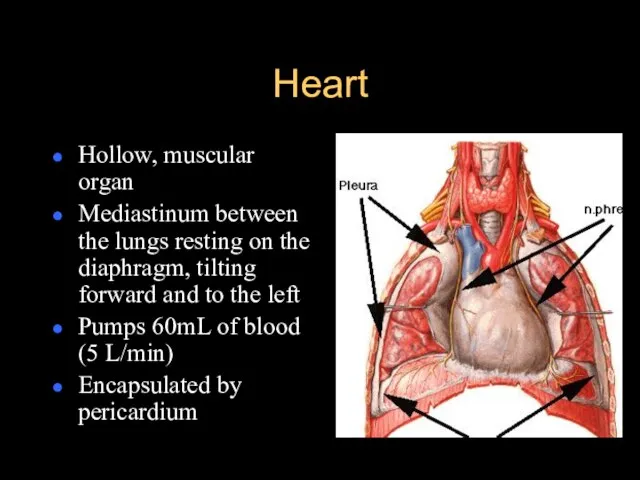
Слайд 2Heart
Hollow, muscular organ
Mediastinum between the lungs resting on the diaphragm, tilting
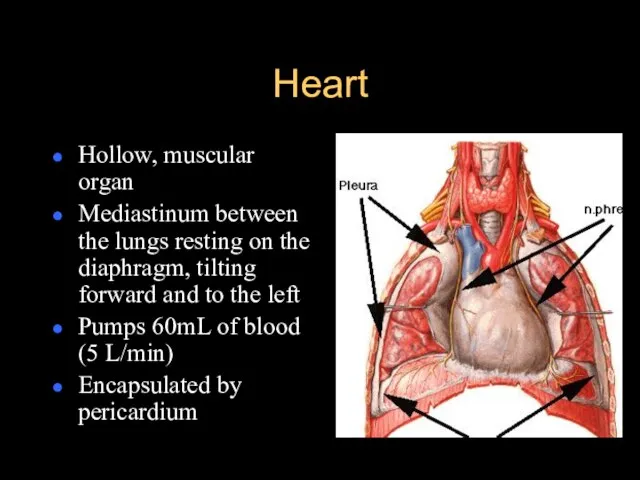
forward and to the left
Pumps 60mL of blood (5 L/min)
Encapsulated by pericardium
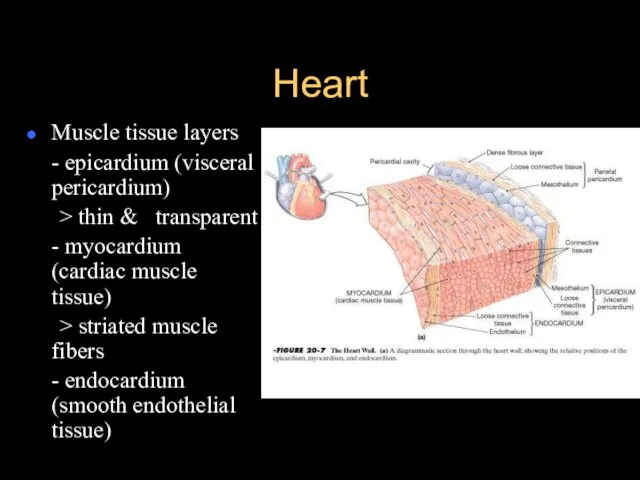
Слайд 3Heart
Muscle tissue layers
- epicardium (visceral pericardium)
> thin & transparent
- myocardium (cardiac muscle
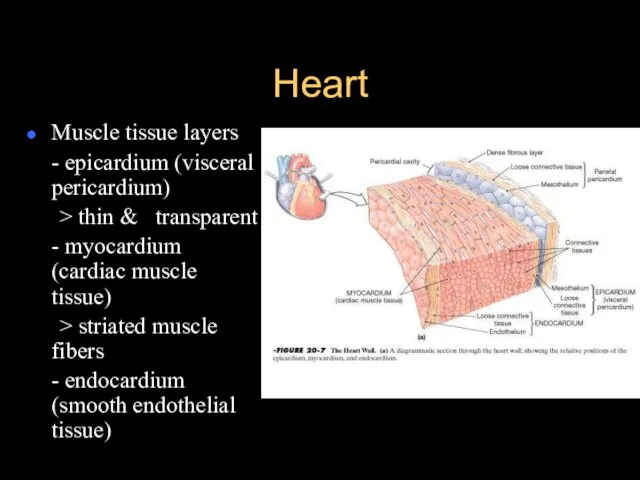
tissue)
> striated muscle fibers
- endocardium (smooth endothelial tissue)
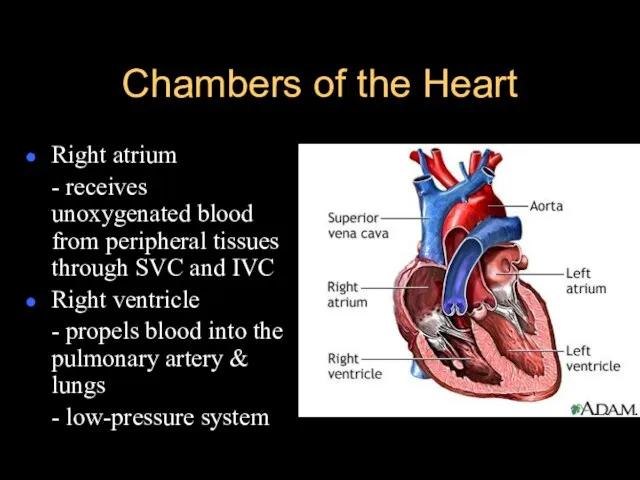
Слайд 4Chambers of the Heart
Right atrium
- receives unoxygenated blood from peripheral tissues through
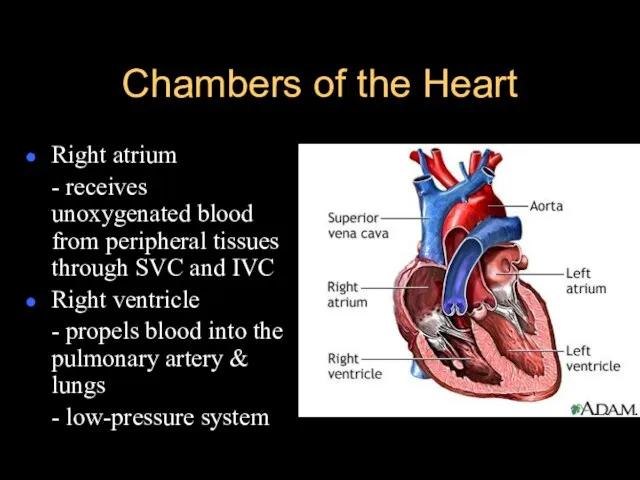
SVC and IVC
Right ventricle
- propels blood into the pulmonary artery & lungs
- low-pressure system
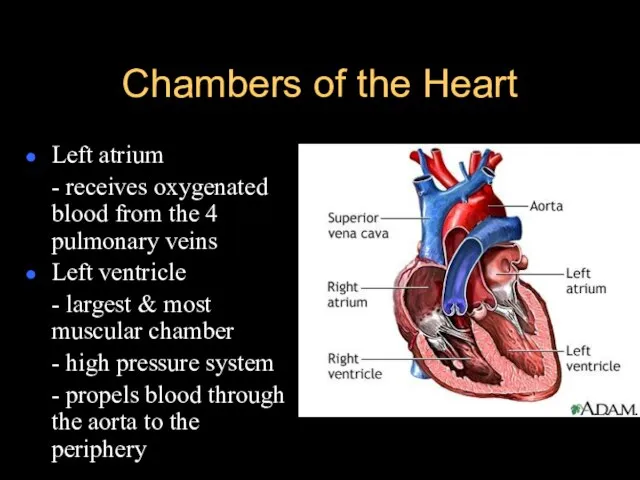
Слайд 5Chambers of the Heart
Left atrium
- receives oxygenated blood from the 4 pulmonary
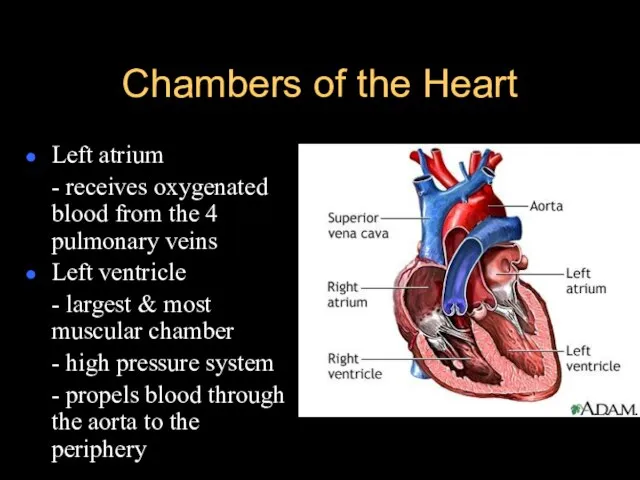
veins
Left ventricle
- largest & most muscular chamber
- high pressure system
- propels blood through the aorta to the periphery
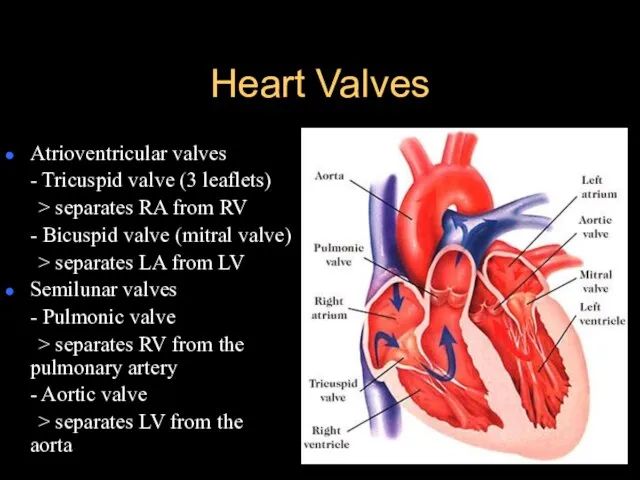
Слайд 6Heart Valves
Atrioventricular valves
- Tricuspid valve (3 leaflets)
> separates RA from RV
- Bicuspid
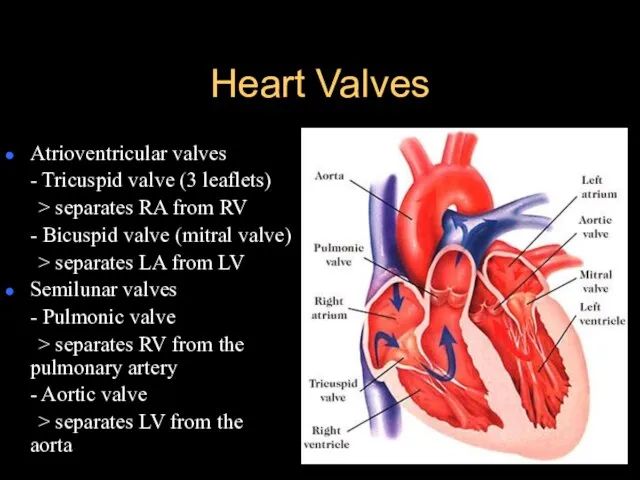
