Слайд 2SOME GENERAL PRINCIPLES
Antibiotics can be naturally produced, semi-synthetic, or synthetic substances
Designed to
have as much selective toxicity on the bacteria as possible
This is more likely to be achieved compared to antimicrobials acting against eukaryotic cells (fungi, protozoa)
Слайд 3EXAMPLES OF SELECTIVE ACTION
Penicillin on bacterial cell wall (organisms without cell wall
won’t be inhibited eg Mycoplasma pneumoniae)
Sulphonamides prevent bacteria synthesising folic acid whereas humans can use preformed folate
Generally drugs acting on cell membranes or protein synthesis are more toxic to humans
Слайд 4ANTIBIOTICS ACTING ON CELL WALL OF BACTERIA
Beta lactams:
Penicillins, cephalosporins, carbapenems, monobactam
Glycopeptides:
Vancomycin, teicoplanin
Слайд 5THE IDEAL ANTIBIOTIC?:PENICILLIN
Narrow spectrum
Bactericidal
Very selective mode of action
Low serum protein binding
Widely distributed
in body esp. CNS
Excreted by the kidneys
Слайд 6THE DEVELOPMENT OF THE BETA LACTAMS
Benzylenicillin and early cephalosporins mainly active against
gram positive bacteria
(strep and staph)
Then “broad spectrum” penicillins appeared: ampicillin, ureidopenicillins and cephalosporins: cefuroxime, cefotaxime
Carbapenems and latest generation of cephalosporins, eg ceftazidime more active against gram negatives
Слайд 7BENZYLPENICILLIN: MAIN INDICATIONS
Strep pyogenes sepsis (from sore throat to fasciitis)
Pneumococcal pneumonia, meningitis
Meningococcal
meningitis, sepsis
Infective endocarditis (strep)
Strep group B sepsis
Diphtheria
Syphilis, leptospirosis
Слайд 8Broader spectrum penicillins
Ampicillin, amoxycillin cover most organisms hit by penicillin but also
Esch coli, some Proteus (cause UTI’s)
Augmentin stable to TEM1 beta lactamase because of the clavulanic acid therefore more active than ampicillin
Tazocin: broader coverage than augmentin against gram negatives including Pseudomonas
Слайд 9Organisms producing TEM1beta lactamase
Haemophilus influenzae
Neisseria gonorrhoeae
Bacteroides fragilis
Staph aureus
Esch coli
Слайд 10Carbapenems
Imipenem, meropenem: have a very broad spectrum activity against gram-negative bacteria, anaerobes,
streps
Now used to treat gram negative infections due to so called ESBL producing organisms eg, E coli, Klebsiella
Ertapenem is a new member of the group but its not active against Pseudomonas
Слайд 11PENICILLIN IS GENERALLY VERY SAFE BUT….
Allergic reactions not uncommon-rashes
Most severe reaction being
anaphylaxis
A history of anaphylaxis, urticaria, or rash immediately after penicillin indicates risk of immediate hypersensitivity after a further dose of any penicillin or cephalosporin (therefore these must be avoided)
Allergy is not dependent on the dose given ie, a small dose could cause anaphylaxis
Very high doses of penicillin can cause neurotoxicity
Never give penicillin intrathecally
Слайд 12What antibiotics can be used in penicillin allergy?
