Слайд 2Ethics are not …
Ethics is not the same as feelings
Ethics is not
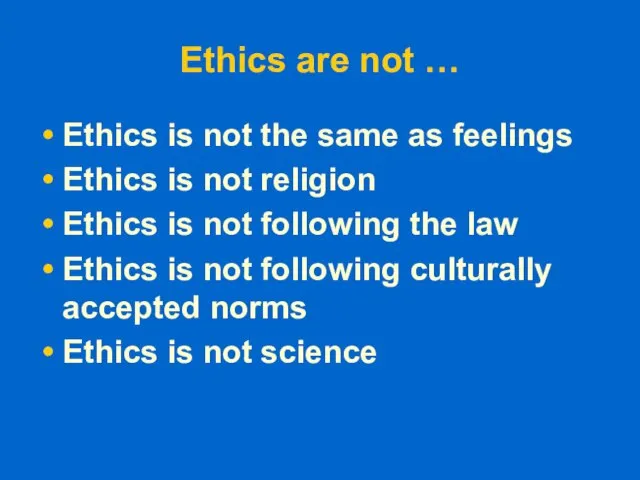
religion
Ethics is not following the law
Ethics is not following culturally accepted norms
Ethics is not science
Слайд 3Ethics are …
Moral Principles
What is good and bad
What is right and wrong
Based
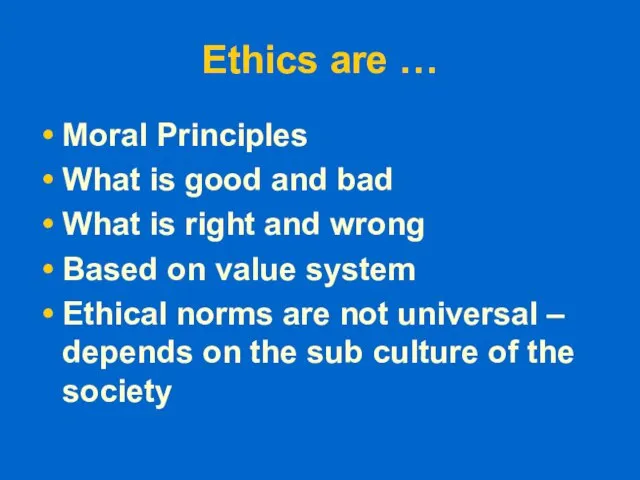
on value system
Ethical norms are not universal – depends on the sub culture of the society
Слайд 4ethics refers to standards of behavior that tell us how human beings
ought to act in the many situations in which they find themselves
as friends, parents, children, citizens, businesspeople, teachers, professionals, and so on.
Слайд 5Historically
medical ethics may be traced to guidelines on the duty of physicians
such as the Hippocratic oath
Слайд 6a physician must recognize responsibility to patients first and foremost, as well
as to society, to other health professionals, and to self. These are not laws, but standards of conduct which define the essentials of honorable behavior for the physician
Слайд 7Four basic Principles of Medical Ethics
Autonomy
Beneficence
Non maleficience
Justice
Слайд 8Autonomy
Patient has freedom of thought, intention and action when making decisions regarding
health care procedures
For a patient to make a fully informed decision, she/he must understand all risks and benefits of the procedure and the likelihood of success.
Слайд 9Always respect the autonomy of the patient - then the particular patient
is free to choose
Such respect is not simply a matter of attitude, but a way of acting so as to recognize and even promote the autonomous actions of the patient.
The autonomous person may freely choose loyalties or systems of religious belief that may adversely affect him
Слайд 10The patient must be informed clearly the consequences of his action that
may affect him adversely.
Desiring to "benefit" the patient, the physician may strongly want to intervene believing it to be a clear "medical benefit." The physician has a duty to respect the autonomous choice of the patient, as well as a duty to avoid harm and to provide a medical benefit.
Слайд 11But the physician should give greater priority to the respect for patient
autonomy than to the other duties.
However, at times this can be difficult because it can conflict with the paternalistic attitude of many health care professionals.
Слайд 12
In the case of a child, the principle of avoiding the harm
of death, and the principle of providing a medical benefit that can restore the child to health and life, would be given precedence over the autonomy of the child's parents as surrogate decision makers.
Слайд 13Beneficence
The practitioner should act in “the best interest” of the patient -
the procedure be provided with the intent of doing good to the patient
Слайд 14This needs health care provider to,
- develop and maintain skills and knowledge by
continually updating training
- consider individual circumstances of all patients
Слайд 15Non maleficence
“Above all, do no harm,“ – Make sure that the procedure
does not harm the patient or others in society
Слайд 16When interventions undertaken by physicians create a positive outcome while also potentially
doing harm it is known as the "double effect."
Eg,. the use of morphine in the dying patient. eases pain and suffering while hastening the demise through suppression of the respiratory drive
Слайд 17Physicians are obligated not prescribe medications they know to be harmful.
Some interpret
this value to exclude the practice of euthanasia
Violation of non-maleficence is the subject of medical malpractice litigation
Слайд 18Medical malpractice
An act or omission by a health care provider that deviates
from accepted standards of practice in the medical community which causes injury to the patient.
