Содержание
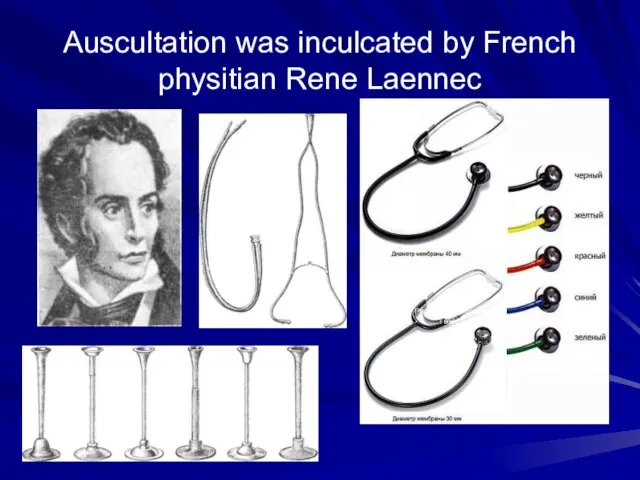
- 2. Auscultation was inculcated by French physitian Rene Laennec Рис. 10. Стетоскопи тверд!.
- 3. First device for auscultation was a stetoscope
- 4. First binaural stetoscope
- 5. First phonendoscope
- 6. Modern stetophonendoscope
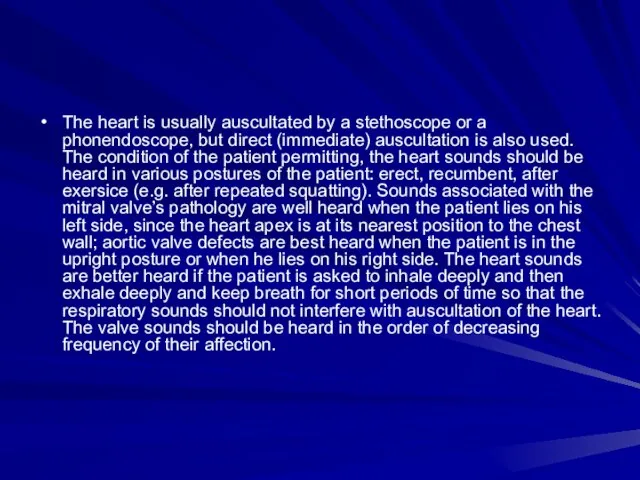
- 7. The heart is usually auscultated by a stethoscope or a phonendoscope, but direct (immediate) auscultation is
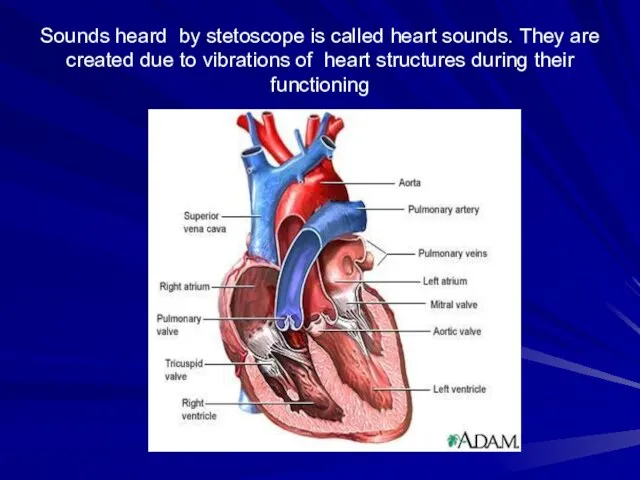
- 9. Sounds heard by stetoscope is called heart sounds. They are created due to vibrations of heart
- 10. Examination sequence -> Explain that you wish to examine the chest and ask the patient to
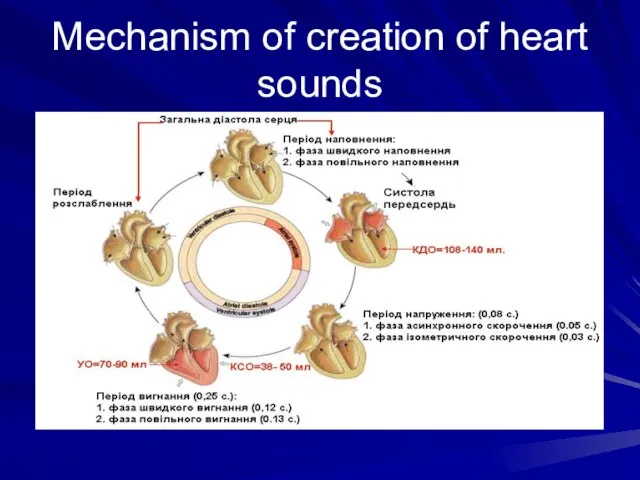
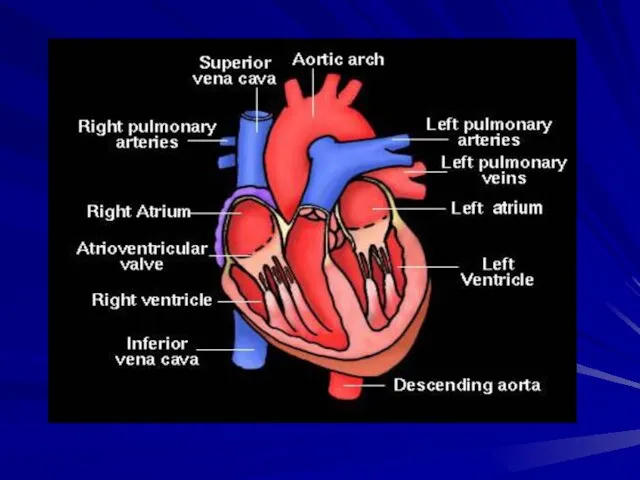
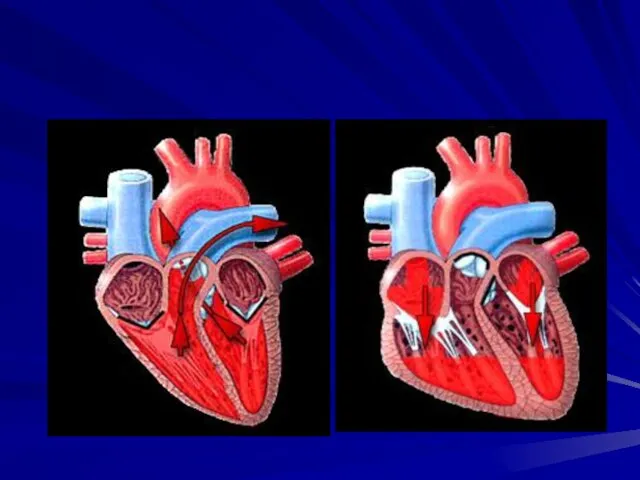
- 13. Mechanism of creation of heart sounds
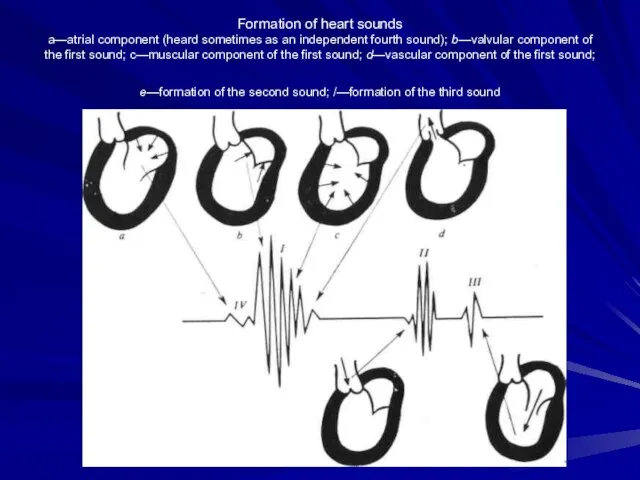
- 15. Formation of heart sounds a—atrial component (heard sometimes as an independent fourth sound); b—valvular component of
- 16. Auscultation involves listening for heart sounds with the stethoscope, similar to the procedure used in assessing