Macrolides: erythromycin, clarithromycin
(mainly gram positive
cover)
Quinolones: ciprofloxacin, levofloxacin (mainly gram positive cover)
Glycopeptides (serious infections)
Fusidic acid, rifampicin, clindamycin (mainly gram positive)
Слайд 13REMEMBER WHAT THE OTHER BETA LACTAMS ARE:
All penicillins: ampicillin, augmentin, piperacillin, cloxacillin
Cephalosporins:
cefuroxime, cefotaxime, ceftriaxone, ceftazidime (5-10% cross sensitivity)
Monobactam: aztreonam (low cross sensitivity)
Carbapenems: imipenem, meropenem
Слайд 14CLOXACILLIN
Narrow spectrum: Staph aureus (MSSA)
Stable to TEM1 beta lactamase
Similar antibiotics are methicillin,
nafcillin
Similar safety profile to benzylpenicillin
MRSA emerged in the early 1970’s (MecA gene encoding additional pbp)
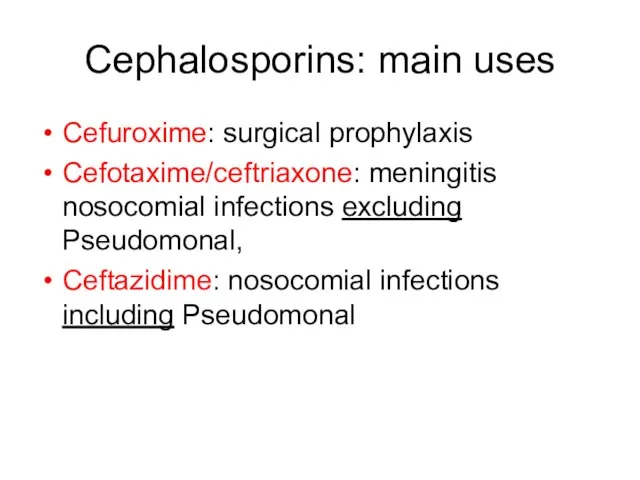
Слайд 15Cephalosporins: main uses
Cefuroxime: surgical prophylaxis
Cefotaxime/ceftriaxone: meningitis nosocomial infections excluding Pseudomonal,
Ceftazidime: nosocomial
infections including Pseudomonal
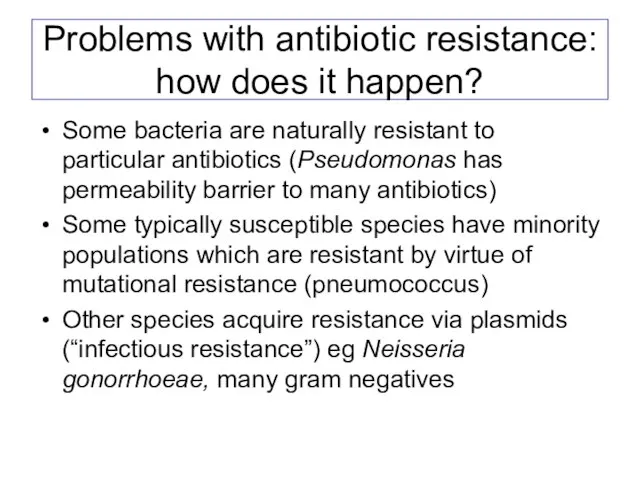
Слайд 16Problems with antibiotic resistance: how does it happen?
Some bacteria are naturally resistant
to particular antibiotics (Pseudomonas has permeability barrier to many antibiotics)
Some typically susceptible species have minority populations which are resistant by virtue of mutational resistance (pneumococcus)
Other species acquire resistance via plasmids (“infectious resistance”) eg Neisseria gonorrhoeae, many gram negatives
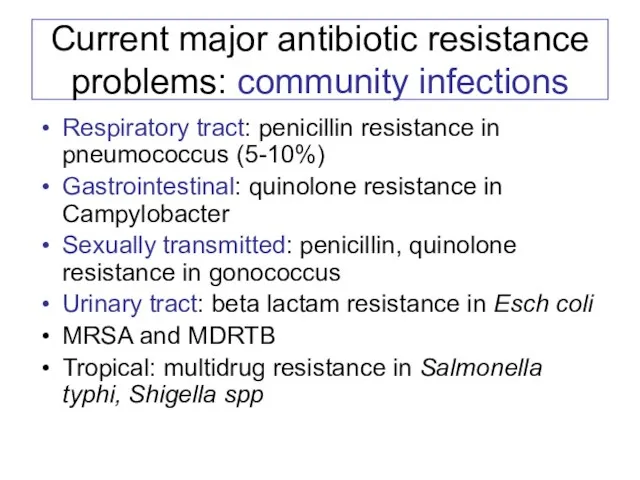
Слайд 17Current major antibiotic resistance problems: community infections
Respiratory tract: penicillin resistance in pneumococcus
(5-10%)
Gastrointestinal: quinolone resistance in Campylobacter
Sexually transmitted: penicillin, quinolone resistance in gonococcus
Urinary tract: beta lactam resistance in Esch coli
MRSA and MDRTB
Tropical: multidrug resistance in Salmonella typhi, Shigella spp
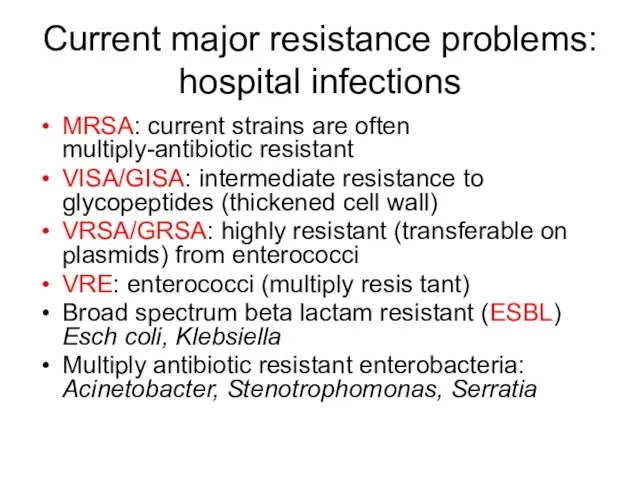
Слайд 18Current major resistance problems: hospital infections
MRSA: current strains are often multiply-antibiotic resistant
VISA/GISA:
intermediate resistance to glycopeptides (thickened cell wall)
VRSA/GRSA: highly resistant (transferable on plasmids) from enterococci
VRE: enterococci (multiply resis tant)
Broad spectrum beta lactam resistant (ESBL) Esch coli, Klebsiella
Multiply antibiotic resistant enterobacteria: Acinetobacter, Stenotrophomonas, Serratia
Слайд 19Other major antibiotic groups: aminoglycosides
