Слайд 2 Introduction
5-10% of all trauma
Overall mortality rate as high as 11%
Major vessel injury
fatal in 65%, including prehospital deaths
Attending physician must have excellent knowledge of anatomy
Слайд 3Historical Perspective/ pre WW I
Ligation of the major vessels described as early
as 1522 by Ambrose Pare
Ligation was the procedure of choice for vascular injury through WW 1
Associated mortality rates up to 60%
Significant neurologic impairment in 30 %
Слайд 4Historical / post WW II
Mandatory exploration of all penetrating neck wounds, through
the platysma
Fogelman and Stewart reported Parkland Memorial Hospital experience of early, mandatory exploration with mortality of 65 vs.. 35% for delayed exploration
40% to 60% rate of negative explorations with mandatory exploration
Present mortality for civilian wounds is 4% to 6%
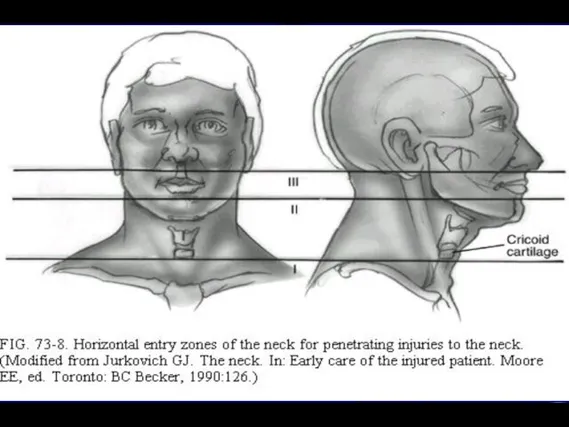
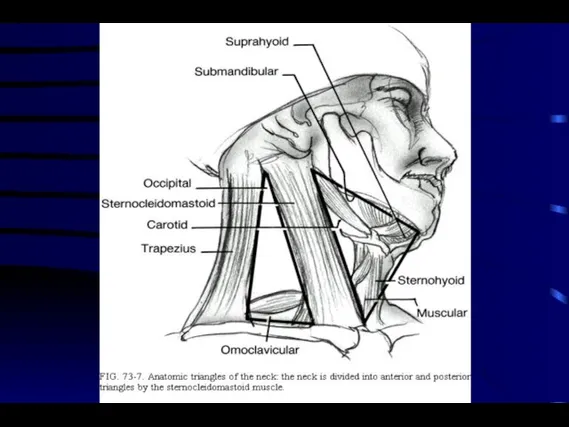
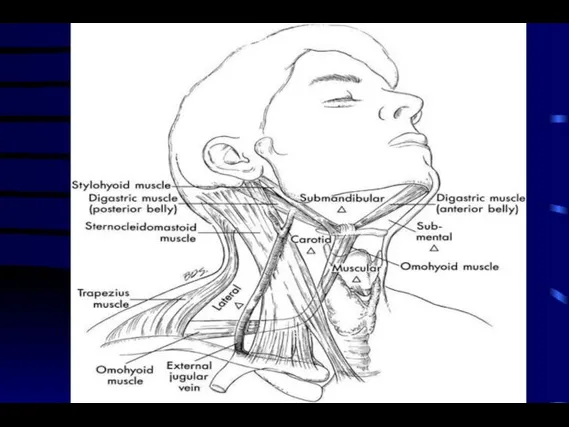
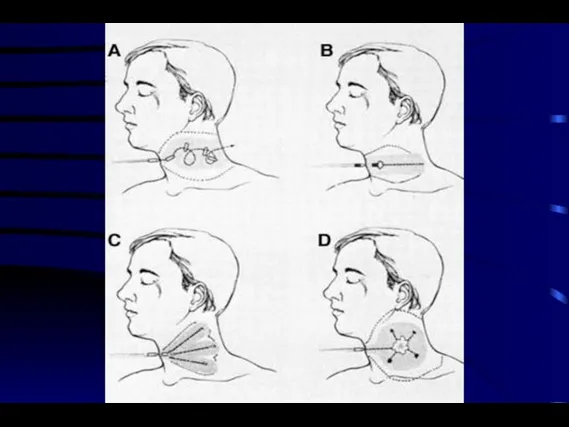
Слайд 6Anatomy/Zone I
Bound superiorly by the cricoid and inferiorly by the sternum and
clavicles
Contains the subclavian arteries and veins, the dome of the pleura, esophagus, great vessels of the neck, recurrent nerve, trachea
