Содержание
- 2. Disorders of the Parathyroid Glands Maintenance of calcium, phosphate and magnesium homeostasis is under the influence
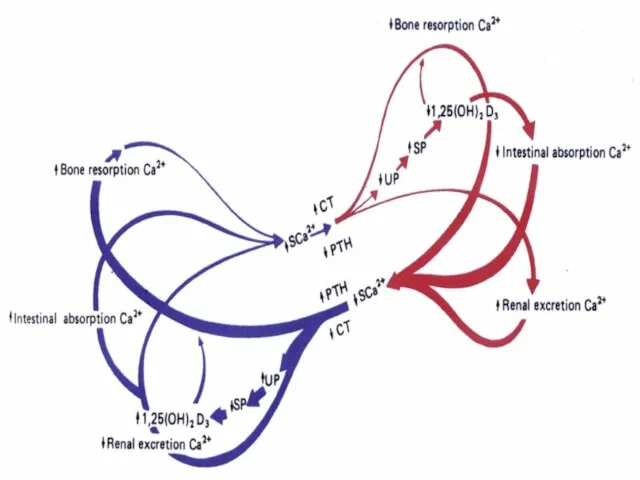
- 3. Disorders of the Parathyroid Glands These hormones regulate the flow of minerals in and out of
- 4. Disorders of the Parathyroid Glands The PTH acts directly on the bones and kidneys and indirectly
- 5. Disorders of the Parathyroid Glands Calcitonin is released by the “C” cells (parafollicular cells in the
- 6. Disorders of the Parathyroid Glands Calcitonin is therefore the physiological antagonist of PTH. The two hormones
- 8. Disorders of the Parathyroid Function Primary hyperparathyroidismis due to excessive production of PTH by one or
- 9. Disorders of the Parathyroid Function The cause of primary hyperparathyroidism is unknown. A genetic factor may
- 10. Disorders of the Parathyroid Function The incidence of the disease increases dramatically after the age of
- 11. Disorders of the Parathyroid Function The two major sites of potential complications are the bones and
- 12. Disorders of the Parathyroid Function In skeleton a condition called osteitis fibrosa cystica could occur with
- 13. Disorders of the Parathyroid Function Now a days almost 90% of diagnosed cases in the developed
- 14. Disorders of the Parathyroid Function Other symptoms include muscle weakness, easy fatigability, peptic ulcer disease, pancreatitis,
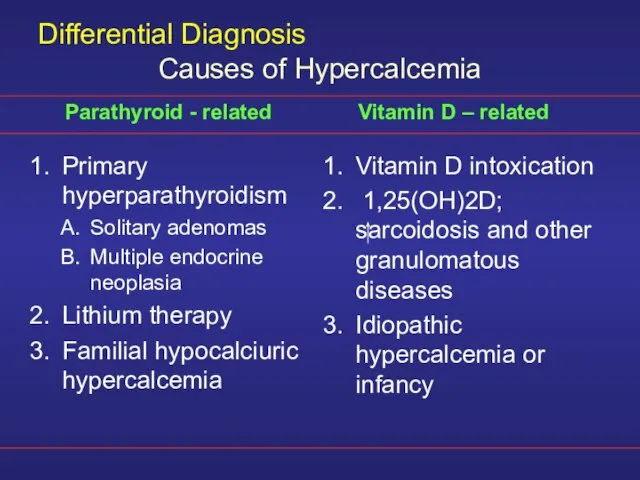
- 15. Differential Diagnosis Primary hyperparathyroidism Solitary adenomas Multiple endocrine neoplasia Lithium therapy Familial hypocalciuric hypercalcemia Vitamin D
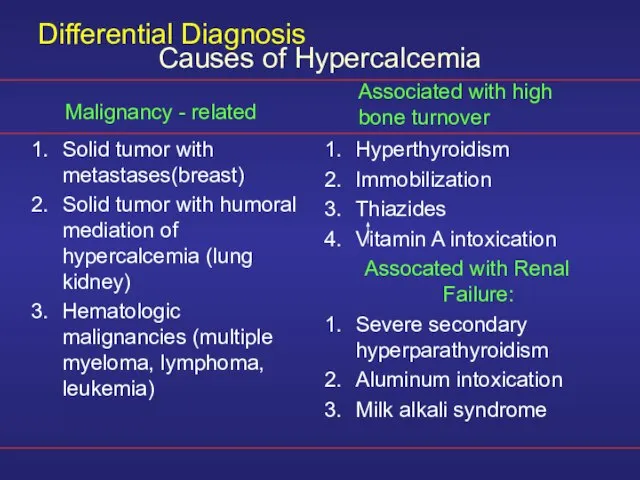
- 16. Differential Diagnosis Solid tumor with metastases(breast) Solid tumor with humoral mediation of hypercalcemia (lung kidney) Hematologic
- 17. Diagnosis The presence of established hypercalcaemia in more than one serum measurement accompanied by elevated immunoreactive
- 18. Diagnosis Serum phosphate is usually low but may be normal. Hypercalcaemia is common and blood alkaline
- 19. Other Diagnostic tests The heypercalcaemic of non-parathyroid origin e.g., vitamin D intoxication, sarcoidosis and lymphoproliferative syndromes
- 20. Other Diagnostic tests The response is unusual in hypercalcaemia secondary to primary hyperparathyroidism and ectopic PTH
- 21. Other Diagnostic tests Plain X-ray of hands can be diagnostic showing subperiosteal bone resorption usually on
- 22. Other Diagnostic tests Ultrasonography MRI CT Thallium 201 – Tehcnichum99m scan (subtraction study) Pre-operative localization of
- 23. Treatment A large proportion of patients have “biochemical” hyperparathyroidism but with prolonged follow up they progress
- 24. Medical Treatment of the hypercalcaemia In acute severe forms the main stay of therapy is adequate
- 25. Other agents Glucocostiroids In hypercalcaemia associated the hematological malignant neoplasms Mythramycin A toxic antibiotics which inhibit
- 26. Other agents Calcitonin Also inhibit osteoclast activity and prevent bone resorption Bisphosphonates They are given intravenously
- 27. Other agents Phosphate Oral phosphate can be used as an antihypercalcaemic agent and is commonly used
- 28. Surgery Surgical treatment should be considered in all cases with established diagnosis of primary hyperparthyroidism. During
- 29. Other Complications Deterioration of renal function Metabolic disturbance e.g. hypomagnesia, pancreatitis, gout or pseudogout
- 30. Secondary hyperparathyroidism An increase in PTH secretion which is adaptive and unrelated to intrinsic disease of
