Содержание
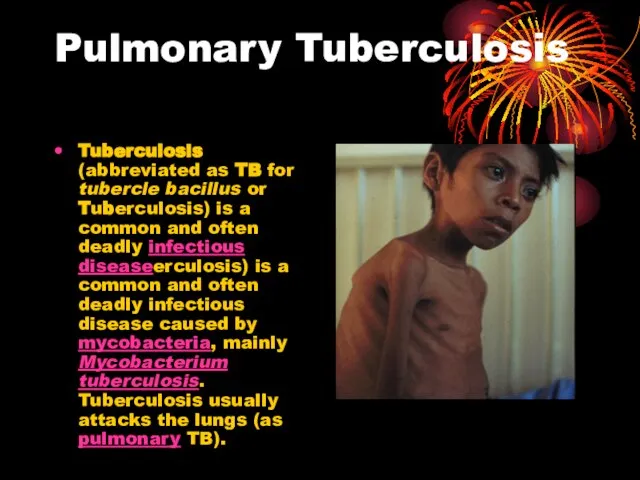
- 2. Pulmonary Tuberculosis Tuberculosis (abbreviated as TB for tubercle bacillus or Tuberculosis) is a common and often
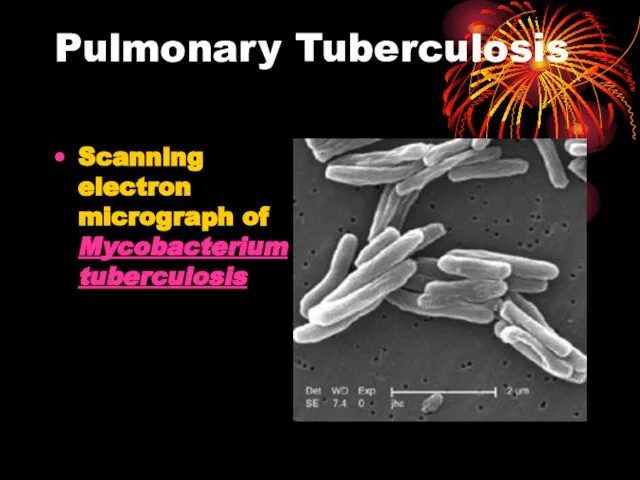
- 3. Pulmonary Tuberculosis Scanning electron micrograph of Mycobacterium tuberculosis
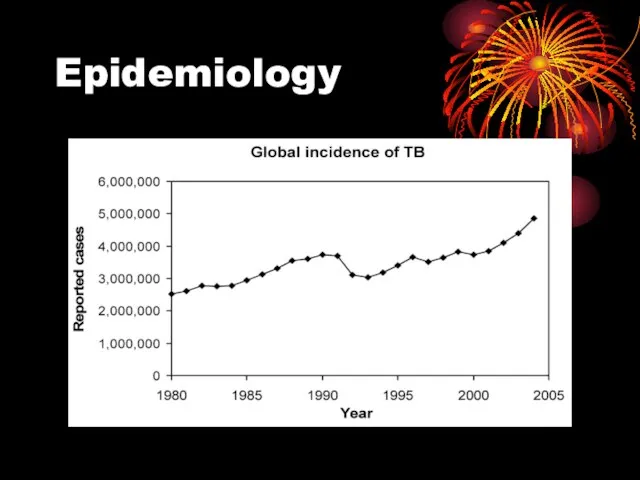
- 4. Epidemiology According to the World Health Organization (WHO), nearly 2 billion people—one third of the world's
- 5. Epidemiology Most common infectious cause of death worldwide Latent phase of TB enabled it to spread
- 6. Epidemiology
- 7. Epidemiology Major changes in trends secondary to HIV - 1953-1985 cases decreased from 84,304 to 22,201
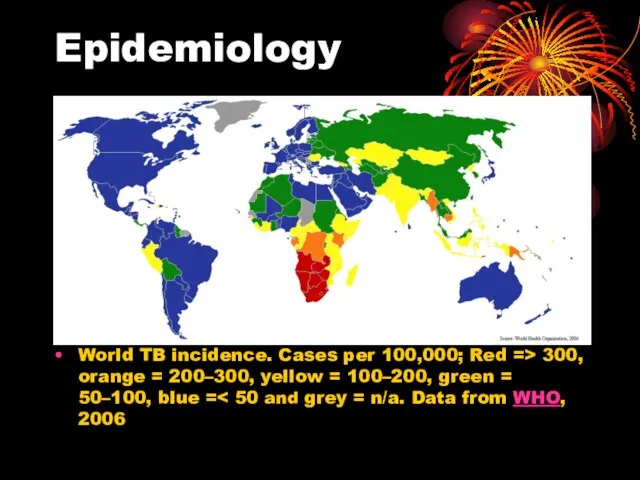
- 8. Epidemiology World TB incidence. Cases per 100,000; Red => 300, orange = 200–300, yellow = 100–200,
- 9. Incidence 1985-1990 TB cases increased 55% in Hispanics and 27% in African Americans Populations at risk