Signs of significant injury may be hidden from inspection in the mediastinum or chest
Слайд 7Anatomy/Zone II
Bound inferiorly by the cricoid and superiorly by the angle of
the mandible
Contains the larynx, pharynx, base of tongue, carotid artery and jugular vein, phrenic, vagus, and hypoglossal nerves
Injuries here are seldom occult
Common site of carotid injury
Слайд 8Anatomy/Zone III
Lies above the angle of the mandible
Contains the internal and external
carotid arteries, the vertebral artery, and several cranial nerves
Vascular and cranial nerve injuries common
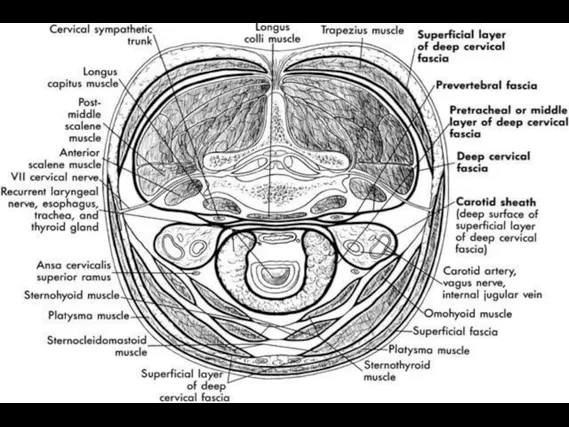
Слайд 9Fascial Layers
Superficial cervical fascia - platysma
Deep cervical fascia
Investing: sternocleidomastoid muscle, trapezius muscle
Pretracheal:
larynx, trachea, thyroid gland, pericardium
Prevertebral: prevertebral muscles, phrenic nerve, brachial plexus, axillary sheath
Carotid sheath: carotid artery, internal jugular vein, vagus nerve
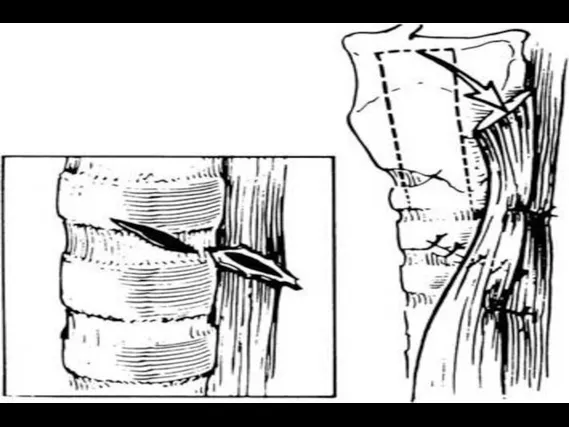
Слайд 13Ballistics
Over 95% of penetrating neck wounds are from guns and knives, remainder
from motor vehicle, household, and industrial accidents
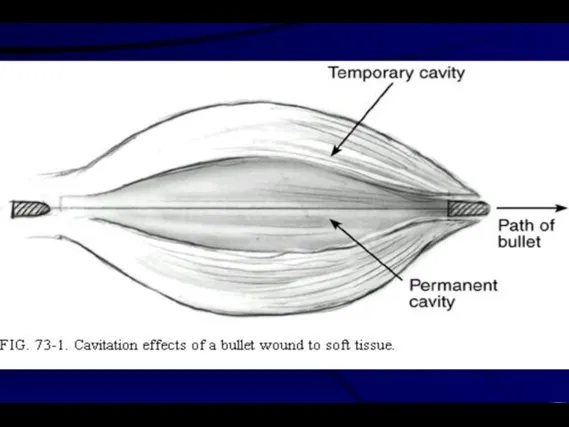