- 31. Major causes of chronic hypocalcemia other than hypoparathyroidism Dietary deficiency of vitamin D or calcium Decreased
- 32. Major causes of chronic hypocalcemia other than parathyroprival hypoparathyroidism States of tissue resistance to vitamin D
- 33. Hypoparathyroidism Deficient secretion of PTH which manifests itself biochemically by hypocalcemia, hyperphospatemia diminished or absent circulating
- 34. Hypoparathyroidism Surgical hypoparathyroidism – the commonest After anterior neck exploration for thyroidectomy, abnormal parathyroid gland removal,
- 35. Hypoparathyroidism Idiopathic hypoparathyroidism A form occuring at an early age (genetic origin) with autosomal recessive mode
- 36. Hypoparathyroidism Idiopathic hypoparathyroidism Circulating antibodies for the parathyroid glands and the adrenals are frequently present. Other
- 37. Hypoparathyroidism Idiopathic hypoparathyroidism The late onset form occurs sporadically without circulating grandular autoantibodies. Functional hypoparathyroidism In
- 38. Hypoparathyroidism Neuromuscular The rate of decrease in serum calcium is the major determinant for the development
- 39. Hypoparathyroidism Neuromuscular Parathesia Tetany Hyperventilation Adrenergic symptoms Convulsion (More common in young people and it can
- 40. Hypoparathyroidism Other clinical manifestation Posterio lenticular cataract Cardiac manifestation: Prolonged QT interval in the ECG Resistance
- 41. Hypoparathyroidism Other clinical manifestation Dental Manifestation Abnormal enamel formation with delayed or absent dental eruption and
- 42. Hypoparathyroidism In the absence of renal failure the presence of hypocalcaemia with hyperphosphataemia is virtually diagnostic
- 43. Hypoparathyroidism The mainstay of treatment is a combination of oral calcium with pharmacological doses of vitamin
- 44. Emergency Treatment for Hypocalcaemic Calcium should be given parenterally till adequate serum calcium level is obtained
- 45. Emergency Treatment for Hypocalcaemic In patients with hyperparathyroidism and severe bone disease who undergo successful parathyroidectomy
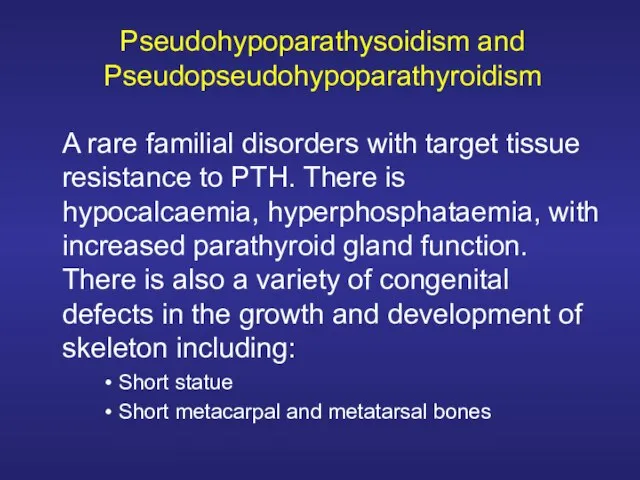
- 46. Pseudohypoparathysoidism and Pseudopseudohypoparathyroidism A rare familial disorders with target tissue resistance to PTH. There is hypocalcaemia,
- 48. Скачать презентацию
 ОБЛАКА (6 класс)
ОБЛАКА (6 класс) Язык программирования Pascal. Процедуры и функции
Язык программирования Pascal. Процедуры и функции Поговорим об этикете
Поговорим об этикете Всемирный Банк и МолодежьThe Young Professionals Program
Всемирный Банк и МолодежьThe Young Professionals Program Руководство Ernst&Young по составления бизнес-планов
Руководство Ernst&Young по составления бизнес-планов Формированиеруководящих органов Платформы и план работ на I квартал 2011 (представление проектарешения заседания)
Формированиеруководящих органов Платформы и план работ на I квартал 2011 (представление проектарешения заседания) Бакланова Людмила Николаевна, учитель географии высшей квалификационной категории МОУ Чайковская средняя общеобразовательная ш
Бакланова Людмила Николаевна, учитель географии высшей квалификационной категории МОУ Чайковская средняя общеобразовательная ш Русская культура. Предметы русского быта
Русская культура. Предметы русского быта Welcome to 2011:что ждет рекламодателей
Welcome to 2011:что ждет рекламодателей Наука как деятельность. Спорт как объект научного исследования
Наука как деятельность. Спорт как объект научного исследования Космос, земля, человек.
