатообразующие факторы Ячменев Александр Александрович
Ячменев Александр Александрович Крестовые походы
Крестовые походы Полиуретаны, силиконы
Полиуретаны, силиконы Система подготовки к ГИА по математике в 9 кл.
Система подготовки к ГИА по математике в 9 кл. Создание системы общественного экологического мониторингав Московской области
Создание системы общественного экологического мониторингав Московской области Arete outdoor centre
Arete outdoor centre Либеральные работы 60-70 годов 19 века
Либеральные работы 60-70 годов 19 века  На арене цирка
На арене цирка Средник для лучковой пилы
Средник для лучковой пилы Личная гигиена. Гигиена кожи, одежды.
Личная гигиена. Гигиена кожи, одежды. На сколько больше? На сколько меньше?
На сколько больше? На сколько меньше? Формирование ключевых компетентностей у учащихся в процессе преподавания математики с использованием И К Т
Формирование ключевых компетентностей у учащихся в процессе преподавания математики с использованием И К Т Холодные супы
Холодные супы Химический состав и свойства крови
Химический состав и свойства крови  Нарезание резьб плашками
Нарезание резьб плашками What king of sport is it?
What king of sport is it?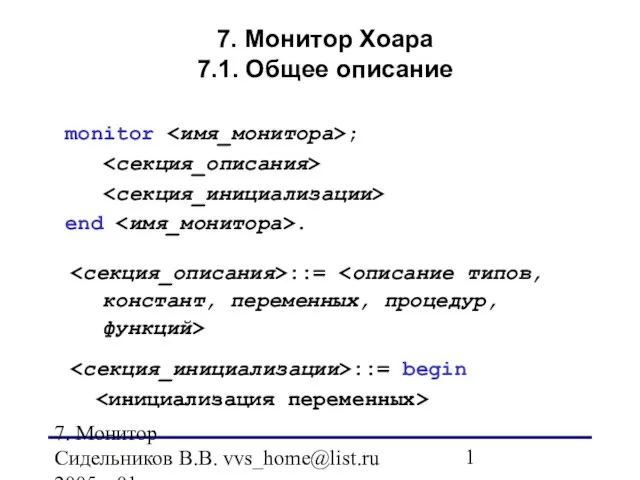 7. Монитор Хоара7.1. Общее описание
7. Монитор Хоара7.1. Общее описание Я-концепция как основа жизненного стиля
Я-концепция как основа жизненного стиля Лесные опасности
Лесные опасности Потребление воды и минеральных ресурсов
Потребление воды и минеральных ресурсов Чертежи деталей из сортового проката
Чертежи деталей из сортового проката Этические и правовые нормы информационной деятельности
Этические и правовые нормы информационной деятельности Универсальный гибридный вездеход Пионер-III для малого бизнеса (модель для трубопроводов)
Универсальный гибридный вездеход Пионер-III для малого бизнеса (модель для трубопроводов)