- 17. Сomponents of heart sounds I heart sound: the valve component, i.e. vibrations of the cusps of
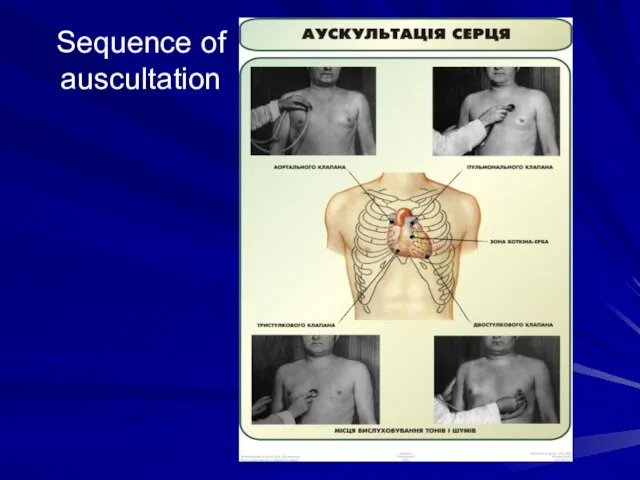
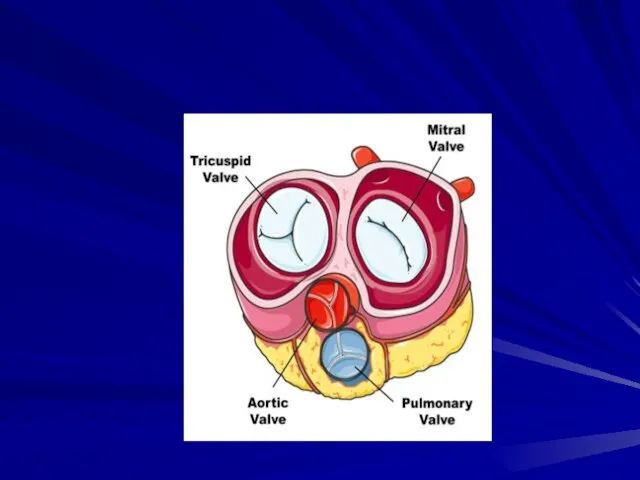
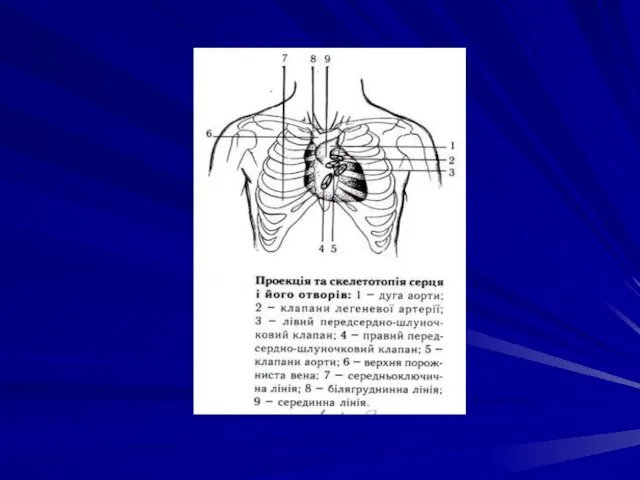
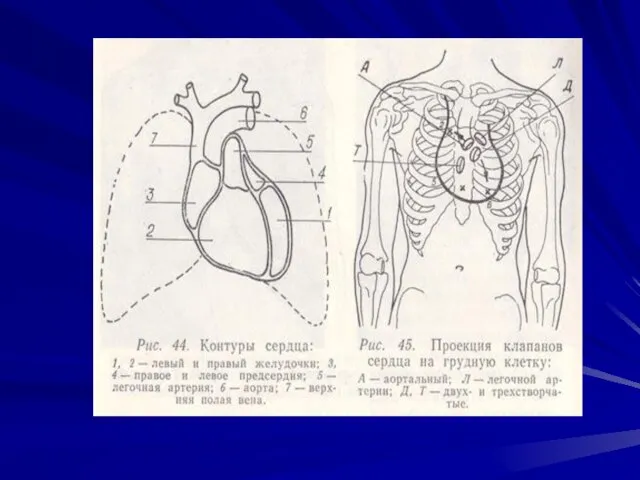
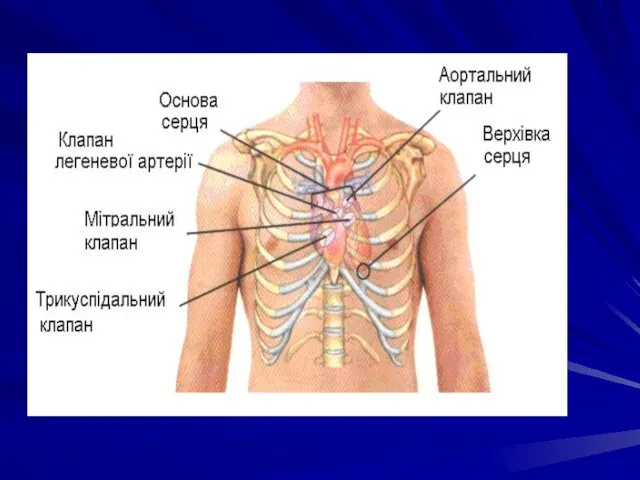
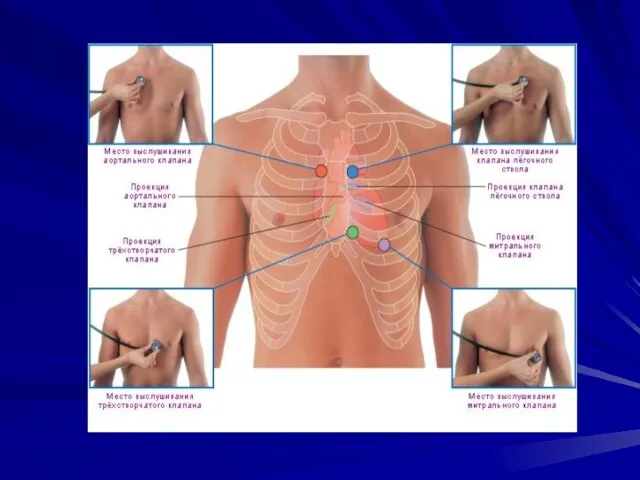
- 18. Sequence of auscultation The mitral valve - at the heart apex; the aortic valve - in
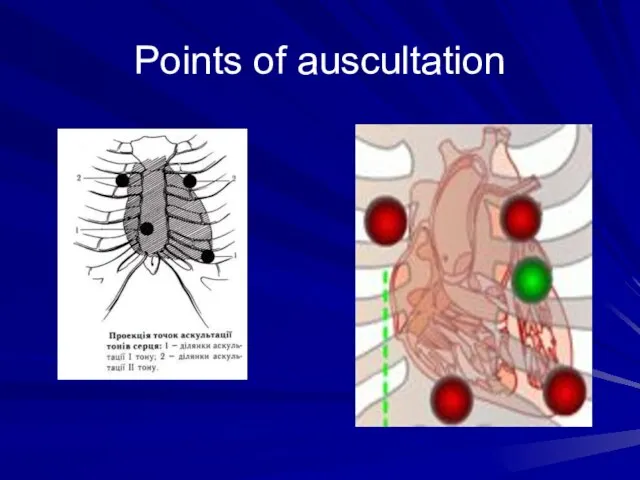
- 23. Points of auscultation
- 24. Rules for auscultation of the heart. The heart is usually auscultated by a stethoscope or a
- 25. Sequence of auscultation
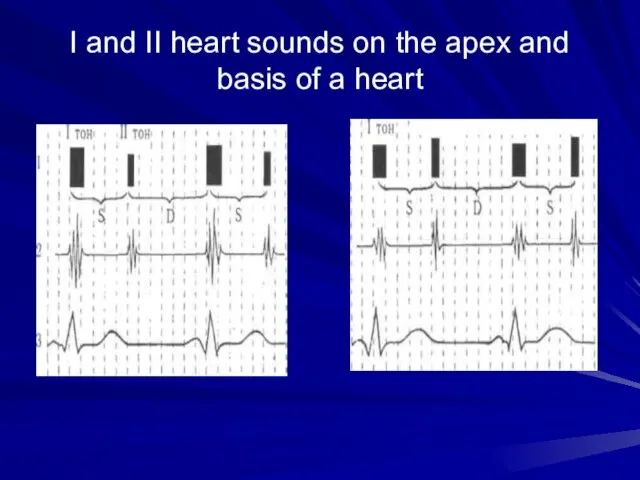
- 27. Differential features of I and II heart sounds I heart sound II heart sound The place
- 29. I and II heart sounds on the apex and basis of a heart
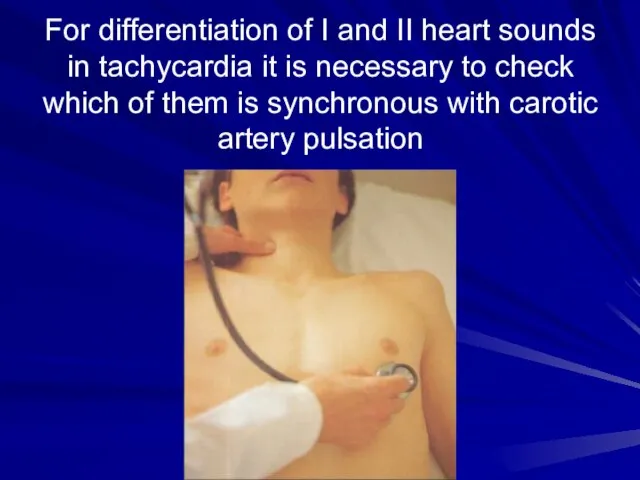
- 30. For differentiation of I and II heart sounds in tachycardia it is necessary to check which
- 31. Intensity of the heart sounds may depend on conditions of the sound wave transmission The intensity
