Содержание
- 2. HEART FAILURE Randa Mahmoud Al-Harizy Prof. of Internal Medicine
- 3. HEART FAILURE Clinical syndrome that can result from any structural or functional cardiac disorder that impairs
- 4. Main causes Ischemic heart disease, Cardiomyopathy, Hypertension Other causes: Valvular heart disease, Congenital heart disease, Alcohol
- 5. Impaired cardiac contractility as in myocardial infarction and cardiomyopathy Ventricular outflow obstruction (pressure overload) as in
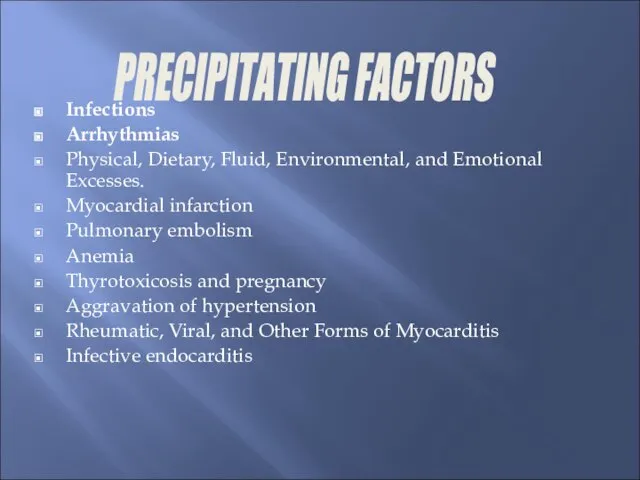
- 6. Infections Arrhythmias Physical, Dietary, Fluid, Environmental, and Emotional Excesses. Myocardial infarction Pulmonary embolism Anemia Thyrotoxicosis and
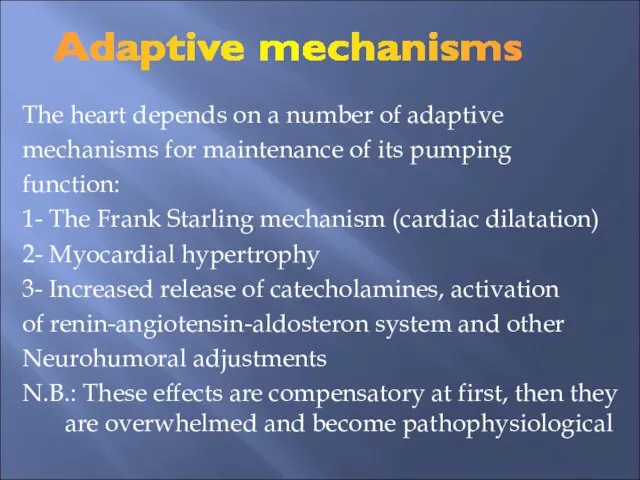
- 7. The heart depends on a number of adaptive mechanisms for maintenance of its pumping function: 1-
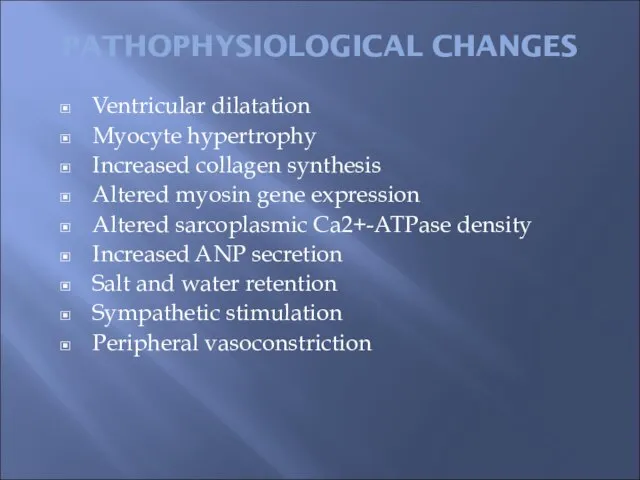
- 8. PATHOPHYSIOLOGICAL CHANGES Ventricular dilatation Myocyte hypertrophy Increased collagen synthesis Altered myosin gene expression Altered sarcoplasmic Ca2+-ATPase
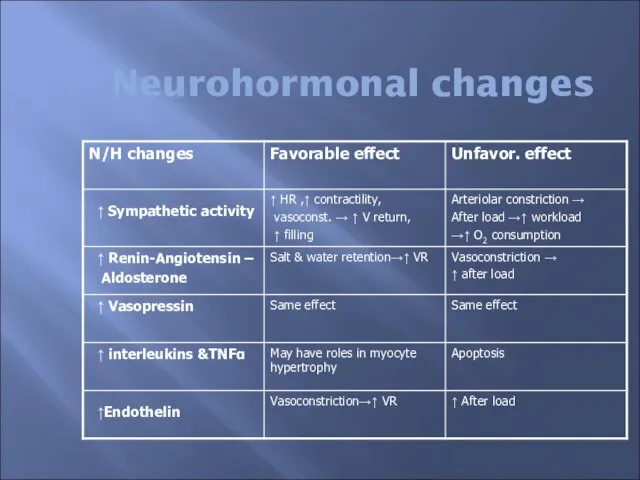
- 9. Neurohormonal changes
