Содержание
- 2. THE Guideline Global Initiative for Chronic Obstructive Lung Disease (GOLD), World Health Organization (WHO), National Heart,
- 3. Definition of COPD COPD is a preventable and treatable chronic lung disease characterized by airflow limitation
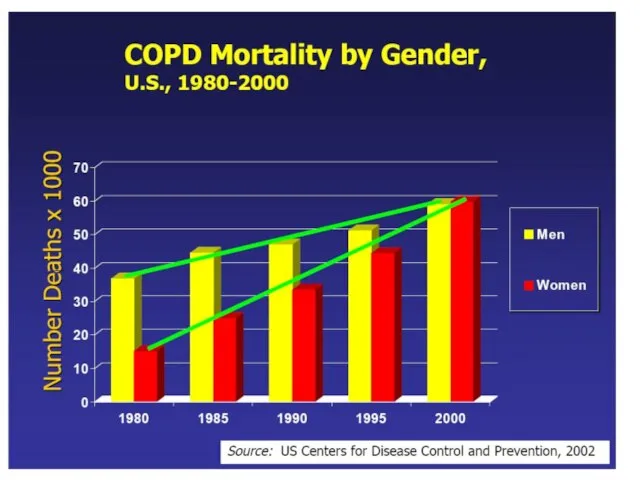
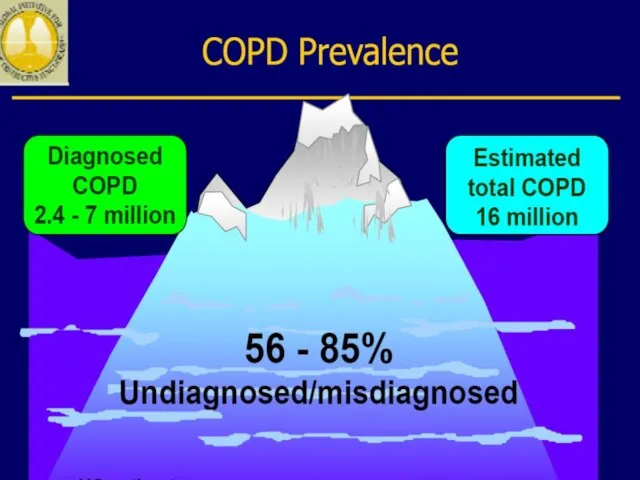
- 4. Epidemiology of COPD 4th leading cause of death in world 4th leading cause of death in
- 5. COPD includes: chronic bronchitis chronic bronchiolitis (small air way disease) Emphysema
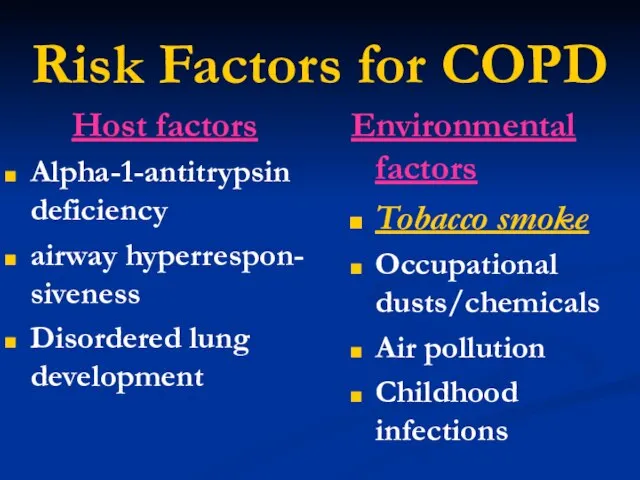
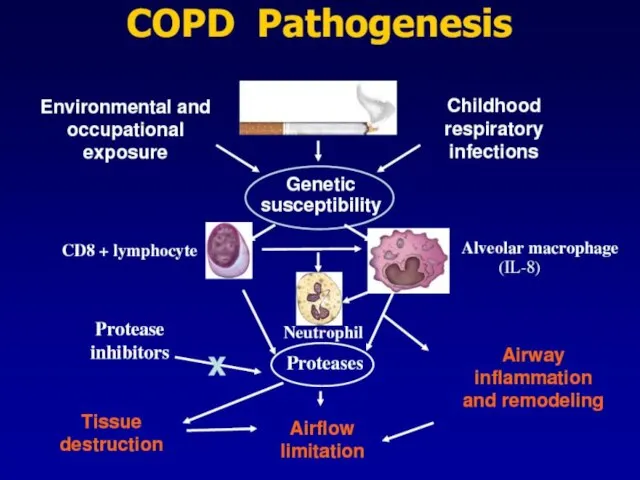
- 8. Risk Factors for COPD Host factors Alpha-1-antitrypsin deficiency airway hyperrespon- siveness Disordered lung development Environmental factors
- 10. Risk factors cigarette smoking remains the most important. Susceptibility to cigarette smoke varies but both the
- 11. Alpha-1-antitrypsin deficiency α1-Antitrypsin is a proteinase inhibitor which is produced in the liver, secreted into the
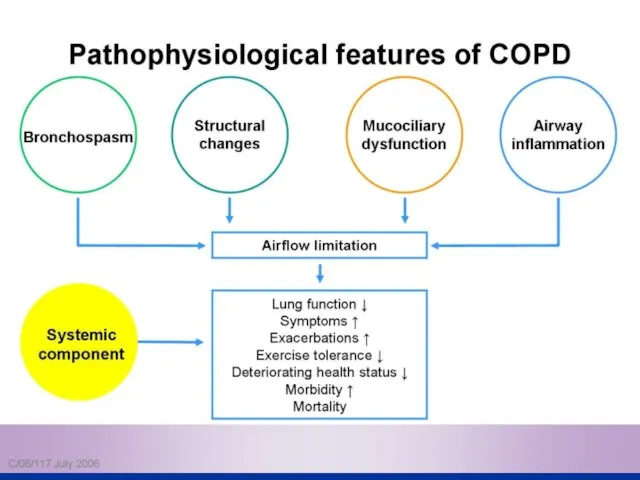
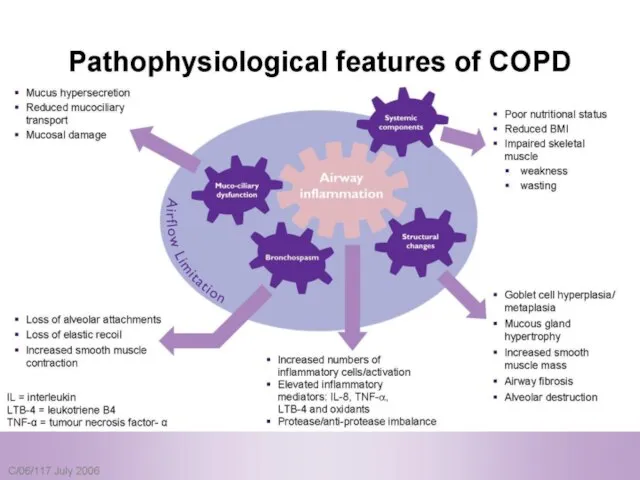
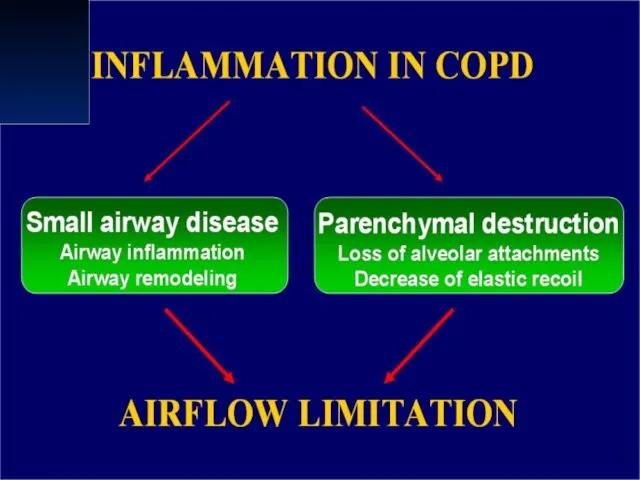
- 12. Pathophysiology COPD has both Pulmonary components Systemic components
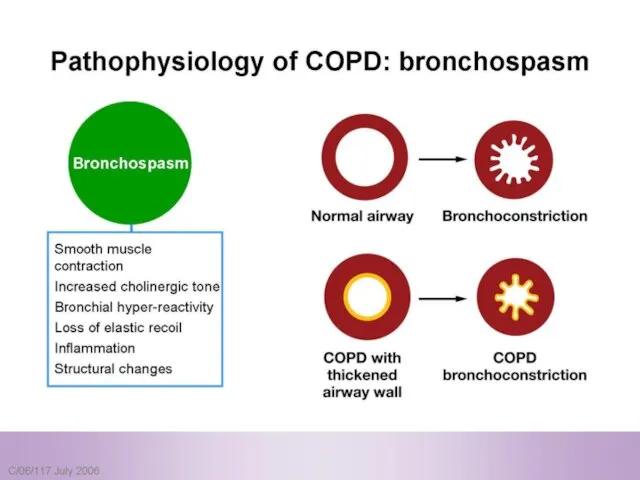
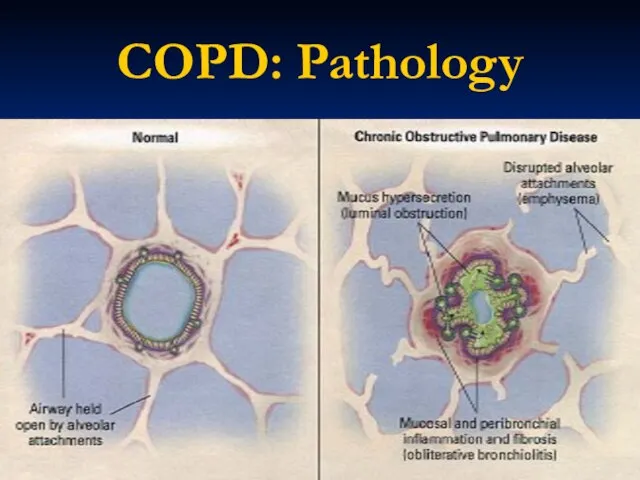
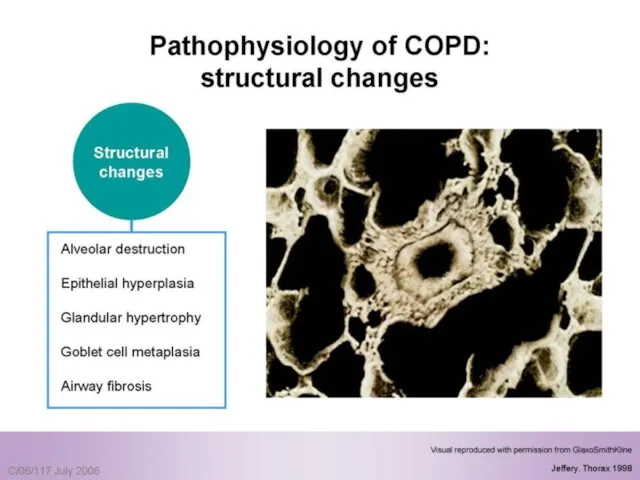
- 13. Pulmonary components: Mucus secretion An enlargement of mucous secreting glands and an increasing number of goblet
