Слайд 2INFLAMMATORY BOWEL DISEASE
Refers to two chronic diseases of unknown etiology that cause
inflammation of the intestine with extra intestinal manifestations
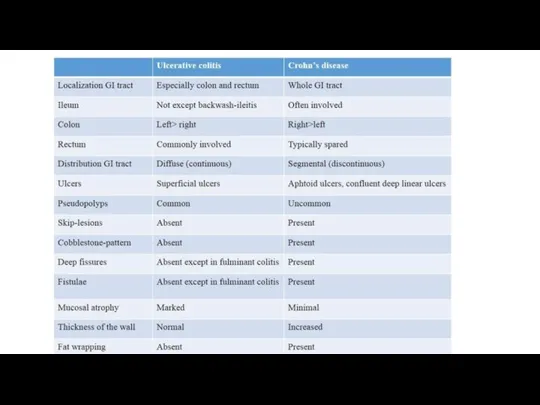
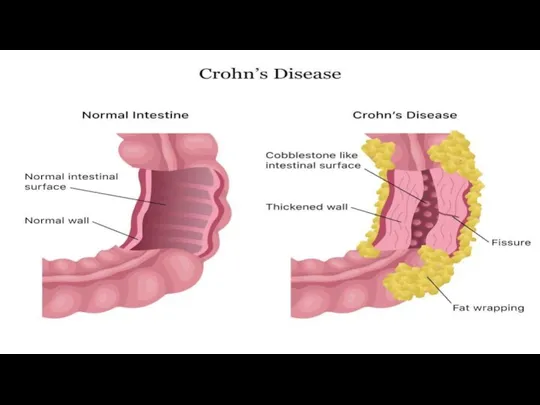
Ulcerative colitis and Crohn's disease
Although the diseases have some features in common, there are some important differences.
Слайд 3INTRODUCTION
Ulcerative colitis is an idiopathic form of acute and chronic ulcero-inflammatory
colitis affecting chiefly the mucosa and submucosa of the rectum and descending colon, though sometimes it may involve the entire length of the large bowel.
these disorders primarily affect the bowel but may have systemic involvement in the form of polyarthritis, uveitis, ankylosing spondylitis, skin lesions and hepatic involvement.
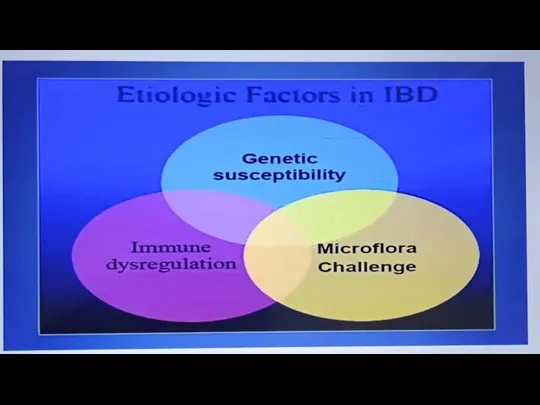
Слайд 5ETIOLOGY
1 Genetic factors. Genetic factors are implicated in the etiopathogenesis of
IBD is supported by the following evidences:
i) There is about 3 to 20 times higher incidence of occurrence of IBD in first degree relatives.
Ii) Overall, there is approximately 50% chance of development of IBD in
iii) Genome wide search has revealed that disease-predisposing loci are present in chromosomes 16q, 12p, 6p, 14q and 5q. Iv) HLA studies show that ulcerative colitis is more common in HLA-DRB1 alleles while Crohn’s disease is more common in HLA-DR7 and DQ4 alleles.
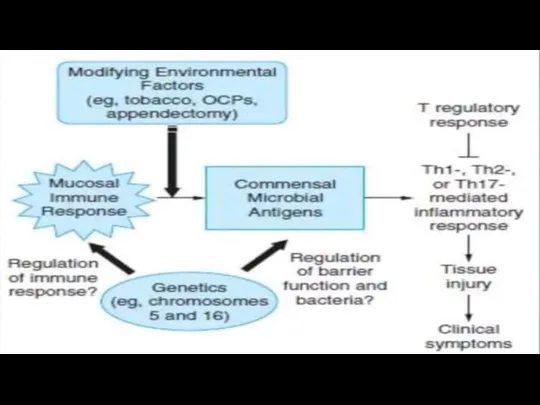
Слайд 62. Immunologic factors. Defective immunologic regulation in IBD has been shown to
play significant role in the pathogenesis of IBD:
i) Defective regulation of immune suppression. The mechanism responsible for this is by activation of CD4+ T cells secreting cytokines inhibitory to inflammation (IL-10, TGF-B) which suppress inflammation in the gut wall.