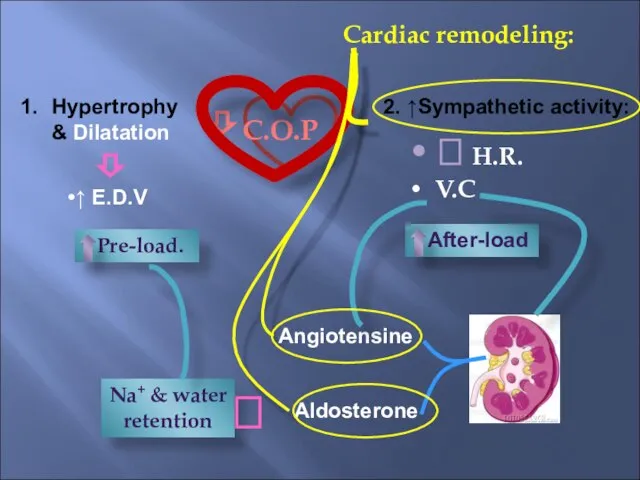
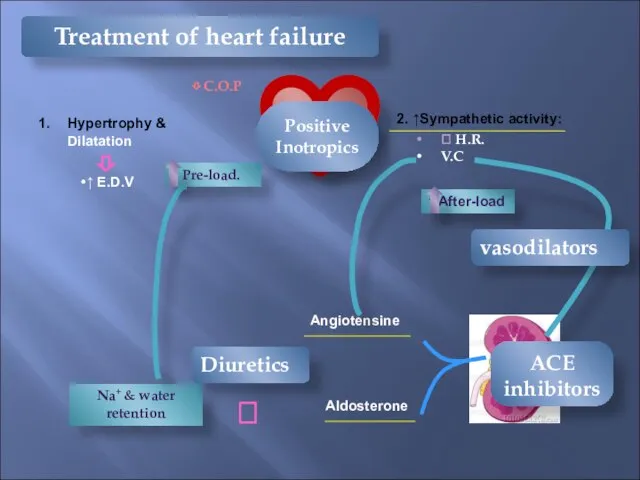
- 10. ⇩ C.O.P Cardiac remodeling: Hypertrophy & Dilatation ↑ E.D.V ⇩ 2. ↑Sympathetic activity: ⮥ H.R. V.C
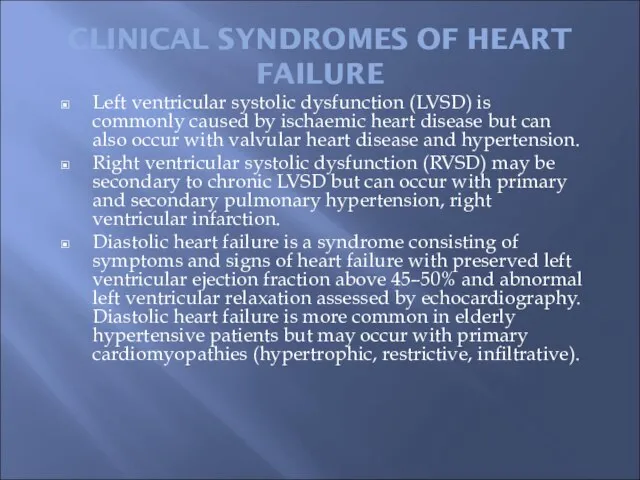
- 11. CLINICAL SYNDROMES OF HEART FAILURE Left ventricular systolic dysfunction (LVSD) is commonly caused by ischaemic heart
- 12. SYMPTOMS & SIGNS OF HEART FAILURE Left heart failure Symptoms are predominantly fatigue, exertional dyspnoea, orthopnoea
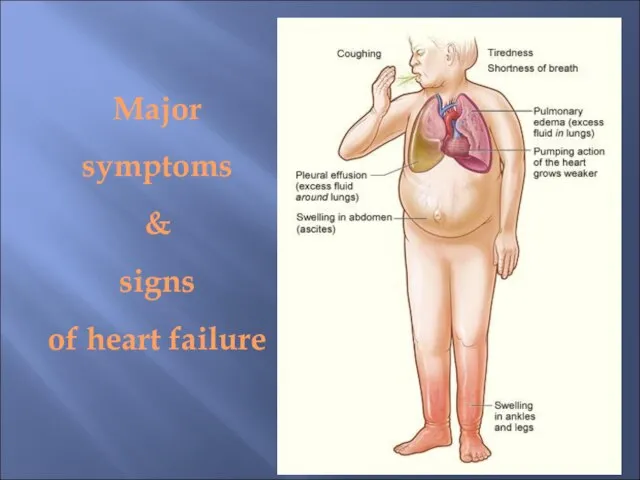
- 13. Right heart failure Symptoms (fatigue, breathlessness, anorexia and nausea) relate to distension and fluid accumulation in
- 14. Major symptoms & signs of heart failure
- 15. New York Heart Association (NYHA) Classification of heart failure Class I No limitation. Normal physical exercise
- 16. Framingham Criteria for Diagnosis of Congestive Heart Failure MAJOR CRITERIA PND, Neck vein distention, Rales, Cardiomegaly,
- 17. Diagnostic Investigations Blood tests - CBC, liver biochemistry, urea and electrolytes, cardiac enzymes , BNP or
- 18. BRAIN NATRIURETIC PEPTIDE (BNP) Pre pro-BNP is formed in the ventricles and, with myocyte stretch, is