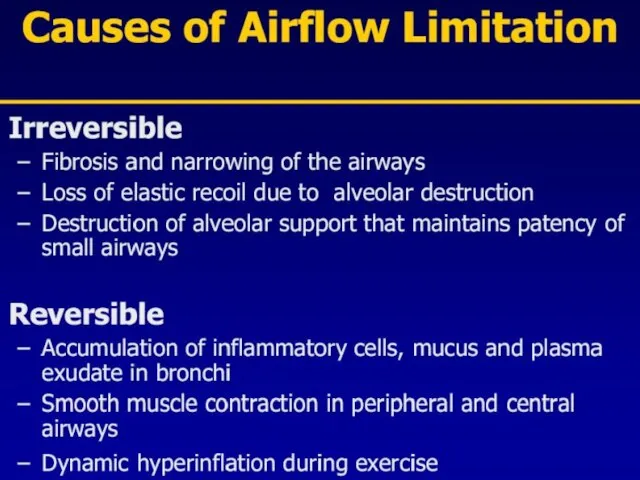
- 14. Pulmonary components: Premature airway closure leads to gas trapping and hyperinflation → ↓ pulmonary and chest
- 15. Pulmonary components: Flattening of the diaphragmatic muscles and increase horizontal alignment of the intercostals muscles →
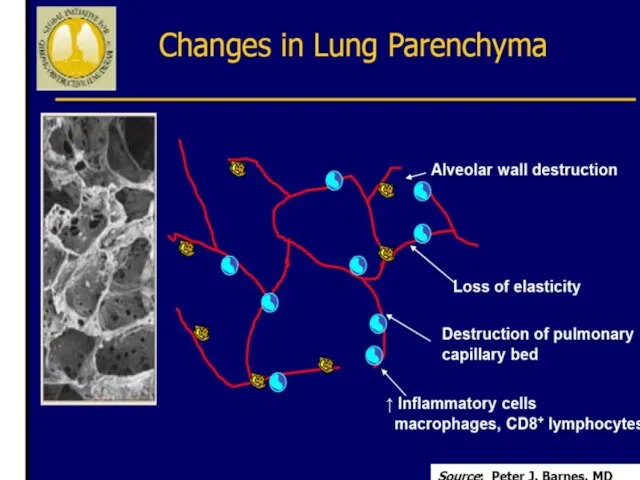
- 16. Pulmonary components: In the alveolar capillary units the unopposed action of proteases and oxidants → destruction
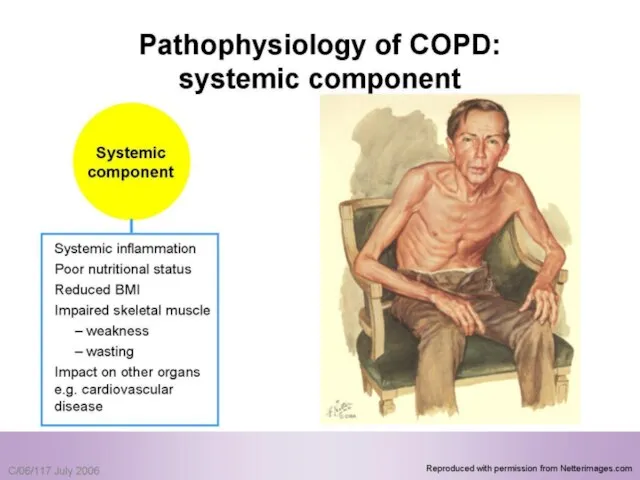
- 18. Systemic components: 1. Skeletal muscle weakness. 2. Increase circulating inflammatory markers. 3. Impaired salt and water
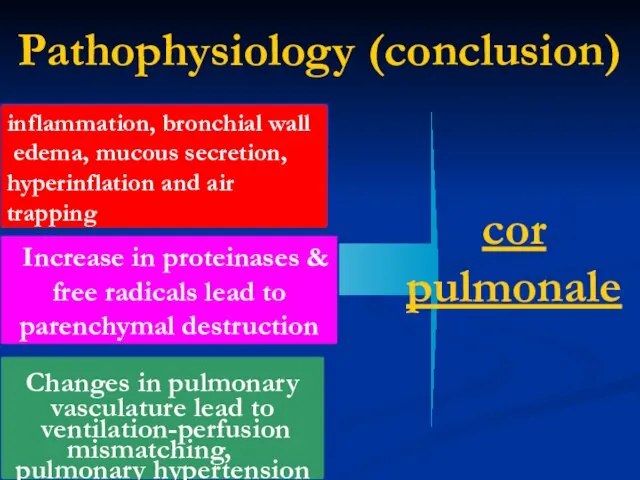
- 22. Pathophysiology (conclusion) inflammation, bronchial wall edema, mucous secretion, hyperinflation and air trapping Increase in proteinases &
- 25. COPD: Pathology
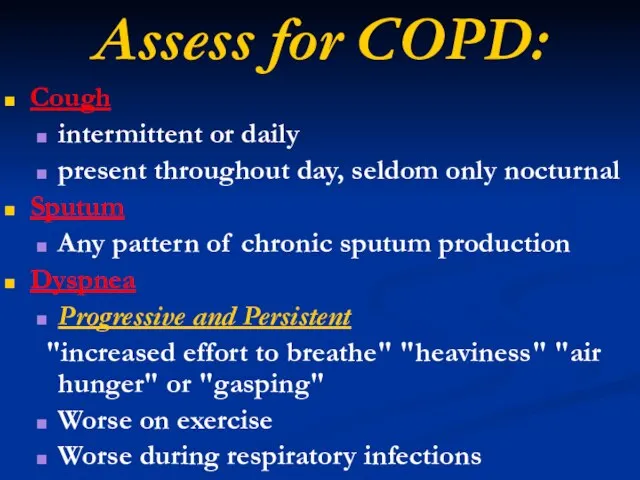
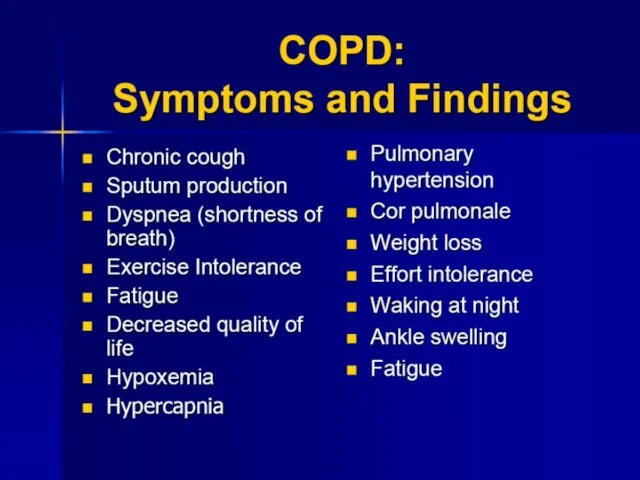
- 29. Assess for COPD: Cough intermittent or daily present throughout day, seldom only nocturnal Sputum Any pattern
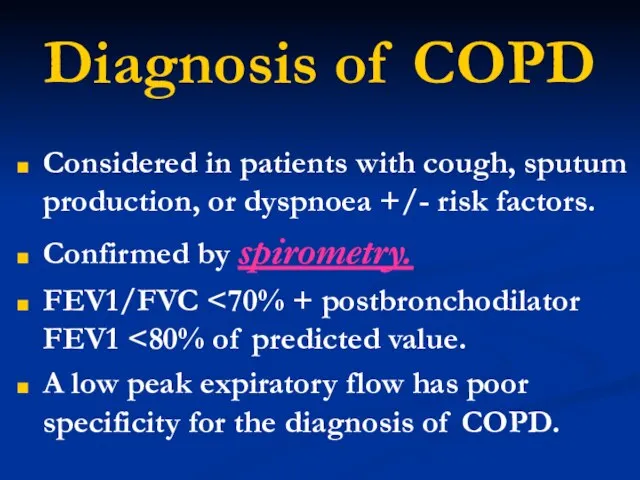
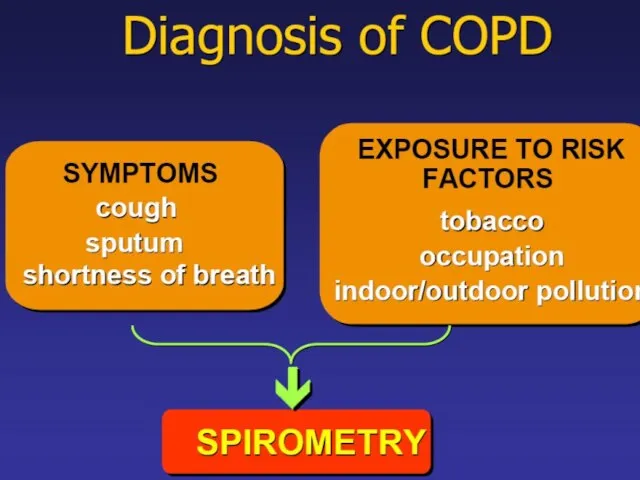
- 31. Diagnosis of COPD Considered in patients with cough, sputum production, or dyspnoea +/- risk factors. Confirmed
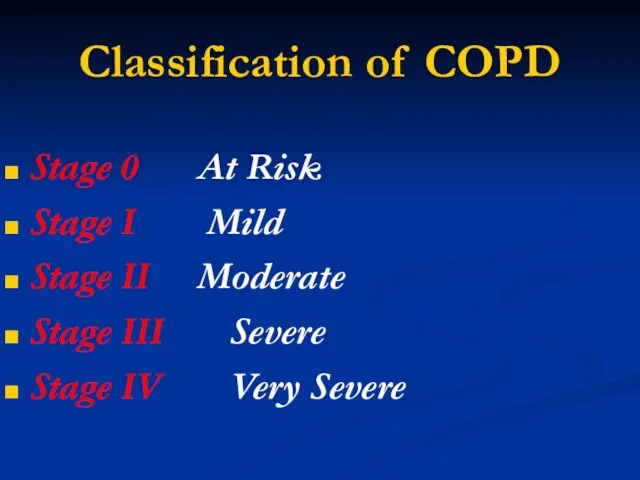
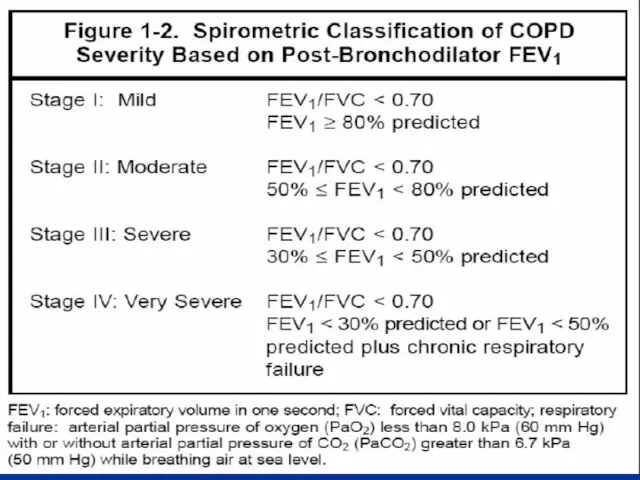
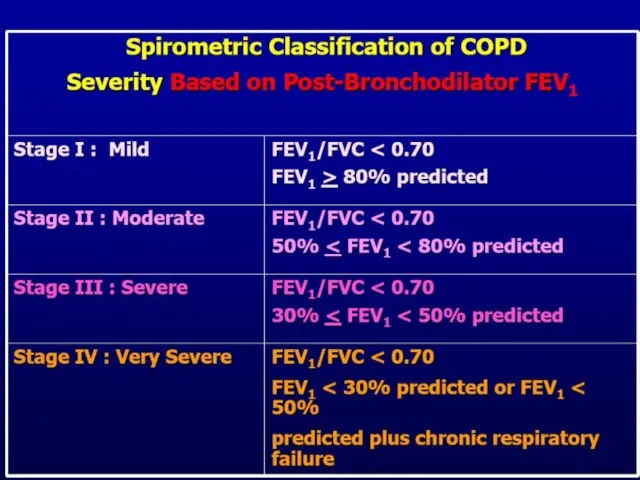
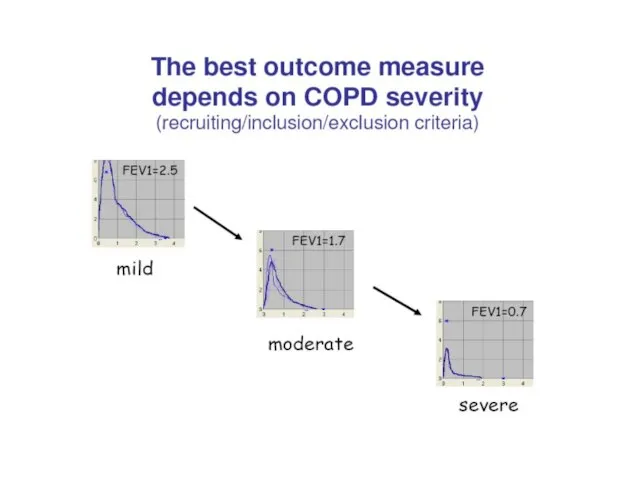
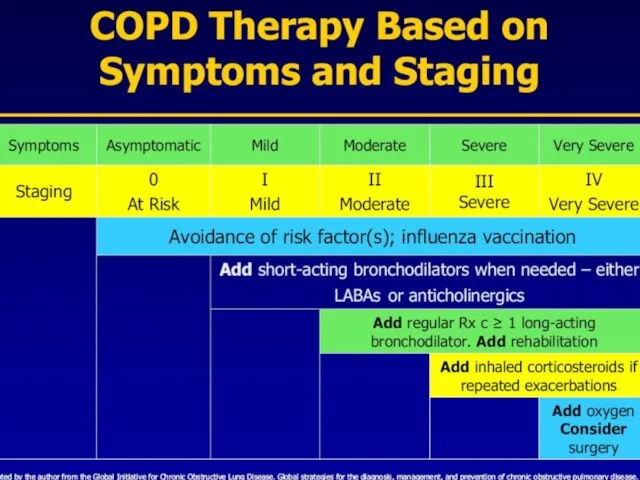
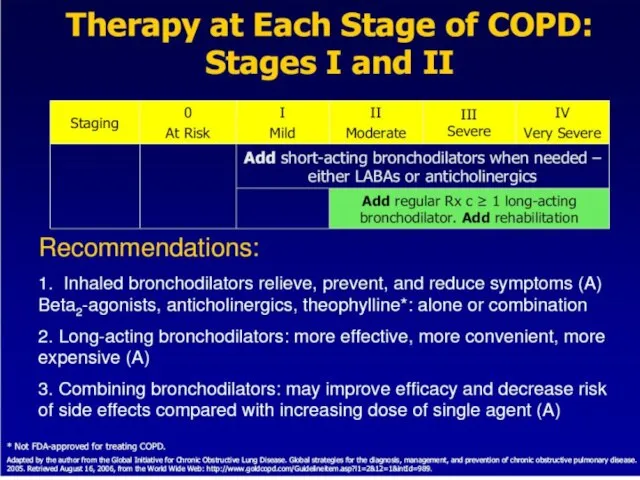
