Содержание
- 2. Introduction
- 4. Definitions & Terminology Fertility: the capacity to reproduce or the state of being fertile. Fecundability: the
- 5. Definitions & Terminology Infertility: one year of unprotected coitus without conception. Primary infertility: couple who has
- 6. Epidemiology Fecundability rate in the general reproductive-aged population is fairly constant and is approximately 0.22 per
- 7. Fecundability 20-25% of couples will conceive/cycle. 50% should conceive after 3-4 months. 95% should conceive after
- 8. Infertility Affects 1 in 6 married couples of childbearing age Primary infertility : 58.6%. Secondary infertility:
- 9. Etiology of Infertility
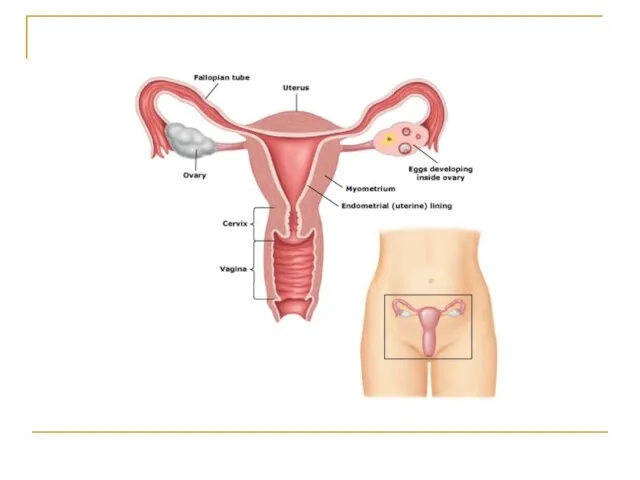
- 10. Requirements for Normal Reproduction Release of a normal preovulatory oocyte. Production of adequate spermatozoa. Normal transport
- 11. Female Factor Infertility Female factor infertility can be divided into several categories: Cervical factor infertility Uterine
- 12. Cervical factor infertility Account for 5-10% of infertility. Can be caused by: Cervical stenosis Abnormalities of
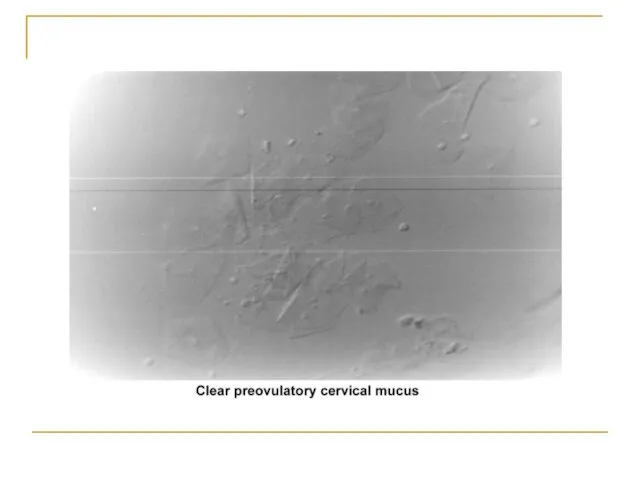
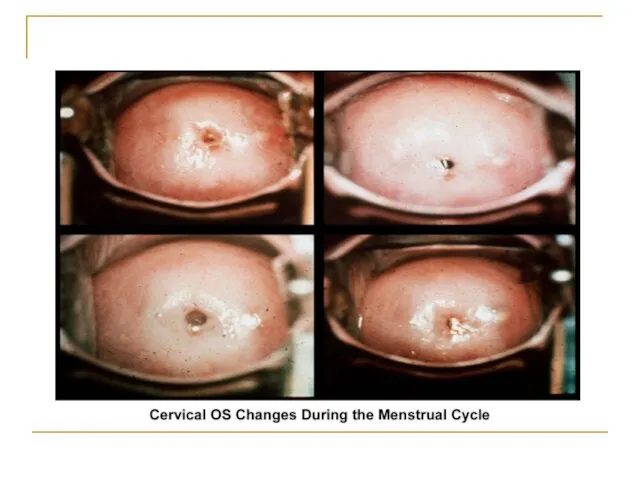
- 13. Cervical mucus production and characteristics It changes according to the estrogen concentration during the late follicular
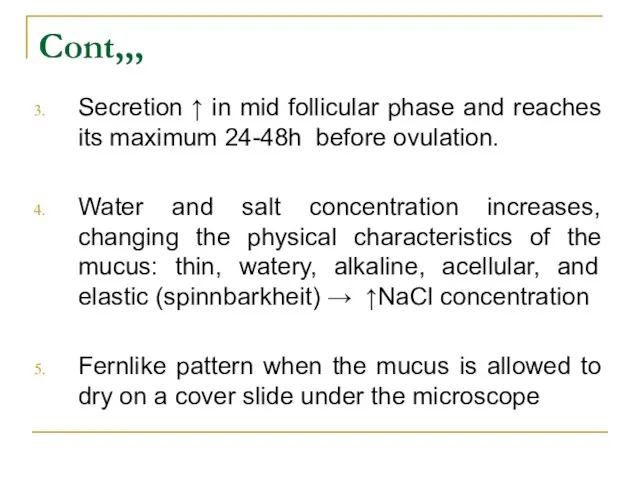
- 15. Cont,,, Secretion ↑ in mid follicular phase and reaches its maximum 24-48h before ovulation. Water and
- 17. Cont,,, The mucus organizes itself, forming multiple microchannels so the spermatozoa can travel through. Spermatozoa simultaneously
- 18. Cont,,, Mucus secretion may be altered by hormonal changes and medications, especially drugs like clomiphene citrate,
- 19. Cont,,, Cervical stenosis can cause infertility by blocking the passage of sperm from the cervix to
- 21. Uterine factor infertility May be associated with primary infertility or with pregnancy wastage and premature delivery.