Ii) Transgenic mouse experimental model studies. Gene ‘knock out’ studies on colitis in mice have revealed that multiple immune abnormalities may be responsible for IBD as under:
Слайд 73. Exogenous factors. In addition to role of genetic factors and deranged
T-cell mediated immunity, a role for several exogenous and environmental factors has been assigned:
i) Microbial factors, ii) Psychosocial factors, iii) Smoking and iv) Oral contraceptives.
i) Microbial factors: At different times, role of a variety of microbes in initiation of inflammatory response by the body has been suspected. Accordingly, several microorganism species (bacteria, viruses, protozoa and fungi) have been suspect but without definite evidence: Mycobacterium paratuberculosis, Salmonella, Shigella, Helicobacter, Clostridia, bacteroides, Escherichia, Measles virus etc.
Слайд 8Ii) Psychosocial factors: It has been observed that individuals who are unduly
sensitive, dependent on others and unable to express themselves, or some major life events such as illness or death in the family, divorce, interpersonal conflicts etc, suffer from irritable colon or have exacerbation of symptoms.
iii) Smoking: Role of smoking in causation of Crohn's diseasehas been reported.
iv) Oral contraceptives: An increased risk to develop Crohn's disease with long-term use of oral contraceptives has been found in some studies but there is no such increased risk for ulcerative colitis.
Слайд 10RISE OF INCIDENCE IN IBD IN INDIA
Familial aggregation
Nicotine Consumption
Oral Contraceptives
• Dietary
Habits-Refined sugars, Fast food, cereals, bakers yeast etc
Physical inactivity Early weaningHygiene
• Infectious diseases- TB, MeaslesSaveㅁO
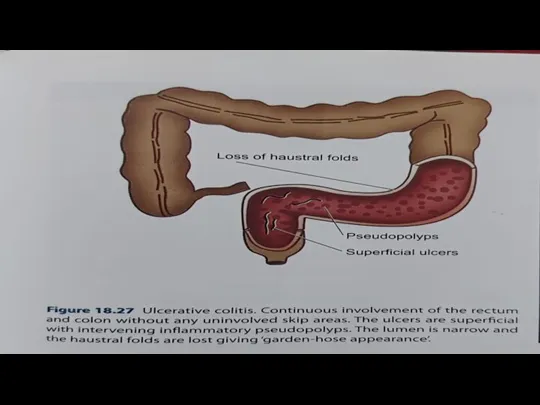
Слайд 11MORPHOLOGY
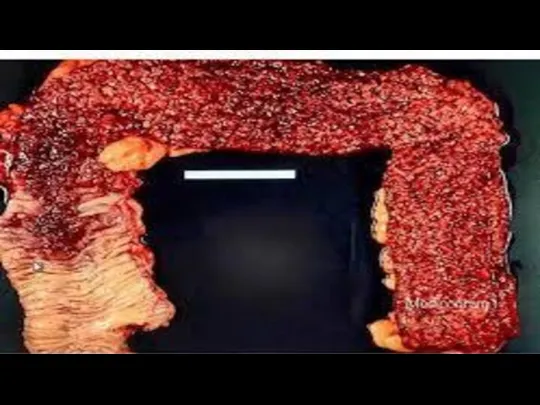
Mucosa shows linear and superficial ulcers, usually not penetrating the muscular
layer. The intervening intact mucosa may form inflammatory 'pseudopolyps. The muscle layer is thickened due to contraction, producing shortening and narrowing of the affected colon with loss of normal haustral folds giving 'garden-hose appearance'
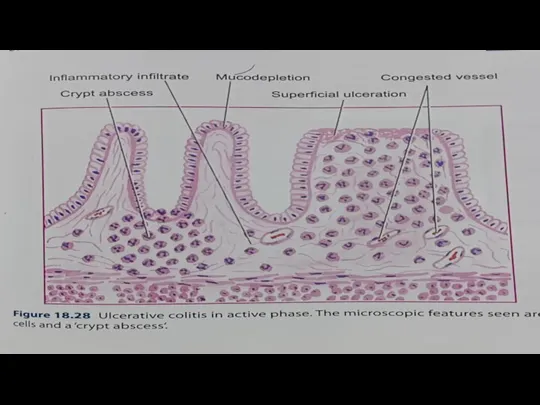
Слайд 14CHARACTERISTICS FORM OF CHRONIC COLITIS ACCORDING TO BIOPSY
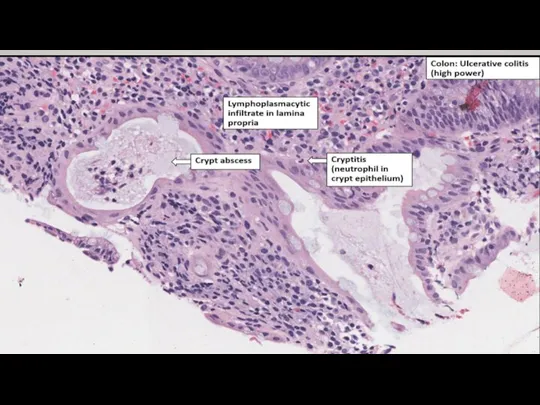
1Crypt distortion, cryptitis and
focal accumulations of neutrophils forming crypt abscesses.