Космос, земля, человек. Плетение
Плетение Презентация на тему Русская культура
Презентация на тему Русская культура Антибактериальный гель для рук
Антибактериальный гель для рук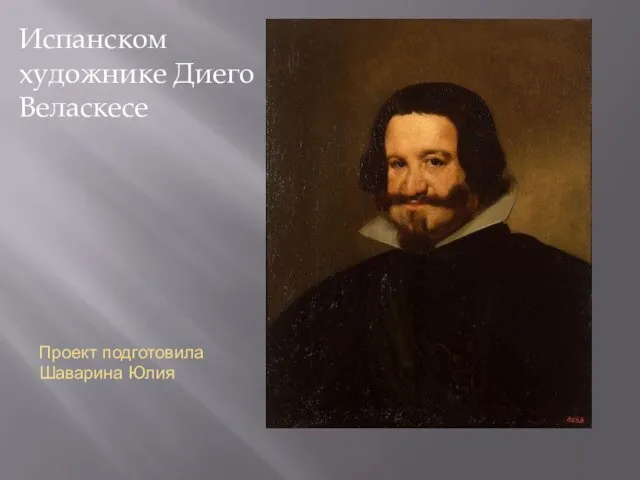 Испанском художнике Диего Веласкесе
Испанском художнике Диего Веласкесе Использование информационных средств обучения на уроках истории и обществознания
Использование информационных средств обучения на уроках истории и обществознания DIU - Активные виды деятельности
DIU - Активные виды деятельности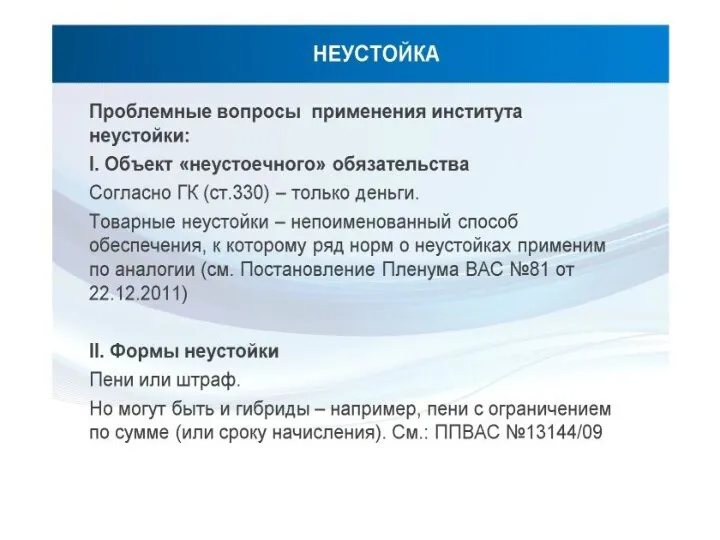 Неустойка. Формы неустойки
Неустойка. Формы неустойки Презентация на тему Нью-Йорк
Презентация на тему Нью-Йорк Презентация
Презентация Использование опорных схем на уроках русского языка- один из способов формирования информационных и коммуникативных компетентно
Использование опорных схем на уроках русского языка- один из способов формирования информационных и коммуникативных компетентно mdk_02
mdk_02 Идеальная бровь
Идеальная бровь Избирательная система РФ
Избирательная система РФ 2022.10.28_Презентация на Думу
2022.10.28_Презентация на Думу ЦУКУРОВ Олег Анатольевич Заместитель Генерального директора ОАО «Институт сварки России», член Технического комитета по станда
ЦУКУРОВ Олег Анатольевич Заместитель Генерального директора ОАО «Институт сварки России», член Технического комитета по станда Контрперенос и принципы работы бессознательного
Контрперенос и принципы работы бессознательного Рунические формулы на все случаи жизни
Рунические формулы на все случаи жизни