Содержание
- 2. Overview Aortic Stenosis Mitral Stenosis Aortic Regurgitation Acute and Chronic Mitral Regurgitation Acute and Chronic
- 3. Etiology Pathophysiology Physical Exam Natural History Testing Treatment
- 4. Aortic Stenosis
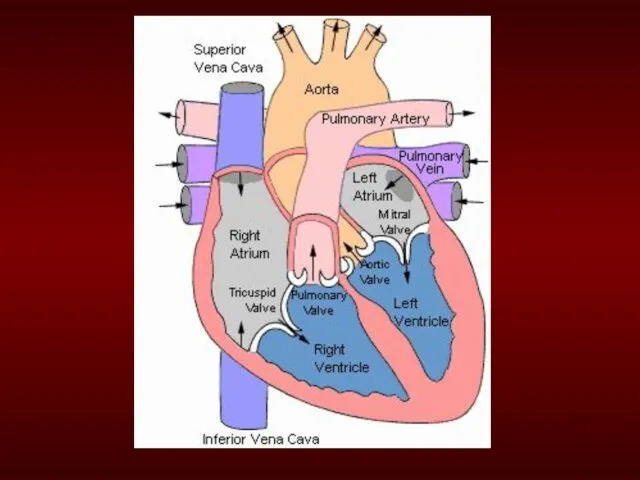
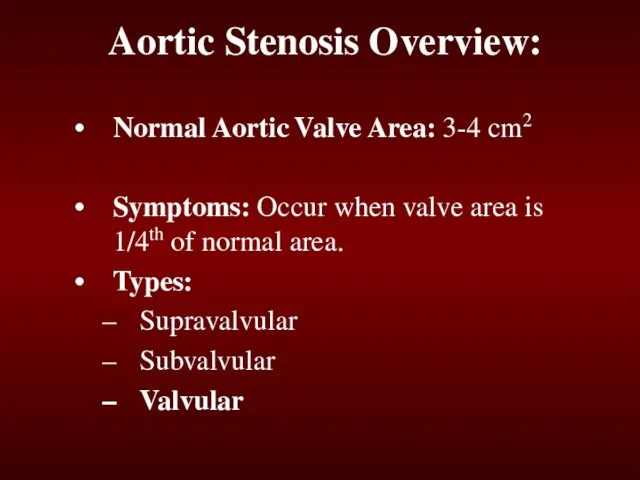
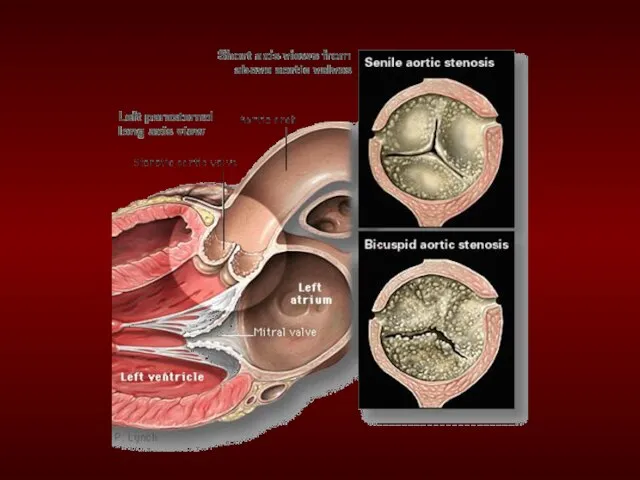
- 6. Aortic Stenosis Overview: Normal Aortic Valve Area: 3-4 cm2 Symptoms: Occur when valve area is 1/4th
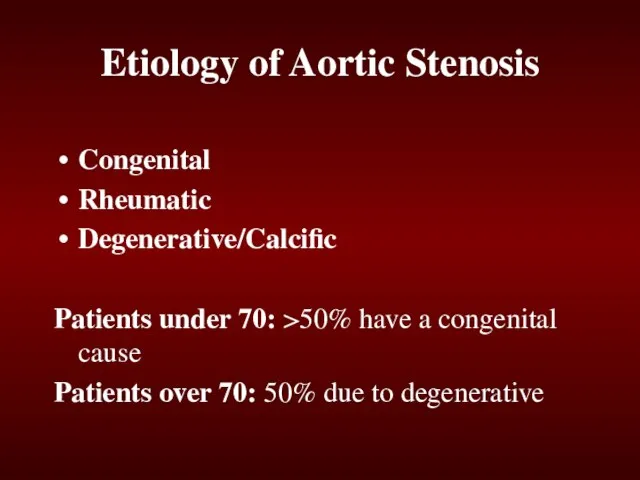
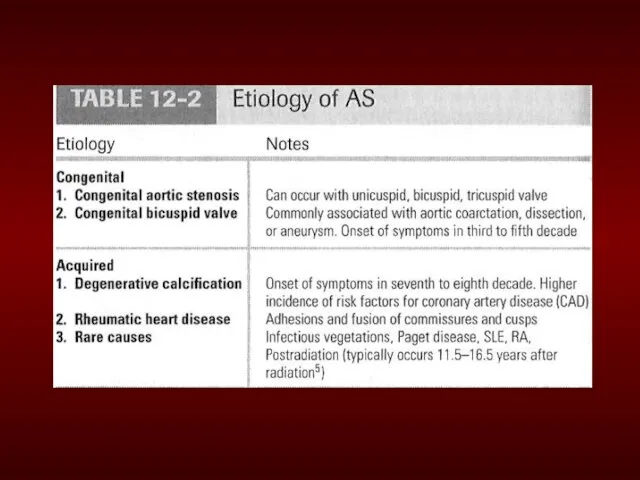
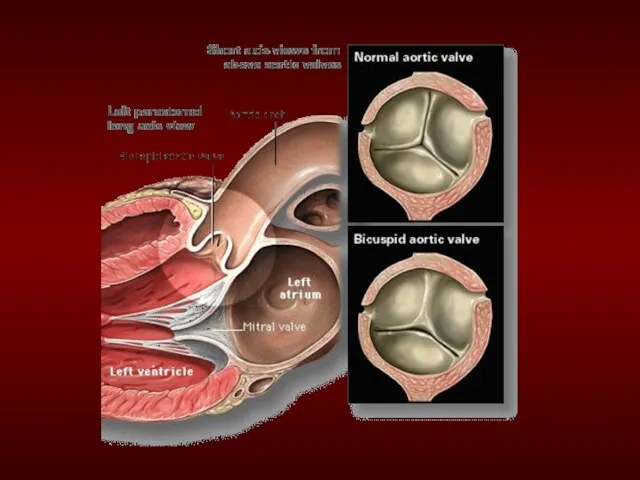
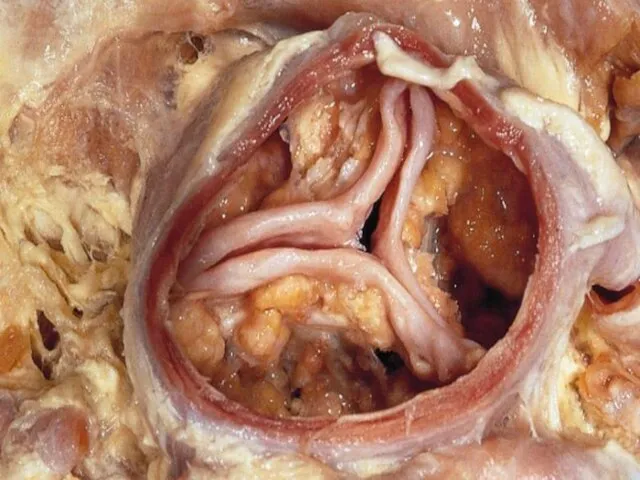
- 7. Etiology of Aortic Stenosis Congenital Rheumatic Degenerative/Calcific Patients under 70: >50% have a congenital cause Patients
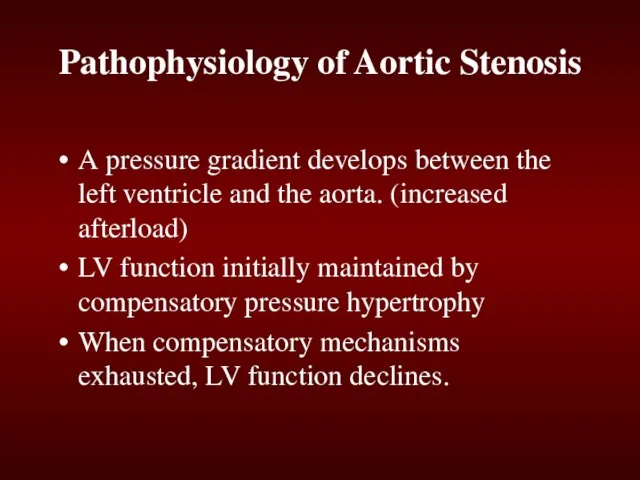
- 12. Pathophysiology of Aortic Stenosis A pressure gradient develops between the left ventricle and the aorta. (increased
- 13. Presentation of Aortic Stenosis Syncope: (exertional) Angina: (increased myocardial oxygen demand; demand/supply mismatch) Dyspnea: on exertion
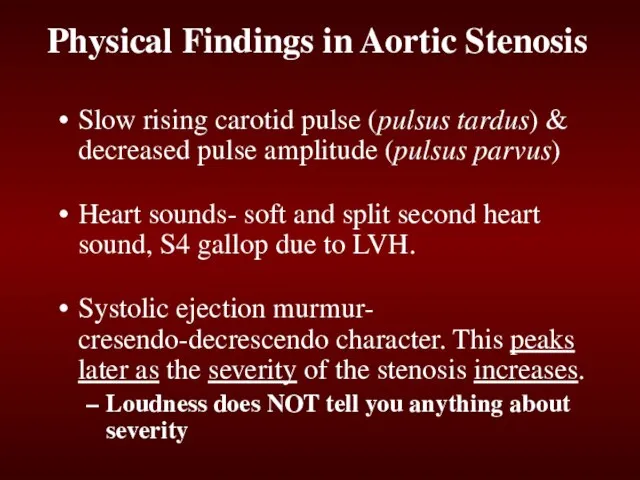
- 14. Physical Findings in Aortic Stenosis Slow rising carotid pulse (pulsus tardus) & decreased pulse amplitude (pulsus
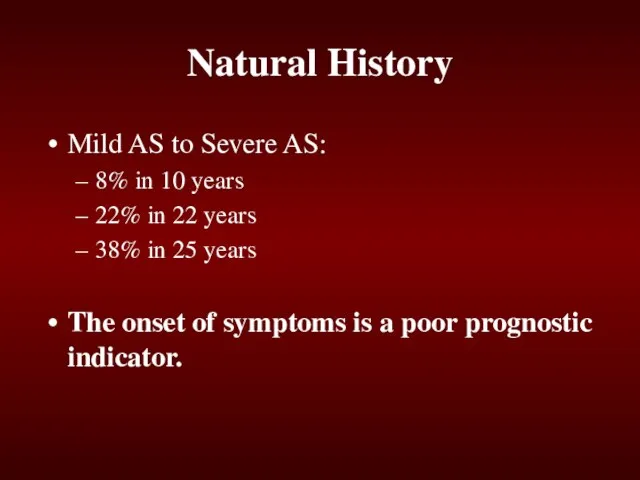