- 32. The intensity of the heart sounds increases if their transmission to the chest becomes better: thin
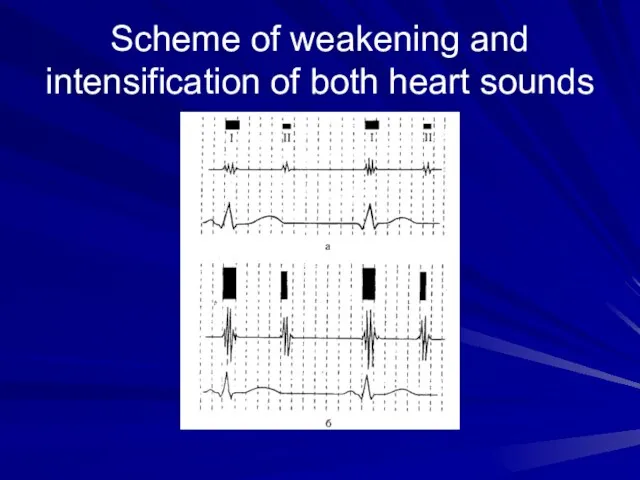
- 33. Scheme of weakening and intensification of both heart sounds
- 34. Separate changes of one heart sound (I or II): First heart sound diminishes: in the mitral
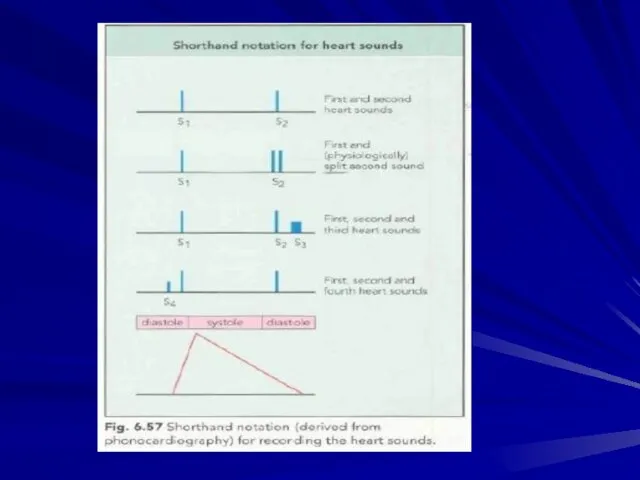
- 35. Splitting or reduplication of the sounds occurs in asynchronous work and right chambers of the heart
- 36. The second sound is reduplicated more frequently Reduplication occurs due to asynchronous closure of the valve
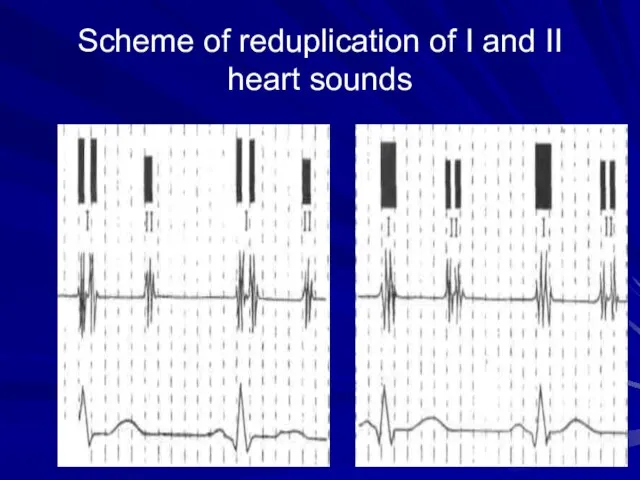
- 37. Scheme of reduplication of I and II heart sounds
- 38. Adventitious heart sounds The third heart sound (S3) is the result of vibrations produced during ventricular
- 40. Heart melodies Intensification of S3 or S4 sounds gives a three-sound or even four- three-sound rhythm,
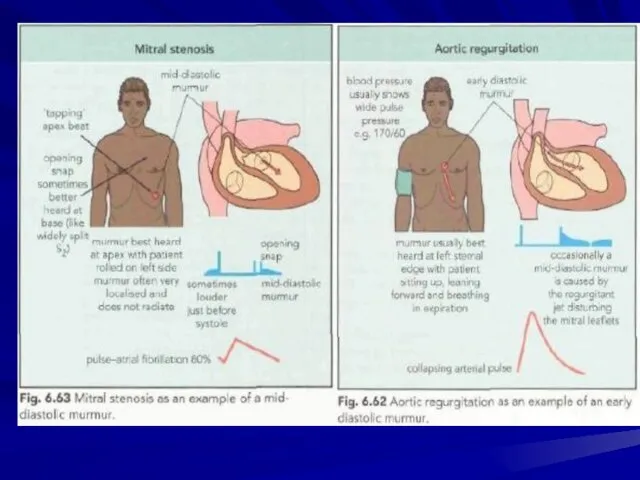
- 41. Triple rrhythm (Rhithmus coeturnici) It is a cardiac rhythm which is auscultated only in mitral stenosis
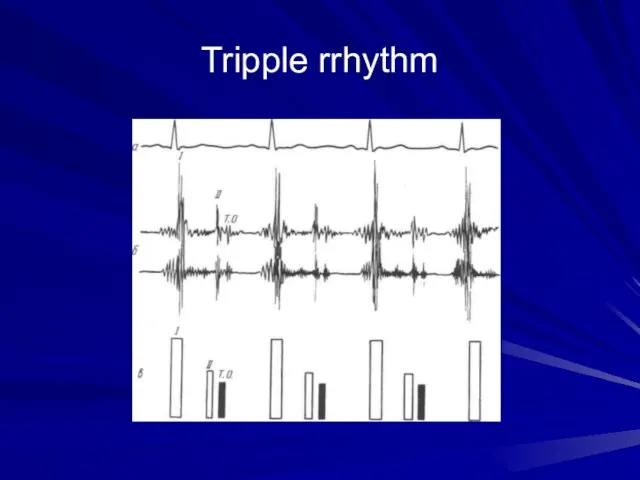
