Содержание
- 2. The traumatic shock. The prehospital management. The blood replacement in trauma patients. Professor of the department
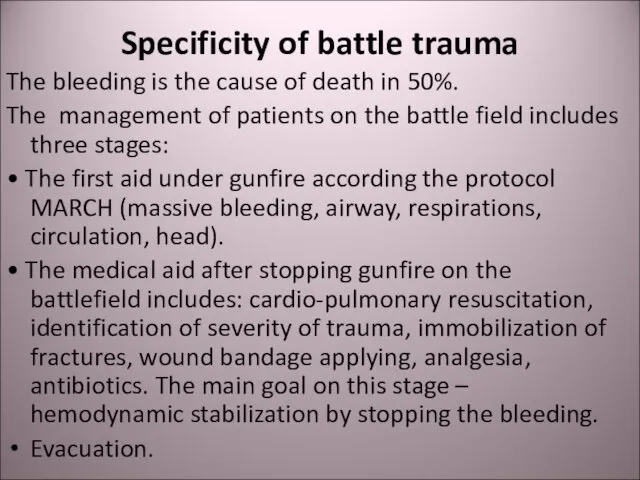
- 3. Specificity of battle trauma The bleeding is the cause of death in 50%. The management of
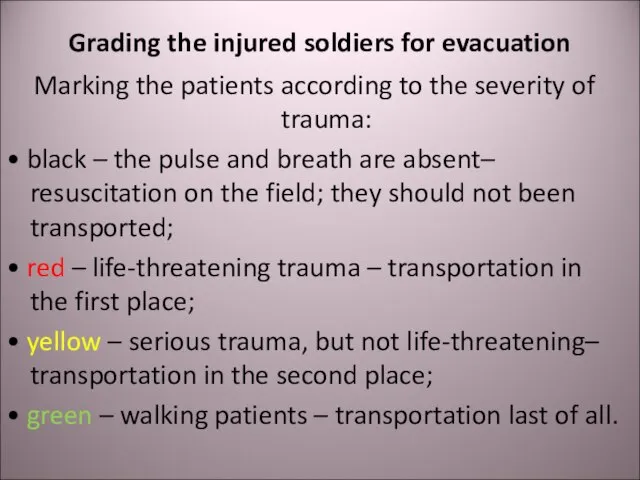
- 4. Grading the injured soldiers for evacuation Marking the patients according to the severity of trauma: •
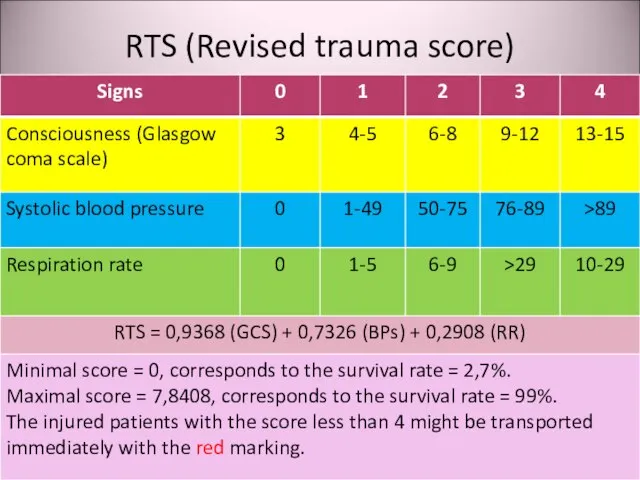
- 5. RTS (Revised trauma score)
