Содержание
- 2. Key points of the lecture Graves' disease: definition, history, causes, symptoms and signs, taking diagnosis and
- 3. The main thyroid and parathyroid disorders include: Graves' disease Hypothyroidism Hashimoto’s thyroiditis Hypoparathyroidism
- 4. Graves' disease Graves' disease is an autoimmune disease of a thyroid. It most commonly affects the
- 5. History Graves' disease owes its name to the Irish doctor Robert James Graves, who described a
- 6. Epidemiology and causes Graves' disease affects up to 2% of the female population, sometimes appears after
- 7. Pathophysiology There appears to be a genetic predisposition for Graves' disease. Graves' disease is an autoimmune
- 8. Exophthalmos It`s protrusion of the eyeball from the orbit, caused by disease, especially hyperthyroidism, or injury.
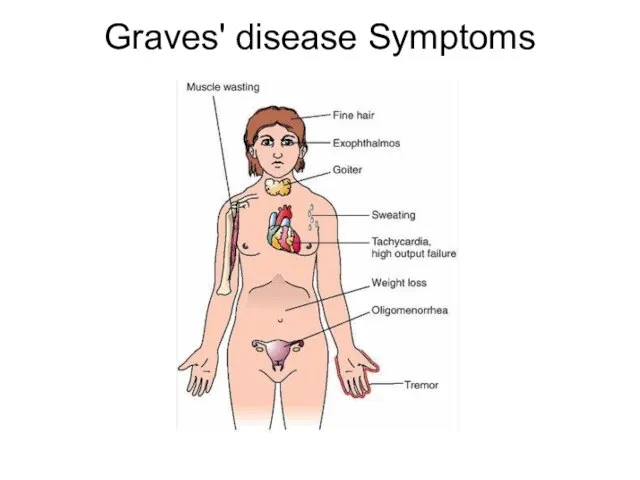
- 9. Classical clinical features (triad) of Graves' disease Goiter is an enlarged thyroid gland and is of
- 10. Other main symptoms and signs Fatigue Weight loss with increased appetite Muscle weakness Non-pitting edema (pretibial
- 11. Graves' disease Symptoms
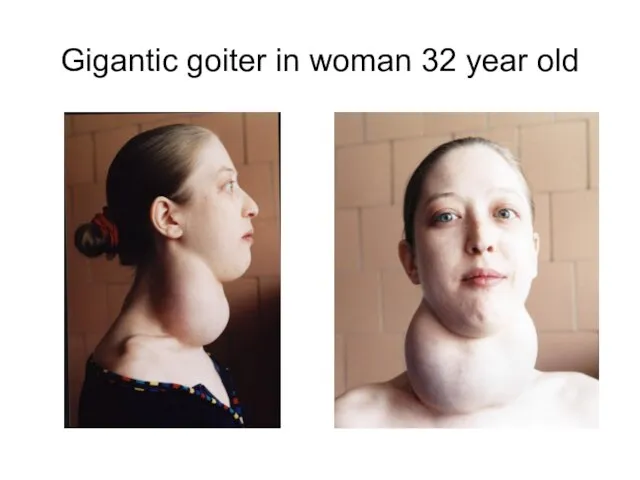
- 12. Gigantic goiter in woman 32 year old
- 13. Graves' ophthalmopathy Thyroid-associated ophthalmopathy is one of the most typical symptoms of Graves' disease. The ocular
- 14. Diagnosis Another sign of Graves' disease is hyperthyroidism – overproduction of the thyroid hormones T3 and
- 15. Treatment Treatment of Graves' disease includes antithyroid drugs which reduce the production of thyroid hormone, radioiodine
- 16. Antithyroid drugs The main antithyroid drugs are carbimazole (in the UK), methimazole (in the US), and
- 17. Radioiodine Radioiodine (radioactive iodine-131) was developed in the early 1940s at the Mallinckrodt General Clinical Research
- 18. Surgery This modality is suitable for young patients and pregnant patients. Indications are: a large goitre
- 19. Hypothyroidism Hypothyroidism is the disease state in humans and in vertebrates caused by insufficient production of
- 20. Causes Iodine deficiency is the most common cause of hypothyroidism worldwide. In iodine-replete individuals hypothyroidism is
- 21. Early symptoms and signs in adults Poor muscle tone (muscle hypotonia) Fatigue Cold intolerance, increased sensitivity
- 22. Late symptoms Slow speech and a hoarse, breaking voice – deepening of the voice can also
- 23. Diagnostic testing To diagnose primary hypothyroidism, many doctors simply measure the amount of thyroid-stimulating hormone (TSH)
- 24. Hashimoto's thyroiditis Hashimoto's thyroiditis is an autoimmune disease in which the thyroid gland is gradually destroyed
- 25. Epidemiology This disorder is believed to be the most common cause of primary hypothyroidism in North
- 26. Causes The family history of thyroid disorders is common, with the HLA-DR5 gene most strongly implicated
- 27. Hashimoto’s thyroiditis histology Physiologically, antibodies against thyroid peroxidase and/or thyroglobulin cause gradual destruction of follicles in
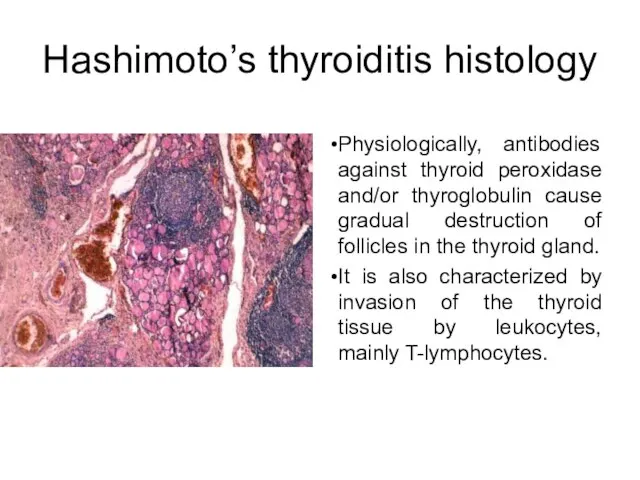
- 28. Symptoms and signs Symptoms of Hashimoto's thyroiditis include weight gain, depression, mania, sensitivity to heat and