The amount of energy transferred to tissue is difference between the kinetic energy of the projectile when it enters the tissue, and the kinetic energy of any exiting fragments or projectiles
The velocity of the projectile is the most significant aspect of energy transfer (K.E. = 1/2 mv^2
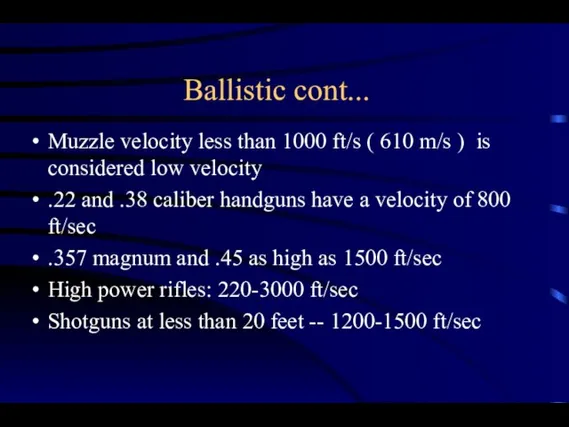
Слайд 14Ballistic cont...
Muzzle velocity less than 1000 ft/s ( 610 m/s ) is
considered low velocity
.22 and .38 caliber handguns have a velocity of 800 ft/sec
.357 magnum and .45 as high as 1500 ft/sec
High power rifles: 220-3000 ft/sec
Shotguns at less than 20 feet -- 1200-1500 ft/sec
Слайд 15Ballistic cont.
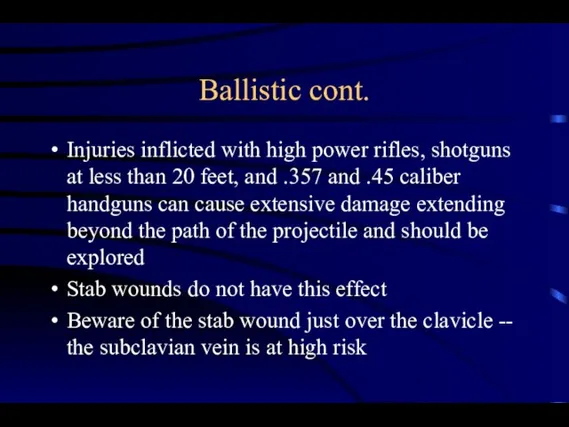
Injuries inflicted with high power rifles, shotguns at less than 20
feet, and .357 and .45 caliber handguns can cause extensive damage extending beyond the path of the projectile and should be explored
Stab wounds do not have this effect
Beware of the stab wound just over the clavicle -- the subclavian vein is at high risk
Слайд 18Stabilization/Airway
Established Airway
be prepared to obtain an airway emergently
intubation or cricothyrotomy
beware of cutting
the neck in the region of the hematoma -- disruption there of may lead to massive bleeding
must assume cervical spine injury until proven otherwise