- 6. Shock Acute hemodynamic instability, which leads to organ dysfunction due to poor perfusion, with poor oxygen
- 7. Causes of traumatic shock Hypovolemia due to bleeding or dehydration in burned patients; Cardiac failure due
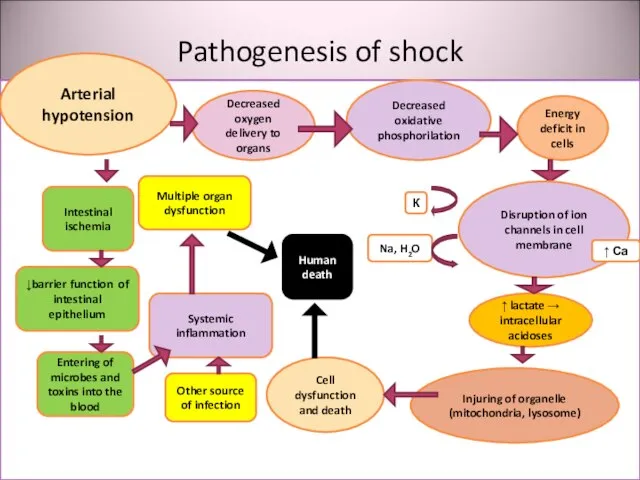
- 8. Pathogenesis of shock утрата Arterial hypotension Decreased oxygen delivery to organs Decreased oxidative phosphorilation Energy deficit
- 9. Clinical signs of shock Paleness Tachycardia Breathlessness Oliguria → anuria Impairment of consciousness Decreased blood pressure
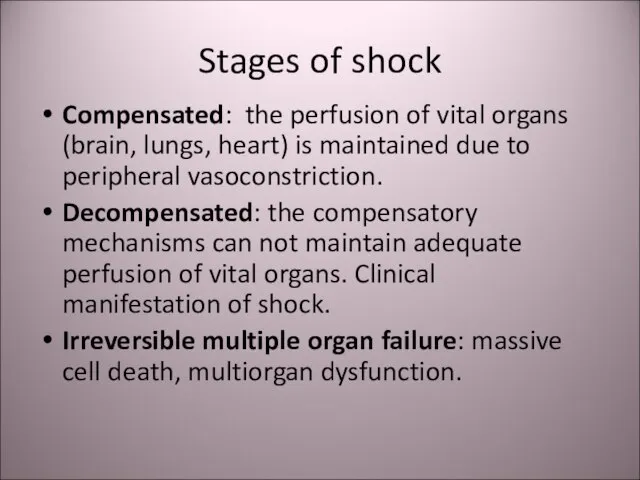