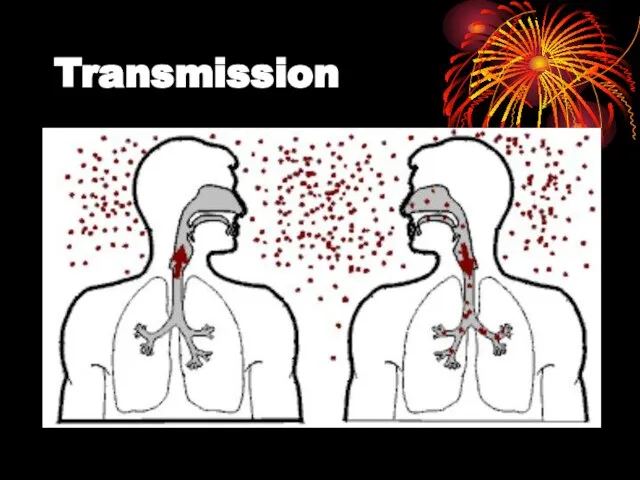
- 10. Transmission When people suffering from active pulmonary TB cough, sneeze, speak, or spit, they expel infectious
- 11. Transmission
- 12. Transmission people who inject drugs using unsanitary needles, residents and employees of high-risk congregate settings, medically
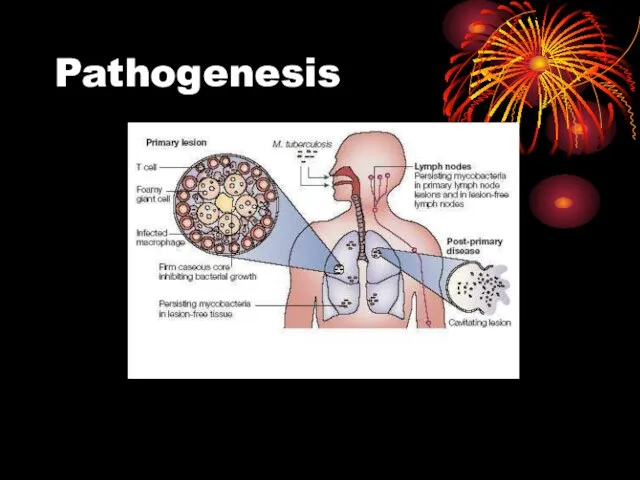
- 13. Pathogenesis
- 14. Pathogenesis Hyperlink to Microsoft Word Pathophysiology of Pulmonary Tuberculosis.doc Pathogenesis of TB infection and disease.doc
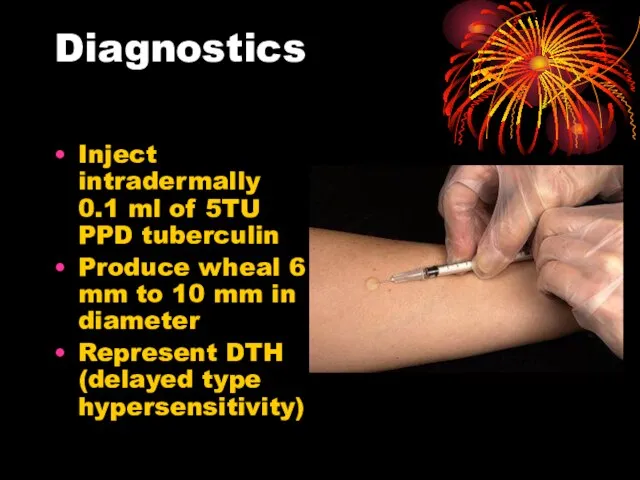
- 15. Diagnostics Inject intradermally 0.1 ml of 5TU PPD tuberculin Produce wheal 6 mm to 10 mm
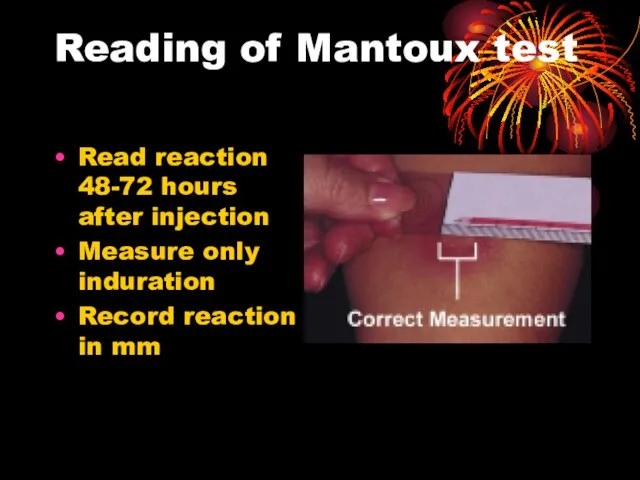
- 16. Reading of Mantoux test Read reaction 48-72 hours after injection Measure only induration Record reaction in