- 43. Tripple rrhythm
- 44. Pendulum rhythm In the case of pendulum rhythm the large (diastolic) heart pause is so shortened,
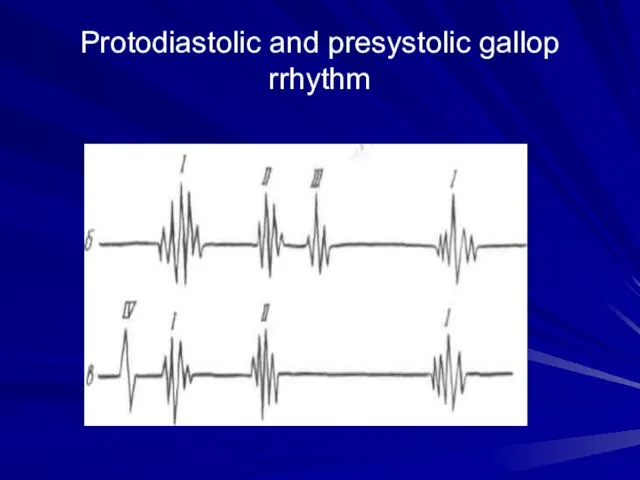
- 45. Protodiastolic and presystolic gallop rrhythm
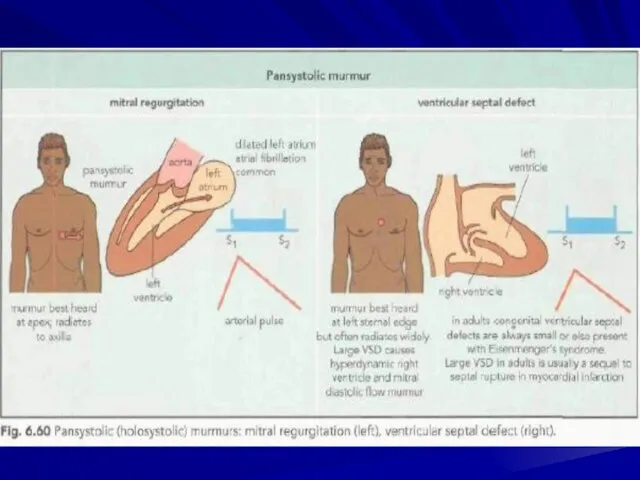
- 46. Cardiac murmurs- phenpmena which arise due to pathological blood flow in the heart Intracardial murmurs: Organic
- 47. Properties of murmurs Duration The murmurs of mitral (and tricuspid) regurgitation start simultaneously with the first
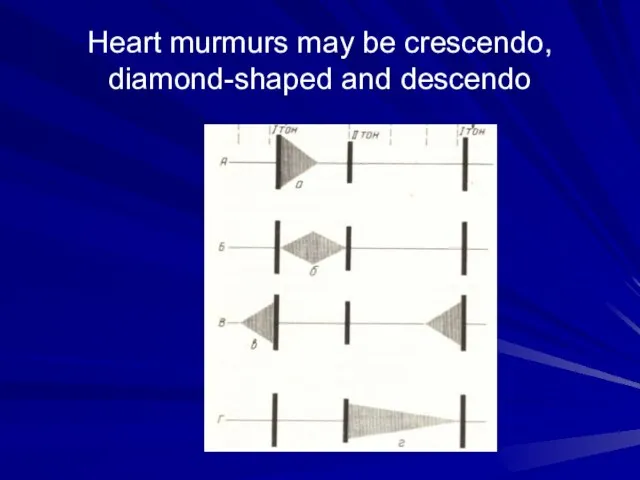
- 48. Heart murmurs may be crescendo, diamond-shaped and descendo
- 49. Intensity There are six grades of intensity used to describe murmurs. Diastolic murmurs are rarely louder
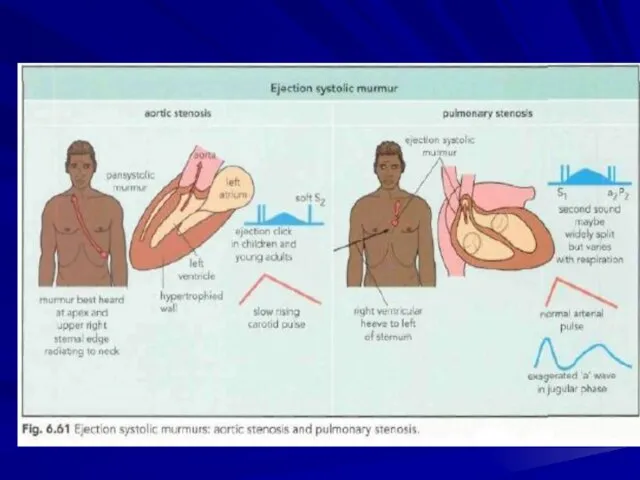
- 50. Causes of systolic murmurs Ejection systolic murmur Increased flow through normal valves • 'Innocent systolic murmur':
- 54. At an auscultation it is necessary to determine: 1) relation of murmur to the phase of
- 55. Murmurs are auscultated better at points of auscultation of those valves, in which they were formed.
