Содержание
- 3. Trichomonas vaginalis is an anaerobic, flagellated protozoan parasite and the causative agent of trichomoniasis. It is
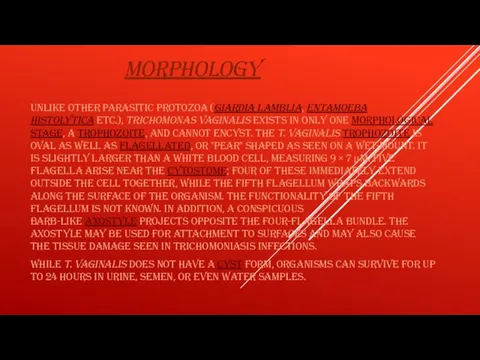
- 5. MORPHOLOGY Unlike other parasitic protozoa (Giardia lamblia, Entamoeba histolytica etc.), Trichomonas vaginalis exists in only one
- 6. TRICHOMONAS VAGINALIS, A PARASITIC PROTOZOAN, IS THE ETIOLOGIC AGENT OF TRICHOMONIASIS, AND IS A SEXUALLY TRANSMITTED
- 7. HISTORY Alfred Francois Donné (1801–1878) was the first to describe a procedure to diagnose trichomoniasis through
- 8. COMPLICATIONS Some of the complications of T. vaginalis in women include: preterm delivery, low birth weight,
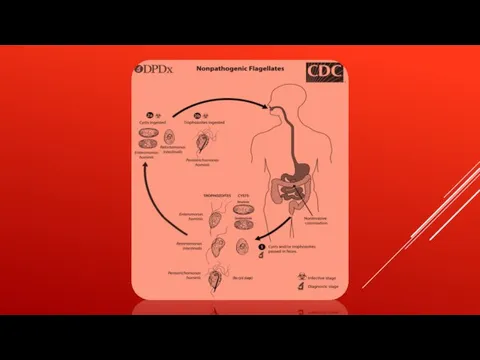
- 9. LIFE CYCLE Trichomonas vaginalis resides in the female lower genital tract and the male urethra and
- 11. GENETIC DIVERSITY Recent studies into the genetic diversity of T.vaginalis has shown that there are two
- 12. GENOME SEQUENCING AND STATISTICS The T. vaginalis genome was found to be approximately 160 megabases in
- 14. VIRULENCE FACTORS One of the hallmark features of Trichomonas vaginalis is the adherence factors that allow
- 15. PROTEIN FUNCTION Trichomonas vaginalis lacks mitochondria and therefore necessary enzymes and cytochromes to conduct oxidative phosphorylation.
- 16. INCREASED SUSCEPTIBILITY TO HIV The damage caused by Trichomonas vaginalis to the vaginal epithelium increases a
- 17. DIAGNOSIS Classically, with a cervical smear, infected women may have a transparent "halo" around their superficial
- 18. TREATMENT Infection is treated and cured with metronidazole[19] or tinidazole. The CDC recommends a one time
- 19. FOR BETTER UNDERSTANDING https://www.youtube.com/watch?v=SYd4lLed3CI https://www.youtube.com/watch?v=yk0P7IpSiIg https://www.youtube.com/watch?v=TlNBQx9rH20&list=TLPQMTMwNjIwMjBRQCLpCuaiHQ&index=3
- 21. Скачать презентацию


![TREATMENT Infection is treated and cured with metronidazole[19] or tinidazole. The CDC](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/875909/slide-17.jpg)
 Ребятам о муравьях (средняя группа)
Ребятам о муравьях (средняя группа) Растения луга
Растения луга Что растёт на клумбе
Что растёт на клумбе Остеология. Осевой скелет
Остеология. Осевой скелет Мутація у живих організмів
Мутація у живих організмів Обобщающий урок Ткани животных
Обобщающий урок Ткани животных Каково строение гидры?
Каково строение гидры? Комары
Комары Єноти - хижі ссавці, що належать до однойменного сімейства єнотових
Єноти - хижі ссавці, що належать до однойменного сімейства єнотових Микробы
Микробы Деление клетки. Митоз
Деление клетки. Митоз Орг-вещ9конц
Орг-вещ9конц Запуск аквариума. Инструкция для начинающих
Запуск аквариума. Инструкция для начинающих Витамины. Классификация
Витамины. Классификация Презентация на тему Увеличительные приборы и правила работы с ними
Презентация на тему Увеличительные приборы и правила работы с ними  Пластиды
Пластиды Физиология гиппокампа
Физиология гиппокампа Гиганты и лилипуты в мире насекомых
Гиганты и лилипуты в мире насекомых Критерии вида
Критерии вида Роль витаминов в жизни человека
Роль витаминов в жизни человека Пустельга обыкновенная
Пустельга обыкновенная Звуки, которые может издавать человек
Звуки, которые может издавать человек Проращивание фасоли
Проращивание фасоли Генетика 18
Генетика 18 Методи селекції
Методи селекції Мои питомцы
Мои питомцы Наглядное пособие Скелет Бронтозавра
Наглядное пособие Скелет Бронтозавра Окружающий мир (1 класс)
Окружающий мир (1 класс)