Содержание
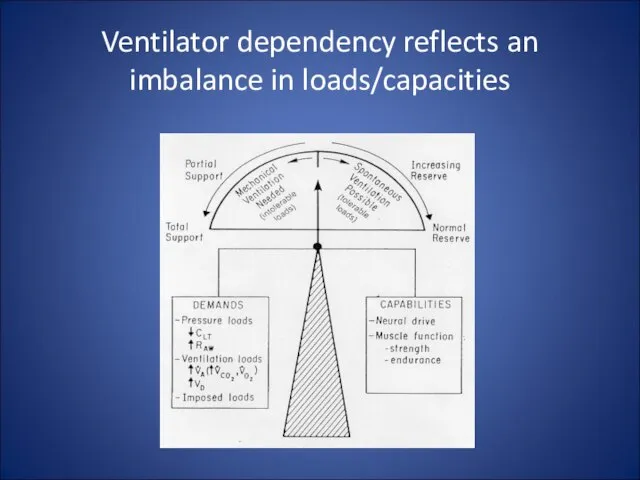
- 2. Ventilator dependency reflects an imbalance in loads/capacities
- 3. Ventilator dependency can also be iatrogenic Failure to recognize discontinuation potential Imposed loading: insufficient support insensitive/unresponsive
- 4. The Ventilator Discontinuation Process - EBM Projects AHCPR - McMaster comprehensive evidence based review 5000 papers
- 5. The Ventilator Discontinuation Process - EBM Projects ACCP/SCCM/AARC Task Force Organized May 1999 Used McMaster report
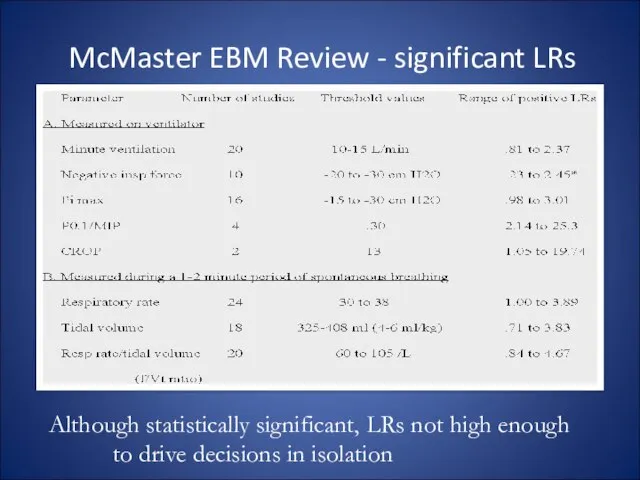
- 6. McMaster EBM Review - significant LRs Although statistically significant, LRs not high enough to drive decisions
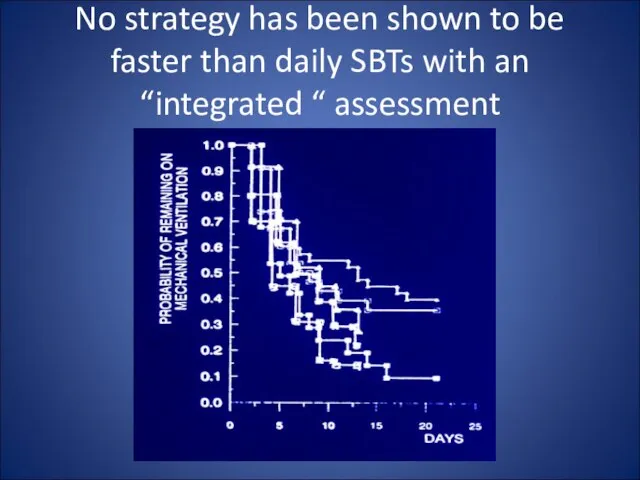
- 7. No strategy has been shown to be faster than daily SBTs with an “integrated “ assessment
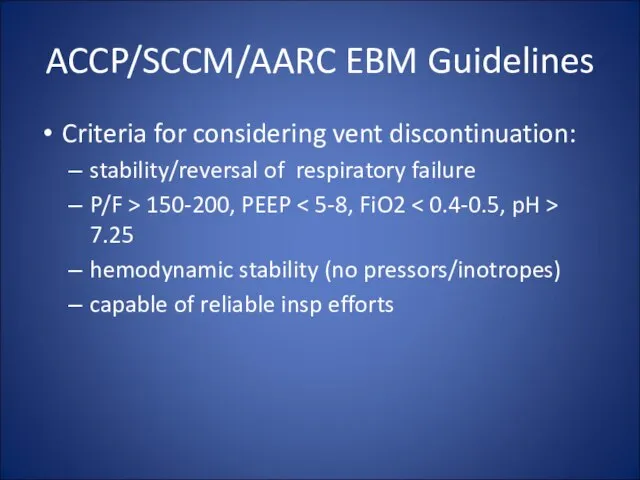
- 8. ACCP/SCCM/AARC EBM Guidelines Criteria for considering vent discontinuation: stability/reversal of respiratory failure P/F > 150-200, PEEP