Слайд 19Breathing
Zone I injuries with concomitant thoracic injuries
pneumothorax
hemopneumothorax
tension pneumothorax
Слайд 20Circulation
Bleeding should be controlled by pressure
Do not clamp blindly or probe the
wound depths
The absence of visible hemorrhage does not rule out
Two large bore IVs
Careful of IV in arm unilateral to subclavian injury
Слайд 21History
Obtain from EMS witnesses, patient
Mechanisms of injury - stab wounds, gunshot wound,
high-energy, low-energy, trajectory of stab
Estimate of blood loss at scene
Any associated thoracic, abdominal, extremity injuries
Neurologic history
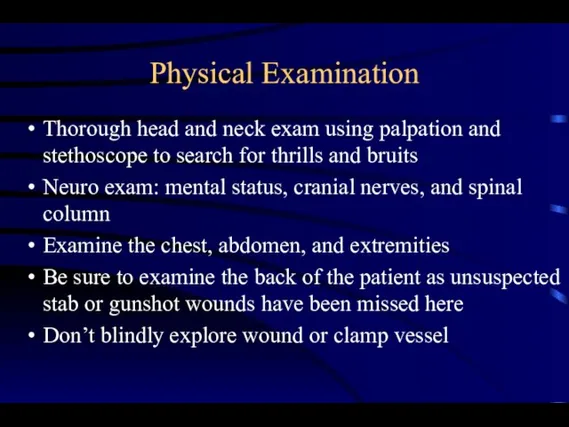
Слайд 22Physical Examination
Thorough head and neck exam using palpation and stethoscope to search
for thrills and bruits
Neuro exam: mental status, cranial nerves, and spinal column
Examine the chest, abdomen, and extremities
Be sure to examine the back of the patient as unsuspected stab or gunshot wounds have been missed here
Don’t blindly explore wound or clamp vessel
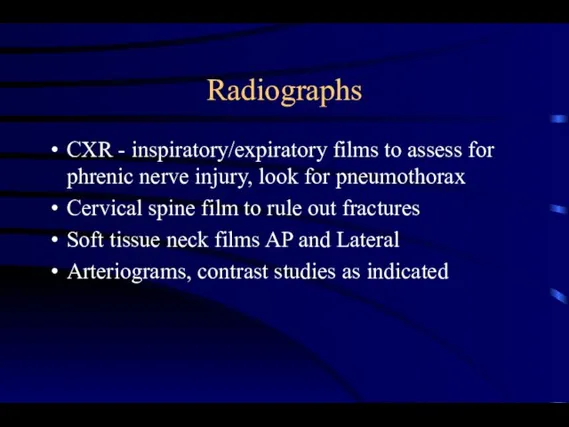
Слайд 23Radiographs
CXR - inspiratory/expiratory films to assess for phrenic nerve injury, look for
pneumothorax
Cervical spine film to rule out fractures
Soft tissue neck films AP and Lateral