valve (mitral valve)
> separates LA from LV
Semilunar valves
- Pulmonic valve
> separates RV from the pulmonary artery
- Aortic valve
> separates LV from the aorta
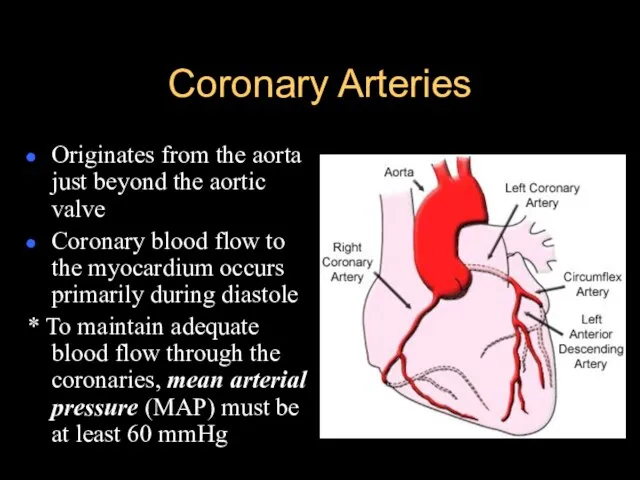
Слайд 7Coronary Arteries
Originates from the aorta just beyond the aortic valve
Coronary blood flow
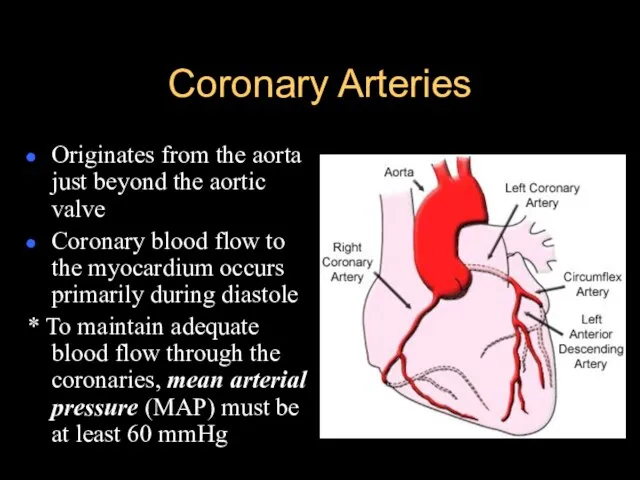
to the myocardium occurs primarily during diastole
* To maintain adequate blood flow through the coronaries, mean arterial pressure (MAP) must be at least 60 mmHg
Слайд 8Coronary Arteries
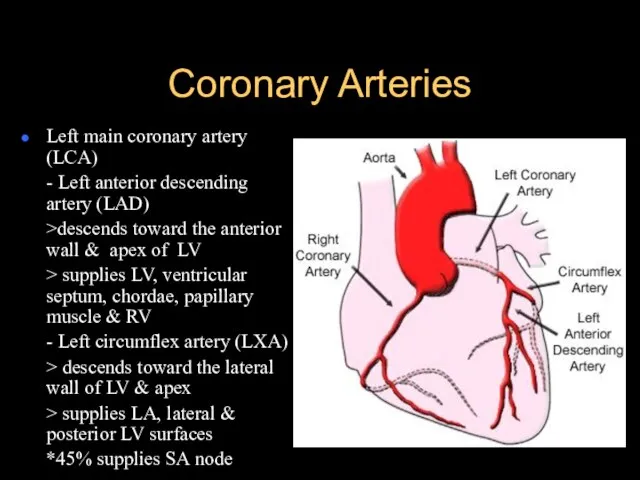
Left main coronary artery (LCA)
- Left anterior descending artery (LAD)
>descends toward
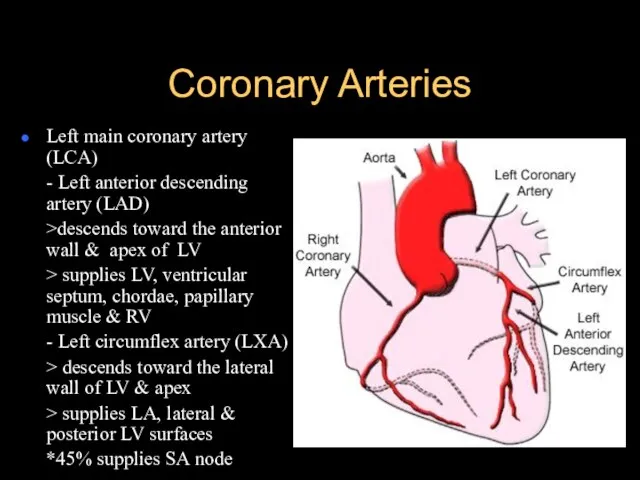
the anterior wall & apex of LV
> supplies LV, ventricular septum, chordae, papillary muscle & RV
- Left circumflex artery (LXA)
> descends toward the lateral wall of LV & apex
> supplies LA, lateral & posterior LV surfaces
*45% supplies SA node
Слайд 9Coronary Arteries
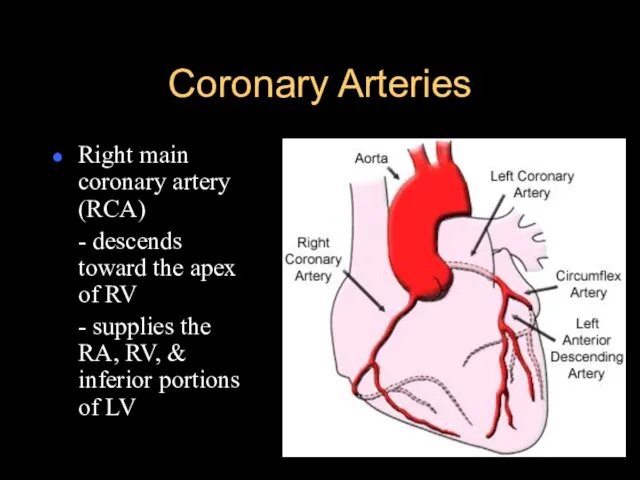
Right main coronary artery (RCA)
- descends toward the apex of RV
-
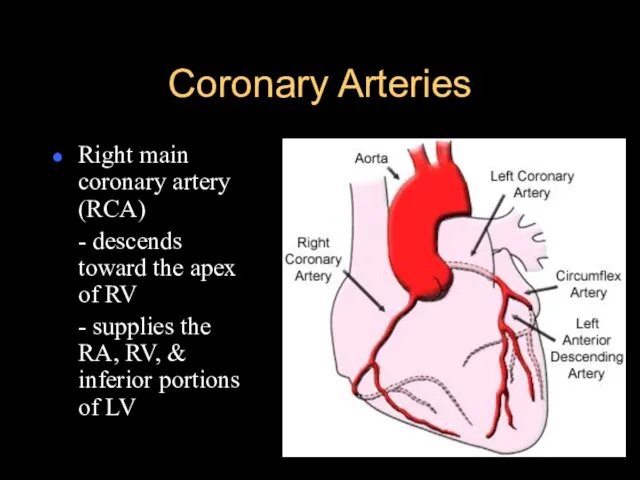
supplies the RA, RV, & inferior portions of LV
Слайд 11Physiology of the Heart
Electrophysiologic properties (regulates heart rate & rhythm)
- Automaticity –