- 17. Classifying the Tuberculin Reaction >5 mm is classified as positive in HIV-positive persons Recent contacts of
- 18. Classifying the tuberculin reaction >10 mm is classified as positive in Recent arrivals from high-prevalence countries
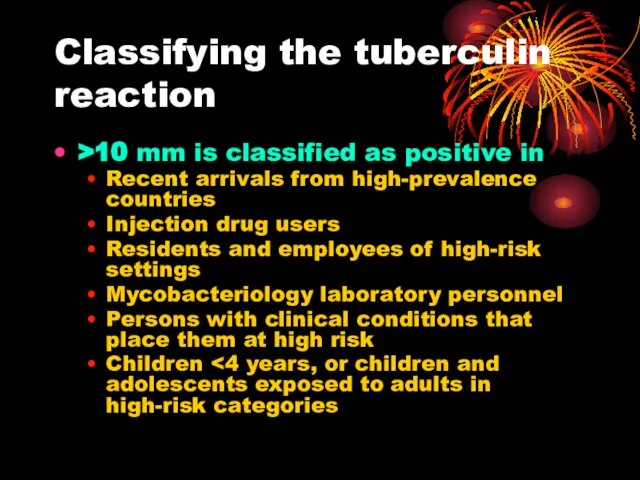
- 19. Classifying the tuberculin reaction >15 mm is classified as positive in Persons with no known risk
- 20. Factors may affect TST False negative Faulty application Anergy Acute TB (2-10 wks to convert) Very
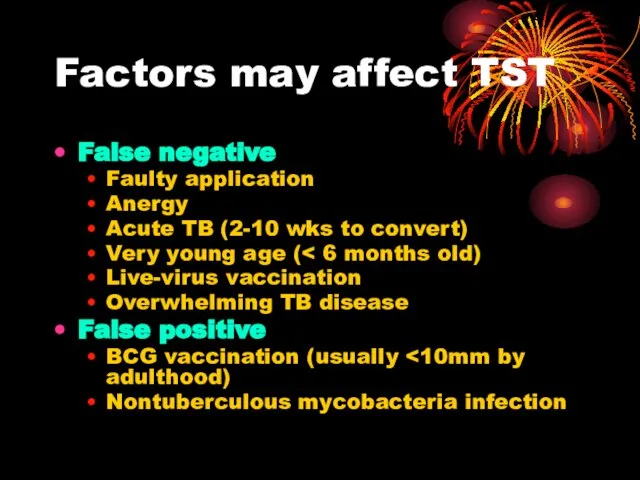
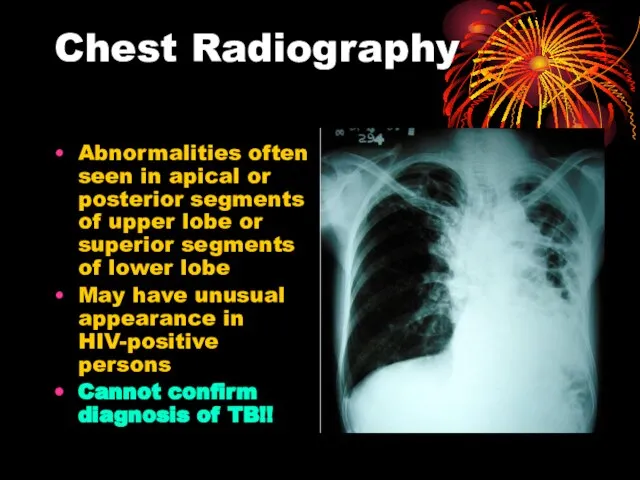
- 21. Chest Radiography Abnormalities often seen in apical or posterior segments of upper lobe or superior segments
- 22. Chest radiography No chest X-ray pattern is absolutely typical of TB 10-15% of culture-positive TB patients
- 23. Specimen Collection Obtain 3 sputum specimens for smear examination and culture Persons unable to cough up
