Содержание
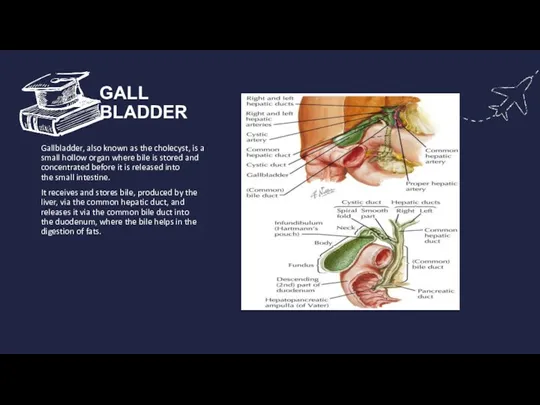
- 2. GALL BLADDER Gallbladder, also known as the cholecyst, is a small hollow organ where bile is
- 3. CHOLECYSTITIS Cholecystitis or infl ammation of the gallbladder may be acute, chronic, or acute superimposed on
- 4. CAUSES SEVERE ILLNESS BILE DUCT BLOCKAGE INFECTION TUMOR GALLSTONES
- 5. TYPES OF CHOLECYSTITIS CHRONIC ACUTE
- 6. CHRONIC CHOLECYSTITIS Chronic cholecystitis is the commonest type of clinical gallbladder disease. Th ere is almost
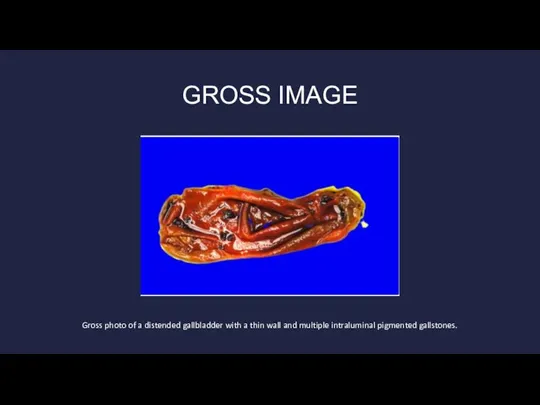
- 7. GROSS IMAGE Gross photo of a distended gallbladder with a thin wall and multiple intraluminal pigmented
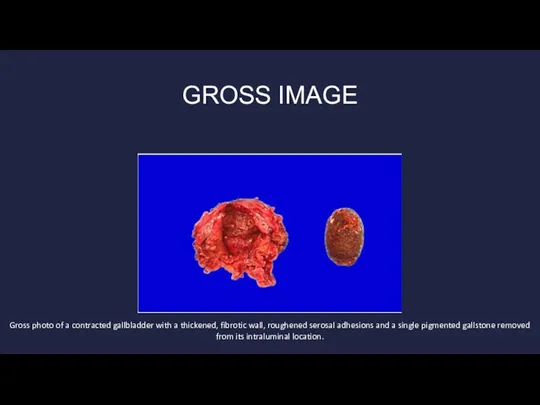
- 8. GROSS IMAGE Gross photo of a contracted gallbladder with a thickened, fibrotic wall, roughened serosal adhesions
- 9. MORPHOLOGIC FEATURES The gallbladder is generally contracted but may be normal or enlarged . The wall
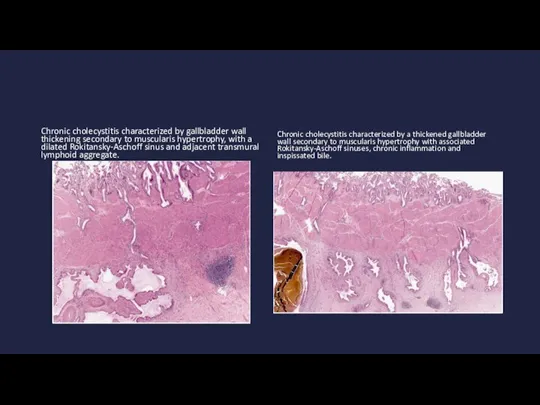
- 10. Chronic cholecystitis characterized by gallbladder wall thickening secondary to muscularis hypertrophy, with a dilated Rokitansky-Aschoff sinus
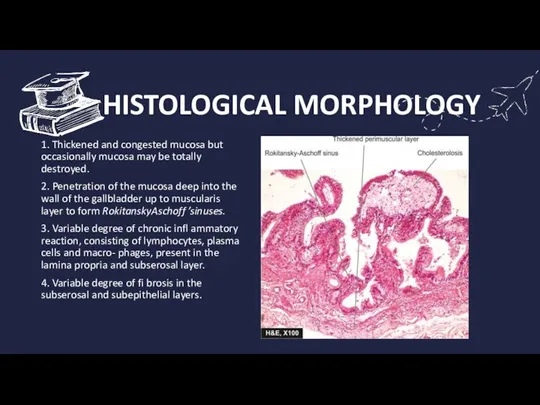
- 11. HISTOLOGICAL MORPHOLOGY 1. Thickened and congested mucosa but occasionally mucosa may be totally destroyed. 2. Penetration
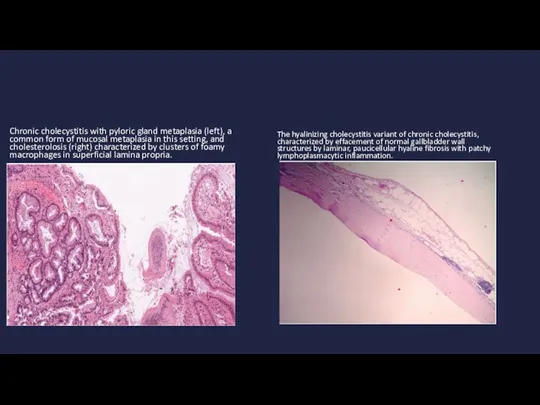