- 10. Stages of shock Compensated: the perfusion of vital organs (brain, lungs, heart) is maintained due to
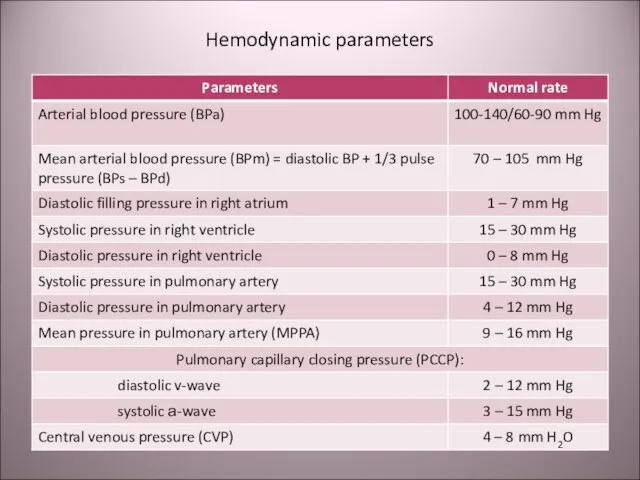
- 11. Hemodynamic parameters
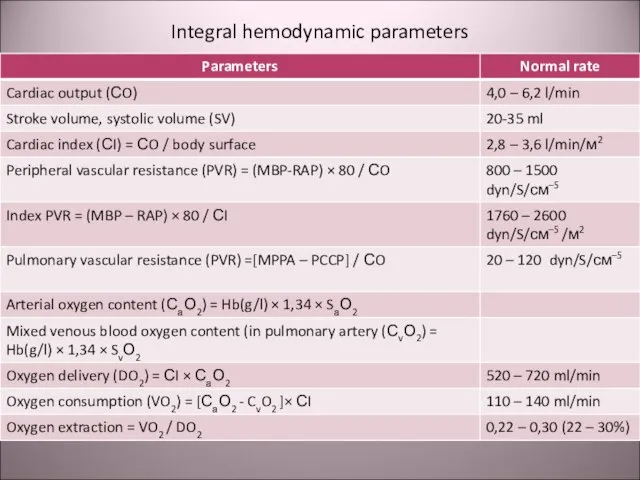
- 12. Integral hemodynamic parameters
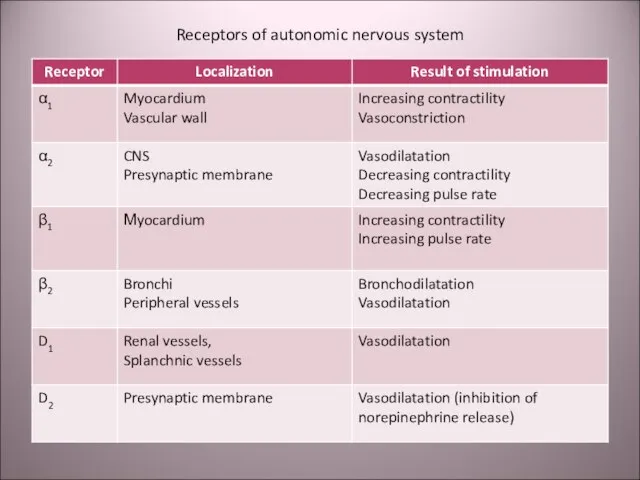
- 13. Receptors of autonomic nervous system
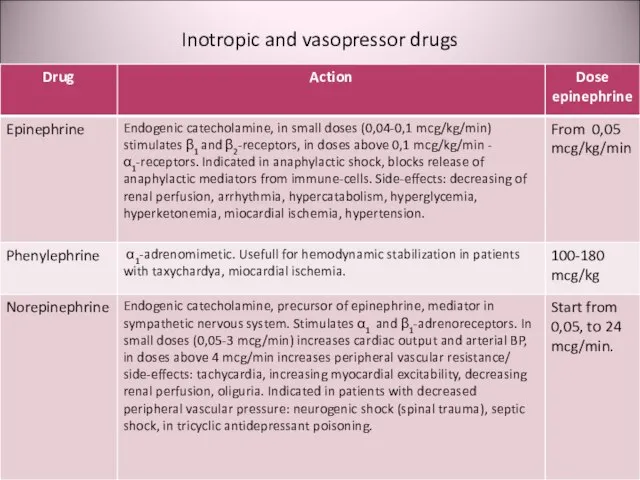
- 14. Inotropic and vasopressor drugs
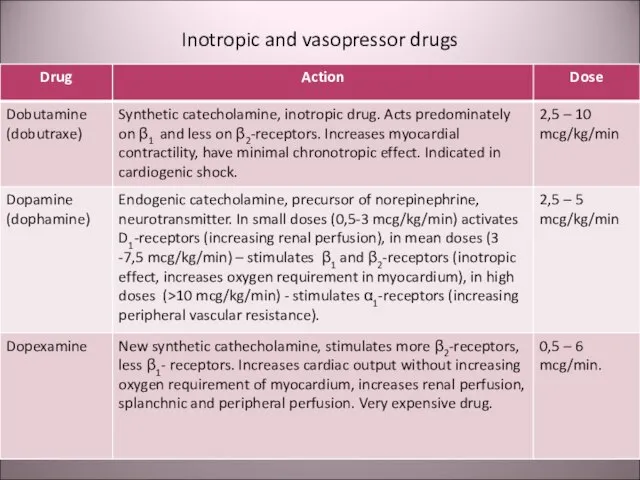
- 15. Inotropic and vasopressor drugs
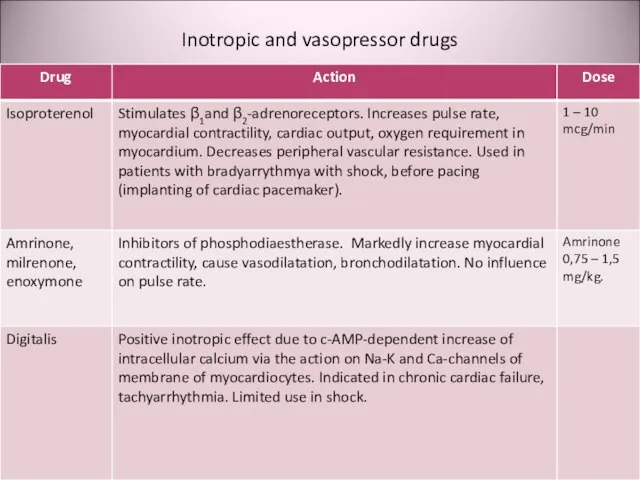