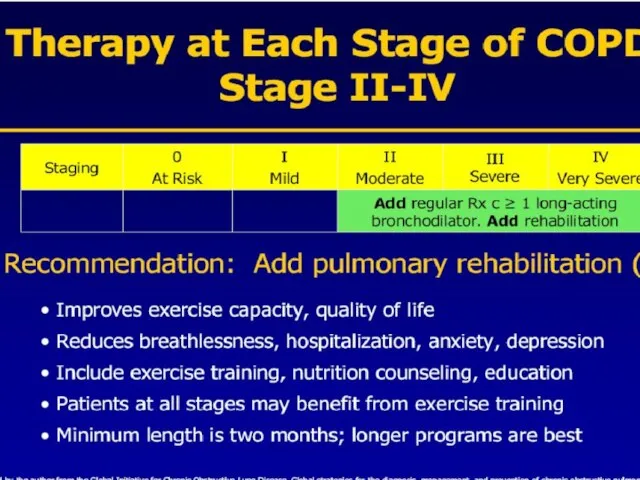
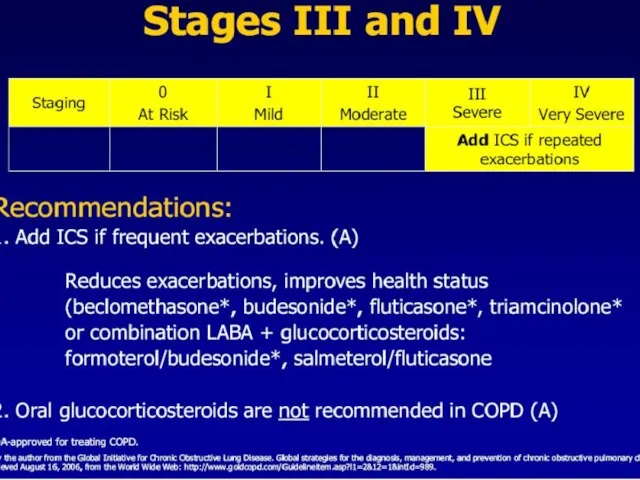
- 32. Classification of COPD Stage 0 At Risk Stage I Mild Stage II Moderate Stage III Severe
- 34. Stage 0 At Risk Normal spirometry +/- Chronic symptoms (cough, sputum, production)
- 35. Stage I Mild COPD FEV1/FVC FEV1 >80% predicted With or without chronic symptoms (cough, sputum production)
- 36. Stage II Moderate COPD FEV1/FVC 50% With or without chronic symptoms (cough, sputum production)
- 37. Stage III Severe COPD FEV1/FVC 30% With or without chronic symptoms (cough, sputum production)
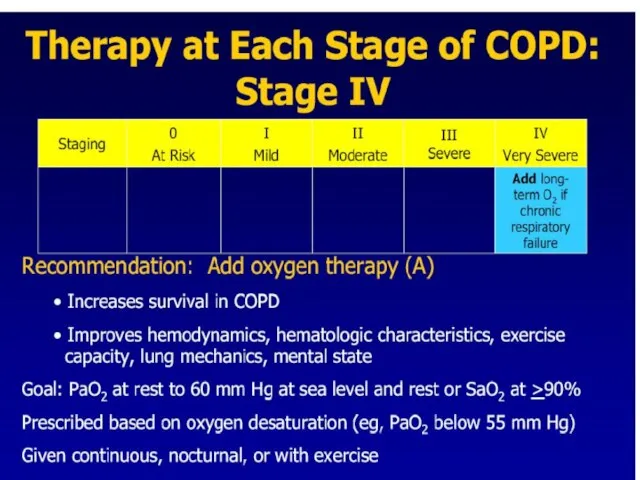
- 38. Stage IV Very Severe COPD FEV1/FVC FEV1 chronic respiratory failure
- 41. Diagnosis of COPD
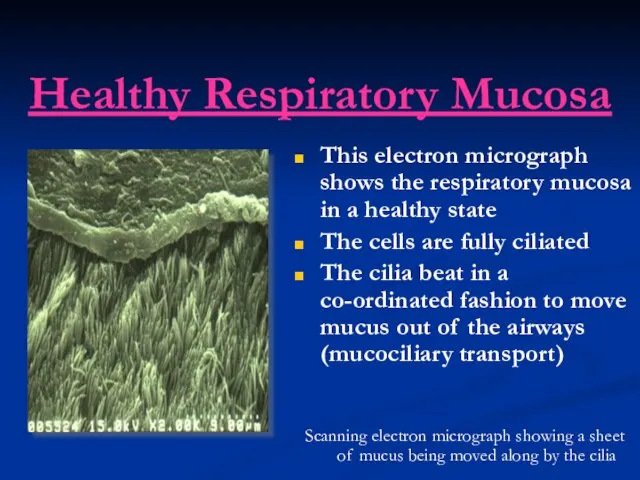
- 42. Healthy Respiratory Mucosa This electron micrograph shows the respiratory mucosa in a healthy state The cells
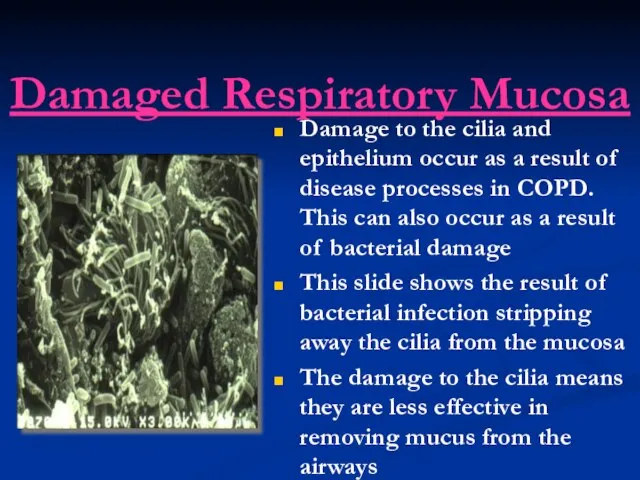
- 43. Damaged Respiratory Mucosa Damage to the cilia and epithelium occur as a result of disease processes
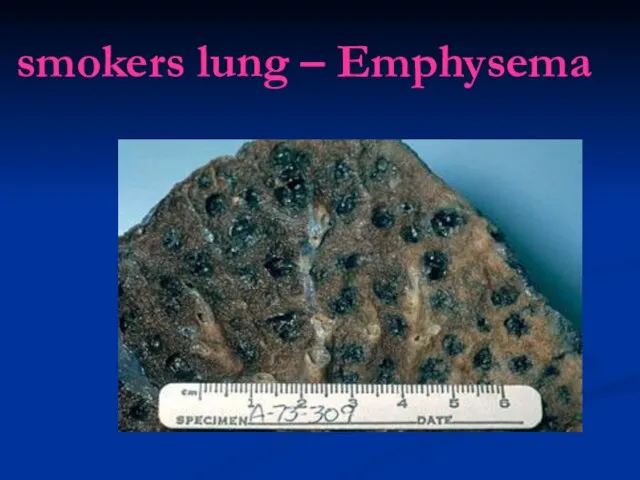
- 45. smokers lung – Emphysema
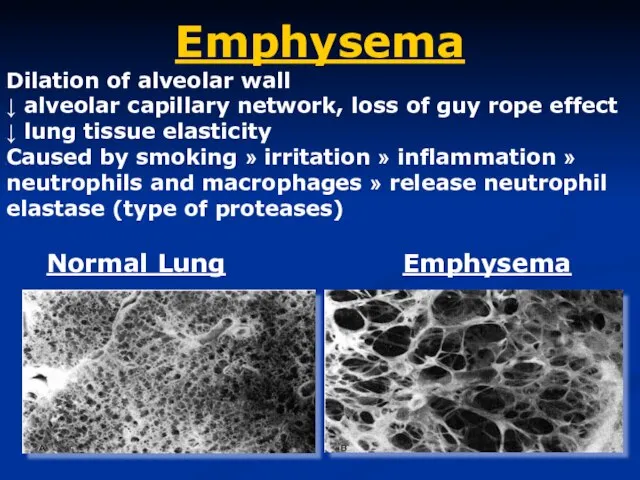
- 46. Emphysema Dilation of alveolar wall ↓ alveolar capillary network, loss of guy rope effect ↓ lung
- 47. Emphysema is defined pathologically as dilatation and destruction of the lung tissue distal to the terminal
- 48. classification Centri-acinar emphysema. Pan-acinar emphysema. Irregular emphysema.