- 12. Chronic cholecystitis with pyloric gland metaplasia (left), a common form of mucosal metaplasia in this setting,
- 13. A few morphologic variants of chronic chole cystitis are considered below: Cholecystitis glandularis, when the mucosal
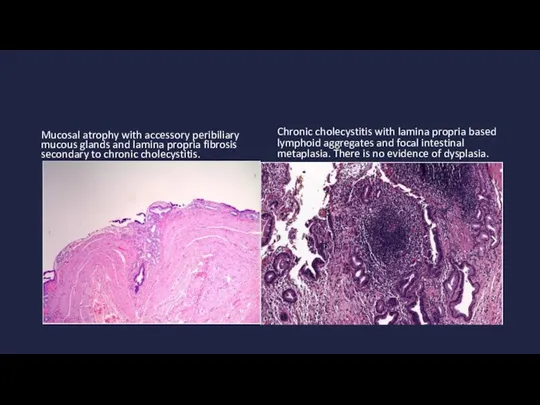
- 14. Mucosal atrophy with accessory peribiliary mucous glands and lamina propria fibrosis secondary to chronic cholecystitis. Chronic
- 15. Complications If untreated, cholecystitis can lead to a number of serious complications, including: Infection within the
- 16. PREVENTION You can reduce your risk of cholecystitis by taking the following steps to prevent gallstones:
- 17. DIAGONISTIC To diagnose cholecystis, your health care provider will likely do a physical exam and discuss
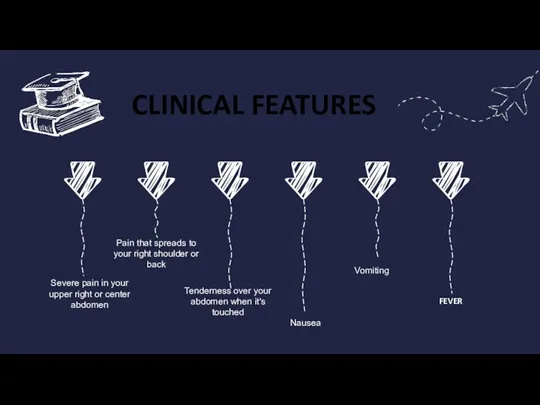
- 18. CLINICAL FEATURES Vomiting Tenderness over your abdomen when it's touched Nausea Pain that spreads to your
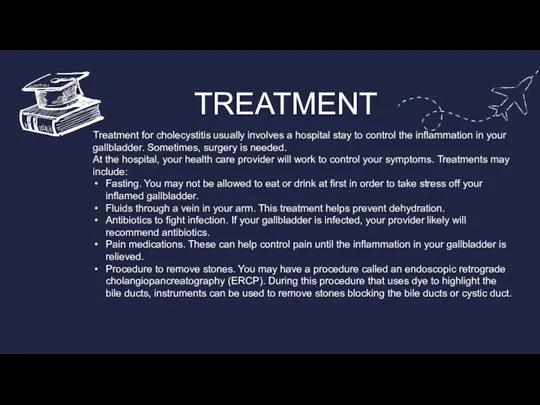
- 19. TREATMENT Treatment for cholecystitis usually involves a hospital stay to control the inflammation in your gallbladder.
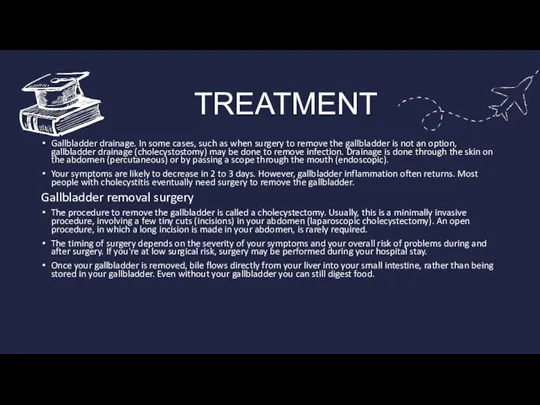
- 20. TREATMENT Gallbladder drainage. In some cases, such as when surgery to remove the gallbladder is not
- 22. Скачать презентацию

 АССОЦИАЦИЯ
АССОЦИАЦИЯ Культура и Религия Японии
Культура и Религия Японии Поиск информации в сети Интернет Катерина Ефимова «Информационная эвристика» НБ УрГУ