ability of all cardiac cells to initiate an impulse spontaneously & repetitively
- Excitability – ability of cardiac cells to respond to stimulus by initiating an impulse (depolarization)
- Conductivity – cardiac cells transmit the electrical impulses they receive
- Contractility – cardiac cells contract in response to an impulse
- Refractoriness – cardiac cells are unable to respond to a stimulus until they’ve recovered (repolarized)
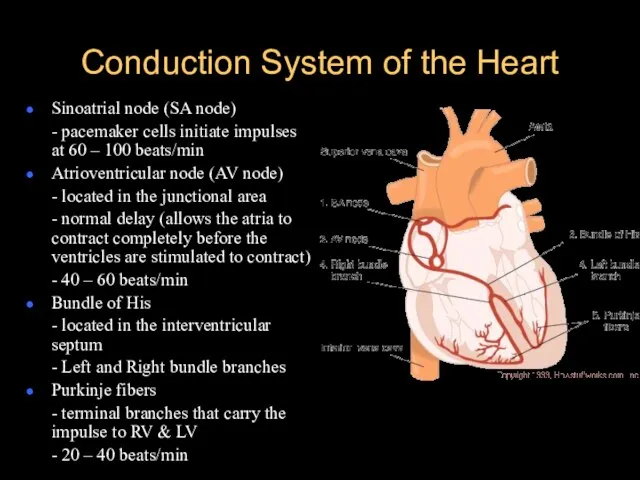
Слайд 12Conduction System of the Heart
Sinoatrial node (SA node)
- pacemaker cells initiate impulses
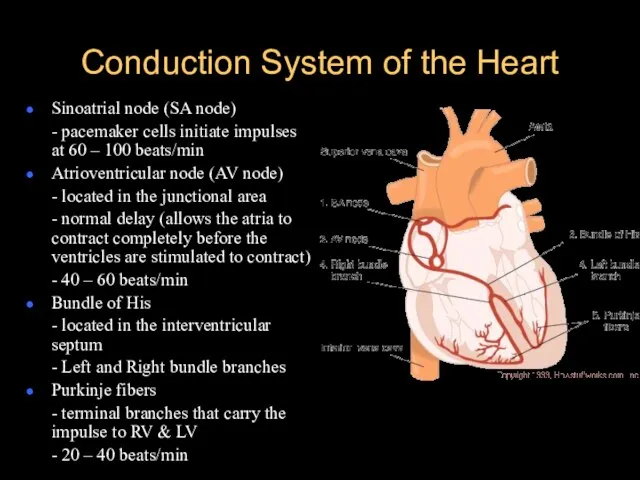
at 60 – 100 beats/min
Atrioventricular node (AV node)
- located in the junctional area
- normal delay (allows the atria to contract completely before the ventricles are stimulated to contract)
- 40 – 60 beats/min
Bundle of His
- located in the interventricular septum
- Left and Right bundle branches
Purkinje fibers
- terminal branches that carry the impulse to RV & LV
- 20 – 40 beats/min
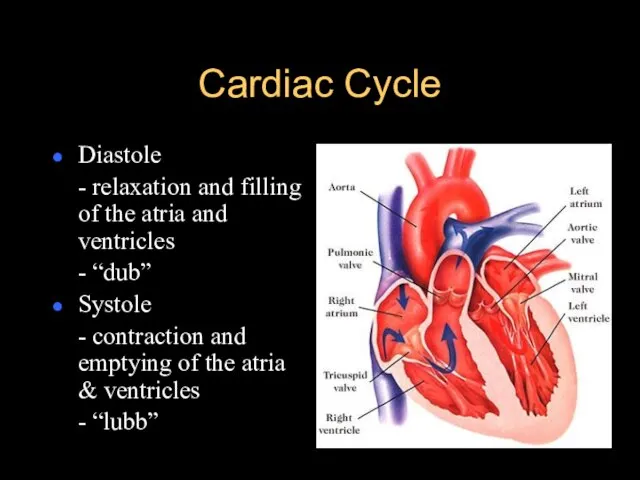
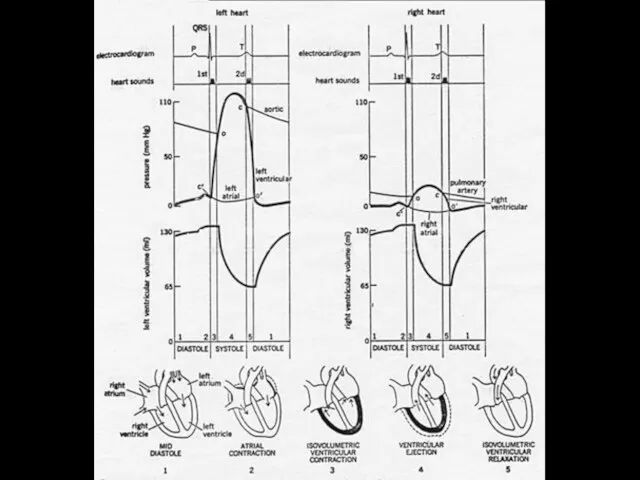
Слайд 13Cardiac Cycle
Diastole
- relaxation and filling of the atria and ventricles
- “dub”
Systole
-
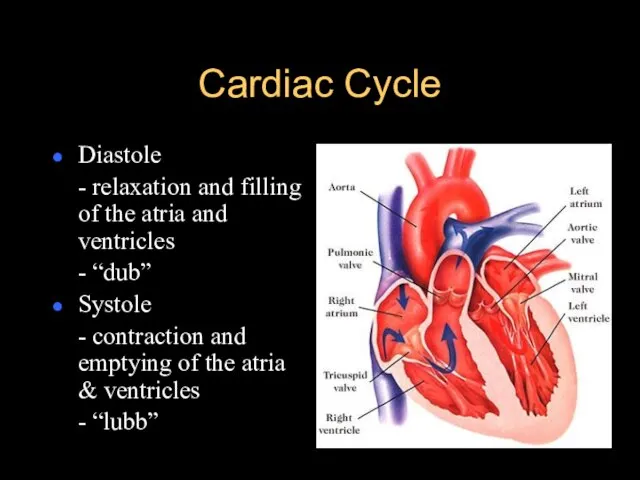
contraction and emptying of the atria & ventricles
- “lubb”
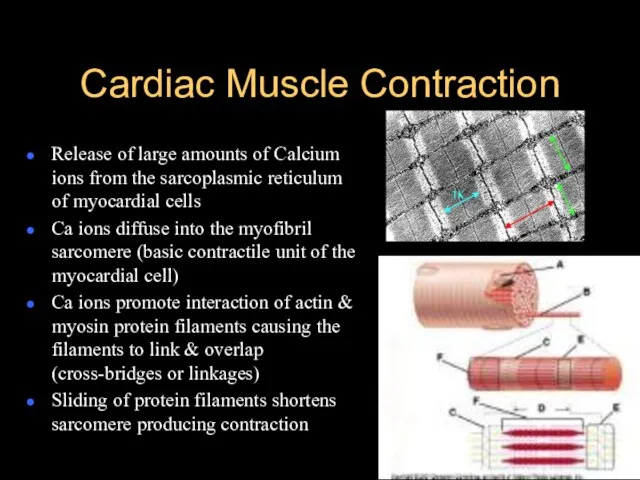