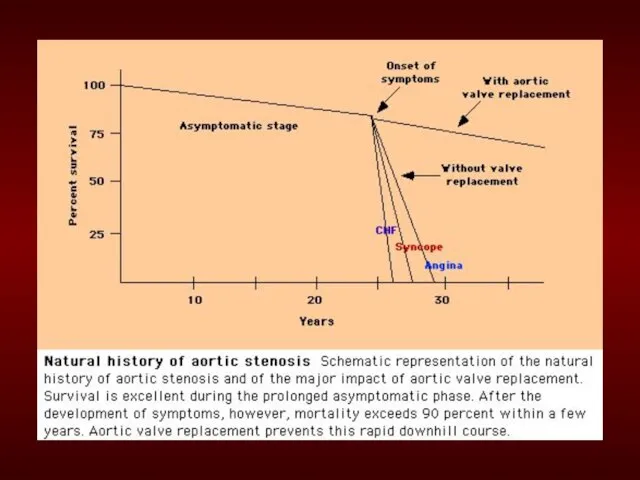
- 15. Natural History Mild AS to Severe AS: 8% in 10 years 22% in 22 years 38%
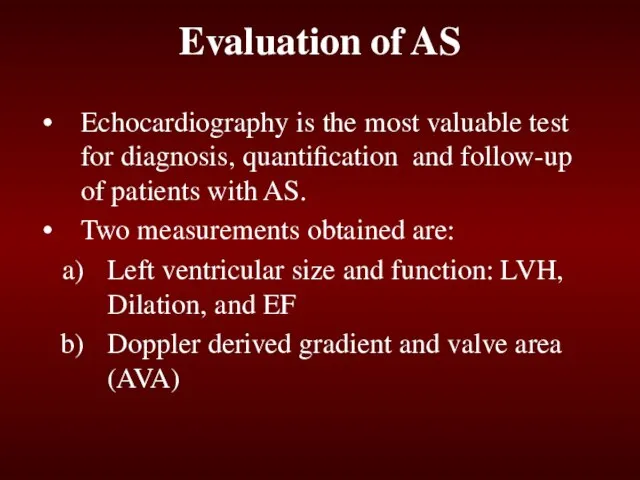
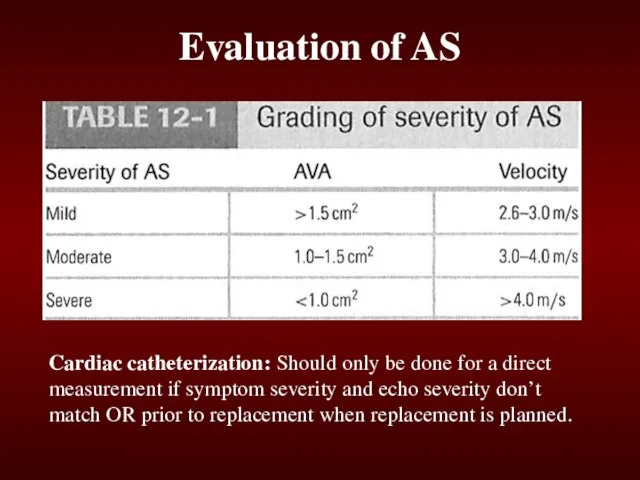
- 17. Evaluation of AS Echocardiography is the most valuable test for diagnosis, quantification and follow-up of patients
- 18. Evaluation of AS Cardiac catheterization: Should only be done for a direct measurement if symptom severity
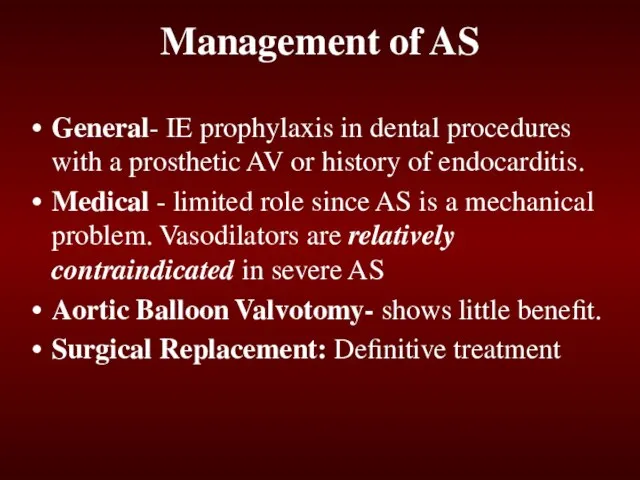
- 19. Management of AS General- IE prophylaxis in dental procedures with a prosthetic AV or history of
- 20. Echo Surveillance Mild: Every 5 years Moderate: Every 2 years Severe: Every 6 months to 1
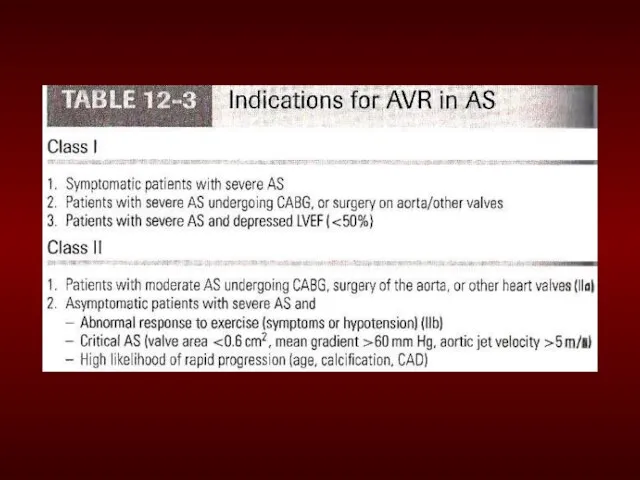
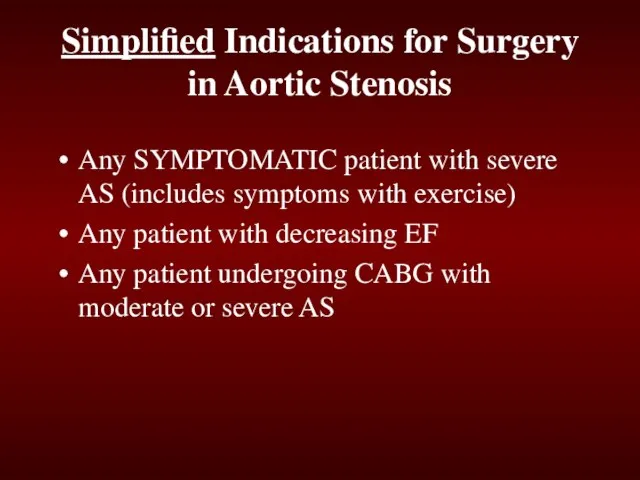
- 22. Simplified Indications for Surgery in Aortic Stenosis Any SYMPTOMATIC patient with severe AS (includes symptoms with
- 23. Summary Disease of aging Look for the signs on physical exam Echocardiogram to assess severity Asymptomatic:
- 24. Mitral Stenosis
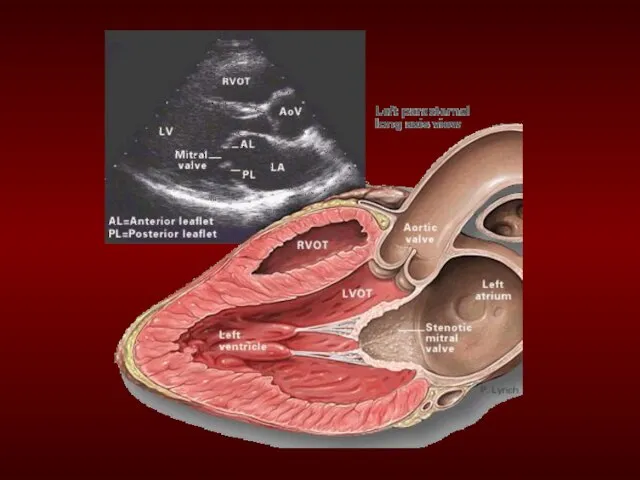
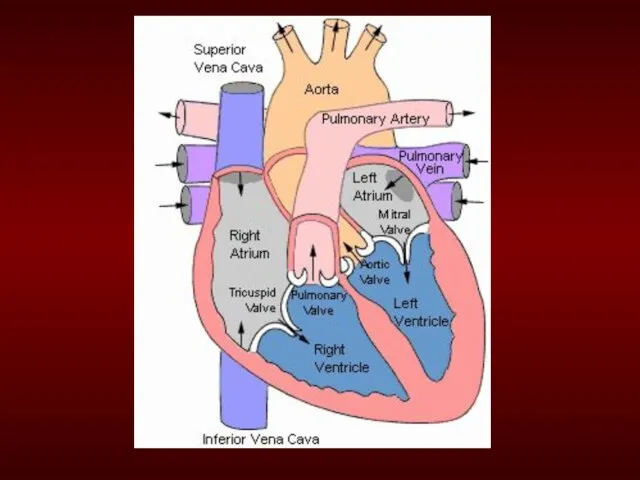
- 25. Mitral Stenosis Overview Definition: Obstruction of LV inflow that prevents proper filling during diastole Normal MV