Gentamicin, amikacin (tobramycin, streptomycin)
Mainly active against gram negative
bacteria
Mainly used to treat nosocomial infections: pneumonia in ITU, septicaemia
Limiting factors are nephrotoxicity (and ototoxicity) and resistance
Also used in combination
Слайд 20How we give aminoglycosides
For serious nosocomial infections: “extended interval” or once daily
dosing
5 or 7mg/kg for gentamicin (Hartford nomogram)
Rationale based on concentration- dependent killing and post-antibiotic effect
Reduced risk of nephrotoxicity
In infective endocarditis use lower doses to give synergy with penicillin
Слайд 21Some indications and limitations of particular antibiotics
Слайд 22Community acquired pneumonia
Pneumococcus (and H influenzae) are most likely: therefore ampicillin, amoxycillin
or augmentin
Severe pneumonia: cefotaxime
Severe atypical pneumonia (Legionella): macrolide or quinolone
Resistant pneumococcus: vancomycin or linezolid (new antibiotic!)
A new quinolone moxifloxacin covers most of these pathogens (likely to be used more in community)
Слайд 23Community acquired urinary infections
Ampicillin, amoxycillin, augmentin
Oral cephalosporin: cephradine
Trimethroprim
Nalidixic acid
Nitrofurantoin
Ciprofloxacin
Mecillinam
Слайд 24Skin and soft tissue infections
Cellulitis ? Streptococcal: penicillin or augmentin
Infected eczema ?
Staphylococccal/mixed: penicillin+flucloxacillin or augmentin
Necrotising fasciitis: penicillin+clindamycin
Septic arthritis: fluclox+fusidic acid
Gangrene: metronidazole
Слайд 25Where there is deep-seated infection: bone, abscess
Need an antibiotic with good tissue
and phagocyte penetration
Examples are rifampicin, clindamycin, fusidic acid, ciprofloxacin, metronidazole
So for treatment of Staph aureus osteomyelitis: flucloxacillin+ fusidic acid
Слайд 26Why do we use combination therapy?
When treating serious infection empirically we want
to cover a broad spectrum
(severe pneumonia:cefotaxime+erythromycin)
To prevent the emergence of drug resistance: tuberculosis regimens
For synergy: infective endocarditis (aminoglycoside)
For mixed infections eg, abdominal sepsis (tazocin+metronidazole)
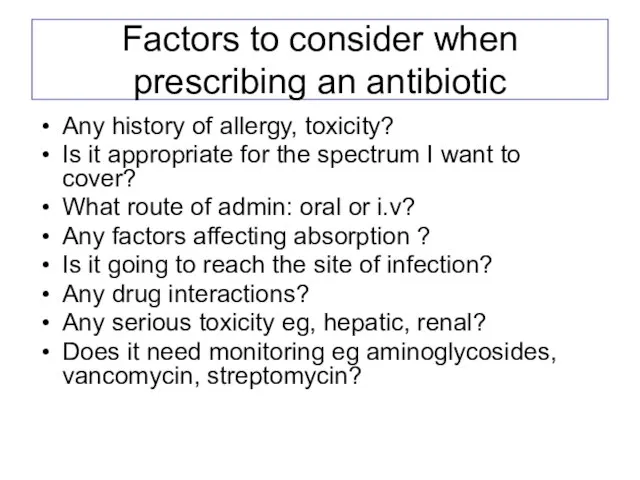
Слайд 27Factors to consider when prescribing an antibiotic
Any history of allergy, toxicity?
Is it
appropriate for the spectrum I want to cover?
What route of admin: oral or i.v?
Any factors affecting absorption ?
Is it going to reach the site of infection?