Слайд 15Cardiac Muscle Contraction
Release of large amounts of Calcium ions from the sarcoplasmic
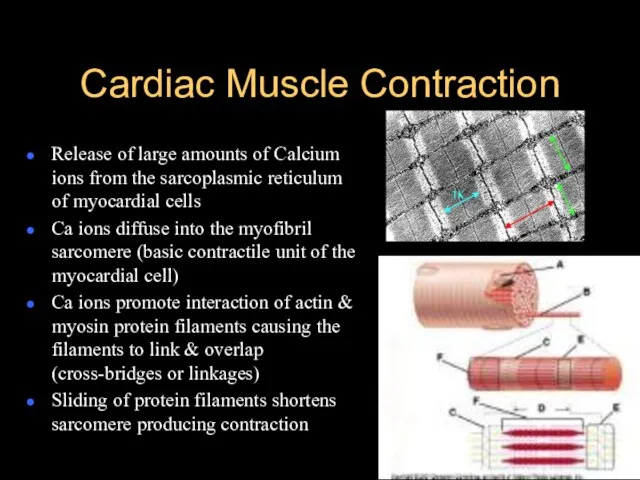
reticulum of myocardial cells
Ca ions diffuse into the myofibril sarcomere (basic contractile unit of the myocardial cell)
Ca ions promote interaction of actin & myosin protein filaments causing the filaments to link & overlap (cross-bridges or linkages)
Sliding of protein filaments shortens sarcomere producing contraction
Слайд 16Mechanical Properties of the Heart
Cardiac output
- volume of blood (liters) ejected by
the heart each minute
- 4 – 7 L/min
- heart rate x stroke volume
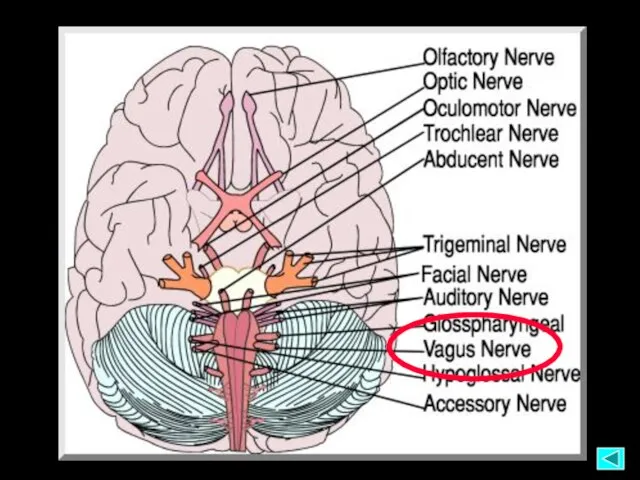
Heart rate
- number of times the ventricles contract each minute
- 60 – 100 beats/min
- controlled by the ANS via the vagus nerve
Stroke volume
- amount of blood ejected by the LV during each systole
Слайд 17Mechanical Properties of the Heart
Preload
- degree of myocardial stretch at the end
of diastole & just before contraction
- determined by the amount of blood returning to the heart from the venous ® & pulmonary system (L) – LVED
*Starling’s law – the more the heart is filled during diastole, the more forcefully it contracts
Слайд 18Mechanical Properties of the Heart
Afterload
- pressure or resistance that the ventricles must