2 Marked congestion, dilatation and haemorrhages frommucosal capillaries.
3 Superficial mucosal ulcerations, usually not penetrating Into the muscle coat, except in severe cases, and is accompanied by nonspecific inflammatory cell infiltrate of lymphocytes, plasma cells, neutrophils, some eosinophils and mast cells in the lamina propria.
Слайд 154 Goblet cells are markedly diminished in cases of activedisease.
5. Areas of
mucosal regeneration and mucodepletion of lining cells.6.
In long-standing cases, epithelial cytologic atypia ranging from mild to marked dysplasia and sometimes developing into carcinoma in situ and frank adeno carcinoma.
Слайд 18SYMPTOMS
Rectal bleeding and tenesmus are universallypresent.
Diarrhea and abdominal pain are more
frequent with proximal colon involvement.
Nausea and weight loss in severe cases.
Severe abdominal pain or fever suggestsfulminant colitis or toxic megacolon.
Слайд 19COMPLICATIONS
1. Toxic megacolon (Fulminant colitis) is the acute fulminating colitis in
which the affected colon is thin-walled and dilated and is prone to perforation and faecal peritonitis. There is deep penetration of the inflammatory cell infiltrate into muscle layer which is disrupted.The summariGISInflabowulceCrohIBD,granthe.
2. Perianal fistula formation may occur rarely.
3. Carcinoma may develop in long-standing cases of ulcerativecolitis of more than 10 years duration.
4. Stricture formation almost never occurs in ulcerative colitis.
 Трудоустройство и занятость населения в России
Трудоустройство и занятость населения в России Restoran_pitania_BIZNES (2)
Restoran_pitania_BIZNES (2) Электрический цех
Электрический цех Западноевропейская философия XIX-XX века
Западноевропейская философия XIX-XX века Государственной ДумеРоссийской федерации – 100 лет
Государственной ДумеРоссийской федерации – 100 лет Тема : « ПРОЦЕНТЫ»
Тема : « ПРОЦЕНТЫ» Мотивационная программа Dentsply для розницы на II полугодие 2017 года
Мотивационная программа Dentsply для розницы на II полугодие 2017 года Теория кодирования
Теория кодирования Е.Н.Ковтунд.ф.н., профессор, заместитель Председателя Совета по филологии УМО по классическому университетскому образованию (МГ
Е.Н.Ковтунд.ф.н., профессор, заместитель Председателя Совета по филологии УМО по классическому университетскому образованию (МГ Педагогическая концепция
Педагогическая концепция План урока
План урока Защита населения от аварийно - химически опасных веществ (АХОВ)
Защита населения от аварийно - химически опасных веществ (АХОВ) Стратегический маркетинг
Стратегический маркетинг Медицинская сестра
Медицинская сестра Коммуникативно-деятельностный подход к речевому развитию младших школьников
Коммуникативно-деятельностный подход к речевому развитию младших школьников Основы вакуумной техники. Экскурс в историю вакуумной техники
Основы вакуумной техники. Экскурс в историю вакуумной техники Общее знакомство с растениями. Мир растений
Общее знакомство с растениями. Мир растений Анализ представленных субъектами Российской Федерации отчетов о достижении показателей результативности реализации субсидий
Анализ представленных субъектами Российской Федерации отчетов о достижении показателей результативности реализации субсидий Психология в сфере экономики
Психология в сфере экономики 6
6 26 sierpnia Najświętszej Maryi Panny Częstochowskiej
26 sierpnia Najświętszej Maryi Panny Częstochowskiej Презентация на тему Урок математики 2 класс
Презентация на тему Урок математики 2 класс  Сравнительная оценка потребительских свойств средств по уходу за волосами отечественного и импортного производства
Сравнительная оценка потребительских свойств средств по уходу за волосами отечественного и импортного производства Істерді ведомстволыќ м±раѓатќа µткізуге дайындау
Істерді ведомстволыќ м±раѓатќа µткізуге дайындау Построение профессиональной карьеры
Построение профессиональной карьеры Изменения в нормативной правовой базе ЕГЭ в 2012 г.
Изменения в нормативной правовой базе ЕГЭ в 2012 г. Хозяйство США
Хозяйство США Пижамные брюки. Обработка верхнего среза пижамных брюк притачным поясом
Пижамные брюки. Обработка верхнего среза пижамных брюк притачным поясом