- 19. Stress echocardiography. Exercise or pharmacological stress echocardiography has no radiation hazard and is a reliable technique
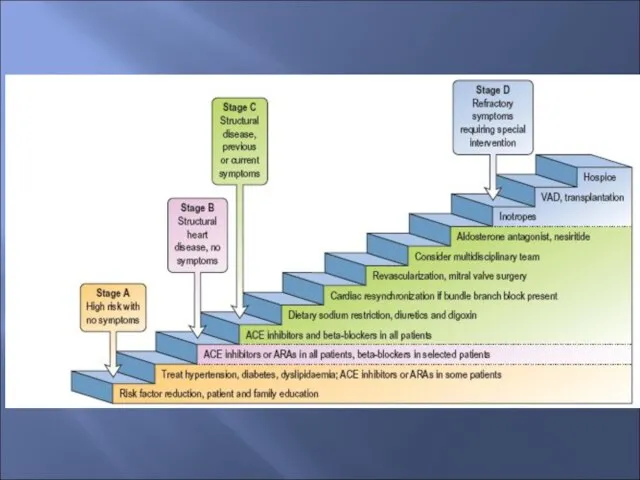
- 20. Treatment of Heart Failure The treatment of HF may be divided into five components: general measures.
- 21. Treatment of Heart Failure General measures: Rest, salt restriction, stop smoking Removal of the cause: This
- 22. ⇩ C.O.P Hypertrophy & Dilatation ↑ E.D.V ⇩ 2. ↑Sympathetic activity: ⮥ H.R. V.C ↑ After-load
- 24. Diuretics • Essential to control symptoms secondary to fluid retention • Prevent progression from HT to
- 25. Diuretics & ACEI reduces the number of sacks on the wagon
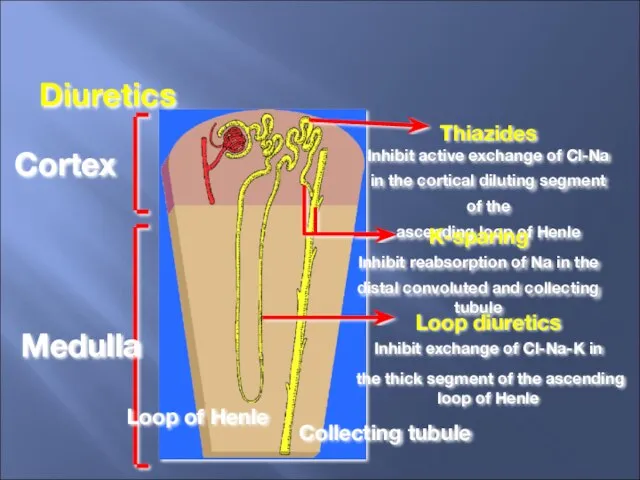
- 26. Cortex Medulla Thiazides Inhibit active exchange of Cl-Na in the cortical diluting segment of the ascending
- 27. Pharmacological Treatment Diuretics (loop diuretics, thiazide diuretics and potassium sparing diuretics) These act by promoting the
- 28. Diuretics (continue) Loop diuretics: such as furosemide and bumetanide Have a rapid onset of action (i.v.