- 56. Differentiation of functional and organic murmurs in the most cases functional murmurs are systolic; the murmurs
- 57. The pericardial friction It is develops in change of visceral and parietal pericardiac layers, when the
- 58. The pleuropericardial friction murmur It arises in inflammation of pleura, immediately accumbent to heart, owing to
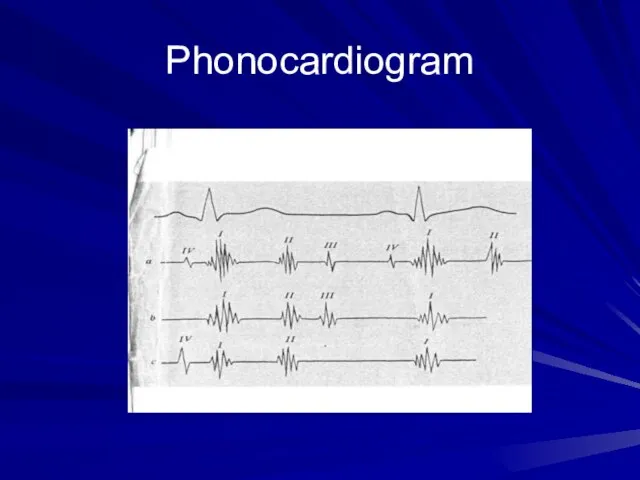
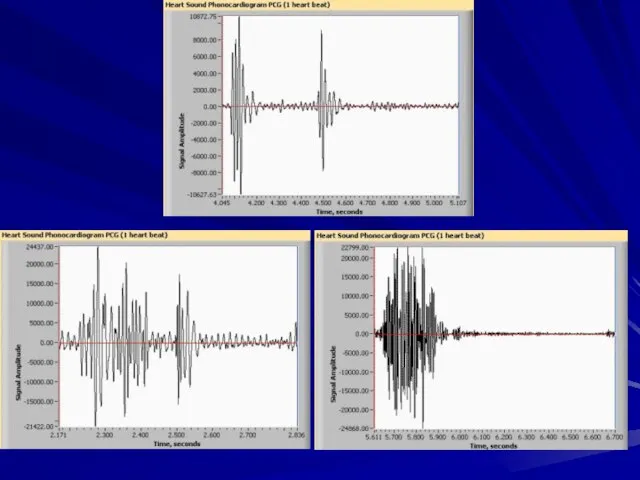
- 59. Phonocardiogram
- 61. AUSCULTATION OF VESSELS Auscultation of arteries. Arteries of medium calibre, such as the carotid, subclavian, or
- 62. In norm: Two sounds can be heard on the carotid and subclavian arteries in healthy persons.
- 63. Systolic sound produced by the stenosed aortal orifice is usually well transmitted onto the carotid and
- 64. Auscultation of veins Neither sounds nor murmurs are normally heard over veins. Auscultation of the jugular
- 66. Скачать презентацию
Слайд 3First device for auscultation was a stetoscope
First device for auscultation was a stetoscope
Слайд 4First binaural stetoscope
First binaural stetoscope

Слайд 5First phonendoscope
First phonendoscope
Слайд 6Modern stetophonendoscope
Modern stetophonendoscope

Слайд 7The heart is usually auscultated by a stethoscope or a phonendoscope, but
The heart is usually auscultated by a stethoscope or a phonendoscope, but
Слайд 9Sounds heard by stetoscope is called heart sounds. They are created due
Sounds heard by stetoscope is called heart sounds. They are created due
Слайд 10 Examination sequence
-> Explain that you wish to examine the chest and
Examination sequence
-> Explain that you wish to examine the chest and
■> With the patient lying at approximately 45° to the
horizontal, listen over the precordium at the base of the heart, apex, and upper left and right sternal edges with both bell and diaphragm. Also listen over the carotid arteries and the axilla.
■> At each site identify the first and second heart sounds and assess their character and intensity; note any splitting of the second heart sound.
■> Concentrate in turn on systole (the interval between S, and S2) and diastole (the interval between the S2 and S,). Listen for added sounds and then for murmurs.
•♦ Roll the patient on to the left side. Listen at the apex using light pressure with the bell, to detect the mid-diastolic and presystolic murmur of mitral stenosis.
Слайд 13Mechanism of creation of heart sounds
Mechanism of creation of heart sounds
Слайд 15Formation of heart sounds
a—atrial component (heard sometimes as an independent fourth sound);
Formation of heart sounds a—atrial component (heard sometimes as an independent fourth sound);
Слайд 16Auscultation involves listening for heart sounds with the stethoscope, similar to the
Auscultation involves listening for heart sounds with the stethoscope, similar to the
The sounds produced by a working heart are called heart sounds. Two sounds can be well heard in a healthy subject; the first sound, which is produced during systole and the second sound, which occurs during diastole.
Слайд 17Сomponents of heart sounds
I heart sound:
the valve component, i.e. vibrations of the
Сomponents of heart sounds
I heart sound:
the valve component, i.e. vibrations of the
the muscular one due to the myocardial isometric contraction
the vascular one. This is due to vibrations of the nearest portions of the aorta and the pulmonary trunk caused by their distention with the blood during the ejection phase
Atrial one is generated by vibrations caused by atrial contractions
II heart sound:
The second sound is generated by vibrations arising at the early diastole when the semilunar cusps of the aortic valve and the pulmonary trunk are shut (the valve component) and by vibration of the walls at the point of origination of these vessels (the vascular component).
The intensity of myocardial and valvular vibrations depends on the rate of ventricular contractions: the higher the rate of their contractions and the faster the intraventricular pressure grows, the greater is the intensity of these vibrations.
Слайд 18Sequence of auscultation
The mitral valve - at the heart apex;
the aortic valve
Sequence of auscultation
The mitral valve - at the heart apex;
the aortic valve
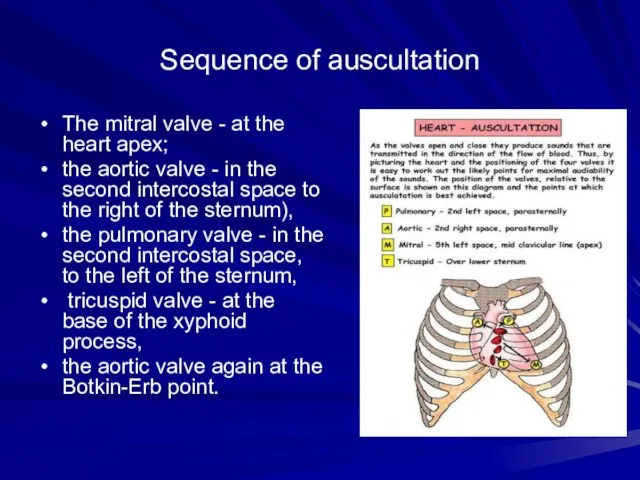
the pulmonary valve - in the second intercostal space, to the left of the sternum,
tricuspid valve - at the base of the xyphoid process,
the aortic valve again at the Botkin-Erb point.
Слайд 23Points of auscultation
Points of auscultation
Слайд 24Rules for auscultation of the heart.
The heart is usually auscultated by a
Rules for auscultation of the heart.
The heart is usually auscultated by a
The condition of the patient permitting, the heart sounds should be heard in various postures of the patient: erect, recumbent, after exercise (e.g. after repeated squatting).
Sounds associated with the mitral valve pathology are well heard when the patient lies on his left side, since the heart apex is at its nearest position to the chest wall; aortic valve defects are best heard when the patient is in the upright posture or when he lies on his right side.
The heart sounds are better heard if the patient is asked to inhale deeply and then exhale deeply and keep breath for short periods of time so that the respiratory sounds should not interfere with auscultation of the heart.