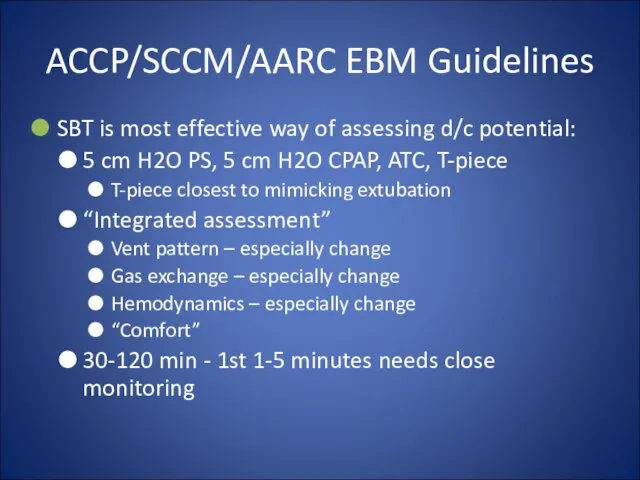
- 9. ACCP/SCCM/AARC EBM Guidelines SBT is most effective way of assessing d/c potential: 5 cm H2O PS,
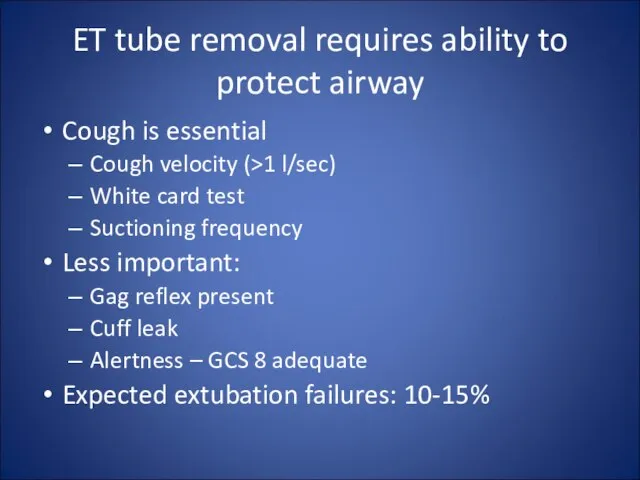
- 10. ET tube removal requires ability to protect airway Cough is essential Cough velocity (>1 l/sec) White
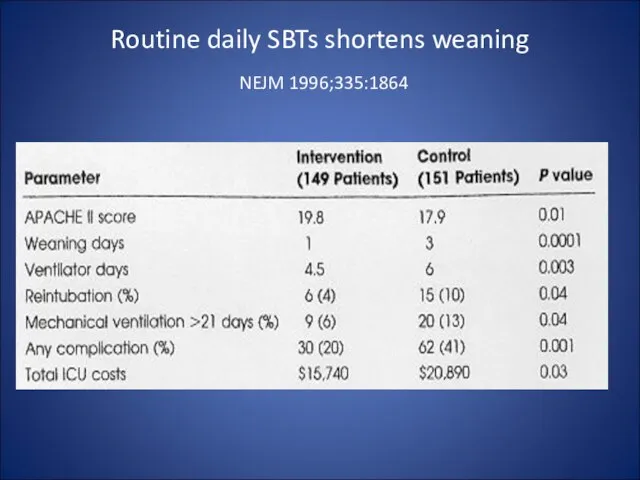
- 11. Routine daily SBTs shortens weaning NEJM 1996;335:1864
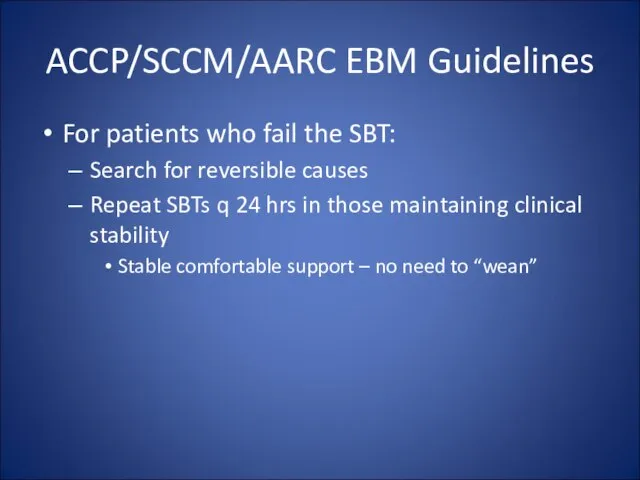
- 12. ACCP/SCCM/AARC EBM Guidelines For patients who fail the SBT: Search for reversible causes
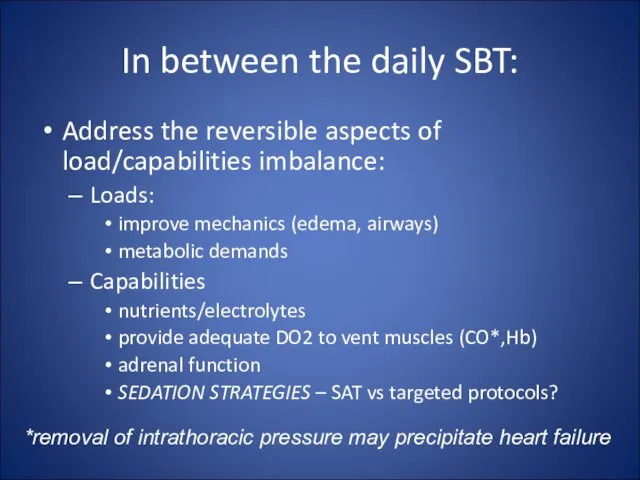
- 13. In between the daily SBT: Address the reversible aspects of load/capabilities imbalance: Loads: improve mechanics (edema,
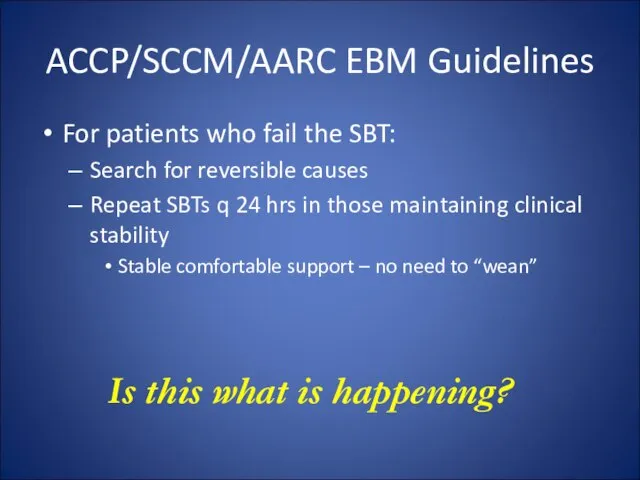
- 14. ACCP/SCCM/AARC EBM Guidelines For patients who fail the SBT: Search for reversible causes Repeat SBTs q
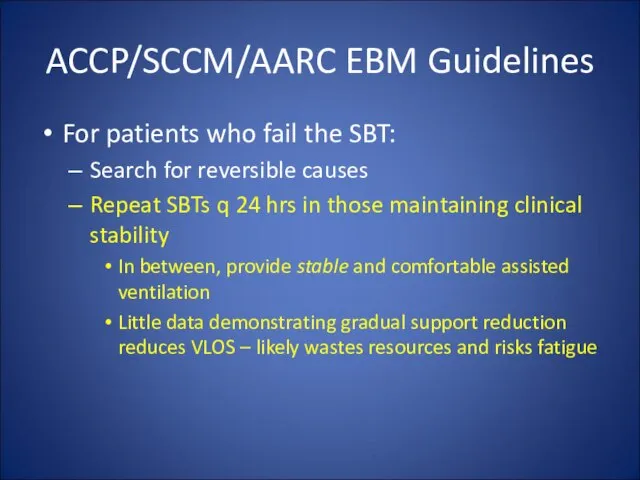