- 16. Inotropic and vasopressor drugs
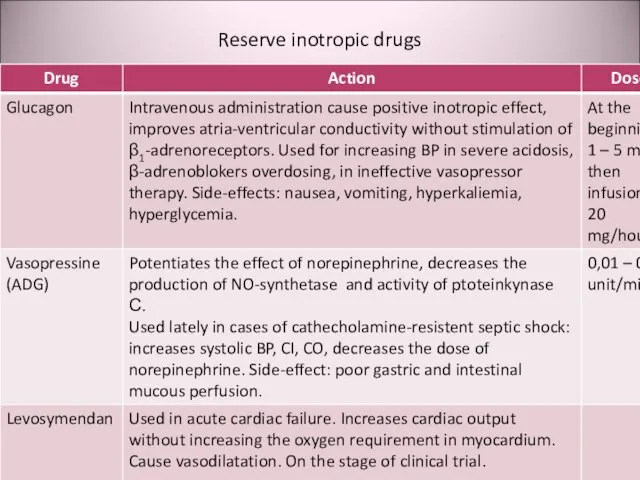
- 17. Reserve inotropic drugs
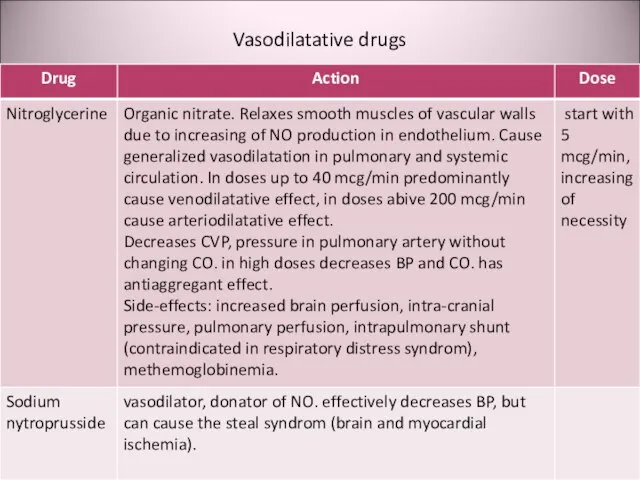
- 18. Vasodilatative drugs
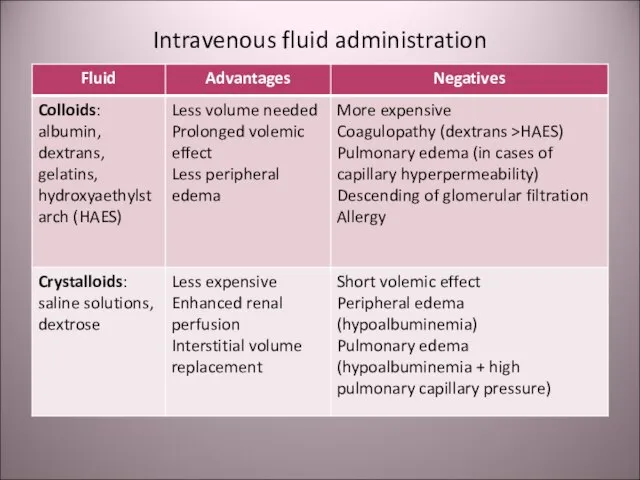
- 19. Intravenous fluid administration
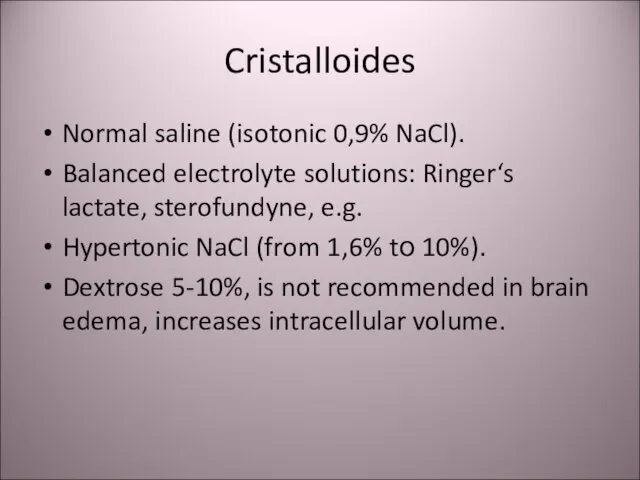
- 20. Cristalloides Normal saline (isotonic 0,9% NaCl). Balanced electrolyte solutions: Ringer‘s lactate, sterofundyne, e.g. Hypertonic NaCl (from
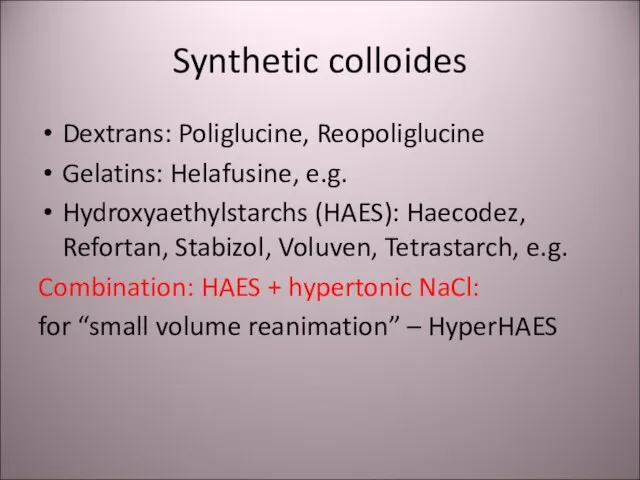
- 21. Synthetic colloides Dextrans: Poliglucine, Reopoliglucine Gelatins: Helafusine, e.g. Hydroxyaethylstarchs (HAES): Haecodez, Refortan, Stabizol, Voluven, Tetrastarch, e.g.
- 22. Polyhydric alcohol solutions: Sorbilact, Reosorbilact, Xylite Crystalloid solutions. Volemic effect is short. Advantages: Energy supply without
- 23. Polivinylpirrolidones: peristoy, haemodez The first synthetic colloides. Repeated administration can lead to depression of reticule-endothelial system
- 24. Perfluorocarbons: Perftoran («blue blood»). The positive effects were exaggerated and did not confirmed in medical practice.