The valve sounds should be heard in the order of decreasing frequency of their affection. The mitral valve should be heard first (at the heart apex); next follows the aortic valve (in the second intercostal space to the right of the sternum), the pulmonary valve (in the second intercostal space, to the left of the sternum), tricuspid valve (at the base of the xiphoid process), and finally the aortic valve again at the Botkin-Erb point.
If any deviations from normal sounds have been revealed at these points, the entire heart area should be auscultated thoroughly.
Слайд 25Sequence of auscultation
Sequence of auscultation
Слайд 27Differential features of I and II heart sounds
I heart sound II
Differential features of I and II heart sounds
I heart sound II
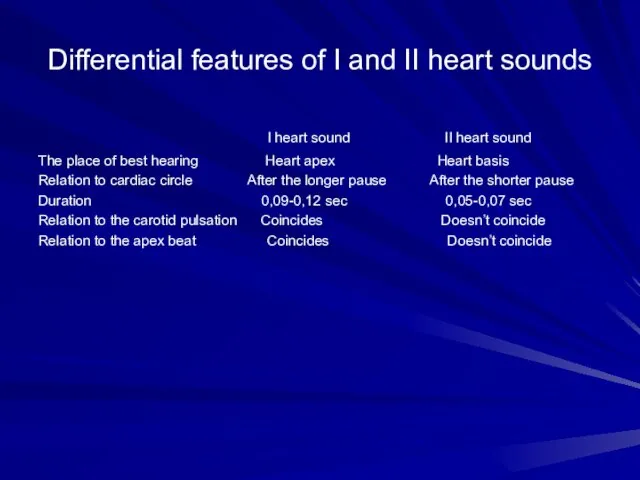
The place of best hearing Heart apex Heart basis
Relation to cardiac circle After the longer pause After the shorter pause
Duration 0,09-0,12 sec 0,05-0,07 sec
Relation to the carotid pulsation Coincides Doesn’t coincide
Relation to the apex beat Coincides Doesn’t coincide
Слайд 30For differentiation of I and II heart sounds in tachycardia it is
For differentiation of I and II heart sounds in tachycardia it is
Слайд 31Intensity of the heart sounds may depend on conditions of the sound
Intensity of the heart sounds may depend on conditions of the sound
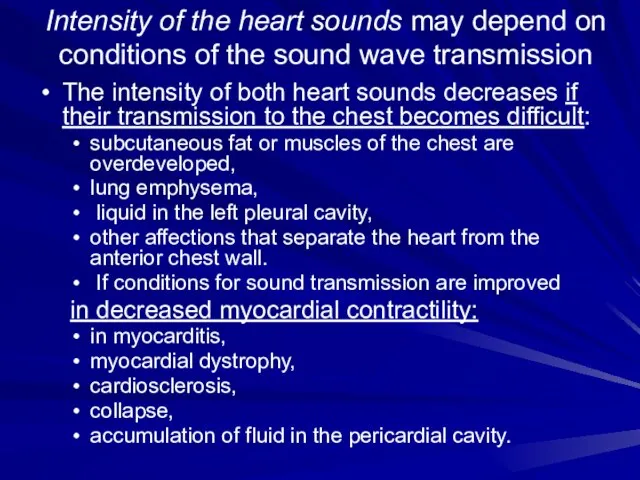
The intensity of both heart sounds decreases if their transmission to the chest becomes difficult:
subcutaneous fat or muscles of the chest are overdeveloped,
lung emphysema,
liquid in the left pleural cavity,
other affections that separate the heart from the anterior chest wall.
If conditions for sound transmission are improved
in decreased myocardial contractility:
in myocarditis,
myocardial dystrophy,
cardiosclerosis,
collapse,
accumulation of fluid in the pericardial cavity.
Слайд 32The intensity of the heart sounds increases if their transmission to the
The intensity of the heart sounds increases if their transmission to the
thin chest wall,
the lung edges are sclerosed,
the heart is pressed against the anterior chest wall by a growing tumour in the posterior mediastinum,
by the resonance in large empty cavities filled with air (a large cavern in the lung, large gastric air-bubble).
if the blood viscosity decreases (in anaemia) or left ventricular feeling drops (bleeding).
due to the effect of the sympathetic nervous system on the heart:
in physical and emotional strain,
during exercise,
in patients toxic goitre.
Слайд 33Scheme of weakening and intensification of both heart sounds
Scheme of weakening and intensification of both heart sounds
Слайд 34Separate changes of one heart sound (I or II):
First heart sound diminishes:
Separate changes of one heart sound (I or II):
First heart sound diminishes:
at the heart apex in stenotic aortal orifice,
In diffuse affections of the myocardium (due to dystrophy, cardiosclerosis or myocarditis), the first heart sound only may be diminished because its muscular component also diminishes in these cases.
The first sound increases at the heart apex if the left ventricle is not adequately filled with blood during diastole:
in stenosis of the left atrioventricular orifice,
In extrasystole.
The second sound can be inaudible over the aorta if:
the aortic valve is much destroyed,
diminishes over the aorta in cases with marked hypotension;
diminishes over the pulmonary trunk in cases with aortic valve incompetence (in very rare cases),
in decreased pressure in the lesser circulation.
The second sound may increase either over the aorta or over the pulmonary trunk indicating hypertension in the proper circle of circulation.
Слайд 35Splitting or reduplication of the sounds occurs in asynchronous work
and right chambers
Splitting or reduplication of the sounds occurs in asynchronous work and right chambers
Asynchronous closure of the right- and left ventricular valves splits the first sound while asynchronous closure of the
semilunar valves causes reduplication of the second heart sound.
Reduplication or splitting of the first sound is due to asynchronous closure of the atrioventricular valves, e.g. during very deep expiration, when the blood is ejected into the left atrium with a greater force to prevent the closure of the mitral valve;
Pathological reduplication of the first sound can occur in impaired intraventricular conduction (through the His bundle) as a result of delays systole of one of the ventricles.
Слайд 36The second sound is reduplicated more frequently
Reduplication occurs due to asynchronous closure
The second sound is reduplicated more frequently
Reduplication occurs due to asynchronous closure
The second heart sound can be duplicated in cases with, diminished or increased filling of one of the ventricles or when pressure in the aorta or the pulmonary artery changes.
Physiological reduplication of the second sound is mostly connected with various respiratory phases: the filling of the right and left ventricles differs during inspiration and expiration and the length of their systole changes, as well as the tinted of closure of the valve of the aorta and pulmonary trunk. The amount oil blood flowing to the left ventricle decreases during inspiration because part of blood is retained in the distended vessels of the lungs. The left ventricular systolic blood volume decreases during inspiration, its systole ends earlier, and the aortic valve therefore closes earlier as well. At the same time, the stroke volume of the right ventricle increases, its systole prolongs, the pulmonary valve closure is delayed and the second sound is thus doubled.
Pathological reduplication of the second sound can be due to delayed closure of the aortic valve in persons suffering from essential hypertension, or if the closure of the pulmonary valve is delayed at increased pressure in the lesser circulation (e.g. in mitral stenosis or emphysema of the lungs).
Слайд 37Scheme of reduplication of I and II heart sounds
Scheme of reduplication of I and II heart sounds
Слайд 38Adventitious heart sounds
The third heart sound (S3) is the result of vibrations
Adventitious heart sounds
The third heart sound (S3) is the result of vibrations
The forth heart sound (S4) is caused by the recoil of vibrations between the atria and ventricles following atrial contraction, at the end of diastole. It is rarely heard as a normal heart sound; usually it is considered indicative of further cardiac evaluation.