- 49. Centri-acinar emphysema Distension and damage of lung tissue is concentrated around the respiratory bronchioles, whilst the
- 50. Pan-acinar emphysema Distension and destruction appear to involve the whole of the acinus, and in the
- 51. Irregular emphysema scarring and damage affect the lung parenchyma patchily without particular regard for acinar structure
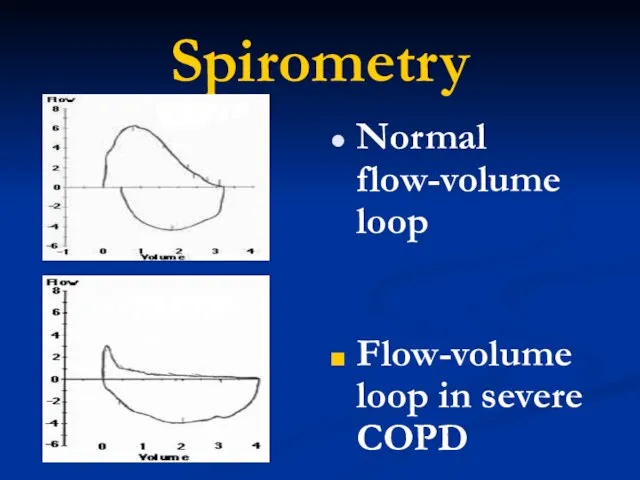
- 52. Spirometry Normal flow-volume loop Flow-volume loop in severe COPD
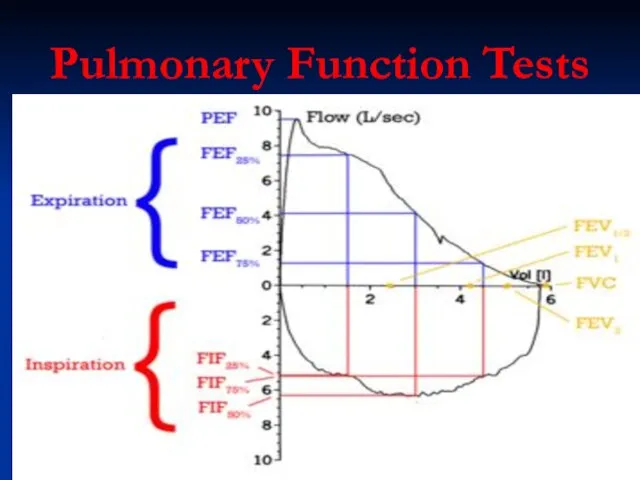
- 54. Pulmonary Function Tests
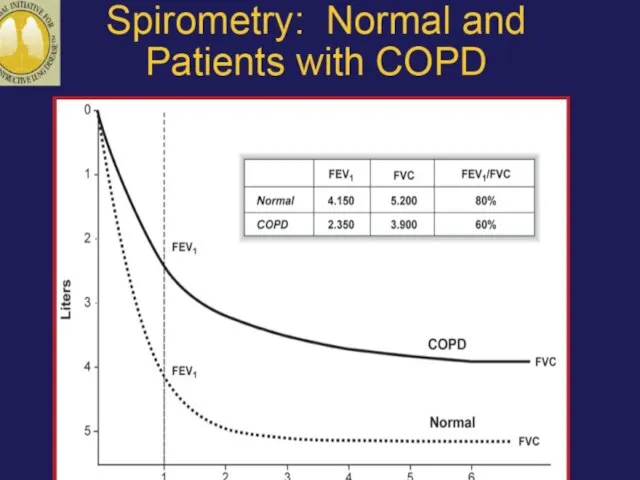
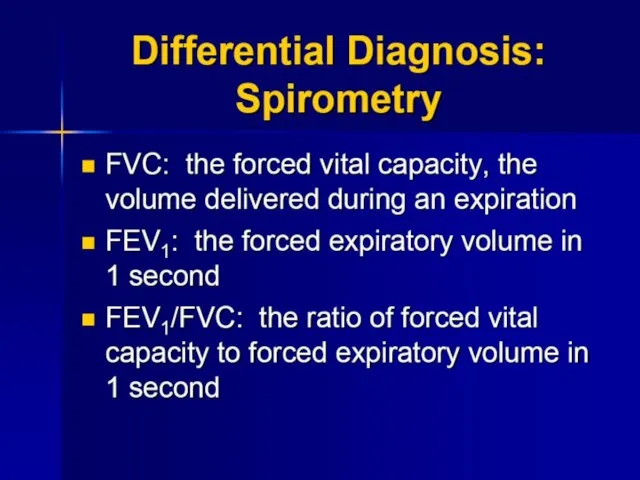
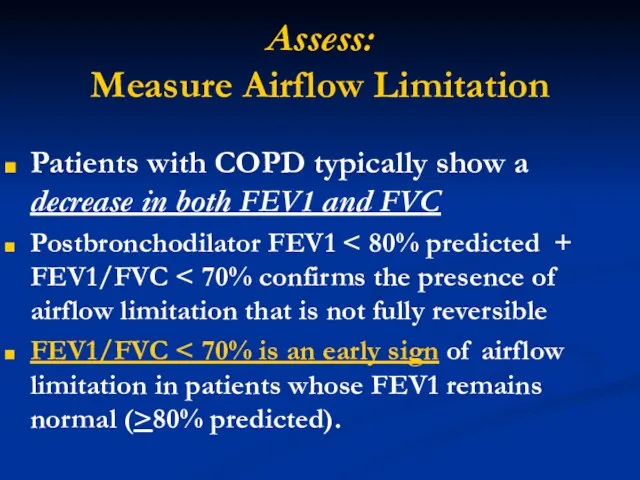
- 57. Assess: Measure Airflow Limitation Patients with COPD typically show a decrease in both FEV1 and FVC
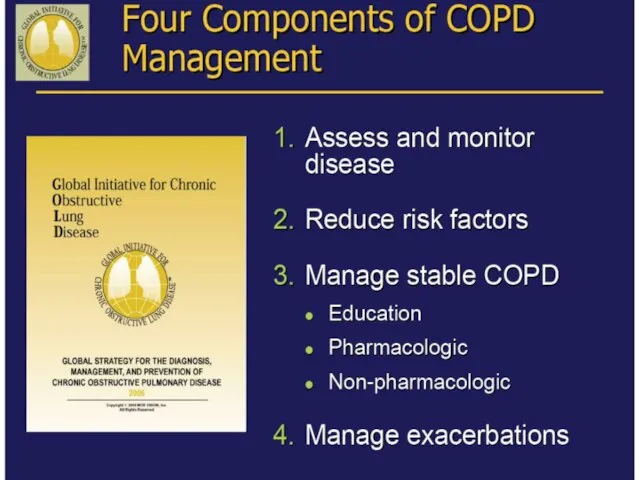
- 60. GOALS of COPD MANAGEMENT Relieve symptoms Prevent disease progression Improve exercise tolerance Improve health status Prevent
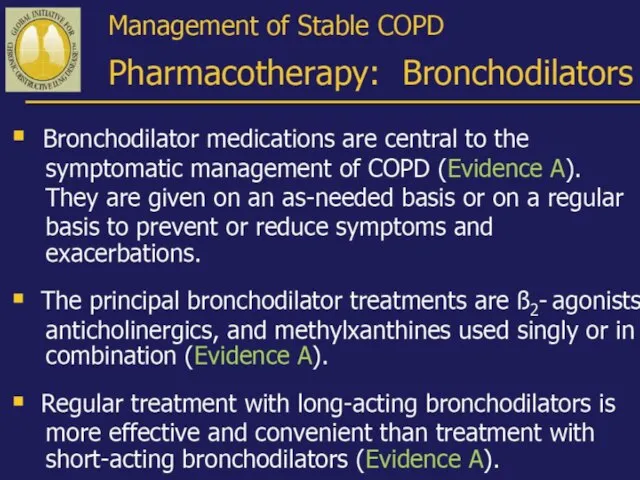
- 62. General Points Only smoking cessation and O2 therapy have been shown to prolong survival Other therapies
- 63. Exacerbation management Chronic stable management Adjuvant therapy
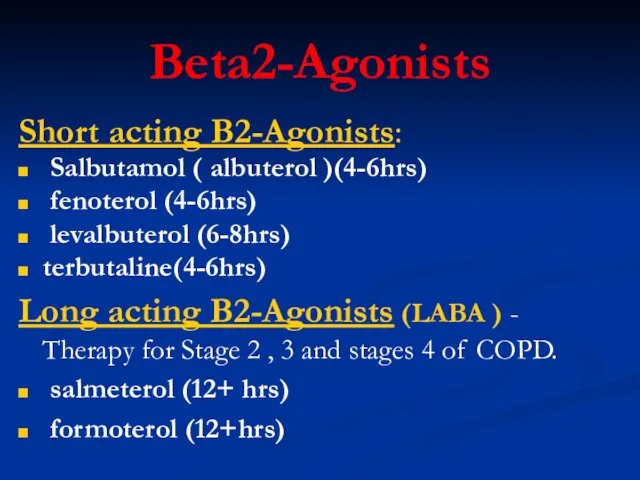
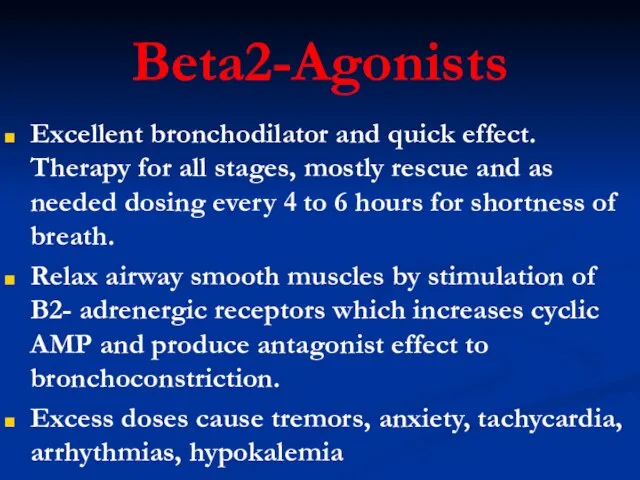
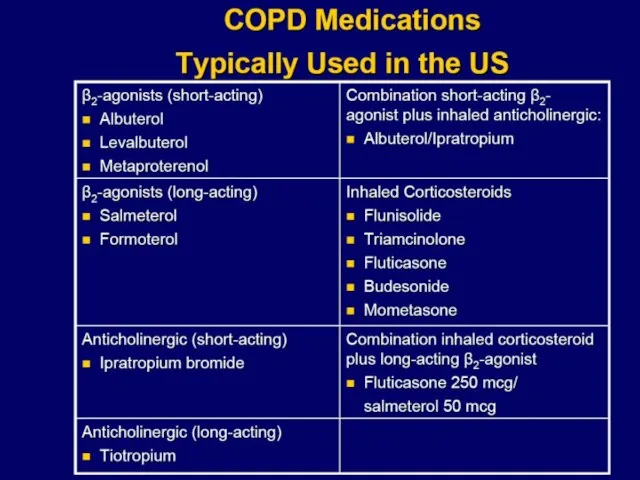
- 66. Beta2-Agonists Short acting B2-Agonists: Salbutamol ( albuterol )(4-6hrs) fenoterol (4-6hrs) levalbuterol (6-8hrs) terbutaline(4-6hrs) Long acting B2-Agonists