overcome to eject blood through the semilunar valves & into the peripheral blood vessels
- directly proportional to the BP & diameter of blood vessels
Impedance (peripheral component of afterload)
- pressure that the heart must overcome to open the aortic valve
- depends on aortic compliance, blood viscosity & arteriolar constriction
Слайд 19Mechanical Properties of the Heart
Myocardial contractility
- force of cardiac contraction independent of
preload
- increased by sympathetic nervous stimulation, calcium release & positive inotropic drugs
- decreased by hypoxemia & acidemia
Слайд 20Vascular System
Provide conduits for blood to travel from the heart to nourish
the body
Carry cellular wastes to the excretory organs
Allow lymphatic flow to drain tissue fluid back to the circulation
Return blood to the heart for recirculation
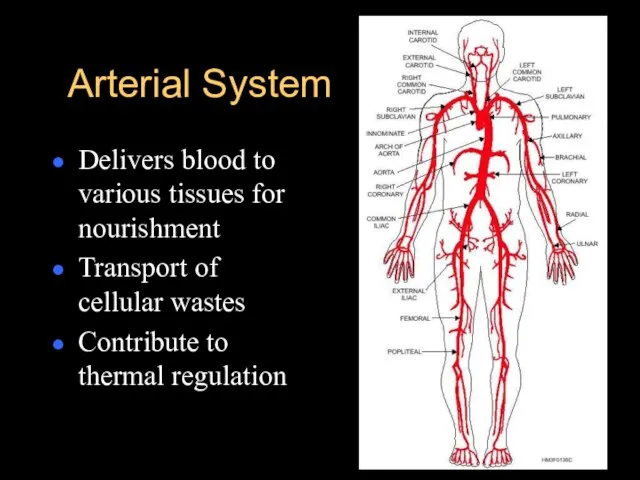
Слайд 21Arterial System
Delivers blood to various tissues for nourishment
Transport of cellular wastes
Contribute to
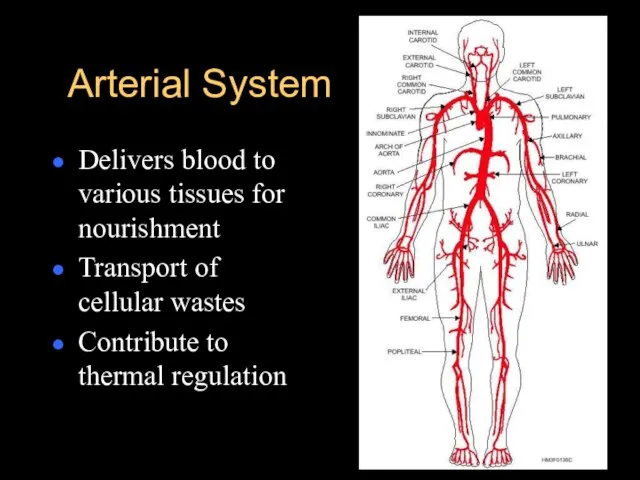
thermal regulation
Слайд 22Arterial System
Blood pressure
- force of blood exerted against the vessel walls
= CO
x peripheral vascular resistance
- regulated by:
> autonomic nervous system (ANS)
> kidneys (renin-angiotensin-aldosterone)