- 22. Congenital defects The full spectrum of congenital/müllerian abnormalities varies from: Total absence of the uterus and
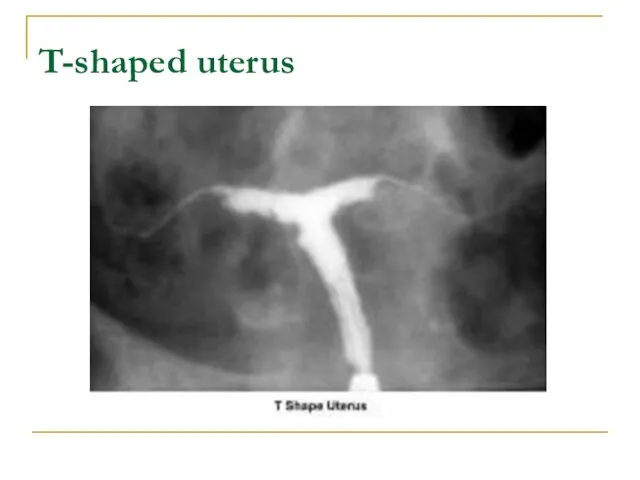
- 23. The most common uterine malformations observed during the past 40 years were drug induced. From the
- 24. Ddiethylstilbestrol (DES) DES was found to be responsible for inducing malformations of the uterine cervix, irregularities
- 25. Premature delivery has been associated with cervical incompetence. Unicornuate uterus associated with a blind horn, and
- 26. Acquired defects Endometritis associated with a traumatic delivery, dilatation and curettage, intrauterine device, or any instrumentation
- 27. Cont,,, Placental polyps may develop from placental remains. Intrauterine and submucosal fibroids are very common, affecting
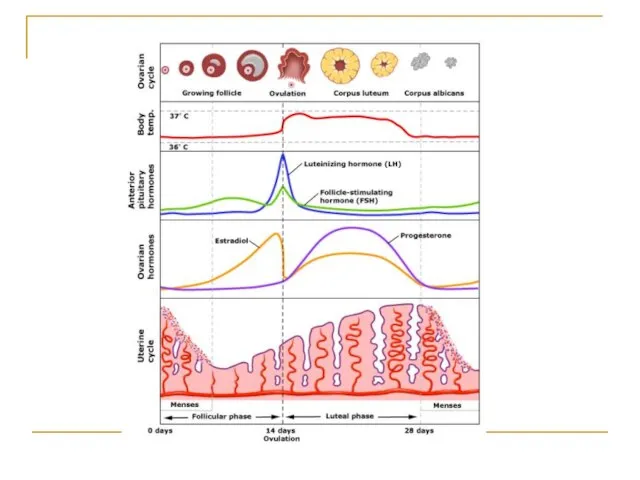
- 28. Ovarian factor infertility Ovulatory dysfunction is defined as an alteration in the frequency and duration of
- 29. Tubal factors infertility Abnormalities or damage to the fallopian tube interferes with fertility and is responsible
- 30. Other tubal factors associated with infertility are either congenital or acquired. Congenital absence of the fallopian
- 31. Advanced age The prevalence of infertility rises dramatically as age increases. Fertility decreases with marriage duration
- 32. Peritoneal Factor Infertility Pelvic inflammatory disease Associated with gonorrhea and chlamydia infection . The rate of
- 33. Endometriosis Remains an enigmatic disease that affects women during their reproductive years. The evolution of the
- 35. Approach To Infertility and Evaluation of Infertile Couple
- 36. General Guidance on Evaluation of Infertility Infertility is a problem that involves both partners. The consultation
- 37. History Type of infertility (primary or secondary) Detailed history of previous pregnancies Specific questions: Frequency of
- 38. Female: menstrual history frequency patterns since menarche.