- 15. In between daily SBTs Properly load the muscles: “Normalize” amount of load avoid atrophy, avoid fatigue
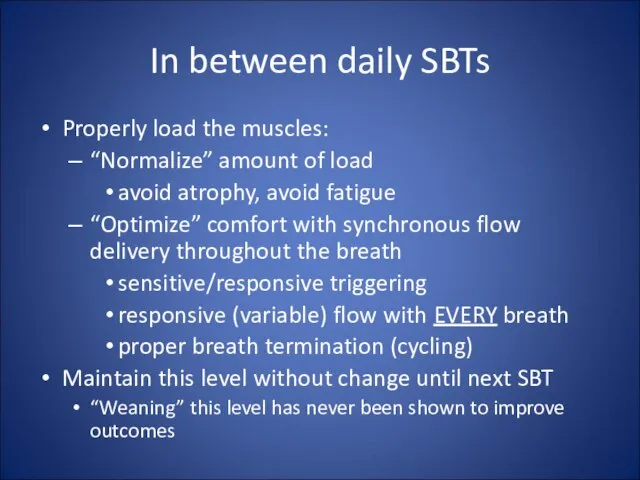
- 16. Practical aspects of “normalized”, comfortable loading Triggering - max sensitivity, “balance” PEEPi with applied PEEP Pressure/flow
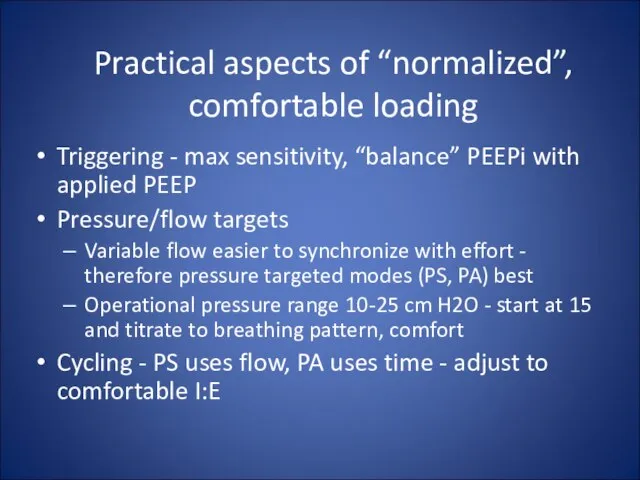
- 17. Newer approaches to improving synchrony Proportional assist ventilation Pressure and flow driven by sensed pt flow
- 18. ACCP/SCCM/AARC EBM Guidelines For patients who fail the SBT: Search for reversible causes Repeat SBTs q
- 19. ACCP/SCCM/AARC EBM Guidelines For patients who fail the SBT: Search for reversible causes Repeat SBTs q
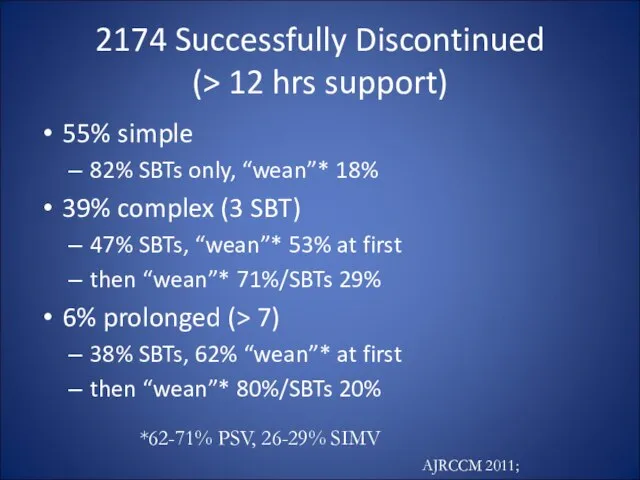
- 20. 2174 Successfully Discontinued (> 12 hrs support) 55% simple 82% SBTs only, “wean”* 18% 39% complex
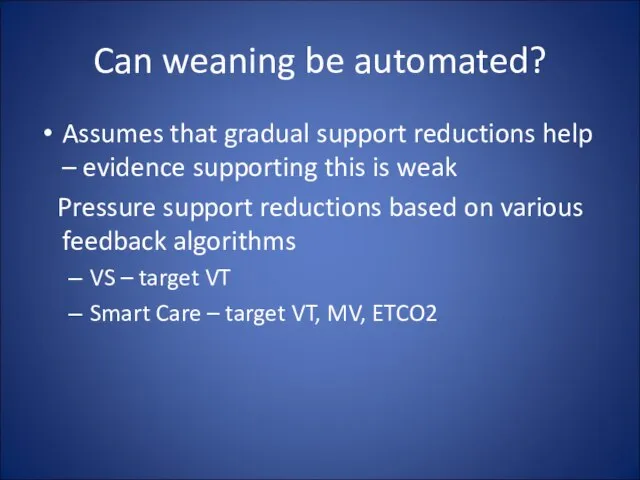
- 21. Can weaning be automated? Assumes that gradual support reductions help – evidence supporting this is weak