- 29. Diuretics (continue) Thiazide diuretics: Thiazides are less effective in patients with reduced glomerular filtration rates. Thiazide
- 30. Diuretics (continue) Potassium-sparing diuretics: Spironolactone is a specific competitive antagonist to aldosterone, producing a weak diuresis
- 31. Vasodilator therapy Angiotensin-converting enzyme inhibitors ACEI: ACEI lower systemic vascular resistance and venous pressure, and reduce
- 32. Vasodilator therapy Angiotensin receptor antagonists: Angiotensin II receptor antagonists (ARA) (e.g. losartan, ibersartan, candesartan and valsartan)
- 33. Arteriolar vasodilators: Drugs such as α-adrenergic blockers (e.g. prazosin) and direct smooth-muscle relaxants (e.g. hydralazine) are
- 34. Venodilators: Short- and long-acting nitrates act by reducing preload and lowering venous pressure, with resulting reduction
- 35. β-Adrenoceptor blocking agents There is considerable evidence to support the use of beta-blockers in patients with
- 36. ß-Blockers Limit the donkey’s speed, thus saving energy
- 37. Inotropic Agents Intravenous inotropes are frequently used to support myocardial function in patients with acute left
- 38. Cardiac Glycosides Cardiac glycosides in clinical use are: Digoxin, Digitoxin Ouabain.
- 39. Digitalis Compounds Like the carrot placed in front of the donkey
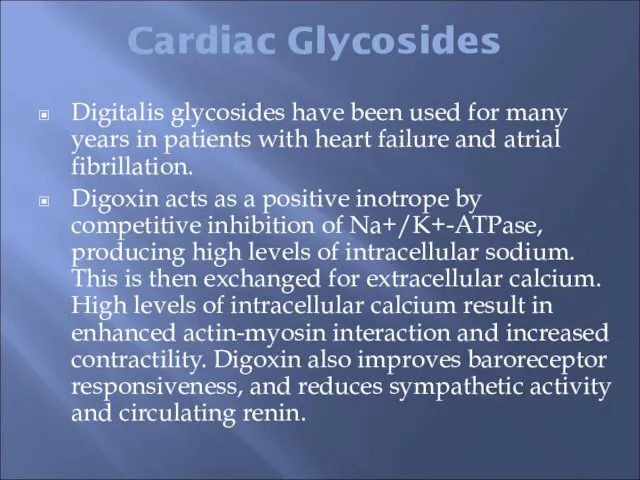
- 40. Cardiac Glycosides Digitalis glycosides have been used for many years in patients with heart failure and
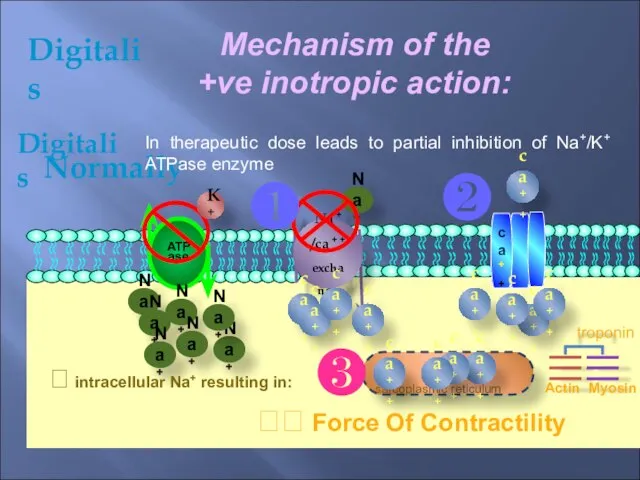
- 41. Digitalis Mechanism of the +ve inotropic action: ca++ ATPase ca++ Na+ Normally Digitalis In therapeutic dose
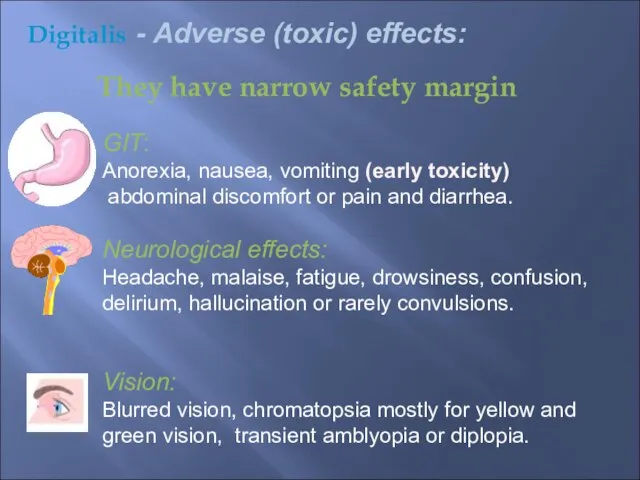
- 42. They have narrow safety margin GIT: Anorexia, nausea, vomiting (early toxicity) abdominal discomfort or pain and
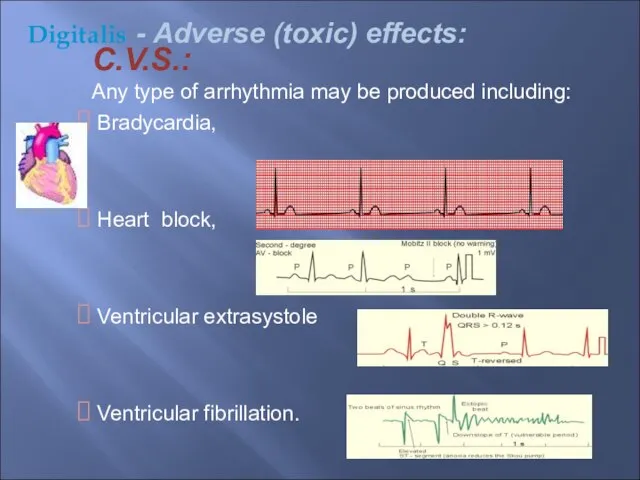
- 43. C.V.S.: Any type of arrhythmia may be produced including: Bradycardia, Heart block, Ventricular extrasystole Ventricular fibrillation.
- 44. Gynecomastia: May be due to steroidal structure. Digitalis - Adverse (toxic) effects:
- 45. Treatment Of Digitalis Toxicitiy: 1) Stop the responsible drug. 2) KCl syrup or slow release or
- 46. ⮲Partial heart block is treated by atropine. ⮲ Ventricular arrhythmia without A-V block is treated by
- 47. OTHER MEDICATIONS Anticoagulants: Oral anticoagulants are recommended in patients with atrial fibrillation and in sinus rhythm