- 39. Male: semen analysis results history of impotence premature ejaculation change in libido history of testicular trauma
- 40. Ask the couple about: surgical contraception weight changes Lifestyle exercise medical treatment Smoking
- 41. Physical Body Mass Index skin evaluation of hair distribution Malformed face or limbs (congenital abnormalities) visual
- 42. Comprehensive Evaluation of Infertility Cervical factors Uterine factors Tubal and peritoneal factors Ovarian factors
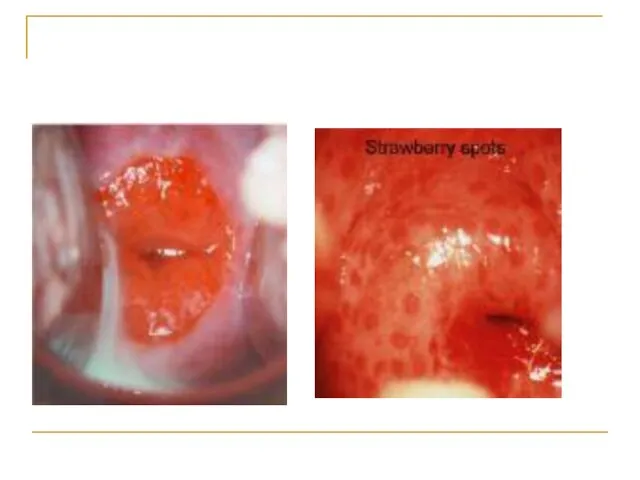
- 44. Cervical factors Congenital: Severe stenosis Inflammatory: chronic cervicitis Neoplastic causes: Cervical polyp or cervical fibroid. Cervical
- 46. Cervical factors The postcoital test: evaluating the amount of spermatozoa and its motility within the cervical
- 47. Uterine factors Congenital causes: Uterine aplasia, hypoplasia, septate uterus. Inflammatory causes: Tuberculous endometritis. Neoplastic causes: Fibroid
- 48. HSG pelvic ultrasonography Hysteroscopy MRI
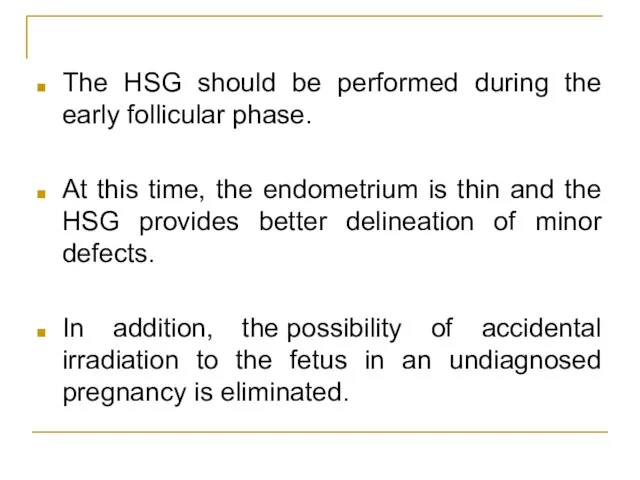
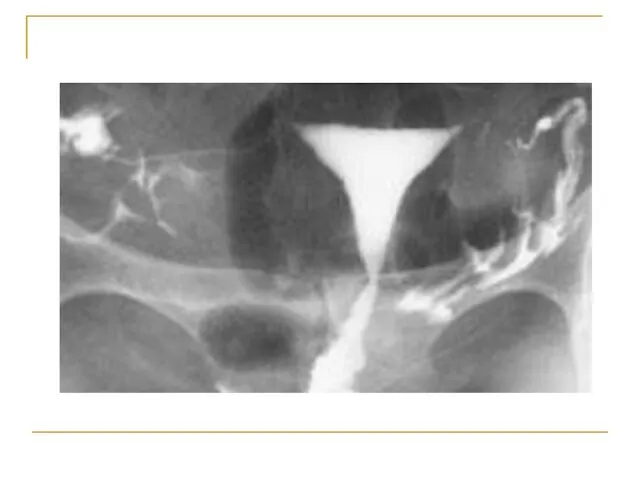
- 49. Hysterosalpingogram To evaluate: endocervical canal diameter and configuration of the internal os endometrial cavity uterine/tubal junction
- 50. The HSG should be performed during the early follicular phase. At this time, the endometrium is
- 52. T-shaped uterus
- 53. Endometrial biopsy
- 54. Tubal and peritoneal factors Congenital: aplasia or hypoplasia of the fallopian tube. Traumatic causes: Tubal ligation
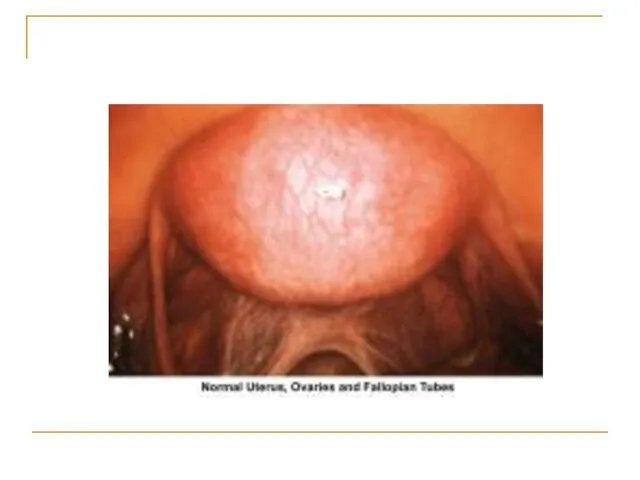
- 55. Laparoscopy hysterosalpingogram
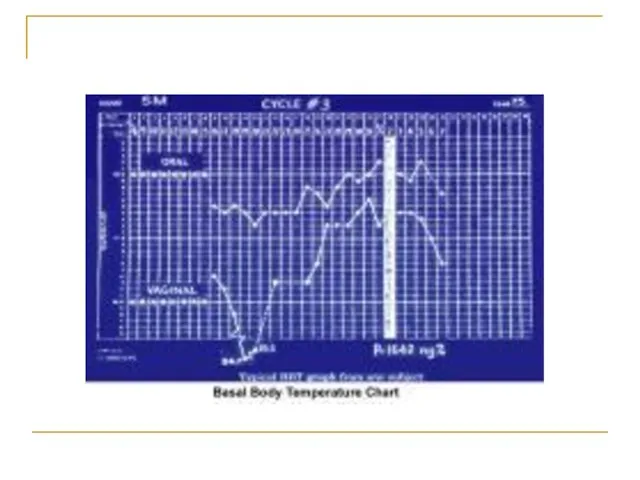
- 57. Ovarian factors Menstrual history Basal body temperature Hormone levels Blood levels of the hormone progesterone are
- 60. Evaluation of the Male Partner Semen analysis: The basic semen analysis assesses sperm concentration motility Morphology