- 25. Blood preparations Whole blood Packed red blood cells Fresh frozen plasma (FFP) Cryoprecipitate Platelets Albumin
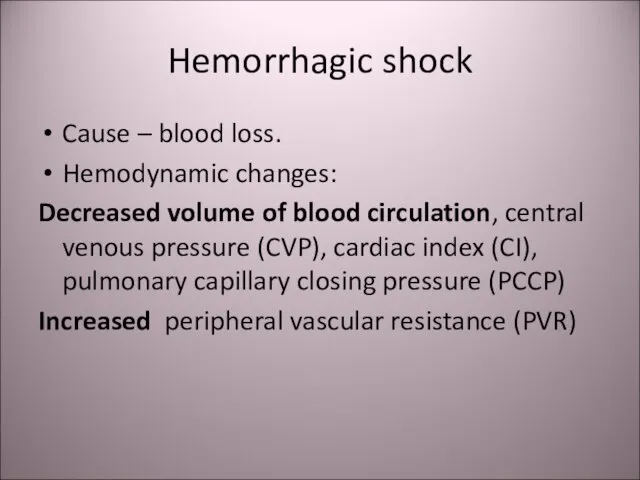
- 26. Hemorrhagic shock Cause – blood loss. Hemodynamic changes: Decreased volume of blood circulation, central venous pressure
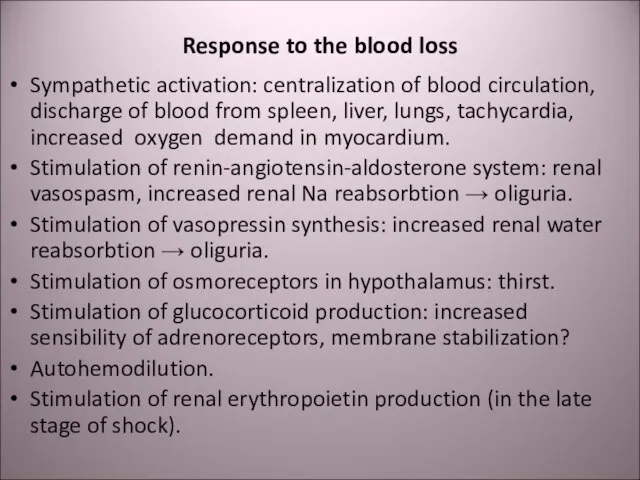
- 27. Response to the blood loss Sympathetic activation: centralization of blood circulation, discharge of blood from spleen,
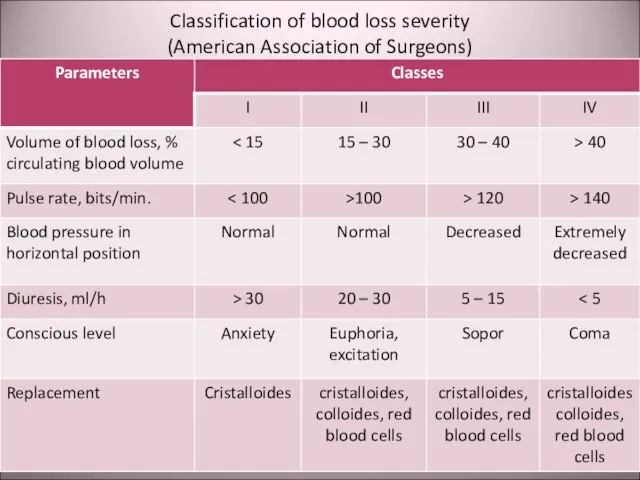
- 28. Classification of blood loss severity (American Association of Surgeons)
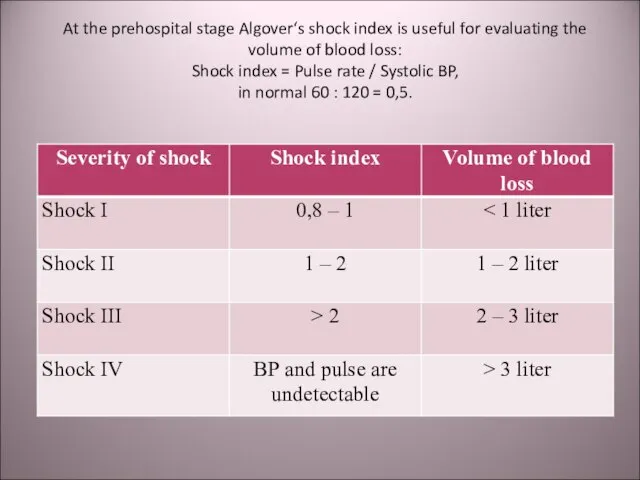
- 29. At the prehospital stage Algover‘s shock index is useful for evaluating the volume of blood loss:
- 30. Nomogram for calculating the blood volume deficit (Blutvolumendefizit [mL] – right vertical axis) according to the
- 31. Shock index: Is not informative in young children and old patients due to the age differences
- 32. Hemorrhagic shock Laboratory dates: Hb ↓. Ht ↓. Lactate ↑. Diuresis ↓. рН ↓.