- 67. Beta2-Agonists Excellent bronchodilator and quick effect. Therapy for all stages, mostly rescue and as needed dosing
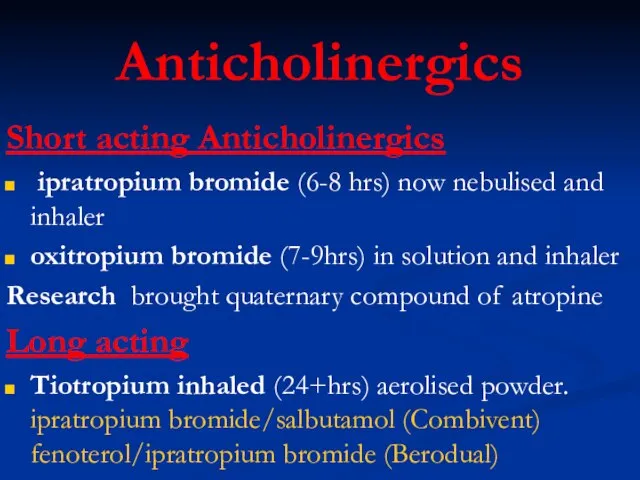
- 68. Anticholinergics Short acting Anticholinergics ipratropium bromide (6-8 hrs) now nebulised and inhaler oxitropium bromide (7-9hrs) in
- 69. Anticholinergics (Tiotropium) Block muscarinic receptors and prevent smooth muscle contraction while ↓ release of secretion from
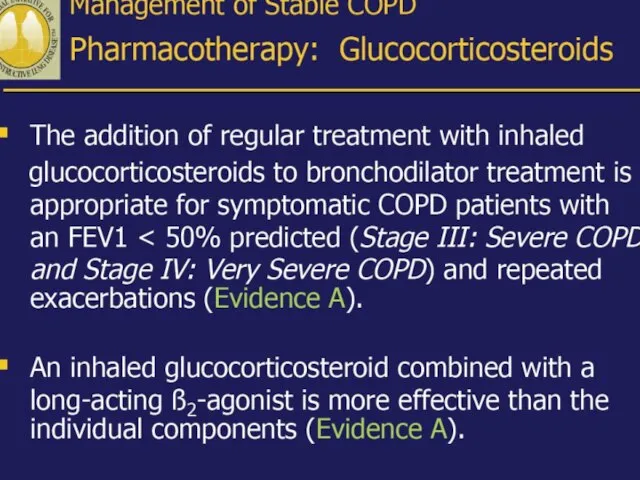
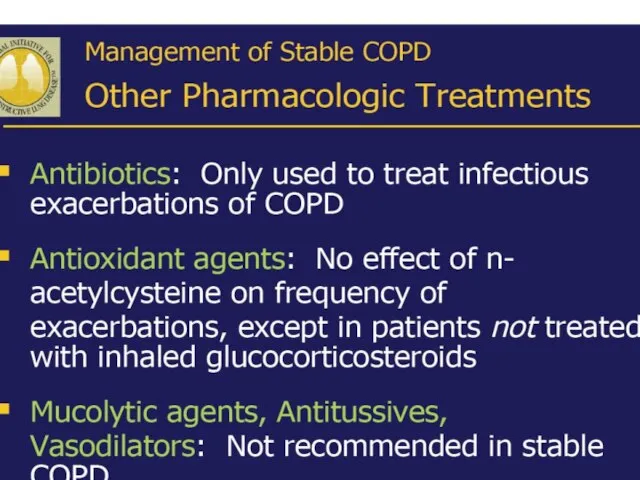
- 70. Drug therapy for COPD begins with long acting anticholinergics and beta-2 agonist bronchodilators. These provide symptom
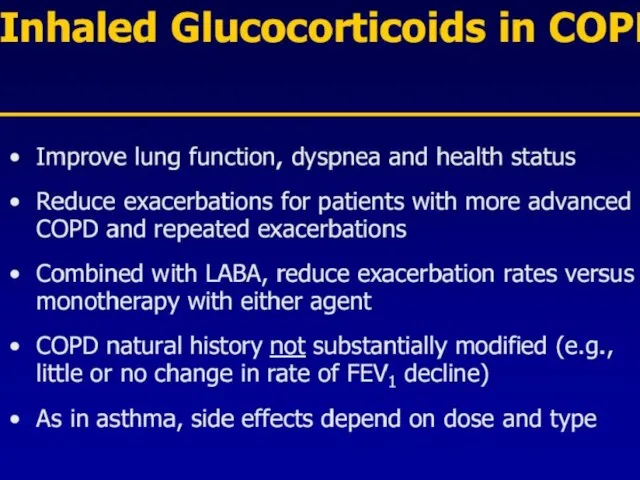
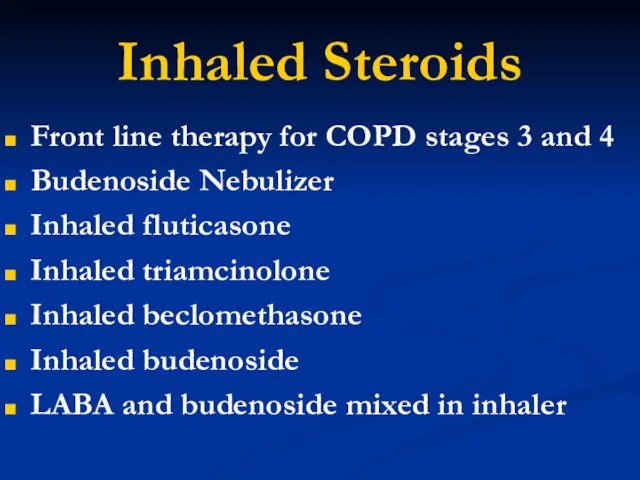
- 76. Inhaled Steroids Front line therapy for COPD stages 3 and 4 Budenoside Nebulizer Inhaled fluticasone Inhaled
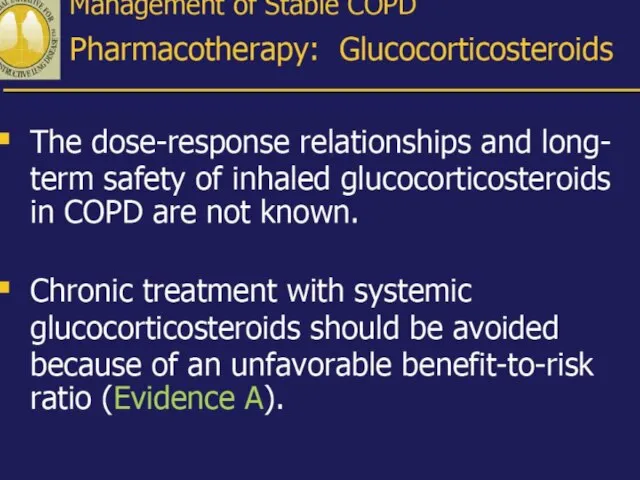
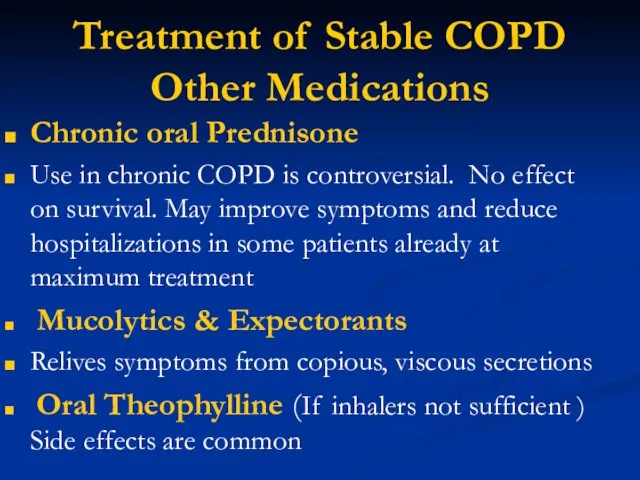
- 79. Treatment of Stable COPD Other Medications Chronic oral Prednisone Use in chronic COPD is controversial. No
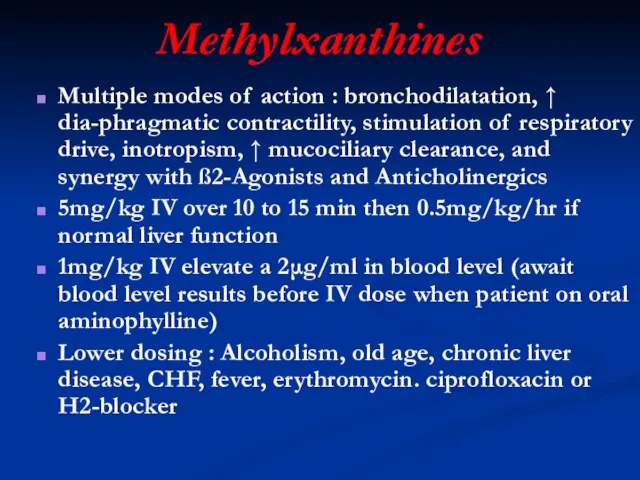
- 80. Methylxanthines Multiple modes of action : bronchodilatation, ↑ dia-phragmatic contractility, stimulation of respiratory drive, inotropism, ↑
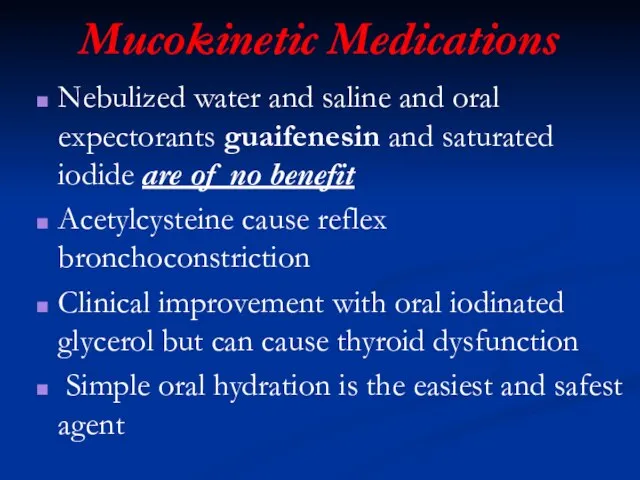
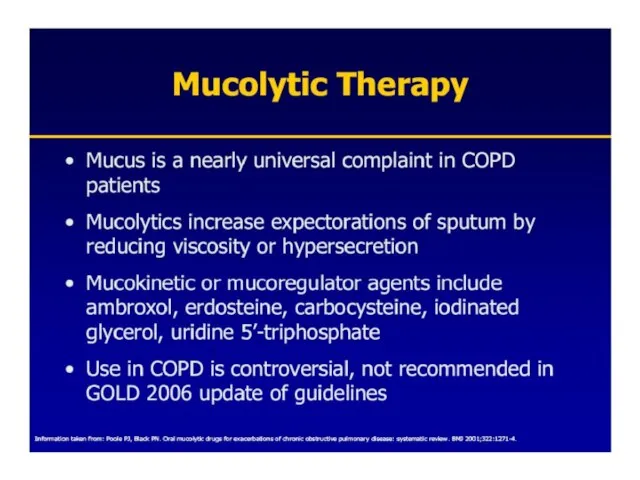
- 81. Mucokinetic Medications Nebulized water and saline and oral expectorants guaifenesin and saturated iodide are of no
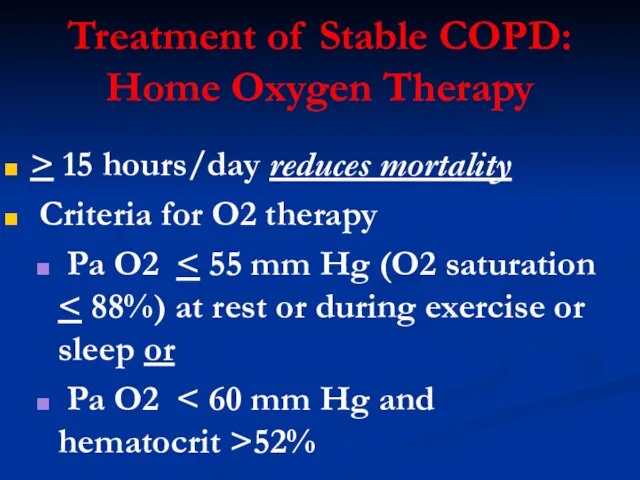
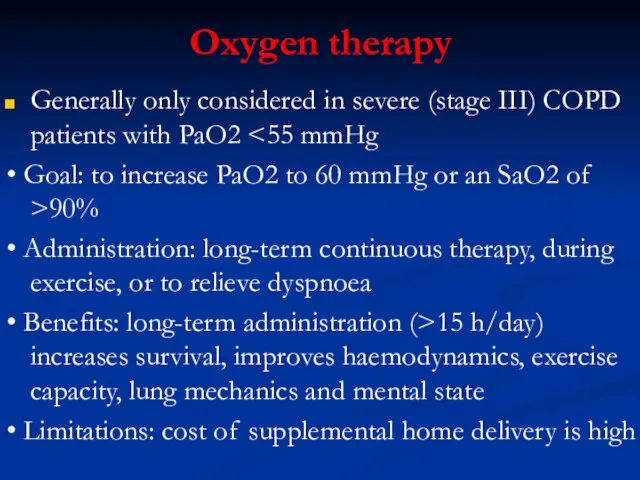