- 61. Volume - 2-5 mL pH level - 7.2-7.8 Sperm concentration - 20 million or greater Motility
- 62. Interpretation of semen analysis Azoospermia indicates absence of sperm Oligozoospermia indicates a concentration of fewer than
- 63. Kruger criteria If the initial semen analysis is abnormal, the clinician will often request an additional
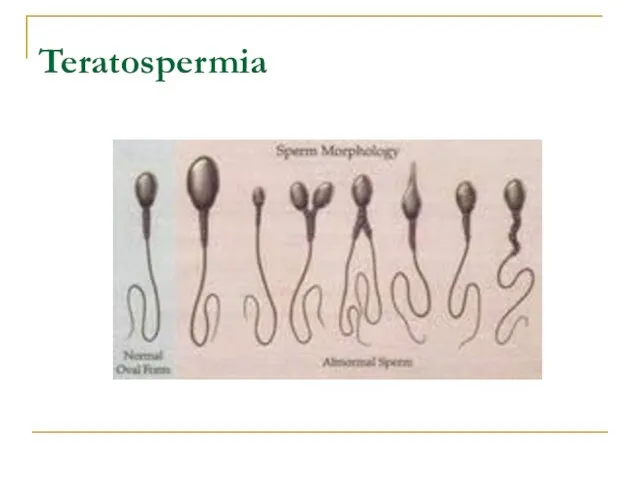
- 64. Teratospermia
- 65. Blood tests: to measure total testosterone, LH , FSH and prolactin may be ordered. Genetic tests:
- 66. Other tests If a blockage in the reproductive tract is suspected, a transrectal ultrasound test may
- 67. Infertility Treatment
- 68. Treatment of infertility depends on the cause, diagnosis, duration of infertility, age of the partners and
- 69. Restoring fertility: These approaches can involve steps related to the male or to the female, or
- 70. Treatment for men General sexual problems: Addressing impotence or premature ejaculation can improve fertility. Treatment for
- 71. Treatment for women Stimulating ovulation with fertility drugs: Fertility drugs are the main treatment for women
- 72. Commonly used fertility drugs include: Clomiphene citrate (Clomid, Serophene): Taken orally and stimulates ovulation in women
- 73. Human menopausal gonadotropin, or hMG (Repronex): This is an injected medication is for women who do
- 74. Follicle-stimulating hormone, or FSH (Gonal-F, Follistim, Bravelle): FSH works by stimulating the ovaries to mature egg
- 75. Gonadotropin-releasing hormone (Gn-RH) analogs: This treatment is for women with irregular ovulatory cycles or who ovulate
- 76. Letrozole (Femara): A class of medications called aromatase inhibitors, which are approved for treatment of advanced