- 48. Antiarrhythmic agents: Precipitating factors should be treated, in particular electrolyte disturbance. Atrial fibrillation is common in
- 49. The administration of synthetic BNP (Nesritide) produces beneficial haemodynamic effects in acute heart failure (reducing pulmonary
- 50. NON-PHARMACOLOGICAL TREATMENT OF HEART FAILURE Revascularization Biventricular pacemaker or implantable cardioverter–defibrillator Cardiac transplantation
- 51. Cardiac Resynchronization Therapy Increase the donkey’s (heart) efficiency
- 52. Acute Heart FAILURE Acute heart failure (AHF) occurs with the rapid onset of symptoms and signs
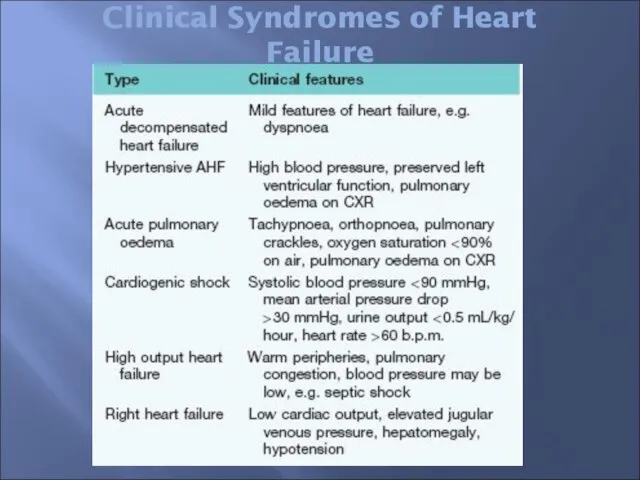
- 53. Clinical Syndromes of Heart Failure
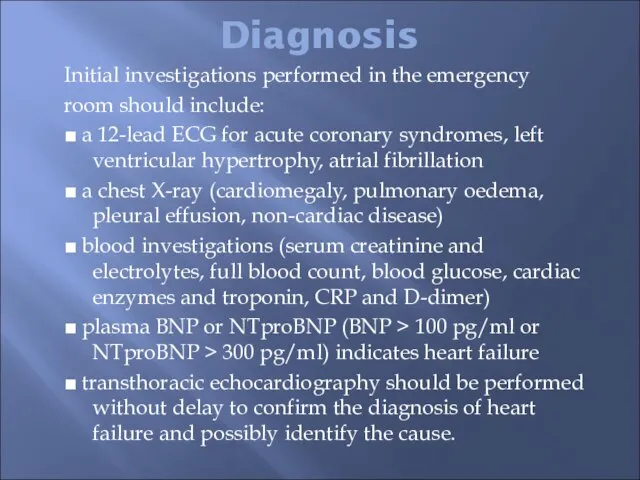
- 54. Diagnosis Initial investigations performed in the emergency room should include: ■ a 12-lead ECG for acute
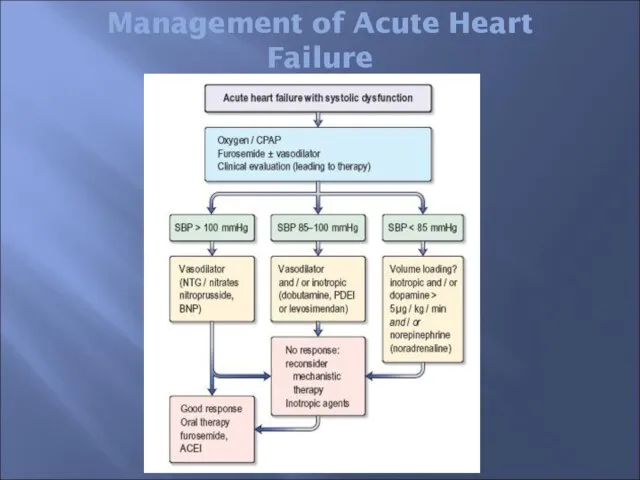
- 55. Management of Acute Heart Failure
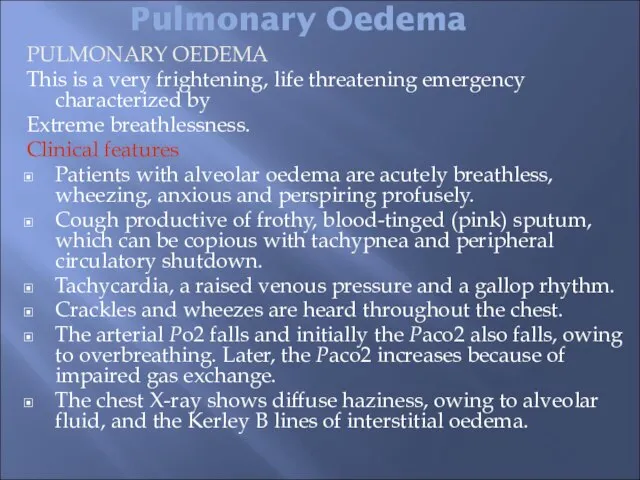
- 56. Pulmonary Oedema PULMONARY OEDEMA This is a very frightening, life threatening emergency characterized by Extreme breathlessness.