Arteriograms, contrast studies as indicated
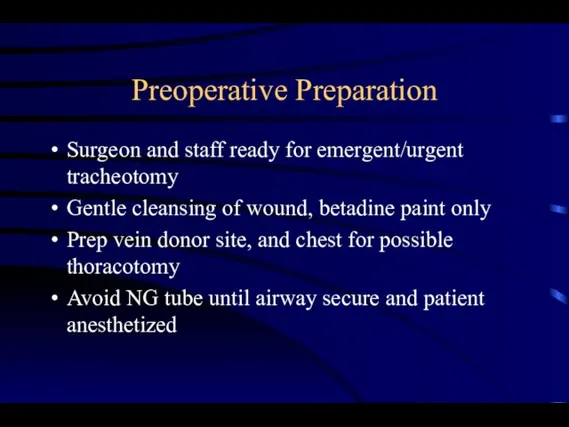
Слайд 24Preoperative Preparation
Surgeon and staff ready for emergent/urgent tracheotomy
Gentle cleansing of wound, betadine
paint only
Prep vein donor site, and chest for possible thoracotomy
Avoid NG tube until airway secure and patient anesthetized
Слайд 25
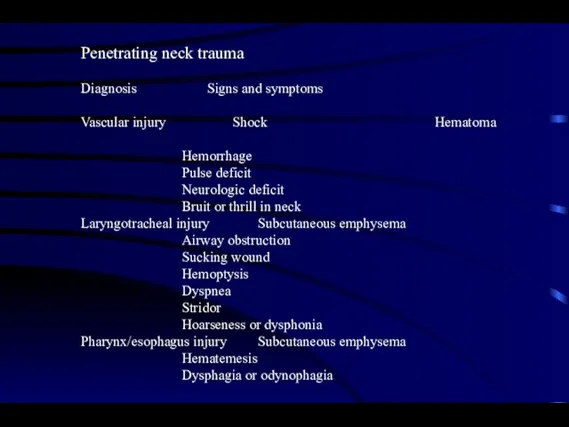
Penetrating neck trauma
Diagnosis Signs and symptoms
Vascular injury Shock Hematoma
Hemorrhage
Pulse deficit
Neurologic
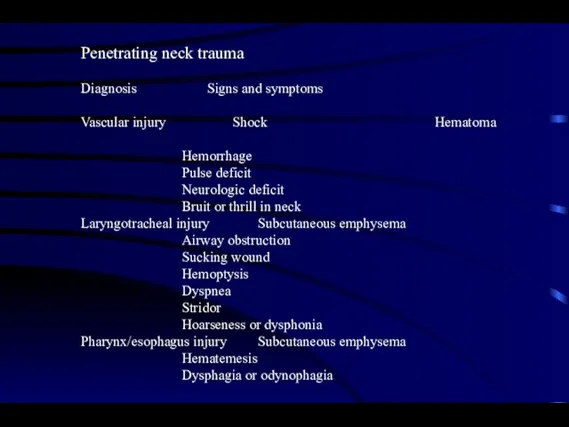
deficit
Bruit or thrill in neck
Laryngotracheal injury Subcutaneous emphysema
Airway obstruction
Sucking wound
Hemoptysis
Dyspnea
Stridor
Hoarseness or dysphonia
Pharynx/esophagus injury Subcutaneous emphysema
Hematemesis
Dysphagia or odynophagia
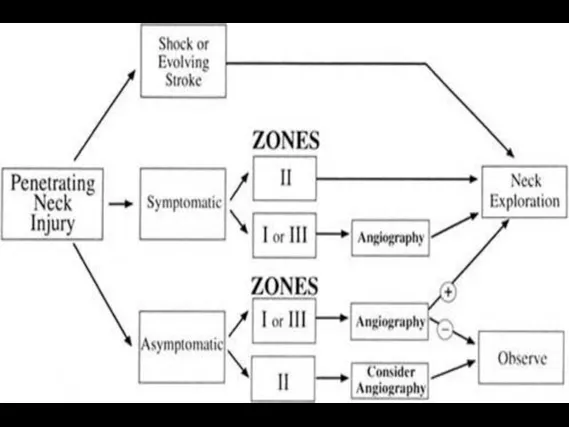
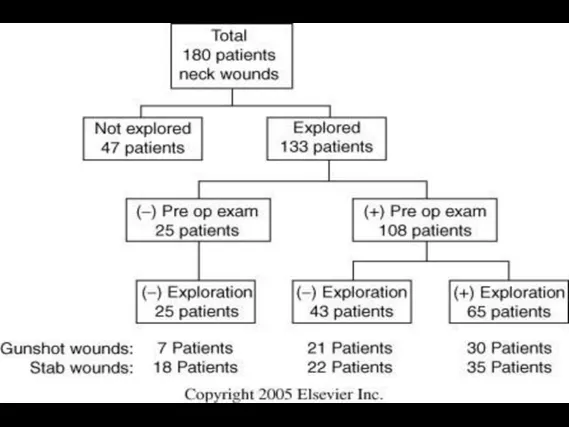
Слайд 26Exploration vs. Observation
Many experts have adopted a policy of selective exploration
Decreased number
of negative explorations, increased number of positive explorations
Decreased cost of medical care, maybe
No increase in mortality when adjunctive diagnostic studies and serial exams performed
Patients taken to OR if clinical exam changes, around 2% in most studies