- 77. Metformin (Glucophage): Oral drug taken to boost ovulation. It is used when insulin resistance is a
- 78. Bromocriptine: This medication is for women whose ovulation cycles are irregular due to elevated levels of
- 79. Fertility drugs and the risk of multiple pregnancies: Injectable fertility drugs increase the chance of multiple
- 80. The greater the number of fetuses, the higher the risk of premature labor. Babies born prematurely
- 81. If a woman requires an HCG injection to trigger ovulation, and ultrasound exams show that too
- 82. Surgery Depending on the cause, surgery may be a treatment option for infertility. Blockages or other
- 83. Assisted reproductive technology (ART)
- 84. Assisted reproductive technology (ART) ART has revolutionized the treatment of infertility. An ART health team includes
- 85. In Vitro Fertilization
- 86. Historical Perspective The first successful human IVF attempt resulted in the 1978 delivery of Louise Brown
- 87. Definition: In Vitro Fertilization is commonly referred to as IVF. It is the process of fertilization
- 88. When the IVF procedure is successful, the process is combined with a procedure known as embryo
- 89. Indications: Failed other treatments Tubal damage Significant male factor Absent uterus Carriers of genetic diseases Family
- 90. Method: There are basically five steps in the IVF and embryo transfer process which include the
- 91. 1. Ovarian stimulation Treatment cycles are typically started on the third day of menstruation. It consists
- 92. Typically approximately 10 days of injections will be necessary. Spontaneous ovulation during the cycle is typically
- 93. 2. Egg retrieval When follicular maturation is judged to be adequate, human chorionic gonadotropin (hCG) is
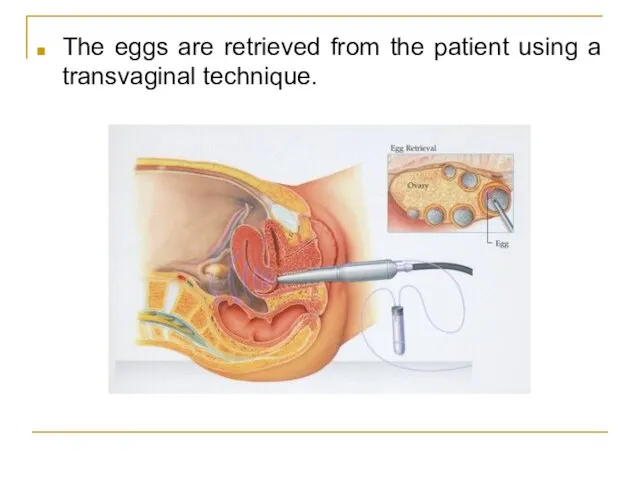
- 94. The eggs are retrieved from the patient using a transvaginal technique.