> endocrine system (catecholamines, kinins, serotonin, histamine)
Слайд 23Blood Pressure
Systolic:
- amount of pressure/force generated by LV to distribute blood
into the aorta w/ each contraction of the heart
- 90 – 135 mmHg (120)
- affected by CO and arterial distention
Diastolic:
- amount of pressure/force sustained by the arteries during the relaxation phase of the heart
- ability of the heart to rest while filling with blood
- affected by peripheral vascular resistance
- 60 – 85 mmHg (80)
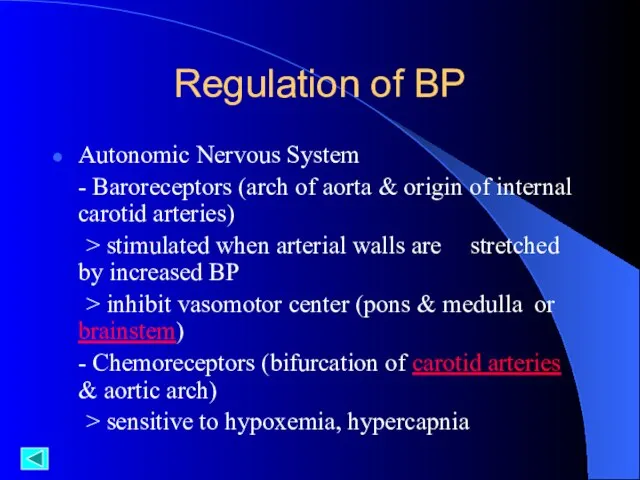
Слайд 24Regulation of BP
Autonomic Nervous System
- Baroreceptors (arch of aorta & origin of
internal carotid arteries)
> stimulated when arterial walls are stretched by increased BP
> inhibit vasomotor center (pons & medulla or brainstem)
- Chemoreceptors (bifurcation of carotid arteries & aortic arch)
> sensitive to hypoxemia, hypercapnia
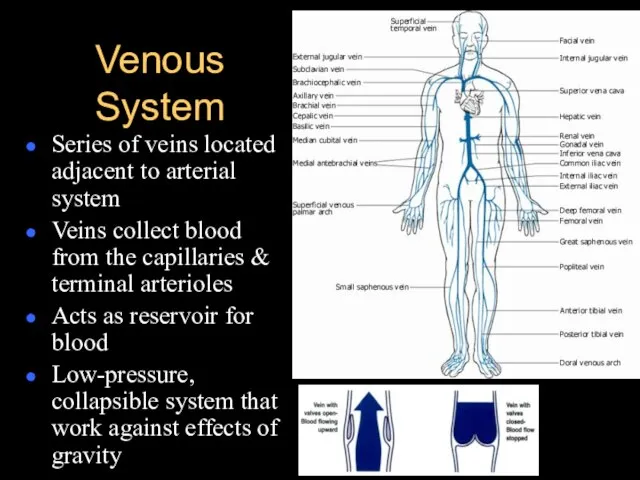
Слайд 25Venous System
Series of veins located adjacent to arterial system
Veins collect blood from
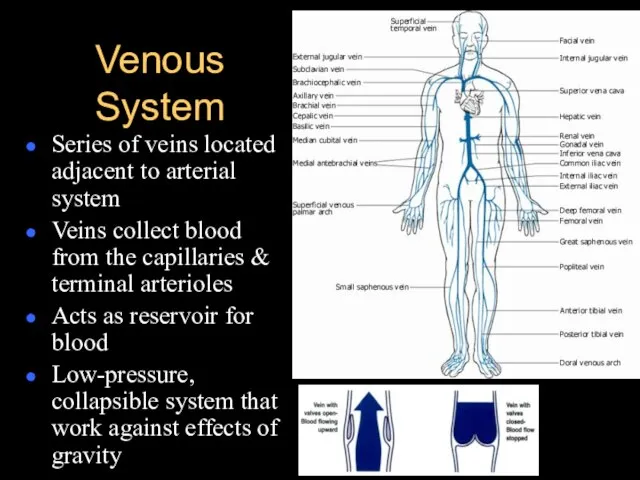
the capillaries & terminal arterioles
Acts as reservoir for blood
Low-pressure, collapsible system that work against effects of gravity
 «Обзор законодательства Республики Казахстан в сфере социальной поддержки и обеспечения социальными услугами»