- 22. Volume Support (VS, ASV) Adjusts pressure to targeted tidal volume In theory: As patient recovers, bigger
- 23. Lellouche, AJRCCM 2006; 174: 894 SmartCare I
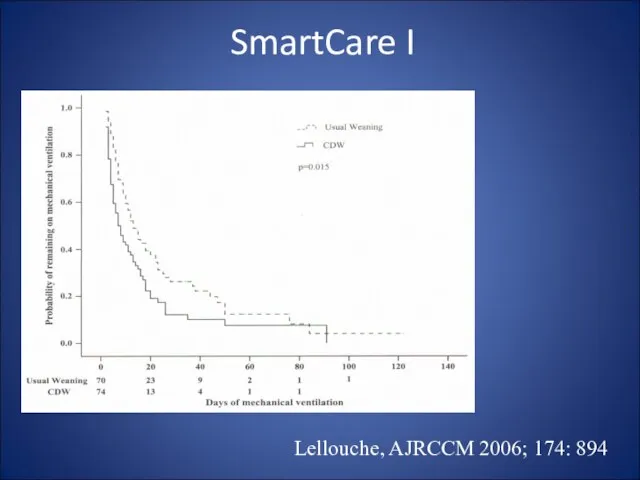
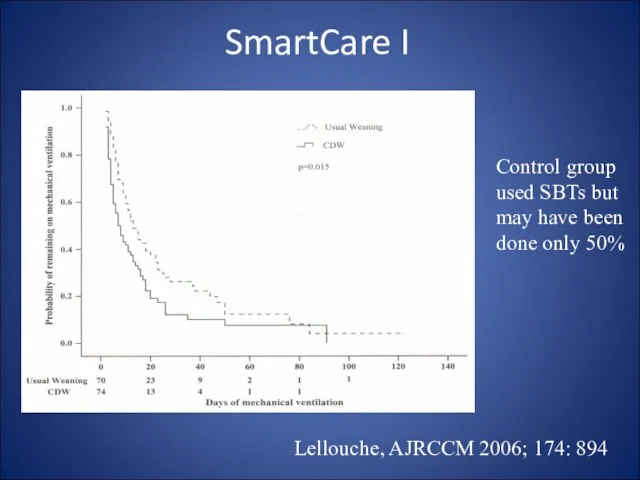
- 24. Lellouche, AJRCCM 2006; 174: 894 Control group used SBTs but may have been done only 50%
- 25. Int Care Med 2008;34:1788 SmartCare II
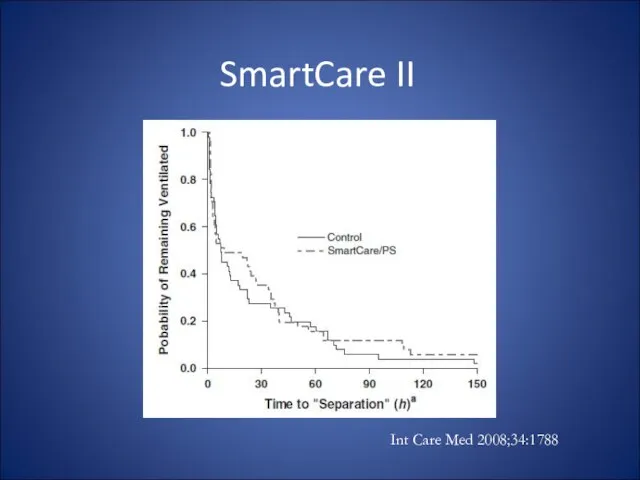
- 26. So is there a role for automatic PS reductions? No evidence that says this facilitates muscle
- 28. NIV and Vent Discontinuation: Two Scenarios The failed/borderline SBT but good airway protection Supportive evidence, especially
- 30. Скачать презентацию

 УАТТ ДЖЕЙМС (1736–1819)
УАТТ ДЖЕЙМС (1736–1819) Физика 7
Физика 7 Разработка проектной идеи образовательного ресурса. №3
Разработка проектной идеи образовательного ресурса. №3 Хумус Бар
Хумус Бар Лекция 7
Лекция 7 Презентация на тему Гаршин сказка о жабе и розе