- 82. Treatment of Stable COPD: Home Oxygen Therapy > 15 hours/day reduces mortality Criteria for O2 therapy
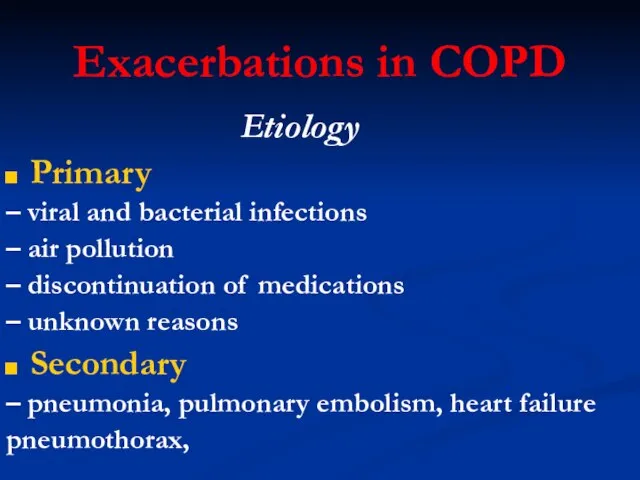
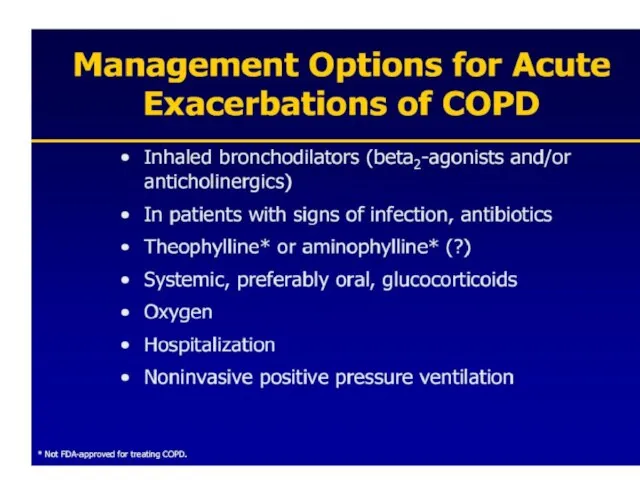
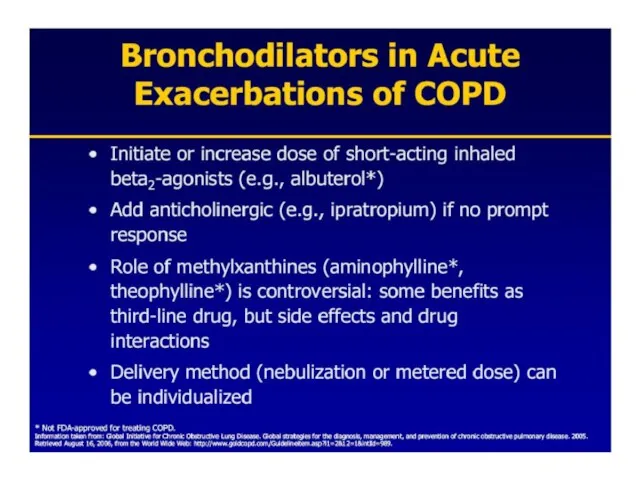
- 84. Exacerbations in COPD Etiology Primary – viral and bacterial infections – air pollution – discontinuation of
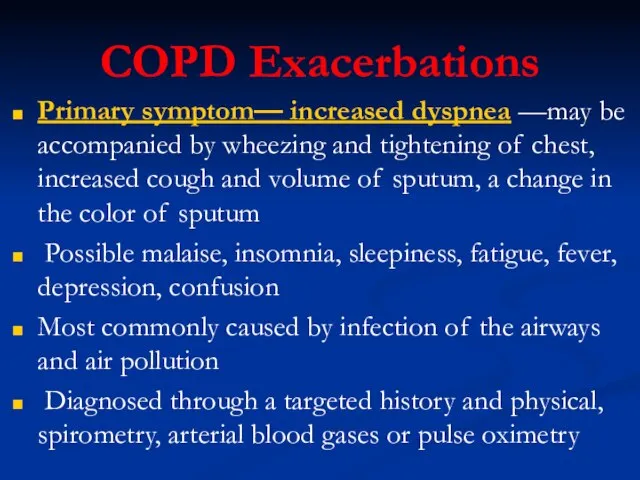
- 85. COPD Exacerbations Primary symptom— increased dyspnea —may be accompanied by wheezing and tightening of chest, increased
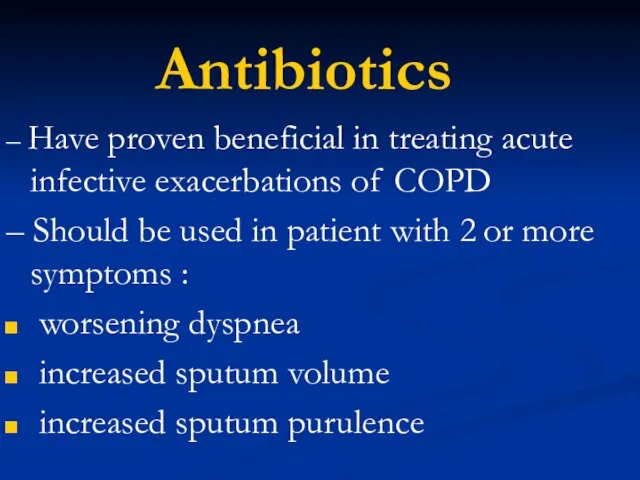
- 92. Antibiotics – Have proven beneficial in treating acute infective exacerbations of COPD – Should be used
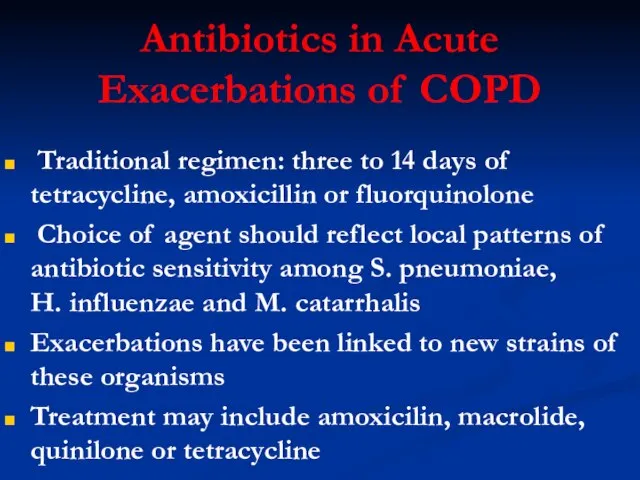
- 93. Antibiotics in Acute Exacerbations of COPD Traditional regimen: three to 14 days of tetracycline, amoxicillin or
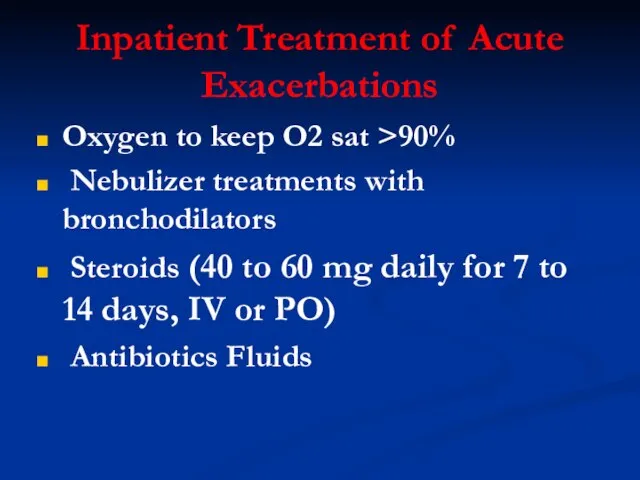
- 94. Inpatient Treatment of Acute Exacerbations Oxygen to keep O2 sat >90% Nebulizer treatments with bronchodilators Steroids
- 96. Oxygen therapy Generally only considered in severe (stage III) COPD patients with PaO2 • Goal: to
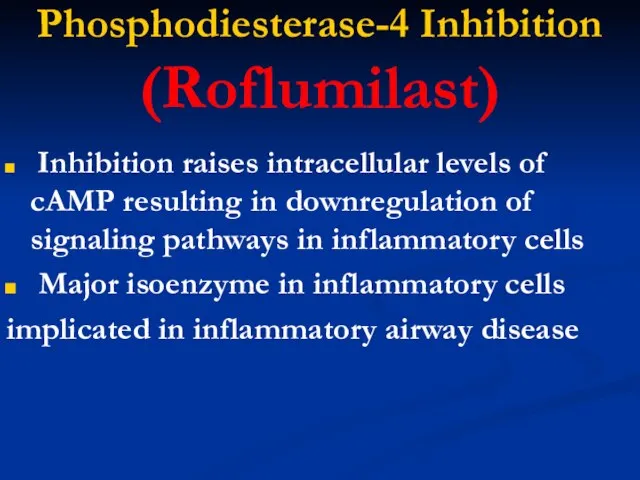
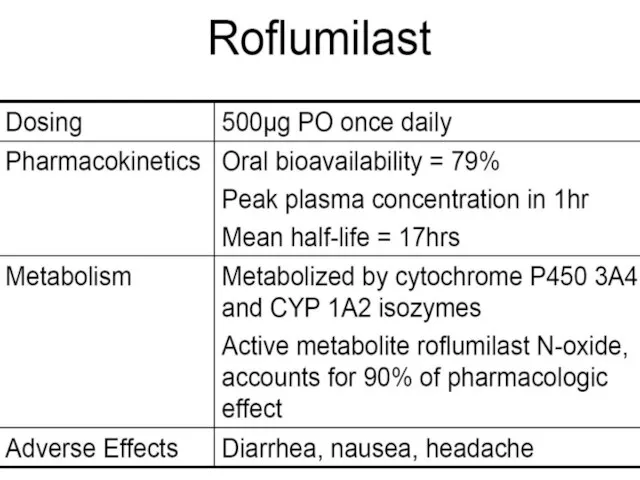
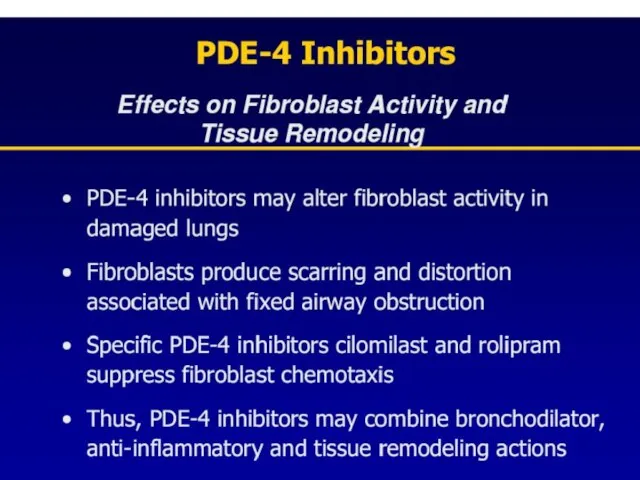
- 98. Phosphodiesterase-4 Inhibition (Roflumilast) Inhibition raises intracellular levels of cAMP resulting in downregulation of signaling pathways in
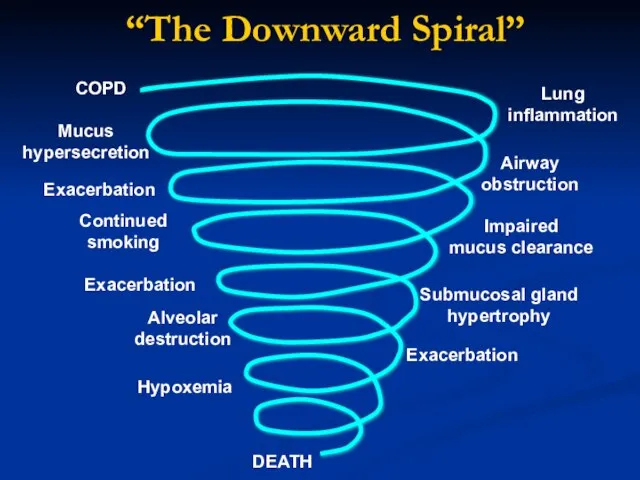