Поиск информации в сети Интернет Катерина Ефимова «Информационная эвристика» НБ УрГУ Игра – это огромное светлое окно, через которое в духовный мир ребенка вливается живительный поток представлений, понятий об окру
Игра – это огромное светлое окно, через которое в духовный мир ребенка вливается живительный поток представлений, понятий об окру Классный час о противопожарной безопасности
Классный час о противопожарной безопасности Презентация на тему Музейная практика как средство воспитания толерантности у обучающихся
Презентация на тему Музейная практика как средство воспитания толерантности у обучающихся Франция в 1848 – 1870 годах
Франция в 1848 – 1870 годах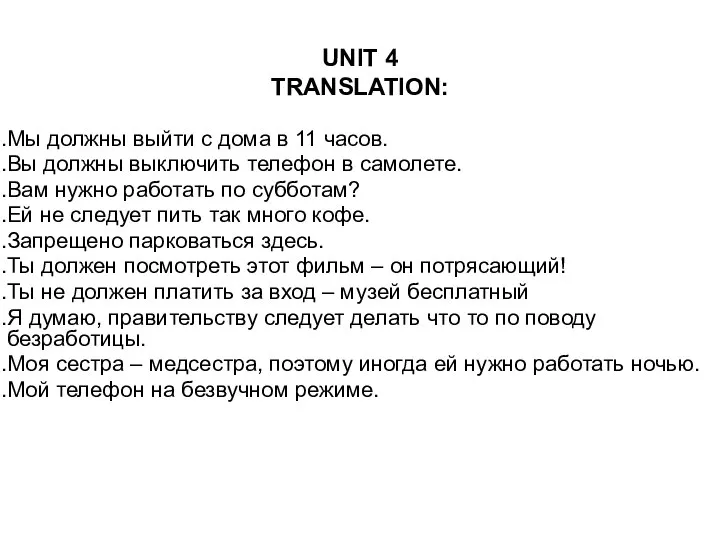 Unit 4 translation
Unit 4 translation Д.Б.Кабалевский - музыкант и педагог
Д.Б.Кабалевский - музыкант и педагог Факультет Управления Кафедра маркетинга и рекламы Группа 13 Панченко Ирина
Факультет Управления Кафедра маркетинга и рекламы Группа 13 Панченко Ирина Концепция и структура курса ОРКиСЭ
Концепция и структура курса ОРКиСЭ Экспертное решение в сфере ремонта. СанПро43
Экспертное решение в сфере ремонта. СанПро43 Природно-ресурсный потенциал России
Природно-ресурсный потенциал России Правила компьютерного набора текста
Правила компьютерного набора текста Влияние англоязычных названий, связанных с космической тематикой, на русский язык