- 26. Etiology of Mitral Stenosis Rheumatic heart disease: 77-99% of all cases Infective endocarditis: 3.3% Mitral annular
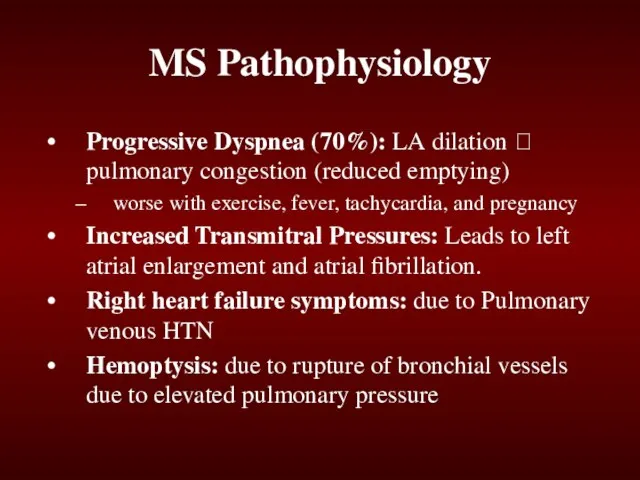
- 31. MS Pathophysiology Progressive Dyspnea (70%): LA dilation ? pulmonary congestion (reduced emptying) worse with exercise, fever,
- 32. Natural History of MS Disease of plateaus: Mild MS: 10 years after initial RHD insult Moderate:
- 33. Physical Exam Findings of MS prominent "a" wave in jugular venous pulsations: Due to pulmonary hypertension
- 34. Diastolic murmur: Low-pitched diastolic rumble most prominent at the apex. Heard best with the patient lying
- 35. Loud Opening S1 snap: heard at the apex when leaflets are still mobile Due to the
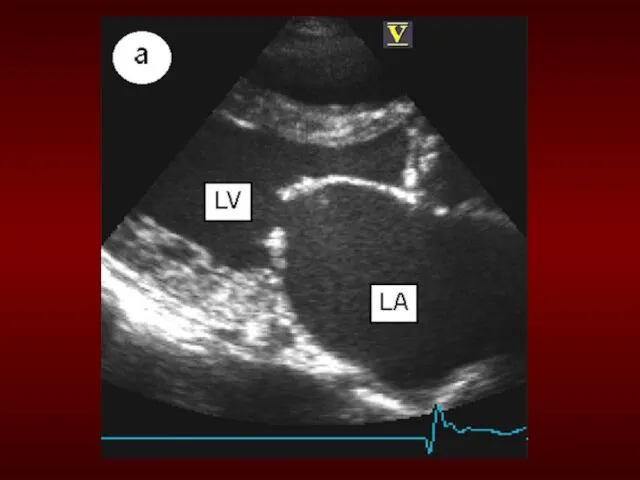
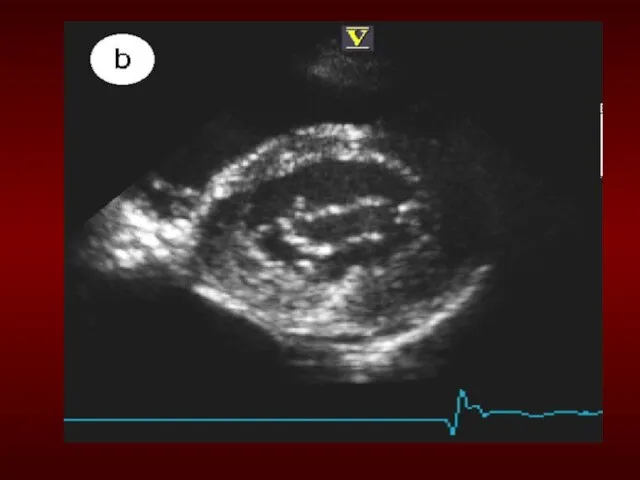
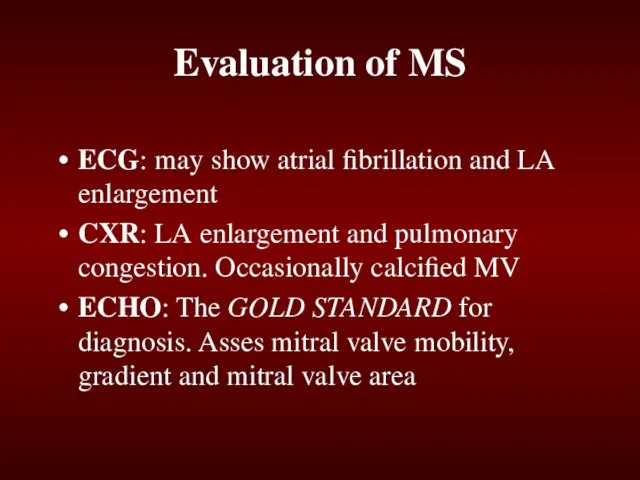
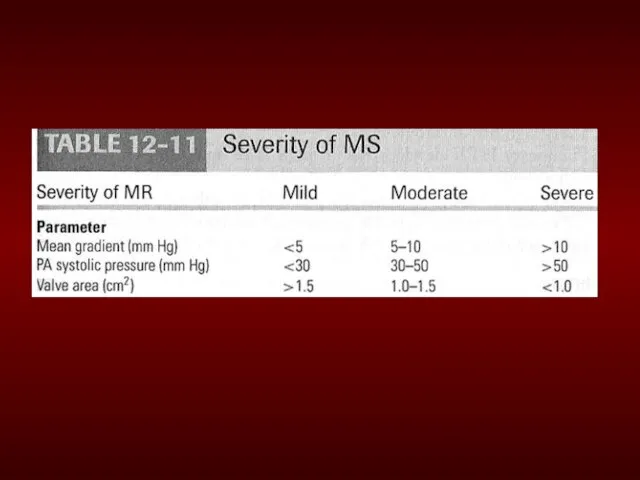
- 36. Evaluation of MS ECG: may show atrial fibrillation and LA enlargement CXR: LA enlargement and pulmonary
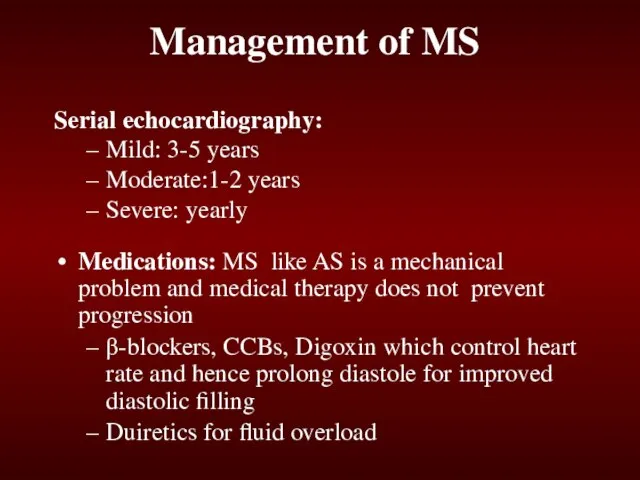
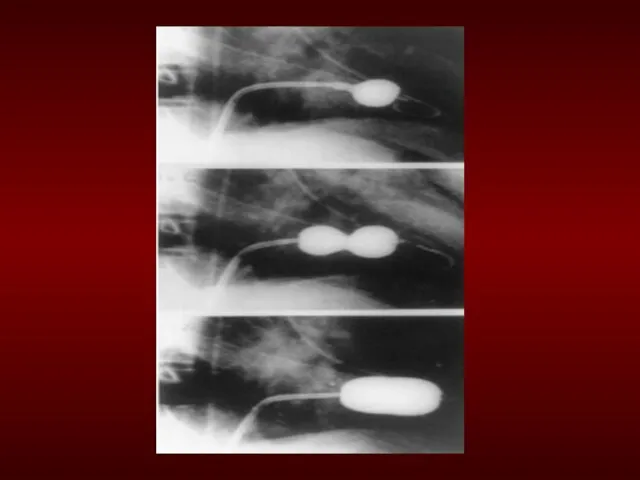
- 38. Management of MS Serial echocardiography: Mild: 3-5 years Moderate:1-2 years Severe: yearly Medications: MS like AS
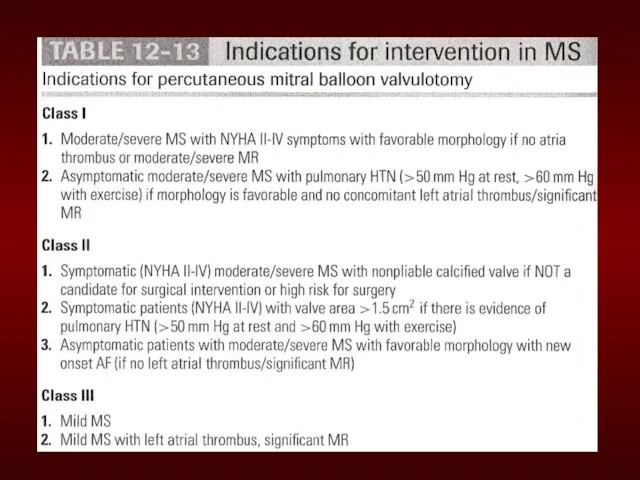
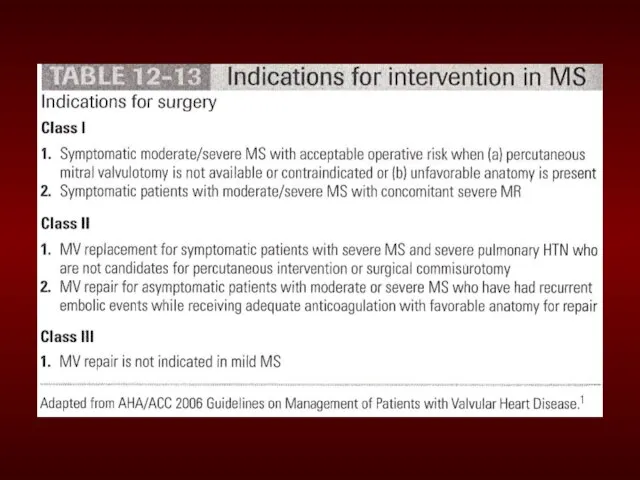