- 103. COPD Airway obstruction Exacerbation Mucus hypersecretion Continued smoking Lung inflammation Alveolar destruction Impaired mucus clearance Submucosal
- 104. SMOKERS “Hope and expect for the best. Prepare for the worst.” Back AL, Arnold RM, Quill
- 105. NEXT STAGE…
- 106. PREVENT COPD
- 107. PREVENT COPD
- 110. Скачать презентацию








 Аппаратчик-оператор
Аппаратчик-оператор Точка кипения МБИ
Точка кипения МБИ Кавказ в творчестве Пушкина
Кавказ в творчестве Пушкина примеры теплопередачи в быту и технике
примеры теплопередачи в быту и технике АЦЦ брендинг прикассовых зон
АЦЦ брендинг прикассовых зон Гончарное искусство
Гончарное искусство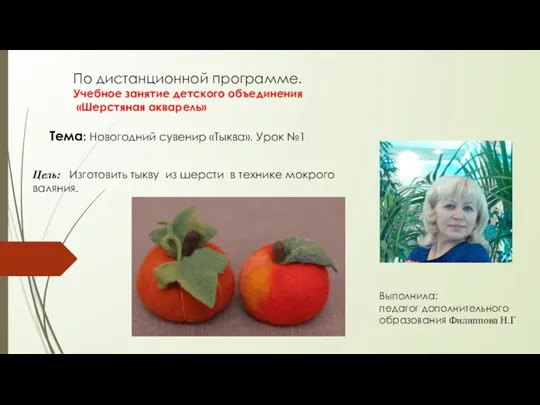 Новогодний сувенир Тыква
Новогодний сувенир Тыква В гости к русской сказке
В гости к русской сказке Вступление в 5 класс. Трудности адаптации пятиклассников в школе
Вступление в 5 класс. Трудности адаптации пятиклассников в школе БОРИС НИКОЛАЕВИЧ СЕРГУНЕНКОВ
БОРИС НИКОЛАЕВИЧ СЕРГУНЕНКОВ Основные образы поэмы
Основные образы поэмы КНИГА 2011
КНИГА 2011 - исторические- политические- культурные предпосылки активного участия общества в деле противодействия организов
- исторические- политические- культурные предпосылки активного участия общества в деле противодействия организов Организация оплаты труда
Организация оплаты труда Работа в сети Интернет. Электронная почта
Работа в сети Интернет. Электронная почта Колизей
Колизей Возникновение письменности на Руси
Возникновение письменности на Руси Жизнь и творчество Н.А. Некрасова (1821-1878)