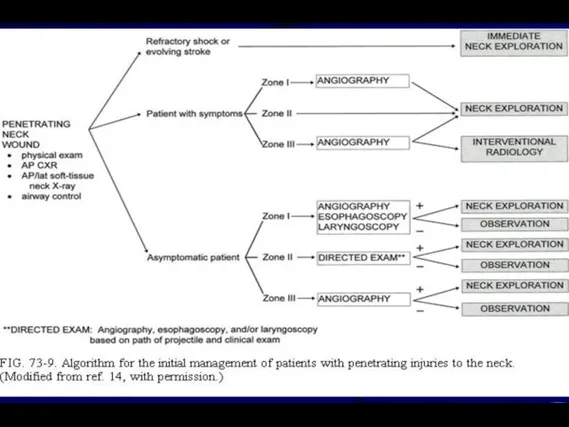
Слайд 29Site/Zone I
Adequate exposure for exploration and repair may require sternotomy, clavicle resection,
or thoracotomy
High morbidity of exploration, thus suspicion must be great before taking the patient to OR
Cardiothoracic surgery consultation a must
Angiography is essential
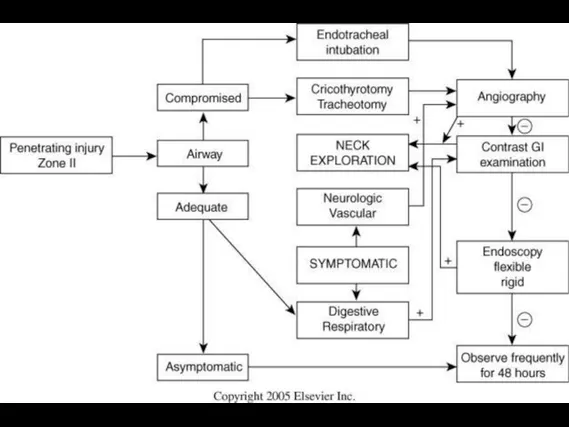
Слайд 30Site/Zone II
Few injuries will escape clinical examination
Most carotid injuries occur here
Adjunctive
studies, except barium swallow and esophagoscopy where indicated, are not necessary
Symptomatic zone II injuries can generally be safely managed by observation
Слайд 31Site/Zone III
High rate of vascular injury, often multiple
Often difficult to obtain proximal
and distal vessel control
Exploration has high rate of injury to cranial nerves
Adequate exposure may require mandibular subluxation or mandibulotomy
Angiography needed to delineate site of injury
Embolization techniques of greatest value here
Слайд 32Clinical Setting
Observation requires admission to an intensive care unit where serial examination
can be performed by a surgeon
Adjunctive studies must be available at all times and at a moments notice