- 39. Management of MS Identify patient early who might benefit from percutaneous mitral balloon valvotomy. IE prophylaxis:
- 44. Simplified Indications for Mitral valve replacement ANY SYMPTOMATIC Patient with NYHA Class III or IV Symptoms
- 45. Aortic Regurgitation
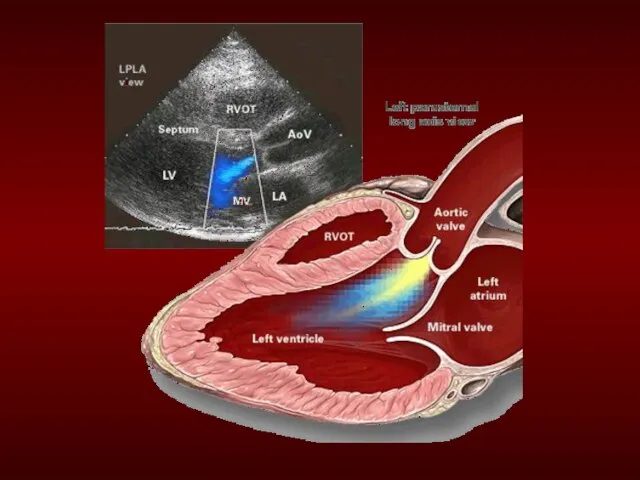
- 47. Aortic Regurgitation Overview Definition: Leakage of blood into LV during diastole due to ineffective coaptation of
- 48. Etiology of Acute AR Endocarditis Aortic Dissection Physical Findings: Wide pulse pressure Diastolic murmur Florid pulmonary
- 49. Treatment of Acute AR True Surgical Emergency: Positive inotrope: (eg, dopamine, dobutamine) Vasodilators: (eg, nitroprusside) Avoid
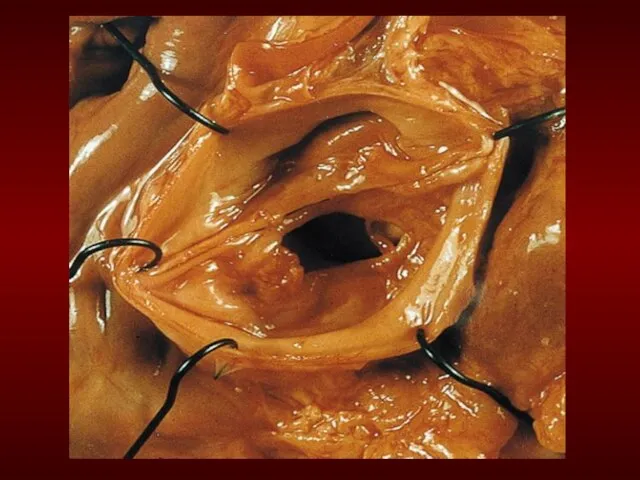
- 51. Etiology of Chronic AR Bicuspid aortic valve Rheumatic Infective endocarditis
- 52. Pathophysiology of AR Combined pressure AND volume overload Compensatory Mechanisms: LV dilation, LVH. Progressive dilation leads
- 53. Natural History of AR Asymptomatic until 4th or 5th decade Rate of Progression: 4-6% per year
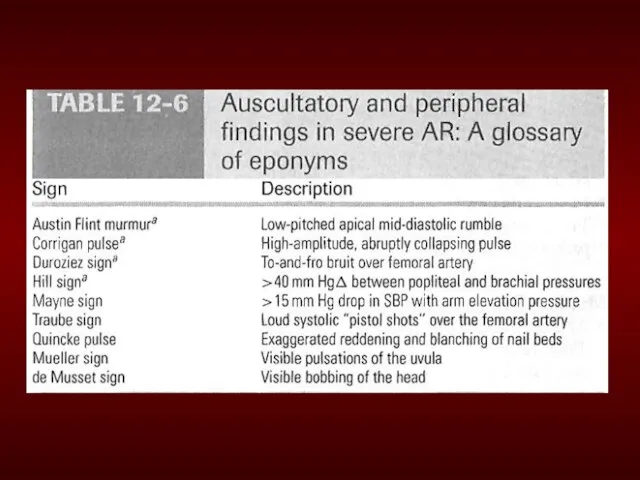
- 54. Physical Exam findings of AR Wide pulse pressure: most sensitive Hyperdynamic and displaced apical impulse Auscultation-
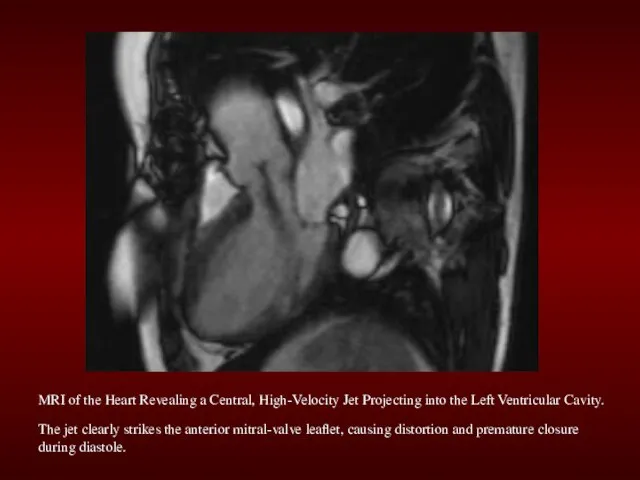