Жизнь и творчество Н.А. Некрасова (1821-1878) Тема 4. Бюджетное право и бюджетное устройство Российской Федерации 1. Понятие и значение государственного и местного бюджетов 2
Тема 4. Бюджетное право и бюджетное устройство Российской Федерации 1. Понятие и значение государственного и местного бюджетов 2 Презентация1
Презентация1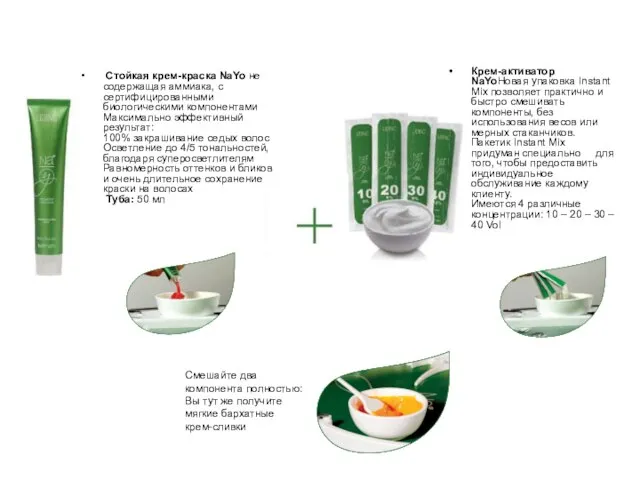 Стойкая крем-краска NaYo не содержащая аммиака, с сертифицированными биологическими компонентамиМаксимально эффективный результа
Стойкая крем-краска NaYo не содержащая аммиака, с сертифицированными биологическими компонентамиМаксимально эффективный результа Презентация на тему: Куликовская битва и ее историческое значение Работу выполнил : студент 1-го курса ЮБ 02/1402 Куликов Андрей
Презентация на тему: Куликовская битва и ее историческое значение Работу выполнил : студент 1-го курса ЮБ 02/1402 Куликов Андрей Проект «Дистанционное обучение детей-инвалидов на дому»
Проект «Дистанционное обучение детей-инвалидов на дому» Среди детей наших групп затеялся спор: «Кто из родителей поможет выиграть главный приз- «ФУТБОЛ». Этот приз, нам детям, очень
Среди детей наших групп затеялся спор: «Кто из родителей поможет выиграть главный приз- «ФУТБОЛ». Этот приз, нам детям, очень  Правописание приставок
Правописание приставок Мастер – класс: клеевой коллаж Дерево
Мастер – класс: клеевой коллаж Дерево Склеротический тип
Склеротический тип Основы делопроизводства
Основы делопроизводства