Слайд 19Justice
The distribution of scarce health resources, and the decision of who gets
what treatment “fairness and equality”
The burdens and benefits of new or experimental treatments must be distributed equally among all groups in society
 Викторина
Викторина Защита в шахматах
Защита в шахматах www.skywards.com
www.skywards.com Основные принципы успешности урока
Основные принципы успешности урока Орнамент филимоновской игрушки
Орнамент филимоновской игрушки Языческие Боги
Языческие Боги Правовой статус гражданина РФ
Правовой статус гражданина РФ Огневая подготовка
Огневая подготовка СОБЫТИЙНЫЙ МАРКЕТИНГ
СОБЫТИЙНЫЙ МАРКЕТИНГ Путь к пицца ДОДО
Путь к пицца ДОДО Какие они разные - эти геометрические фигуры!
Какие они разные - эти геометрические фигуры!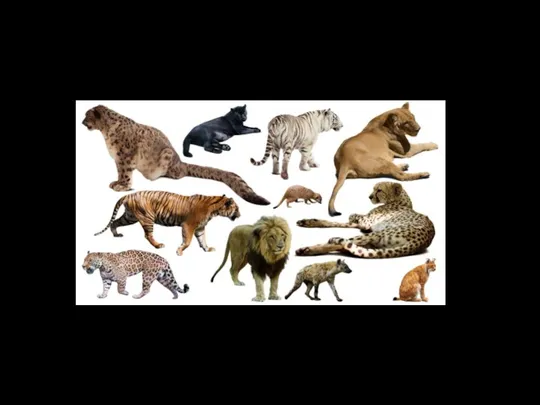 10201_7807318_13
10201_7807318_13 Ремонт одежды вышивкой
Ремонт одежды вышивкой Какое счастье быть полезным людям,учить Его Величество Народ!
Какое счастье быть полезным людям,учить Его Величество Народ! Будьте осторожны на дорогах
Будьте осторожны на дорогах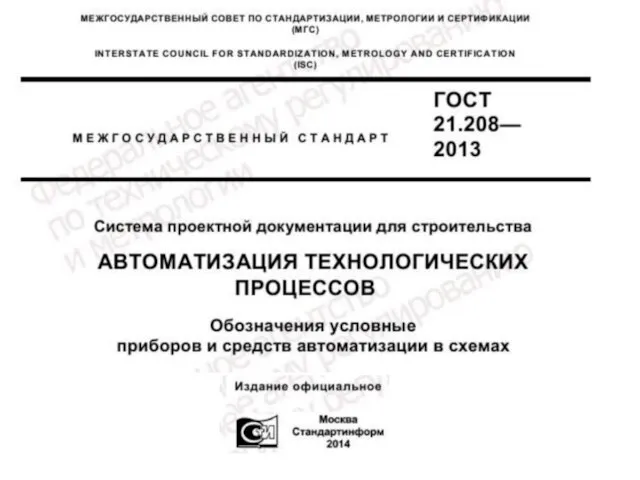 Обозначения условные приборов и средств автоматизации в схемах
Обозначения условные приборов и средств автоматизации в схемах Льготы предоставляемые военнослужащему
Льготы предоставляемые военнослужащему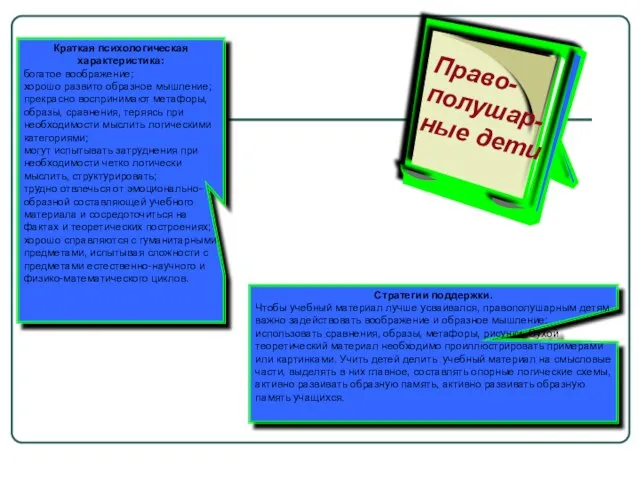 Правополушарные дети
Правополушарные дети В школе...
В школе... Кому нужны деревья
Кому нужны деревья ЛЕКЦИЯ 2 Основы термодинамики
ЛЕКЦИЯ 2 Основы термодинамики Что мы знаем о Балашихе?
Что мы знаем о Балашихе? saltwater fish
saltwater fish Вас приветствует компания «Мир Праздника»
Вас приветствует компания «Мир Праздника» Классный час. ТЕМА: «2014 – год культуры в России» - презентация для начальной школы
Классный час. ТЕМА: «2014 – год культуры в России» - презентация для начальной школы Восточная Сибирь
Восточная Сибирь QUIZ for CT Colonography
QUIZ for CT Colonography Исследование влияния автомобильного и железнодорожного транспорта на экологию нашего микрорайона
Исследование влияния автомобильного и железнодорожного транспорта на экологию нашего микрорайона