Both S3 and S4 may be recorded in heart failure indicating poor muscular tone of the left ventricle.
The mitral valve opening sound (opening snup) is heard at the heart apex of patients with mitral stenosis 0.07-0.13 s following the second sound, during diastole.
Extra-pericardial-sound can occur in pericardial adhesion. It originates during diastole, 0.08-0.14 s after the second sound, and is generated by the vibrating pericardium during the rapid dilatation of the ventricles at the beginning of diastole.
Слайд 40Heart melodies
Intensification of S3 or S4 sounds gives a three-sound or even
Heart melodies
Intensification of S3 or S4 sounds gives a three-sound or even
The gallop rrhythm is conditionally divides into protodiastolic (intensified III sound arises up though 0,12-0,2 sec. after second sound), mesodiastolic(at tachicardia descend coalescence of III and IV sounds and it is accepted at auscultation as a single sound) and presystolic (is conditioned by pathological IV cardiac sound).
A gallop rhythm is better auscultated directly by ear (together with a note is accepted mild impetus transmitted from heart on thoracal cage in diastole phase) in the apical region at left lateral recumbent position of the patient, in III- IV intercostal spaes to the left.
Слайд 41Triple rrhythm
(Rhithmus coeturnici)
It is a cardiac rhythm which is auscultated only
Triple rrhythm
(Rhithmus coeturnici)
It is a cardiac rhythm which is auscultated only
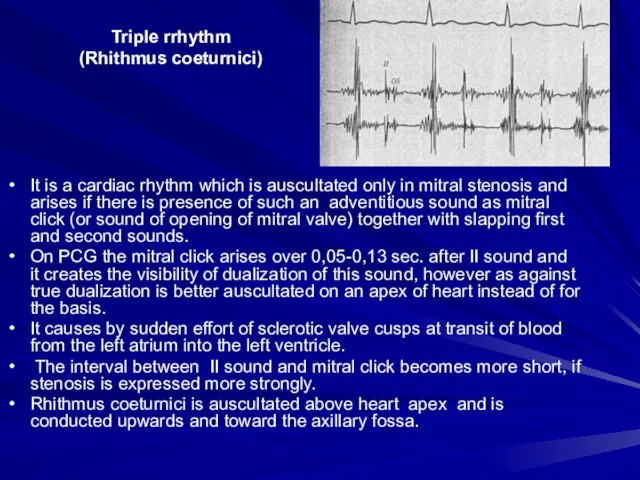
On PCG the mitral click arises over 0,05-0,13 sec. after II sound and it creates the visibility of dualization of this sound, however as against true dualization is better auscultated on an apex of heart instead of for the basis.
It causes by sudden effort of sclerotic valve cusps at transit of blood from the left atrium into the left ventricle.
The interval between II sound and mitral click becomes more short, if stenosis is expressed more strongly.
Rhithmus coeturnici is auscultated above heart apex and is conducted upwards and toward the axillary fossa.
Слайд 43Tripple rrhythm
Tripple rrhythm
Слайд 44Pendulum rhythm
In the case of pendulum rhythm the large (diastolic) heart pause
Pendulum rhythm
In the case of pendulum rhythm the large (diastolic) heart pause
Слайд 45Protodiastolic and presystolic gallop rrhythm
Protodiastolic and presystolic gallop rrhythm
Слайд 46Cardiac murmurs-
phenpmena which arise due to pathological blood flow in the heart
Intracardial
Cardiac murmurs-
phenpmena which arise due to pathological blood flow in the heart
Intracardial
Organic and functional (relative),
Systolic and diastolic,
Ejection and regurgitation murmurs,
They are also different in character, intensity, duration.
Extracardial (pericarial friction murmur and pleuropericardial murmur)
Слайд 47Properties of murmurs
Duration
The murmurs of mitral (and tricuspid) regurgitation start simultaneously with
Properties of murmurs
Duration
The murmurs of mitral (and tricuspid) regurgitation start simultaneously with
Character and pitch
The quality of murmurs is hard to define. Terms such as harsh, blowing, musical, rumbling, high or low pitched arc used. High-pitched murmurs often correspond with high-pressure gradients, so the diastolic murmur of aortic incompetence is higher pitched than that of mitral stenosis.
Location
Record the sitc(s) where you hear the murmur best. This helps to differentiate diastolic murmurs (mitral stenosis al the apex, aortic regurgitation at the left sternal edge), but is less helpful with systolic murmurs, which arc often loud and audible all over the precordium.
Radiation
Murmurs radiate in the direction of the blood flow causing the murmur to specific sites out with the precordium. Do nol j
Слайд 48Heart murmurs may be crescendo, diamond-shaped and descendo
Heart murmurs may be crescendo, diamond-shaped and descendo
Слайд 49Intensity
There are six grades of intensity used to describe murmurs. Diastolic murmurs
Intensity
There are six grades of intensity used to describe murmurs. Diastolic murmurs
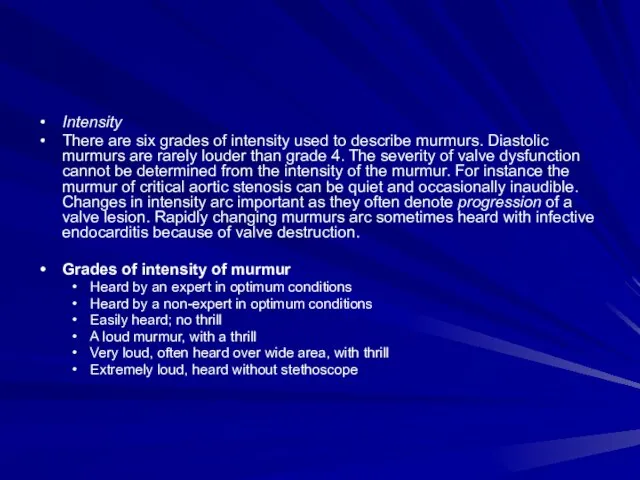
Grades of intensity of murmur
Heard by an expert in optimum conditions
Heard by a non-expert in optimum conditions
Easily heard; no thrill
A loud murmur, with a thrill
Very loud, often heard over wide area, with thrill
Extremely loud, heard without stethoscope
Слайд 50Causes of systolic murmurs
Ejection systolic murmur
Increased flow through normal valves
• 'Innocent systolic murmur':
fever
athletes
Causes of systolic murmurs
Ejection systolic murmur
Increased flow through normal valves
• 'Innocent systolic murmur':
fever
athletes
pregnancy (cardiac output maximum at 15 weeks)
Atrial septal defect (pulmonary flow murmur)
Severe anaemia
Normal or reduced flow though stenotic valve
Aortic stenosis
Pulmonary stenosis
Other causes of flow murmurs
Hypertrophic obstructive cardiomyopathy (obstruction at subvalvular level)
Aortic regurgitation (aortic flow murmur)
Pansystolic murmurs
I caused by a systolic leak from a high to a lower pressure chamber Mitral regurgitation Tricuspid regurgitation Ventricular septal defect Leaking mitral or tricuspid prosthesis
or bradycardia. Atrial septal defect is characterized
Слайд 54At an auscultation it is necessary to determine:
1) relation of murmur
At an auscultation it is necessary to determine:
1) relation of murmur
2) properties of murmur, its character, intensity, duration;
3) localization of murmur, i.e. place of the best auscultation;
4) condution of murmur (irradiation).