- 95. Through this needle follicles can be aspirated, and the follicular fluid is handed to the IVF
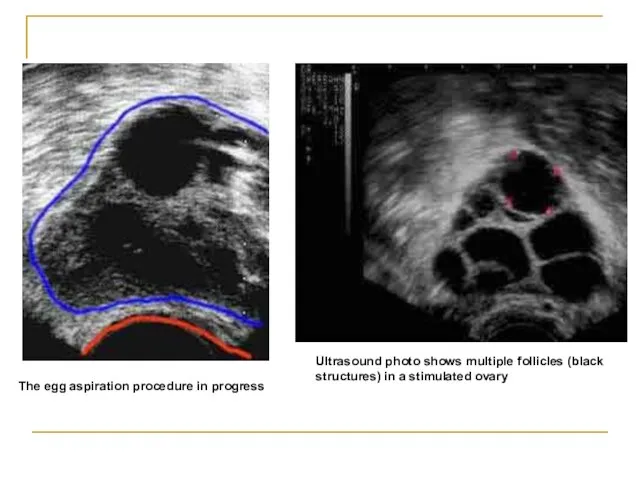
- 96. Ultrasound photo shows multiple follicles (black structures) in a stimulated ovary The egg aspiration procedure in
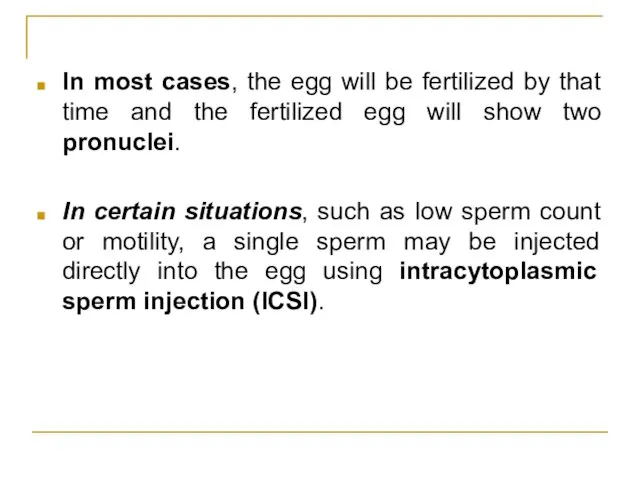
- 97. 3. Fertilization In the laboratory, the identified eggs are stripped of surrounding cells and prepared for
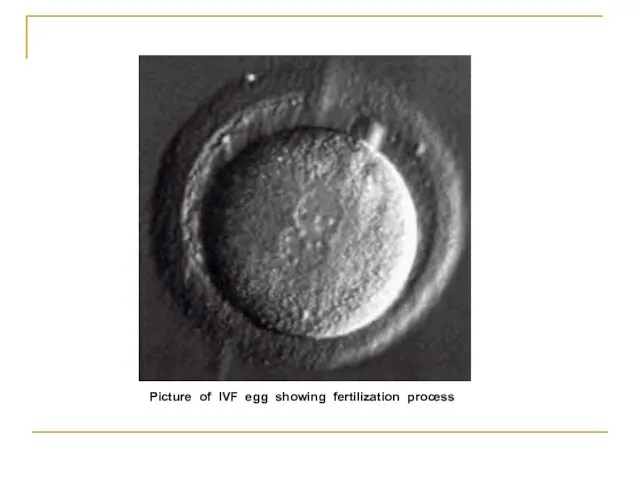
- 98. In most cases, the egg will be fertilized by that time and the fertilized egg will
- 99. Picture of IVF egg showing fertilization process
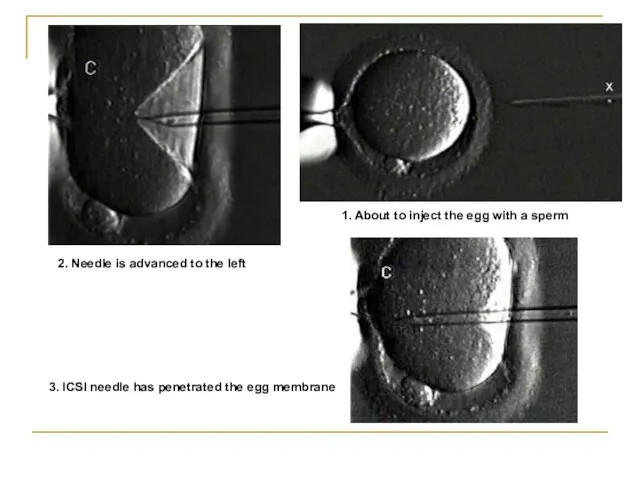
- 100. 1. About to inject the egg with a sperm 2. Needle is advanced to the left
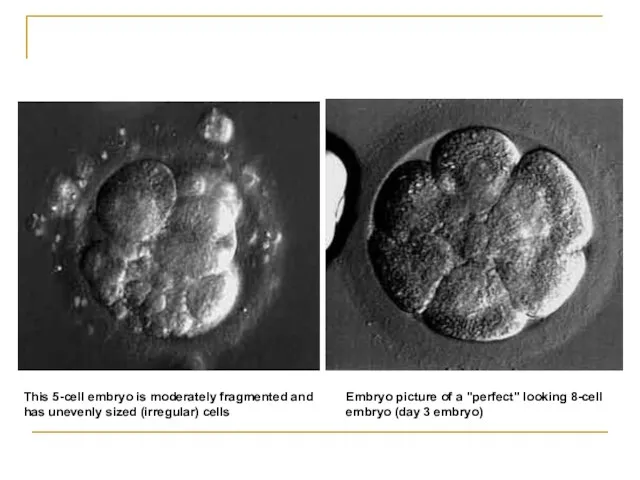