- 33. Prehospital management of hemorrhagic shock Venous access – canulation of 2-3 veins; Crystalloid / colloid infusion;
- 34. Infusion rate in continuous bleeding If the bleeding is not stopped the infusion rate must provide
- 35. War – epidemic trauma In the ІІ word war all countries use the blood transfusion. But
- 36. Change of field doctrine On the basis of understanding the pathophisiology of traumatic shock as the
- 37. Change of doctrine The “liberal” regiment of crystalloid infusion gave rise to doubt in early 1990-th.
- 38. Step-by-step in replacement of blood loss At the first stage: saline cristalloids in restrictive regiment (for
- 39. “Damage control” In XX century wars (in Persian Gulf 1990-1991 and in Vietnam 1961-1973) 24% of
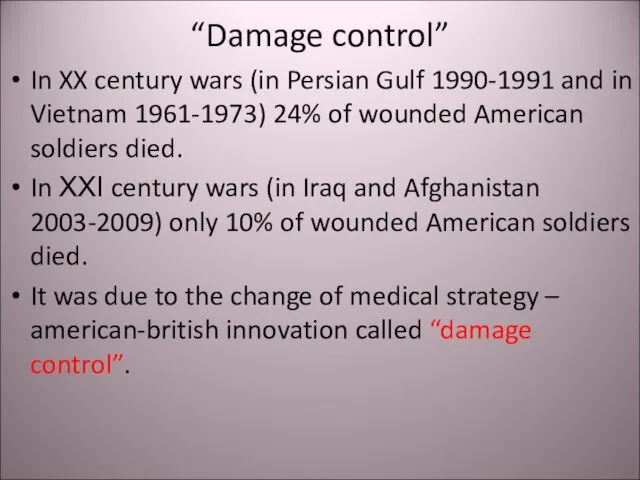
- 40. “Damage control” For surgeons it means the physiological correction, but not anatomical correction. This includes stop
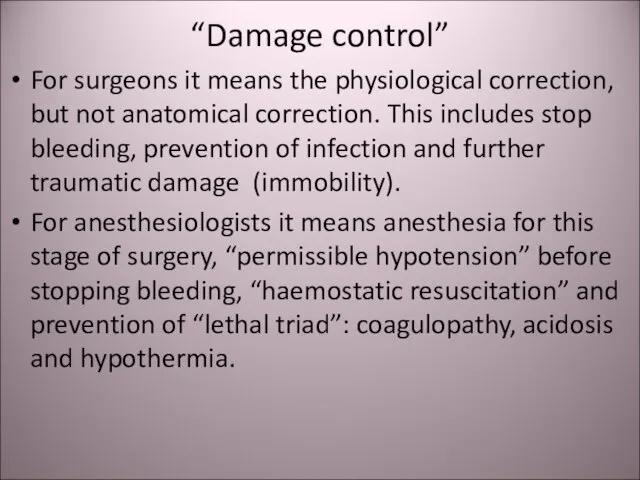
- 41. Complete surgical correction Complete surgical correction may be provided in 1-2 days after the stabilization of
- 42. Thank you for your attention! Questions?