Any drug interactions?
Any serious toxicity eg, hepatic, renal?
Does it need monitoring eg aminoglycosides, vancomycin, streptomycin?
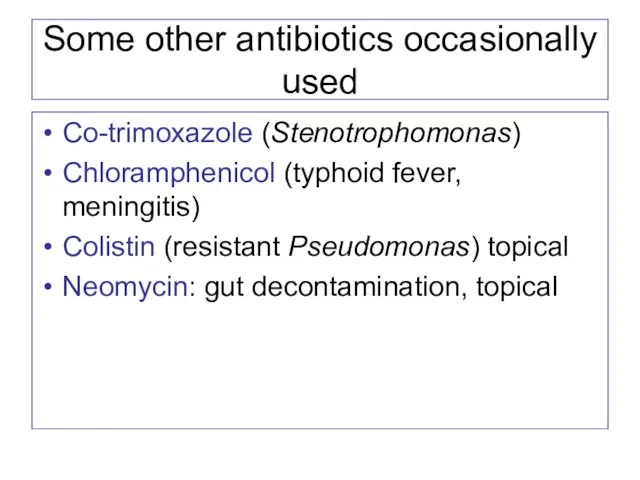
Слайд 28Some other antibiotics occasionally used
Co-trimoxazole (Stenotrophomonas)
Chloramphenicol (typhoid fever, meningitis)
Colistin (resistant Pseudomonas) topical
Neomycin:
gut decontamination, topical
 Батальный жанр в живописи
Батальный жанр в живописи Зан_5_Задание Форма
Зан_5_Задание Форма ПрезентацияМОУ Михайловская средняя (полная) общеобразовательная школа Подготовила заместитель директора по УВРКожевников
ПрезентацияМОУ Михайловская средняя (полная) общеобразовательная школа Подготовила заместитель директора по УВРКожевников Отчет о выверке данных по ИТ-оборудованию в системе Управление ИТ-активами. Шаблон презентации
Отчет о выверке данных по ИТ-оборудованию в системе Управление ИТ-активами. Шаблон презентации Конфликтология
Конфликтология Правовое государство
Правовое государство Фразеологизмы (6 класс)
Фразеологизмы (6 класс) РАЗВИТИЕ УСТНОЙ РЕЧИ УЧАЩИХСЯ с ТНР НА УРОКАХ литературы
РАЗВИТИЕ УСТНОЙ РЕЧИ УЧАЩИХСЯ с ТНР НА УРОКАХ литературы Центр изучения Северного ледовитого океана
Центр изучения Северного ледовитого океана портфолио студента системы СПО
портфолио студента системы СПО Динамика развития вузов России
Динамика развития вузов России Целебные капсулы Тяньши (1)
Целебные капсулы Тяньши (1) Тема: Социальный конфликт и пути его разрешения
Тема: Социальный конфликт и пути его разрешения С.В.Михалков «В снегу стояла елочка»
С.В.Михалков «В снегу стояла елочка» Исполнительный директор НИСКУ
Исполнительный директор НИСКУ Рекламная продукция. Wowspace dekor
Рекламная продукция. Wowspace dekor Мир эмоций
Мир эмоций МОДЕРНИЗАЦИЯ В РОССИИПредставленные предложения являются частными и не претендует на абсолютную истину. Но сам подход к осмысле
МОДЕРНИЗАЦИЯ В РОССИИПредставленные предложения являются частными и не претендует на абсолютную истину. Но сам подход к осмысле ЕГЭ ПО РУССКОМУ ЯЗЫКУ2011
ЕГЭ ПО РУССКОМУ ЯЗЫКУ2011 ЖУРНАЛЭкономическоеразвитие России Валовый Региональный Продукт
ЖУРНАЛЭкономическоеразвитие России Валовый Региональный Продукт  20170717_urok_30_kartochki_s_voprosami_dlya_3_gruppy
20170717_urok_30_kartochki_s_voprosami_dlya_3_gruppy Наш уголок СНТ Прогресс
Наш уголок СНТ Прогресс Тайна имени Кощея Бессмертного
Тайна имени Кощея Бессмертного Развитие кадрового потенциала системы образования
Развитие кадрового потенциала системы образования СТРАНЫ ВОСТОЧНОЙ АЗИИ. ЯПОНИЯ. КИТАЙ
СТРАНЫ ВОСТОЧНОЙ АЗИИ. ЯПОНИЯ. КИТАЙ Типы реакций
Типы реакций Население Евразии и политическая карта
Население Евразии и политическая карта Touchpoll AD & B Monitor
Touchpoll AD & B Monitor