Влияние англоязычных названий, связанных с космической тематикой, на русский язык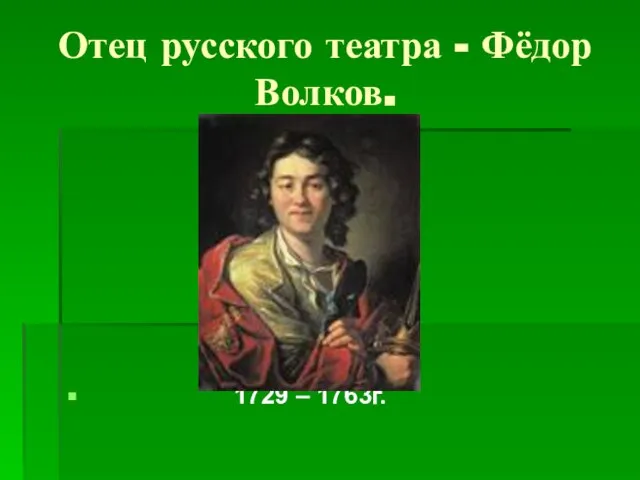 Отец русского театра - Фёдор Волков
Отец русского театра - Фёдор Волков Управление временем
Управление временем Наладка станков с ЧПУ
Наладка станков с ЧПУ Автоматизация звука «Л» в чистоговорках Презентацию подготовила учитель – логопед ГОУ №657 г. Санкт - Петербурга Агельярова Е.В.
Автоматизация звука «Л» в чистоговорках Презентацию подготовила учитель – логопед ГОУ №657 г. Санкт - Петербурга Агельярова Е.В. Кто?Что?Когда?Где?Почему?. Таблица Донны Огл ЗнаюХочу узнатьУзнал Категории информации, которыми мы намерены пользоваться Источни
Кто?Что?Когда?Где?Почему?. Таблица Донны Огл ЗнаюХочу узнатьУзнал Категории информации, которыми мы намерены пользоваться Источни Autumn in Prague
Autumn in Prague 1709 — 2009 « ДЕЛО БЫЛО ПОД ПОЛТАВОЙ… »
1709 — 2009 « ДЕЛО БЫЛО ПОД ПОЛТАВОЙ… » Лавсан
Лавсан Техники подъёмов и спусков на лыжах
Техники подъёмов и спусков на лыжах Королевская семья Великобритании
Королевская семья Великобритании Утренние ритуалы для комфортного перехода на новый уровень
Утренние ритуалы для комфортного перехода на новый уровень Перелёты птиц
Перелёты птиц Как мотивировать детей на учебную деятельность
Как мотивировать детей на учебную деятельность