- 29. Treatment Hypothyroidism caused by Hashimoto's Thyroiditis is treated with thyroid hormone replacement agents such as levothyroxine
- 30. Hypoparathyroidism In medicine (endocrinology), hypoparathyroidism is decreased function of the parathyroid glands, leading to decreased levels
- 31. Causes of the hypoparathyroidism Removal of or trauma to the parathyroid glands in thyroid surgery (thyroidectomy)
- 32. Signs and symptoms Tingling lips, fingers, and toes Muscle cramps Pain in the face, legs, and
- 33. Additional symptoms that may be associated with this disease include Painful menstruation Hand or foot spasms
- 34. Diagnosis Diagnosis is by measurement of calcium, serum albumin (for correction) and PTH in blood. PTH
- 35. Treatment Severe hypocalcemia, a potentially life-threatening condition, is treated as soon as possible with intravenous calcium
- 36. First aid In the event of a life-threatening attack of low calcium levels or tetany (prolonged
- 38. Скачать презентацию
 Волейбол. Правила, техника и тактика игры
Волейбол. Правила, техника и тактика игры Разделение власти по Локку. Разделение власти по Монтескье
Разделение власти по Локку. Разделение власти по Монтескье Тренерские услуги. Спортзал Атлант
Тренерские услуги. Спортзал Атлант Магистерская программа Управление проектами. Псковский государственный университет
Магистерская программа Управление проектами. Псковский государственный университет Системы записи телефонных переговоров Спрут 7
Системы записи телефонных переговоров Спрут 7 Условный Студент
Условный Студент Природные комплексы Северного Кавказа
Природные комплексы Северного Кавказа Урок китайского языка 多少钱一个
Урок китайского языка 多少钱一个 Российский канцелярский форум
Российский канцелярский форум Презентация на тему Мастера русского авангарда
Презентация на тему Мастера русского авангарда Информационно-методические материалы к семинару «Новое в ценообразовании на рынке электроэнергии. Особенности расчетов за эле
Информационно-методические материалы к семинару «Новое в ценообразовании на рынке электроэнергии. Особенности расчетов за эле Краткая инструкция для студентов по питч-сессии
Краткая инструкция для студентов по питч-сессии ЕСЛИ УЧЕНИК В ШКОЛЕ НЕ НАУЧИТСЯ САМ ТВОРИТЬ, ТО И В ЖИЗНИ ОН ВСЕГДА БУДЕТ ТОЛЬКО ПОДРАЖАТЬ, КОПИРОВАТЬ. Л.Н. Толстой
ЕСЛИ УЧЕНИК В ШКОЛЕ НЕ НАУЧИТСЯ САМ ТВОРИТЬ, ТО И В ЖИЗНИ ОН ВСЕГДА БУДЕТ ТОЛЬКО ПОДРАЖАТЬ, КОПИРОВАТЬ. Л.Н. Толстой Строение растительной клетки на примере клеток кожицы чешуи лука
Строение растительной клетки на примере клеток кожицы чешуи лука Symbols of the USA
Symbols of the USA Ya__LIChNOST
Ya__LIChNOST Мир новых возможностей
Мир новых возможностей ОПРЕДЕЛИТЕЛИ И ИХ ПРИМЕНЕНИЯ
ОПРЕДЕЛИТЕЛИ И ИХ ПРИМЕНЕНИЯ Зима поёт зима, аукает
Зима поёт зима, аукает ИНДИВИДУАЛЬНАЯ образовательная ПРОГРАММА
ИНДИВИДУАЛЬНАЯ образовательная ПРОГРАММА Transport
Transport Критерии и показатели, связанные с ИКТ, ЭОР и ИОС
Критерии и показатели, связанные с ИКТ, ЭОР и ИОС Табличное умножение и деление
Табличное умножение и деление Балки. Общие положения
Балки. Общие положения Теория преступности Чезаре Ломброзо
Теория преступности Чезаре Ломброзо Природа Черноморского побережья Кавказа (4 класс)
Природа Черноморского побережья Кавказа (4 класс) ОБЩЕСТВО
ОБЩЕСТВО urok_6 (1)
urok_6 (1)