- 56. MRI of the Heart Revealing a Central, High-Velocity Jet Projecting into the Left Ventricular Cavity. The
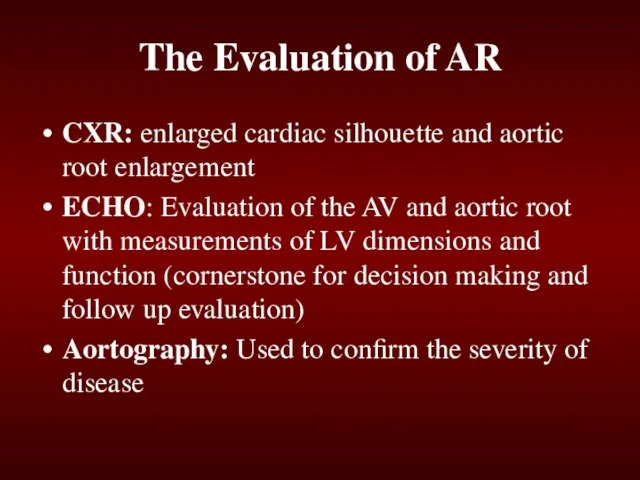
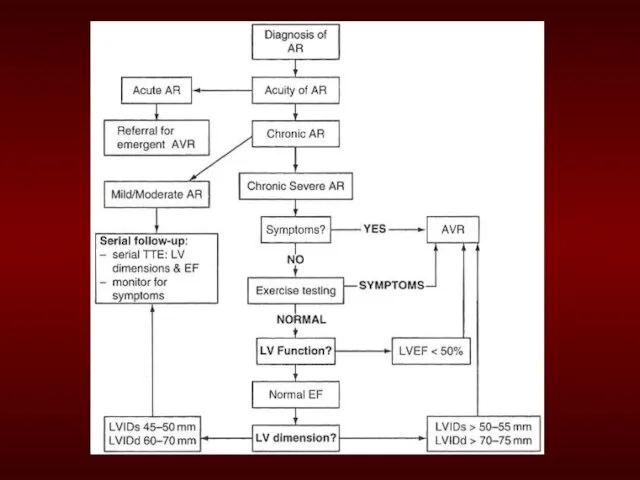
- 57. The Evaluation of AR CXR: enlarged cardiac silhouette and aortic root enlargement ECHO: Evaluation of the
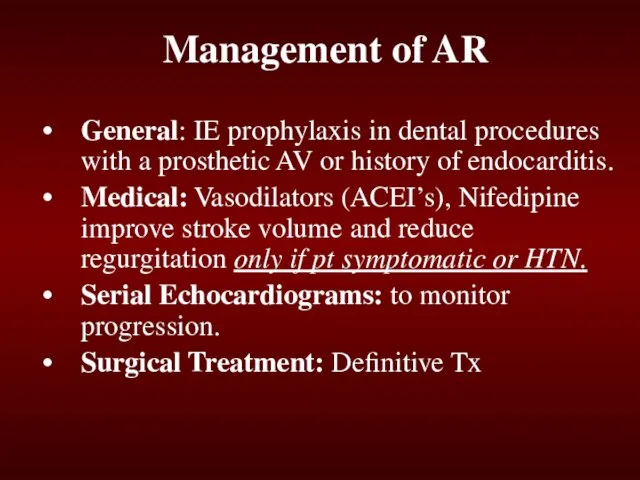
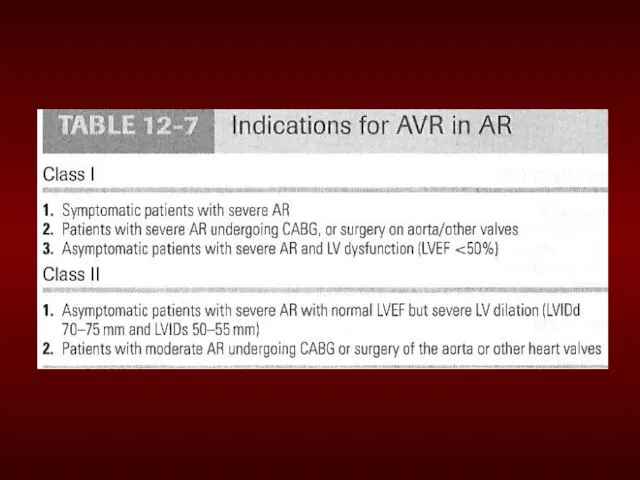
- 59. Management of AR General: IE prophylaxis in dental procedures with a prosthetic AV or history of
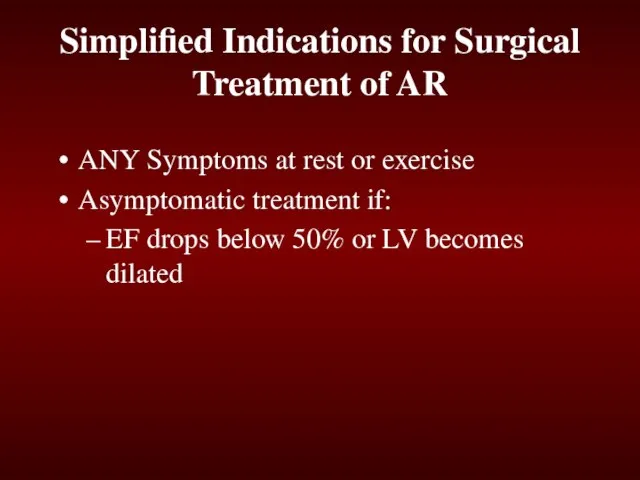
- 62. Simplified Indications for Surgical Treatment of AR ANY Symptoms at rest or exercise Asymptomatic treatment if:
- 63. Mitral Regurgitation
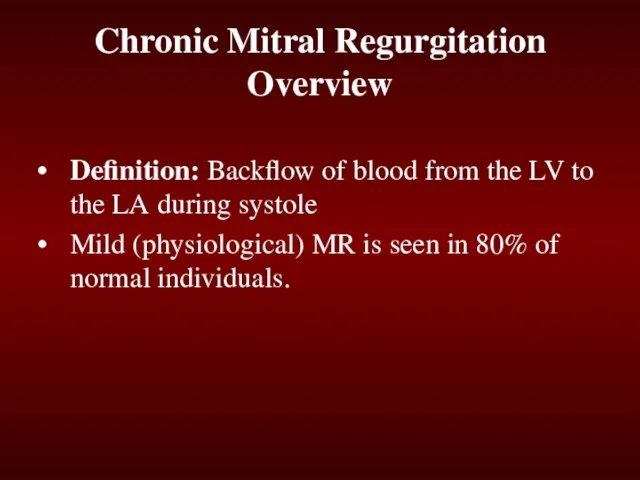
- 64. Definition: Backflow of blood from the LV to the LA during systole Mild (physiological) MR is
- 65. Acute MR Endocarditis Acute MI: Malfunction or disruption of prosthetic valve
- 66. Management of Acute MR Myocardial infarction: Cardiac cath or thrombolytics Most other cases of mitral regurgitation
- 67. Management of Acute MR Do not attempt to alleviate tachycardia with beta-blockers. Mild-to-moderate tachycardia is beneficial
- 68. Treatment of Acute MR Balloon Pump Nitroprusside even if hypotensive Emergent Surgery