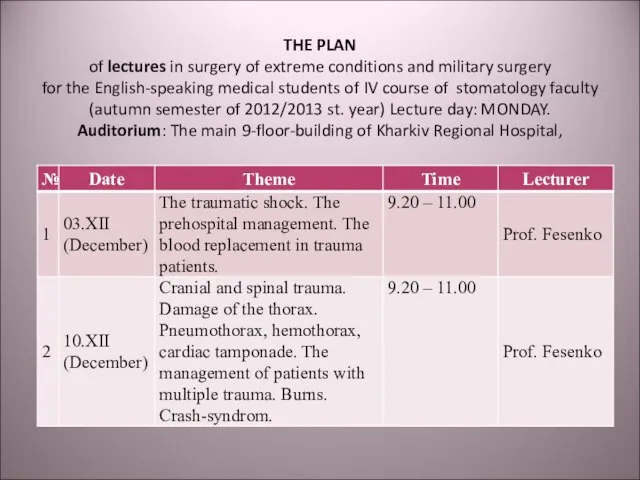
- 43. THE PLAN of lectures in surgery of extreme conditions and military surgery for the English-speaking medical
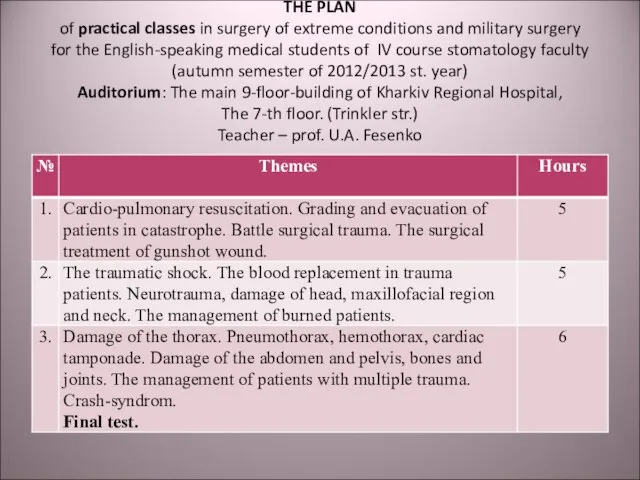
- 44. THE PLAN of practical classes in surgery of extreme conditions and military surgery for the English-speaking
- 46. Скачать презентацию
![Nomogram for calculating the blood volume deficit (Blutvolumendefizit [mL] – right vertical](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/381760/slide-29.jpg)

 Котел Минск 1
Котел Минск 1 Понятие и общая характеристика права собственности на землю
Понятие и общая характеристика права собственности на землю Выцинанка - Храм. Объединение Природа и фантазия
Выцинанка - Храм. Объединение Природа и фантазия Проект. Продвижение кафе
Проект. Продвижение кафе Налог на доходы физических лиц
Налог на доходы физических лиц Архитектура Древнего Рима
Архитектура Древнего Рима Презентация на тему Океаны
Презентация на тему Океаны  Приёмы здоровьесберегающих технологий в начальной школе
Приёмы здоровьесберегающих технологий в начальной школе Методы принятия управленческих решений. Лекция 1
Методы принятия управленческих решений. Лекция 1 Детерминанты коррупции. Социальные последствия коррупции. Тема 2
Детерминанты коррупции. Социальные последствия коррупции. Тема 2 Конституция РФ
Конституция РФ Реинжениринг данных общего архива наблюдений САО РАН
Реинжениринг данных общего архива наблюдений САО РАН Налог на профессиональный доход
Налог на профессиональный доход Развитие универсальных учебных действий при обучении написанию изложения
Развитие универсальных учебных действий при обучении написанию изложения Word-formation in Modern
Word-formation in Modern Тема урока « Наука и семья»8 КЛАСС( химия и литература)
Тема урока « Наука и семья»8 КЛАСС( химия и литература) Процесс многократного рассеяния
Процесс многократного рассеяния Арисова
Арисова Организация деятельности учреждений дополнительного образования с использованием договоров сетевого взаимодействия
Организация деятельности учреждений дополнительного образования с использованием договоров сетевого взаимодействия Экономика Москвы
Экономика Москвы  Гарибян Ирина Ивановна доцент, победитель Фонда «Форум культуры и искусства Узбекистана»
Гарибян Ирина Ивановна доцент, победитель Фонда «Форум культуры и искусства Узбекистана» Формы работы на приходе с молодежью: организация направлений деятельности и приходских кружков
Формы работы на приходе с молодежью: организация направлений деятельности и приходских кружков Презентация1
Презентация1 Борис Иванович Кудрин
Борис Иванович Кудрин Подготовка муниципальных образовательных учреждений к 2011-2012 учебному году
Подготовка муниципальных образовательных учреждений к 2011-2012 учебному году GENTLE DAY
GENTLE DAY Презентация на тему Г. Остер. "Задачник"
Презентация на тему Г. Остер. "Задачник"  Физиологические и мотивационные аспекты волевых действий
Физиологические и мотивационные аспекты волевых действий