- 101. 4. Selection Typically, embryos that have reached the 6-8 cell stage are transferred three days after
- 102. Embryo picture of a "perfect" looking 8-cell embryo (day 3 embryo) This 5-cell embryo is moderately
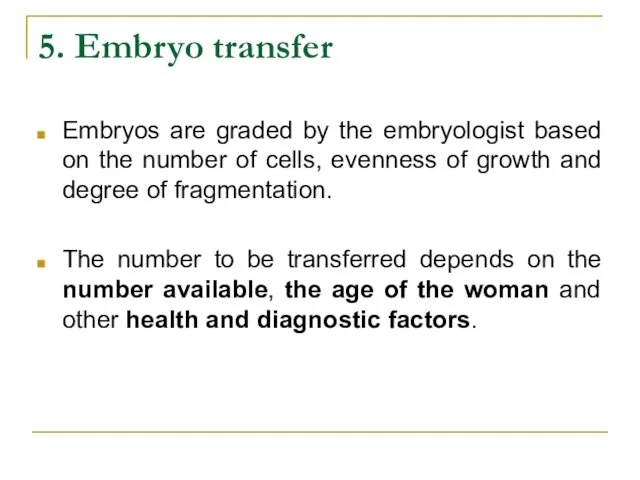
- 103. 5. Embryo transfer Embryos are graded by the embryologist based on the number of cells, evenness
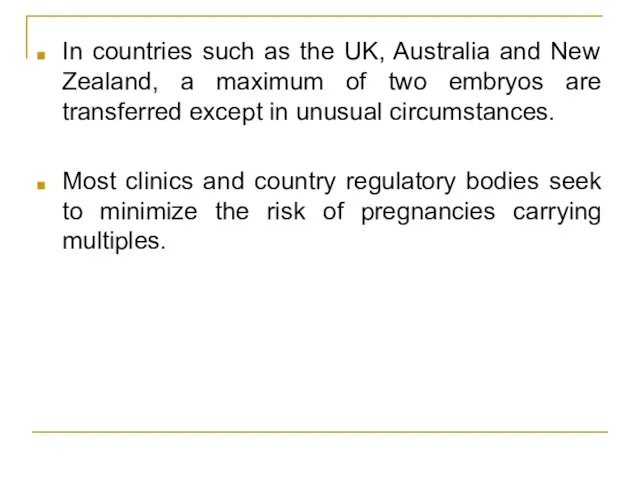
- 104. In countries such as the UK, Australia and New Zealand, a maximum of two embryos are
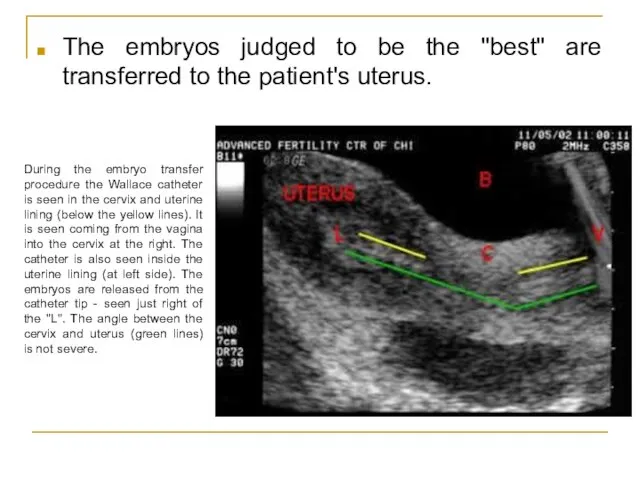
- 105. The embryos judged to be the "best" are transferred to the patient's uterus. During the embryo
- 106. What Happens to the Other Embryos? Freeze Embryos Donate For Research/Stem Cells Embryo Adoption Discard!