- 69. Myxomatous degeneration (MVP) Ischemic MR Rheumatic heart disease Infective Endocarditis Etiologies of Chronic Mitral Regurgitation
- 70. Pathophysiology of MR Pure Volume Overload Compensatory Mechanisms: Left atrial enlargement, LVH and increased contractility Progressive
- 71. Physical Exam findings in MR Auscultation: soft S1 and a holosystolic murmur at the apex radiating
- 72. The Natural History of MR Compensatory phase: 10-15 years Patients with asymptomatic severe MR have a
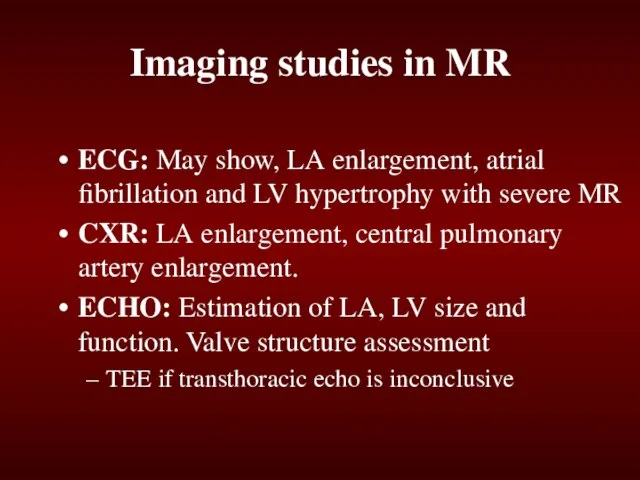
- 73. Imaging studies in MR ECG: May show, LA enlargement, atrial fibrillation and LV hypertrophy with severe
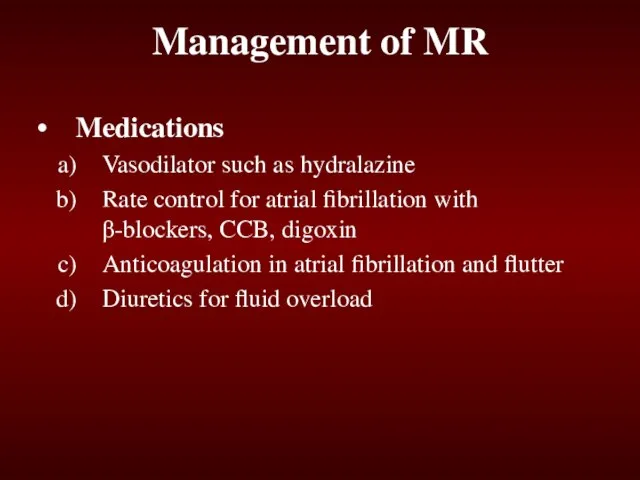
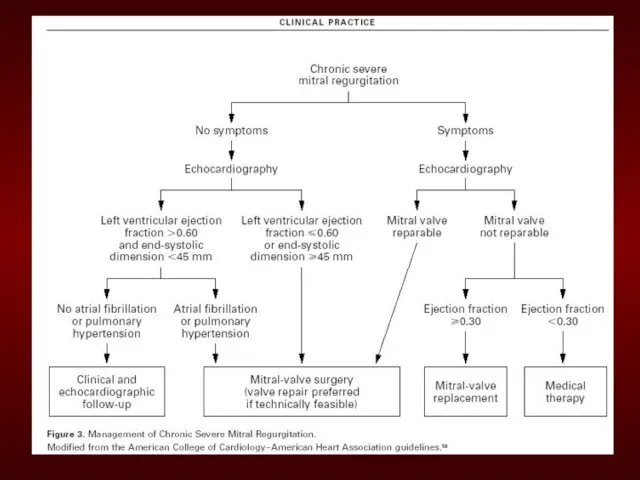
- 75. Management of MR Medications Vasodilator such as hydralazine Rate control for atrial fibrillation with β-blockers, CCB,
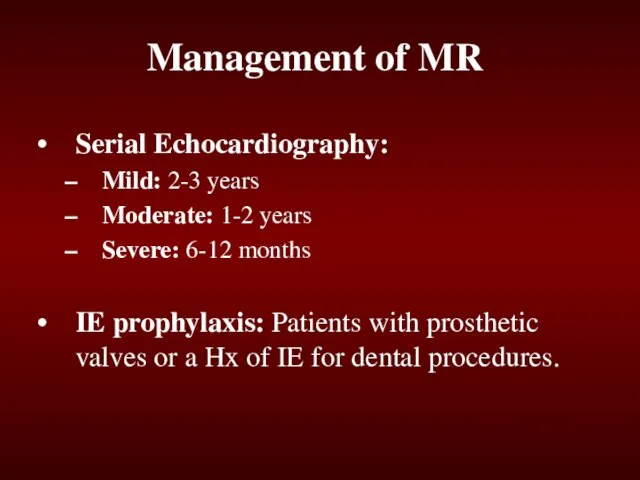
- 76. Management of MR Serial Echocardiography: Mild: 2-3 years Moderate: 1-2 years Severe: 6-12 months IE prophylaxis:
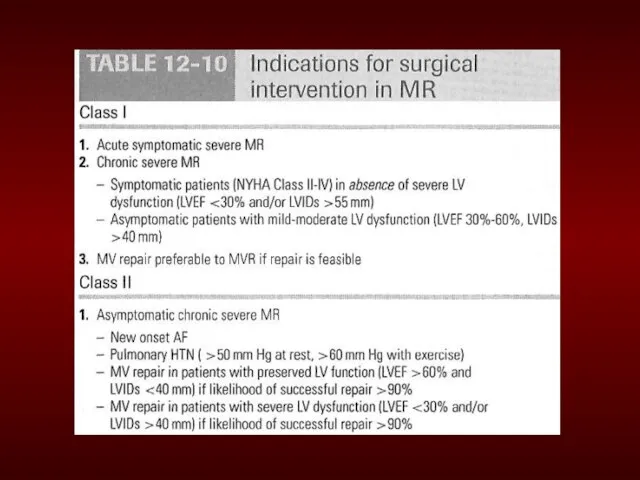
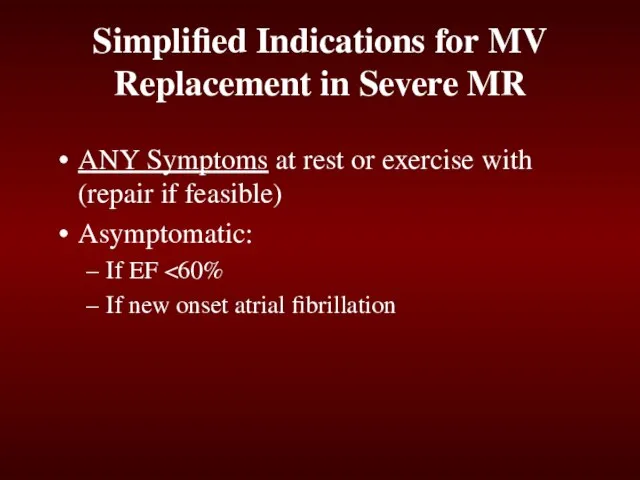
- 79. Simplified Indications for MV Replacement in Severe MR ANY Symptoms at rest or exercise with (repair
- 81. Скачать презентацию



 Особенности проектирования печатных плат на металлическом основании