«Обзор законодательства Республики Казахстан в сфере социальной поддержки и обеспечения социальными услугами» Роспись петуха по мотивам Филимоновской росписи
Роспись петуха по мотивам Филимоновской росписи Гражданское право. Понятие и виды сроков в гражданском праве
Гражданское право. Понятие и виды сроков в гражданском праве Модернизм
Модернизм Какие фигуры изображены на рисунке ?
Какие фигуры изображены на рисунке ? Перенос слова переносятся по слогам
Перенос слова переносятся по слогам Принтеры
Принтеры Методическая разработка «Создание презентаций» Элективный курс для 10 класса.
Методическая разработка «Создание презентаций» Элективный курс для 10 класса. Вейк-лебедка - летний бизнес. Вейкпарк в пляжной зоне
Вейк-лебедка - летний бизнес. Вейкпарк в пляжной зоне Федеральное Собрание РФ
Федеральное Собрание РФ Инжиниринг нефтехимии и нефтегазопереработки
Инжиниринг нефтехимии и нефтегазопереработки Китайский клуб МИИТа
Китайский клуб МИИТа Мой город, с тебя начинается Родина (город Сатка)
Мой город, с тебя начинается Родина (город Сатка) Спартакиада пенсионеров муниципального образования Город Гатчина
Спартакиада пенсионеров муниципального образования Город Гатчина Эры. Основные события органического мира
Эры. Основные события органического мира Презентация на тему Операционные системы на мобильных устройствах