- 107. Pregnancy Rates For IVF, it is the percentage of all attempts that lead to pregnancy. With
- 108. Complications The major complication of IVF is the risk of multiple births. Multiple births are related
- 109. A double blind, randomized study followed IVF pregnancies that resulted in 73 infants (33 boys and
- 110. Another risk of ovarian stimulation is the development of ovarian hyperstimulation syndrome. In 2008, an analysis
- 111. Special IVF Procedures PGD PGD (Preimplantation Genetic Diagnosis) can be performed on embryos before the embryo
- 112. Special IVF Procedures ZIFT In the process of ZIFT (Zygote Intrafallopian Transfer), eggs are removed from
- 113. References: Hacker & Moore's Essentials of Obstetrics and Gynecology www.emedicine.medscape.com/article/274143-overview http://www.mayoclinic.com/health/infertility/ds00310 UpToDate www.ncbi.org http://en.wikipedia.org/wiki/Infertility
- 115. Скачать презентацию
 Закрепление вычислительных приемов умножения и деления
Закрепление вычислительных приемов умножения и деления Морская авиация ВМФ
Морская авиация ВМФ Альдегиды и кетоны
Альдегиды и кетоны Преступление_14.10
Преступление_14.10 Madame Tussauds
Madame Tussauds Проблема непрерывности бизнеса
Проблема непрерывности бизнеса Система товародвижения в маркетинге
Система товародвижения в маркетинге Тема №3
Тема №3 Модуль интеграции CAD-системы "КОМПАС-3D v8" с CAE-системой "Асоника-ТМ"
Модуль интеграции CAD-системы "КОМПАС-3D v8" с CAE-системой "Асоника-ТМ" Государство в политической системе общества
Государство в политической системе общества Литье металлов
Литье металлов Здравствуйте!Я звездочёт - волшебник.
Здравствуйте!Я звездочёт - волшебник. Построение бизнес-моделей
Построение бизнес-моделей Мобильное приложение TAM-TAM-SALE. Скидки рядом с Вами
Мобильное приложение TAM-TAM-SALE. Скидки рядом с Вами Общевоинские уставы ВС РФ
Общевоинские уставы ВС РФ Прогрессивные формы внешнеэкономической деятельности в Ставропольском крае Выполнил: Котов О.Ю 5 курс, 4.1 группа
Прогрессивные формы внешнеэкономической деятельности в Ставропольском крае Выполнил: Котов О.Ю 5 курс, 4.1 группа Отечественная война 1812 года в романе Л.Н.Толстого "Война и мир"
Отечественная война 1812 года в романе Л.Н.Толстого "Война и мир" Положение человека в системе животного мира
Положение человека в системе животного мира Нравственное становление детей дошкольного возраста при использовании краеведческого материала с учётом ФГОС ДО. (Лекция 2)
Нравственное становление детей дошкольного возраста при использовании краеведческого материала с учётом ФГОС ДО. (Лекция 2) Назначение операционных систем
Назначение операционных систем  Мои увлечения. Корнеева Арина
Мои увлечения. Корнеева Арина Теория цвета Ньютон
Теория цвета Ньютон Модели аддиктивного поведения
Модели аддиктивного поведения Колоквиум ХЦВ Сабанцев
Колоквиум ХЦВ Сабанцев Автоматизация звука С в чистоговорках, потешках и стихах
Автоматизация звука С в чистоговорках, потешках и стихах Общая собственность
Общая собственность Психологическое сопровождение учащихся как фактор сохранения психологического здоровья
Психологическое сопровождение учащихся как фактор сохранения психологического здоровья Формула успеха: стратегии поведения выпускников при подготовке к ГИА
Формула успеха: стратегии поведения выпускников при подготовке к ГИА