Особенности проектирования печатных плат на металлическом основании Роботы R2D2, BB-8, C3PO
Роботы R2D2, BB-8, C3PO Светофорик приглашает
Светофорик приглашает Здоровьесберегающие технологии для детей 6-7 лет
Здоровьесберегающие технологии для детей 6-7 лет Бутерброды 5 класс
Бутерброды 5 класс Обзор типовых решений «1С-Рарус». Новые программные продукты
Обзор типовых решений «1С-Рарус». Новые программные продукты Воронеж – город Воинской Славы. . В Воронеже будет отмечается День города – традиционно день народных гуляний, выступлений на площ
Воронеж – город Воинской Славы. . В Воронеже будет отмечается День города – традиционно день народных гуляний, выступлений на площ Зеленые проектыМурманской области
Зеленые проектыМурманской области Налоговая задолженность
Налоговая задолженность Техника бросков мяча в движении, методика обучения
Техника бросков мяча в движении, методика обучения Проектная деятельность учащихся (материалы к педагогическому совету)
Проектная деятельность учащихся (материалы к педагогическому совету) Мастерицы России. Надежда Федоровна Кочетова
Мастерицы России. Надежда Федоровна Кочетова БЕЗОПАСНЫЙ ИНТЕРНЕТ
БЕЗОПАСНЫЙ ИНТЕРНЕТ  Фартуки
Фартуки Презентация на тему Бесполое размножение (6 класс)
Презентация на тему Бесполое размножение (6 класс)  Отряд ЮИД в действии. стр 3