- 24. Number of sputum samples required overall diagnostic yield for sputum examination related to the quantity of
- 25. Smear Examination Strongly consider TB in patients with smears containing acid-fast bacilli (AFB) Results should be
- 26. AFB smear Mycobacterium tuberculosis (stained red) in sputum
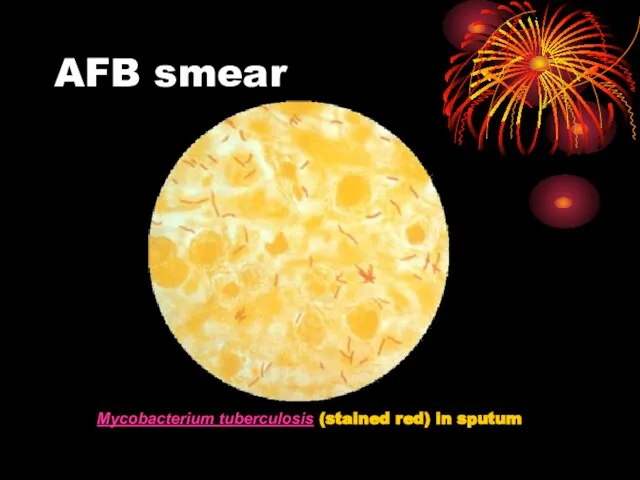
- 27. Cultures
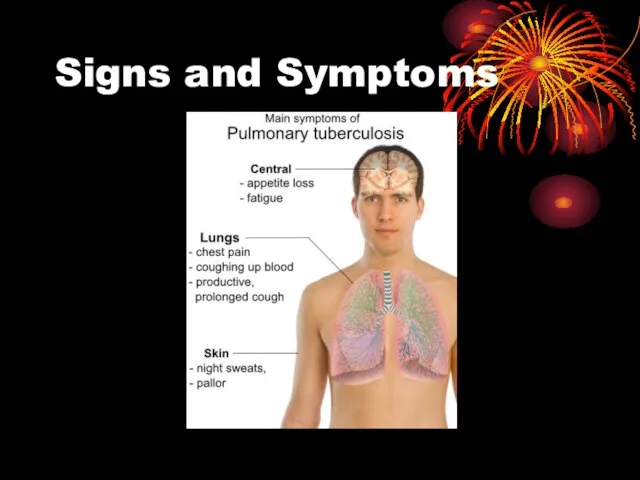
- 28. Signs and Symptoms
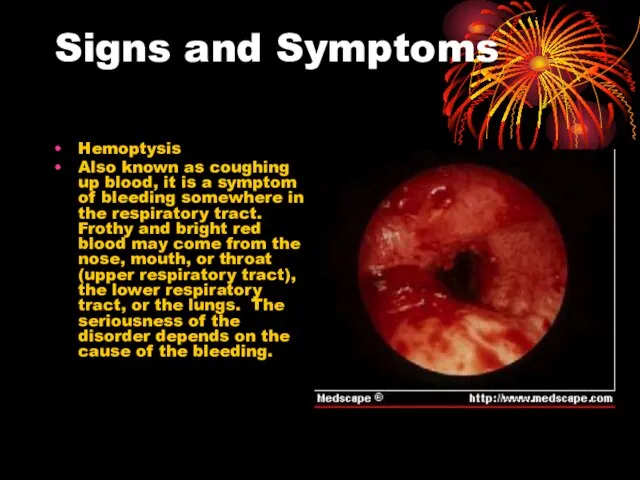
- 29. Signs and Symptoms Hemoptysis Also known as coughing up blood, it is a symptom of bleeding
- 30. Signs and Symptoms Anorexia The sysmptom of poor appetite whatever the cause
- 31. Treatment
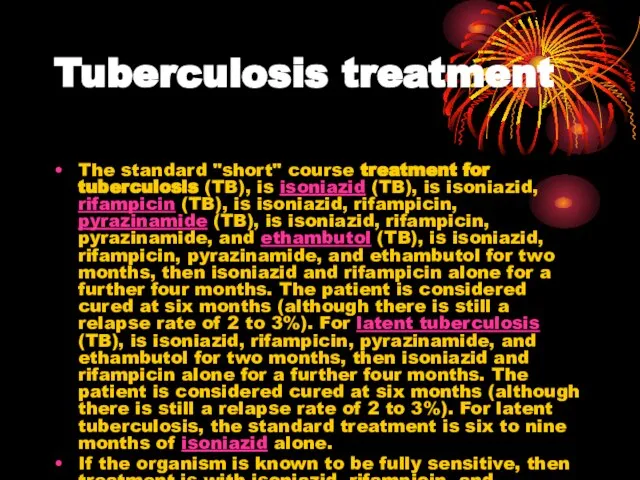
- 32. Tuberculosis treatment The standard "short" course treatment for tuberculosis (TB), is isoniazid (TB), is isoniazid, rifampicin
- 33. Drugs All first-line anti-tuberculous drug names have a standard three-letter and a single-letter abbreviation: ethambutol is
- 34. Drugs There are six classes of second-line drugs (SLDs) used for the treatment of TB. A
- 35. Drugs considered "third-line drugs" not very effective or because their efficacy has not been proven .
- 36. Drugs Daily Dose of TB Drugs
- 37. Drugs Multi-drug resistant TB (MDR-TB) is defined as resistance to the two most effective first-line TB
- 38. Monitoring and DOTS DOTSDOTS stands for "Directly Observed Therapy, Short-course" and is a major plan in
- 39. Prevention TB prevention and control takes two parallel approaches. In the first, people with TB and
- 40. Vaccines Many countries use Bacillus Calmette-Guérin (BCG) vaccine as part of their TB control programs, especially
- 41. Current Surgical Intervention Patients with hemoptysis first received Bronchial Artery Embolization because of the recurrent hemoptysis.