Absence of these dictates exploration of all patients - such as in a rural setting
Слайд 33Pharyngo Esophageal
Gastrografin swallow followed by Barium if negative
Flexible ± rigid esophagoscopy
Invert the
mucosal edges and close with two layers of absorable sutures
JP drain and muscle flap
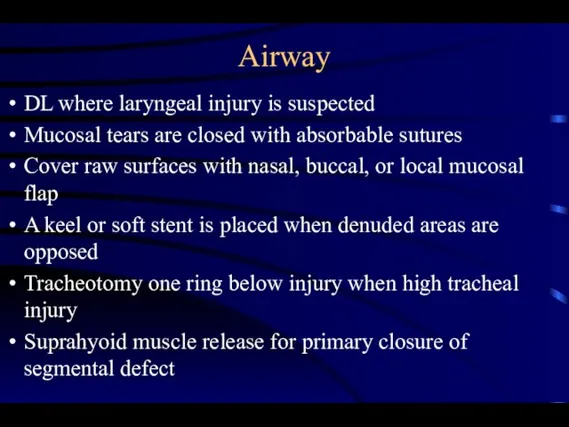
Слайд 35Airway
DL where laryngeal injury is suspected
Mucosal tears are closed with absorbable sutures
Cover raw surfaces with nasal, buccal, or local mucosal flap
A keel or soft stent is placed when denuded areas are opposed
Tracheotomy one ring below injury when high tracheal injury
Suprahyoid muscle release for primary closure of segmental defect
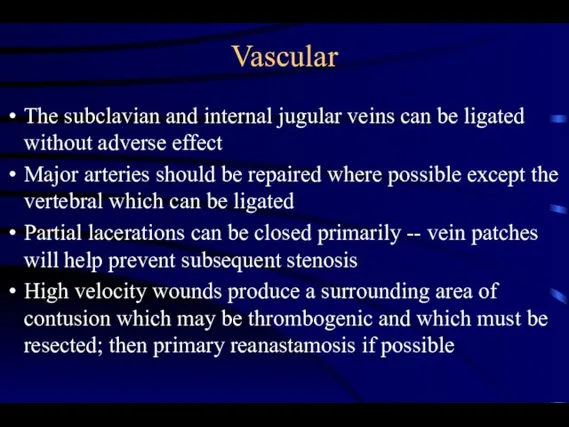
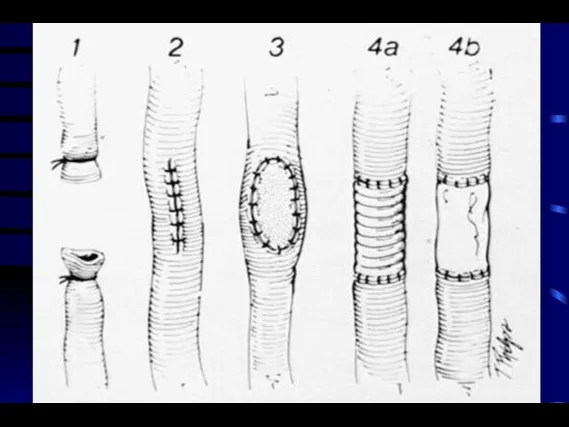
Слайд 36Vascular
The subclavian and internal jugular veins can be ligated without adverse effect
Major
arteries should be repaired where possible except the vertebral which can be ligated
Partial lacerations can be closed primarily -- vein patches will help prevent subsequent stenosis
High velocity wounds produce a surrounding area of contusion which may be thrombogenic and which must be resected; then primary reanastamosis if possible
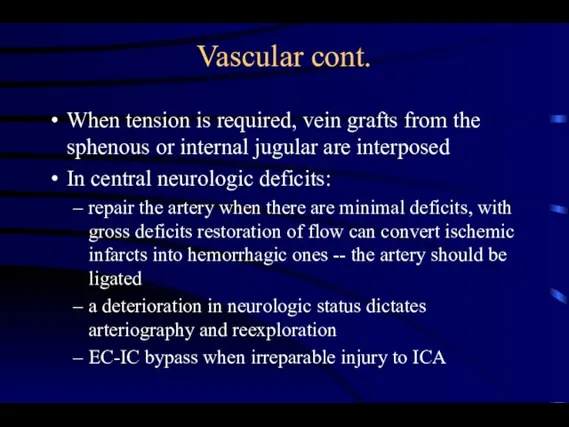
Слайд 39Vascular cont.