Отряд ЮИД в действии. стр 3 Презентация на тему Зелёный пояс Славы
Презентация на тему Зелёный пояс Славы Искусство
Искусство Еңбек нормасы. Өнім нормасы
Еңбек нормасы. Өнім нормасы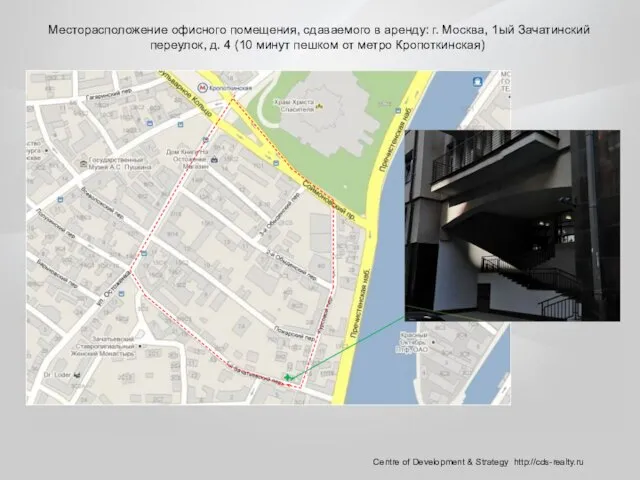 Месторасположение офисного помещения, сдаваемого в аренду: г. Москва, 1ый Зачатинский переулок, д. 4 (10 минут пешком от метро Кропотк
Месторасположение офисного помещения, сдаваемого в аренду: г. Москва, 1ый Зачатинский переулок, д. 4 (10 минут пешком от метро Кропотк наш 9 класс
наш 9 класс 26.09.22 Фізичне тіло. Матеріал. Речовина. Молекула. Атом
26.09.22 Фізичне тіло. Матеріал. Речовина. Молекула. Атом Сравнение сюжета сказок В.А. Жуковского «Спящая царевна» и Ш. Перро «Спящая красавица»
Сравнение сюжета сказок В.А. Жуковского «Спящая царевна» и Ш. Перро «Спящая красавица» Последовательная политика в отношении инвалидов. Рекомендация N (R) 6 Комитета министров от 09.04.1992
Последовательная политика в отношении инвалидов. Рекомендация N (R) 6 Комитета министров от 09.04.1992 Игра С 8 марта
Игра С 8 марта 2 белки - копия
2 белки - копия Правила гигиены и здорового образа жизни
Правила гигиены и здорового образа жизни Решение физических задач графическим способом
Решение физических задач графическим способом