Презентация на тему Операционные системы на мобильных устройствах  Живопись
Живопись Михайленко Юлия Борисовна учитель начальных классов ГБОУ гимназии № 1518 г. Москвы
Михайленко Юлия Борисовна учитель начальных классов ГБОУ гимназии № 1518 г. Москвы Муниципальное общеобразовательное учреждение лингвистическая гимназия № 70
Муниципальное общеобразовательное учреждение лингвистическая гимназия № 70 МОСКВА- ГОРОД ГЕРОЙ . Битва за Москву(30 сентября 1941- 20 апреля 1942)
МОСКВА- ГОРОД ГЕРОЙ . Битва за Москву(30 сентября 1941- 20 апреля 1942) Векторы в пространстве и не только
Векторы в пространстве и не только Презентация на тему История развития отечественной вычислительной техники
Презентация на тему История развития отечественной вычислительной техники Трансформация изображения через трансформацию формы - серия открыток
Трансформация изображения через трансформацию формы - серия открыток ОРНАМЕНТЫ в национальном костюме
ОРНАМЕНТЫ в национальном костюме Цветник для солнечного места “Степной бриз ”
Цветник для солнечного места “Степной бриз ” Презентация на тему Тургенев. Стихи в прозе
Презентация на тему Тургенев. Стихи в прозе 287 Воскресшему служу я
287 Воскресшему служу я Берлину заменить Северный поток-2 другим проектом
Берлину заменить Северный поток-2 другим проектом