When tension is required, vein grafts from the sphenous or internal
jugular are interposed
In central neurologic deficits:
repair the artery when there are minimal deficits, with gross deficits restoration of flow can convert ischemic infarcts into hemorrhagic ones -- the artery should be ligated
a deterioration in neurologic status dictates arteriography and reexploration
EC-IC bypass when irreparable injury to ICA
Слайд 41Conclusions
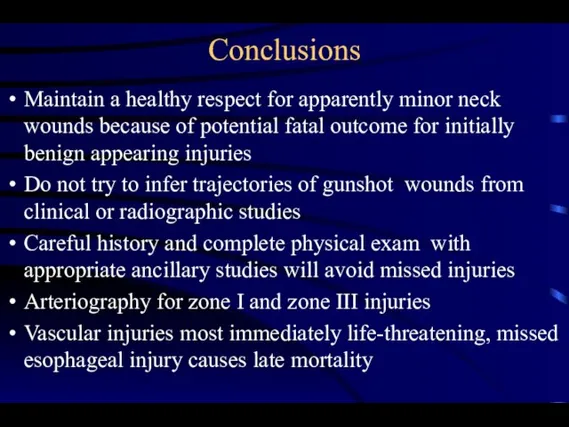
Maintain a healthy respect for apparently minor neck wounds because of potential
fatal outcome for initially benign appearing injuries
Do not try to infer trajectories of gunshot wounds from clinical or radiographic studies
Careful history and complete physical exam with appropriate ancillary studies will avoid missed injuries
Arteriography for zone I and zone III injuries
Vascular injuries most immediately life-threatening, missed esophageal injury causes late mortality

 Ароморфозы
Ароморфозы Презентация на тему Эволюция кровеносной системы хордовых
Презентация на тему Эволюция кровеносной системы хордовых ВТОРИЧНЫЙ ИММУННЫЙ ОТВЕТ. ПОСТВАКЦИНАЛЬНЫЙ ИММУННИТЕТ
ВТОРИЧНЫЙ ИММУННЫЙ ОТВЕТ. ПОСТВАКЦИНАЛЬНЫЙ ИММУННИТЕТ 중국어 PPT자료색갈수정본
중국어 PPT자료색갈수정본 Малоэтажный жилой комплекс Черничная поляна – Ленинградская область, деревня Юкки. Застройщик – ООО АйЭмДэ групп
Малоэтажный жилой комплекс Черничная поляна – Ленинградская область, деревня Юкки. Застройщик – ООО АйЭмДэ групп Большая перемена. Больше, чем просто конкурс
Большая перемена. Больше, чем просто конкурс Презентация на тему Земляника лесная
Презентация на тему Земляника лесная Почему китайцы кушают палочками?
Почему китайцы кушают палочками? Атеросклероз
Атеросклероз Автоматизированные высотные склады штучных грузов
Автоматизированные высотные склады штучных грузов «Лягушка-путешественница»
«Лягушка-путешественница» Оформление слайдов
Оформление слайдов Разработка, оформление и приемка электронных образовательных ресурсов в рамках инновационной образовательной программы
Разработка, оформление и приемка электронных образовательных ресурсов в рамках инновационной образовательной программы Запуск первого искусственного спутника Земли
Запуск первого искусственного спутника Земли История преподавания психологии в средней школе
История преподавания психологии в средней школе Урок правовых знаний
Урок правовых знаний Л.Н. Толстой. Косточка. А.П.Гайдар. Совесть
Л.Н. Толстой. Косточка. А.П.Гайдар. Совесть Презентация на тему Боги Древнего Египта
Презентация на тему Боги Древнего Египта  Политическая система общества
Политическая система общества Презентация на тему Выдающиеся личности в истории Кубани
Презентация на тему Выдающиеся личности в истории Кубани  Производство обжаренного кофе «Кофе Хауз»
Производство обжаренного кофе «Кофе Хауз» Школьное методическое объединение учителей русского языка и литературы
Школьное методическое объединение учителей русского языка и литературы Love&Faith. Письма о любви
Love&Faith. Письма о любви Неопределенный интеграл
Неопределенный интеграл Курс лекций Плодородие
Курс лекций Плодородие Сланцевый газ: революция или эволюция?
Сланцевый газ: революция или эволюция? Ты о пожаре услыхал,Скорей об этом дай сигнал –Смело трубку в руку взять,«01» сумей набрать
Ты о пожаре услыхал,Скорей об этом дай сигнал –Смело трубку в руку взять,«01» сумей набрать Мелодекламация - соединение выразительного произнесения текста и музыки
Мелодекламация - соединение выразительного произнесения текста и музыки