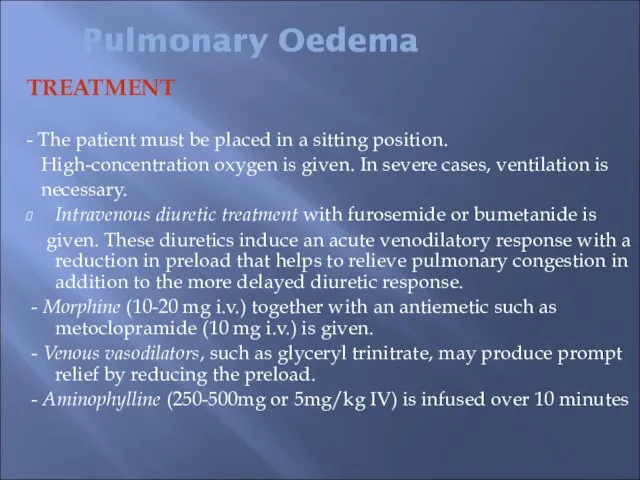
- 57. TREATMENT - The patient must be placed in a sitting position. High-concentration oxygen is given. In
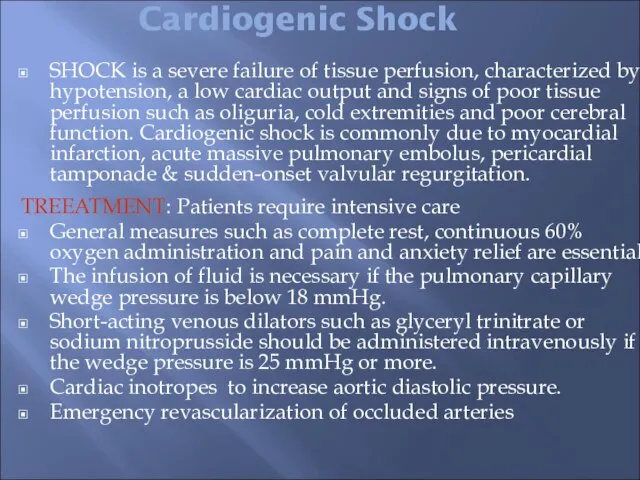
- 58. Cardiogenic Shock SHOCK is a severe failure of tissue perfusion, characterized by hypotension, a low cardiac
- 60. Скачать презентацию

 Повторение
Повторение Психология ведения группы. Лекция 2
Психология ведения группы. Лекция 2 САХАРНЫЙ ДИАБЕТ СОБАК И КОШЕК
САХАРНЫЙ ДИАБЕТ СОБАК И КОШЕК Публичная защита портфолио как форма представления результатов педагогической деятельности преподавателя школы искусств
Публичная защита портфолио как форма представления результатов педагогической деятельности преподавателя школы искусств Введение вGrid и пакет ‘Глобус’ (Globus Toolkit™)
Введение вGrid и пакет ‘Глобус’ (Globus Toolkit™) Презентация на тему Решение задач 5 класс
Презентация на тему Решение задач 5 класс Жилые модули в Китае
Жилые модули в Китае Художник
Художник Никто не забыт, ничто не забыто
Никто не забыт, ничто не забыто Стекольные работы
Стекольные работы Презентация на тему Рычаг
Презентация на тему Рычаг Проект Здоровый образ жизни
Проект Здоровый образ жизни Докладчик: Заместитель директора СКФОМС Булгакова Татьяна Яковлевна
Докладчик: Заместитель директора СКФОМС Булгакова Татьяна Яковлевна Презентация 10-Э класса
Презентация 10-Э класса Перенашивание беременности
Перенашивание беременности  Животноводствотестокружающий мир3 класс
Животноводствотестокружающий мир3 класс Энергия Солнца
Энергия Солнца Презентация на тему Что можно назвать государством
Презентация на тему Что можно назвать государством 1.Гос политика
1.Гос политика КЛАССА "А"
КЛАССА "А" Исследования как основа проведения информационной кампании
Исследования как основа проведения информационной кампании Обобщенная электрическая машина
Обобщенная электрическая машина Бывалые «охотники» компании «МДМ-Комплект» и рекламное агентство для мебельщиков «РЕКАНА»
Бывалые «охотники» компании «МДМ-Комплект» и рекламное агентство для мебельщиков «РЕКАНА» Презентация на тему Жуки-усачи
Презентация на тему Жуки-усачи Студия «Юный журналист»
Студия «Юный журналист» English is like a global in modern world
English is like a global in modern world Молодежная инициатива.
Молодежная инициатива. 4 модуль_Презентация_проекта_Аутсорсинг производства неметаллов
4 модуль_Презентация_проекта_Аутсорсинг производства неметаллов