- 43. Скачать презентацию




 Денежные переводы физических лиц: состояние и тенденции развития (на примере ПАО Сбербанк)
Денежные переводы физических лиц: состояние и тенденции развития (на примере ПАО Сбербанк) Особенности истории информатики
Особенности истории информатики Мотивирование топ-менеджеров в банковской сфере: подходы и инструменты
Мотивирование топ-менеджеров в банковской сфере: подходы и инструменты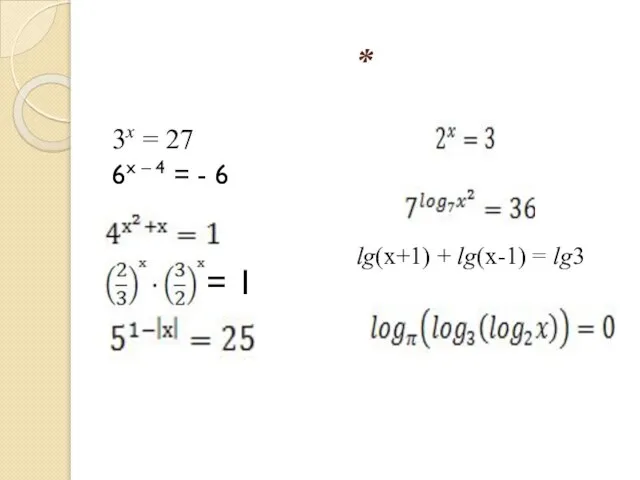 = 1
= 1 Изустная среда мордовского села
Изустная среда мордовского села Показатели рыночной активности
Показатели рыночной активности Выхухоль. Красная книга
Выхухоль. Красная книга Обработка текстовой и графической информации. Создаём комбинированный документ
Обработка текстовой и графической информации. Создаём комбинированный документ Телевидение: я выбираю или меня выбирают. Автор и руководитель проекта: Симонова Ольга Владимировна 2004 год
Телевидение: я выбираю или меня выбирают. Автор и руководитель проекта: Симонова Ольга Владимировна 2004 год Что я сделаю, чтобы доверенный мне магазин стал лучшим на рынке
Что я сделаю, чтобы доверенный мне магазин стал лучшим на рынке Туалетная вода для мужчин Faberlic Intense
Туалетная вода для мужчин Faberlic Intense Межпроцедурные анализы и оптимизации
Межпроцедурные анализы и оптимизации Внешняя политика СССР в 1930-е гг. и накануне Великой Отечественной войны
Внешняя политика СССР в 1930-е гг. и накануне Великой Отечественной войны Урок 3 Человек и Бог в православии-повторение
Урок 3 Человек и Бог в православии-повторение 17 век
17 век ПЕРЕГОВОРЫ
ПЕРЕГОВОРЫ Изготовление вечернего платья
Изготовление вечернего платья Теорiя iгор
Теорiя iгор  Презентация на тему Роль гормонов в обмене веществ, росте и развитии организма биология 8 класс
Презентация на тему Роль гормонов в обмене веществ, росте и развитии организма биология 8 класс аня хочет санчо панчо
аня хочет санчо панчо Создание таблиц в Microsoft Word
Создание таблиц в Microsoft Word Teenagers’ society problems
Teenagers’ society problems Воля познавать
Воля познавать Любимое блюдо моей семьи
Любимое блюдо моей семьи Ладья. Урок №8
Ладья. Урок №8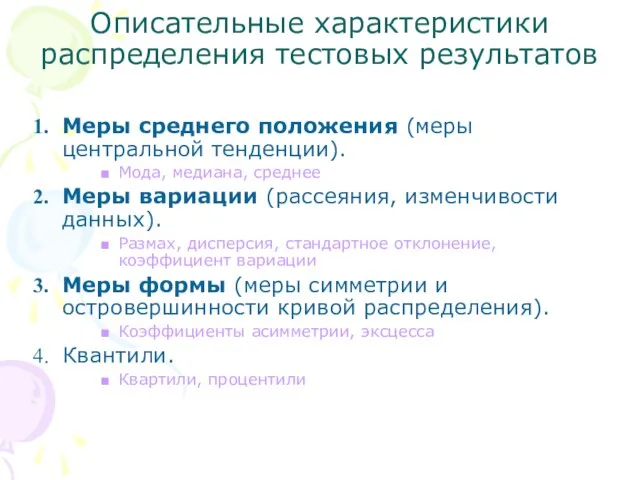 Описательные характеристики распределения тестовых результатов
Описательные характеристики распределения тестовых результатов Презентация на тему Одиночество
Презентация на тему Одиночество Ich gehe mit meine Laterne
Ich gehe mit meine Laterne