Презентация на тему Гаршин сказка о жабе и розе  Презентация на тему Белки
Презентация на тему Белки Презентация на тему Применение жиров
Презентация на тему Применение жиров  Первомайская центральная районная детская библиотека
Первомайская центральная районная детская библиотека Чудо Земли - хлеб
Чудо Земли - хлеб Бытовой жанр в русской живописи конца ХVIII в. - первой половины ХIХ в
Бытовой жанр в русской живописи конца ХVIII в. - первой половины ХIХ в Выставка работ
Выставка работ Отчет о проделанной работе с резидентами по дисциплине Клиническая фармакология, 2019-2021 годы обучения
Отчет о проделанной работе с резидентами по дисциплине Клиническая фармакология, 2019-2021 годы обучения 孔子学院在乌克兰和俄罗斯
孔子学院在乌克兰和俄罗斯 Презентация на тему Саудовская Аравия
Презентация на тему Саудовская Аравия  Методические рекомендации к заполнению классного журнала в государственном образовательном учреждении общего образования
Методические рекомендации к заполнению классного журнала в государственном образовательном учреждении общего образования Представление нечисловой информации
Представление нечисловой информации Дед Мороз на новогодних открытках
Дед Мороз на новогодних открытках Разветвляющийся алгоритм
Разветвляющийся алгоритм Пролог к изучению поэмы Н.В. Гоголя «Мертвые души»
Пролог к изучению поэмы Н.В. Гоголя «Мертвые души» Познавательные процессы (память)
Познавательные процессы (память) Диспансеризация сельскохозяйственных животных при внутренних болезнях
Диспансеризация сельскохозяйственных животных при внутренних болезнях Инвестиционная деятельность предприятия
Инвестиционная деятельность предприятия «МОЯ СТРАНА – МОЯ РОССИЯ»
«МОЯ СТРАНА – МОЯ РОССИЯ» Любовная лирика Ф.И.Тютчева
Любовная лирика Ф.И.Тютчева Нестероидные противовоспалительные средства
Нестероидные противовоспалительные средства Почему болеют мои одноклассники
Почему болеют мои одноклассники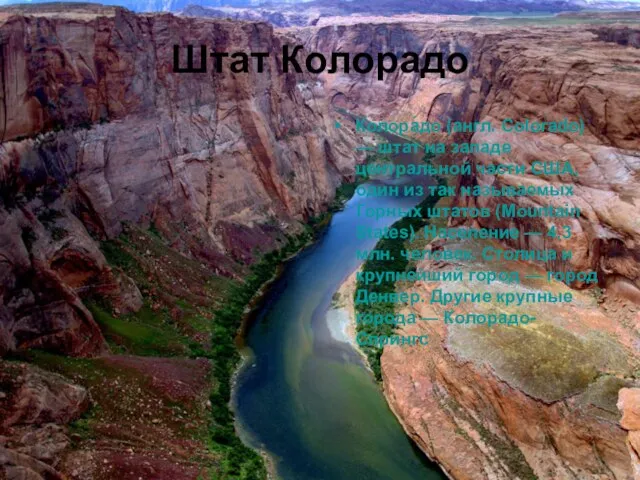 Штат Колорадо
Штат Колорадо