Слайд 55 Murmurs are auscultated better at points of auscultation of those valves,
Murmurs are auscultated better at points of auscultation of those valves,
The systolic murmur in mitral valve incompetene is best auscultated at heart apex; it can be conduted to axillary region or with blood bukflow from a left ventricle in the left atrium — to the second and third intercostal space to the left of a breast bone.
The diastolic murmur in narrowing of the left atrioventricular aperture is usually auscultated on a circumscribed field in apex area.
The systolic murmur in stenosis of aortic rout is audible in the second intercostal space to the right of a breast bone. As a rule, he is well onduted with blood flow towards caroti arteries. As for this defeect rasping and loud (sawing, scratching) murmur is characteristic it can be determined by auscultation above all heart region and can be onduted to interscapular space.
The diastolic murmur aortic valve inompetence is often better auscultated not above the aorti valve, but at Botkin-Erb’s point, where it is onduted with blood bukflow from the aorta to the left ventricle.
Слайд 56Differentiation of functional and organic murmurs
in the most cases functional murmurs are
Differentiation of functional and organic murmurs
in the most cases functional murmurs are
the murmurs are changeable, can arise and decrease in intensity or even disappear at various positions of a body, after an exercise, stress, in different phases of respiration;
most often they are auscultated above a pulmonary trunk, less often — above heart apex,
the murmurs are short, seldom occupy all systole; mild and blowing in character;
the murmurs are usually auscultated on a circumscribed field and are not conducted far from the place of occurence;
The functional murmurs are not accompanied by other attributes of valvular lesions (enlargement of heart chambers, change of sounds etc.).
Слайд 57The pericardial friction
It is develops in change of visceral and parietal pericardiac
The pericardial friction
It is develops in change of visceral and parietal pericardiac
The mechanism of its development is similar to the mechanism of creation of a pleural friction, only instead of respiratory movements the cause of its appearance is the movements of a heart during systole and diastole.
Differential features:
It is heart equally over the whole heart area,
It intensifies if to press motightly to the heart area with a phonendoscope and at inclination of a trunk forward ,
It is sinchronous with heart contractions (is heart in systole and diastole),
it is changeable, disappear and appear again.
Слайд 58The pleuropericardial friction murmur
It arises in inflammation of pleura, immediately accumbent to
The pleuropericardial friction murmur
It arises in inflammation of pleura, immediately accumbent to
As opposite to pericardial friction:
it is auscultated on the left edge of relative cardiac dullness;
is usually combined with pleural friction,
changes the intensity in different phases of respiration strengthens at a penetrating inspiration, when the edge mild adjoins to more closely to the heart, and weakens at expiration, at fall of edge mild sharply.
Слайд 59Phonocardiogram
Phonocardiogram
Слайд 61AUSCULTATION OF VESSELS
Auscultation of arteries. Arteries of medium calibre, such as the
AUSCULTATION OF VESSELS
Auscultation of arteries. Arteries of medium calibre, such as the
Слайд 62In norm:
Two sounds can be heard on the carotid and subclavian arteries
Two sounds can be heard on the carotid and subclavian arteries
The first sound is due to the tension of the arterial wall distended by the running pulse wave, and the second sound is transmitted onto these arteries from the aortic semilunar valve.
One systolic sound can sometimes be heard on the femoral artery.
In aortic incompetence:
the first sound over the arteries becomes louder because of the higher pulse wave, and it can be heard at greater distances from the heart, e.g. on the brachial and radial arteries.
Two sounds can sometimes be heard on the femoral artery in aortic incompetence. This doubled tone (Traube's doubled tone) is generated by intense vibration of the vascular wall during both systole and diastole.
The Vinogradov-Duroziez doubled tone can be heard in aortic incompetence over the femoral artery when it is compressed by a stethoscope bell. The first of these tones is stenotic murmur, which is due to the blood flow through a narrowed (by the pressure of the stethoscope) vessel, while the second sound is explained by the accelerated backflow to the heart during diastole.
Слайд 63Systolic sound produced by the stenosed aortal orifice is usually well transmitted
Systolic sound produced by the stenosed aortal orifice is usually well transmitted
Systolic sound associated with decreased viscosity of blood and increased flow rate (e.g. in anaemia, fever, exophthalmic goitre) can also be heard on these vessels.
Systolic sound sometimes appears in stenosis or aneurysmal dilation of large vessels.
Слайд 64Auscultation of veins
Neither sounds nor murmurs are normally heard over veins.
Auscultation
Auscultation of veins
Neither sounds nor murmurs are normally heard over veins.
Auscultation
It is better heard on the right jugular vein and becomes more intense when the patient turns the head in the opposite side.




 1С-Битрикс Корпоративный портал 10.0 – 10.5
1С-Битрикс Корпоративный портал 10.0 – 10.5 Presentation Title
Presentation Title  Заседание ученого советаПОИПКРО
Заседание ученого советаПОИПКРО СОЦИАЛЬНЫЙ ПРОЕКТ «Там на ухоженных дорожках»
СОЦИАЛЬНЫЙ ПРОЕКТ «Там на ухоженных дорожках» Цель, Процесс, Результат
Цель, Процесс, Результат Гражданское право РФ. Право собственности и иные вещные права
Гражданское право РФ. Право собственности и иные вещные права Энергосбережение в нашей жизни УО «ВГПЛ1 машиностроения им. М.Ф.Шмырева» http://vgpl-1.iatp.by. - презентация
Энергосбережение в нашей жизни УО «ВГПЛ1 машиностроения им. М.Ф.Шмырева» http://vgpl-1.iatp.by. - презентация Интегрированное занятие « Математика + история»
Интегрированное занятие « Математика + история» Тестовые задания
Тестовые задания 3_Биологическая роль воды
3_Биологическая роль воды Презентация на тему Умножение одночлена на многочлен
Презентация на тему Умножение одночлена на многочлен  Иван Сергеевич Тургенев. Начало творческого пути писателя
Иван Сергеевич Тургенев. Начало творческого пути писателя Геометрическая абстракция
Геометрическая абстракция Угол. Сравнение углов. Биссектриса угла
Угол. Сравнение углов. Биссектриса угла Конфликты в семье
Конфликты в семье Вот он цветочек аленький
Вот он цветочек аленький Итоги 2003/2004 учебного года и задачи кафедр по повышению качества подготовки специалистов в новом учебном году Б.Е.Ды
Итоги 2003/2004 учебного года и задачи кафедр по повышению качества подготовки специалистов в новом учебном году Б.Е.Ды Витамин D
Витамин D Профессия Повар-кондитер
Профессия Повар-кондитер Неделя английского языка2011-2012
Неделя английского языка2011-2012 История математической логики
История математической логики Япония 11 класс
Япония 11 класс Склады и пункты приема поставок
Склады и пункты приема поставок Информационно-аналитический проект: Сто дней
Информационно-аналитический проект: Сто дней Тех. задание
Тех. задание Возможности развития познавательной мотивации учащихся.
Возможности развития познавательной мотивации учащихся. Николай Константинович Рерих (874 - 1947)
Николай Константинович Рерих (874 - 1947) Внешняя память компьютера
Внешняя память компьютера