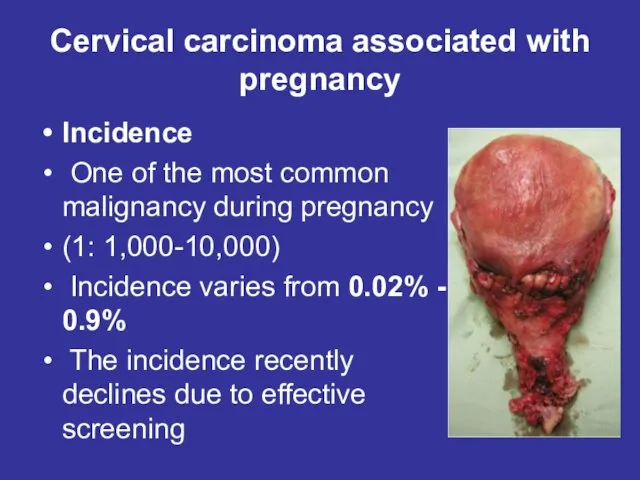
Слайд 2Cervical carcinoma associated with
pregnancy
Incidence
One of the most common malignancy during
pregnancy
(1: 1,000-10,000)
Incidence varies from 0.02% - 0.9%
The incidence recently declines due to effective screening
Слайд 3Physiological changes during pregnancy in the mucous membrane of the cervix
In the
I trimester of the cervix characterized by cyanosis and colposcopic noted the presence of whitish spot elevations due to physiological hypertrophy, and an extensive network of blood vessels.
In the II and III trimesters can be determined visually physiological ectopia prismatic epithelium and colposcopy - white spots on the background metaplastic epithelium vascular pattern. Changes regress within 2-4 months after birth
Слайд 4Symptoms and signs of cervical cancer during pregnancy
Early cervical cancer often doesn’t
have any noticeable signs or symptoms.
Late symptoms include:
- vaginal bleeding
- pelvic pain
- pain during sex.
Vaginal bleeding often regarded in the I trimester miscarriage as a threat, in the II and III trimester - like presentation or premature detachment of the placenta.
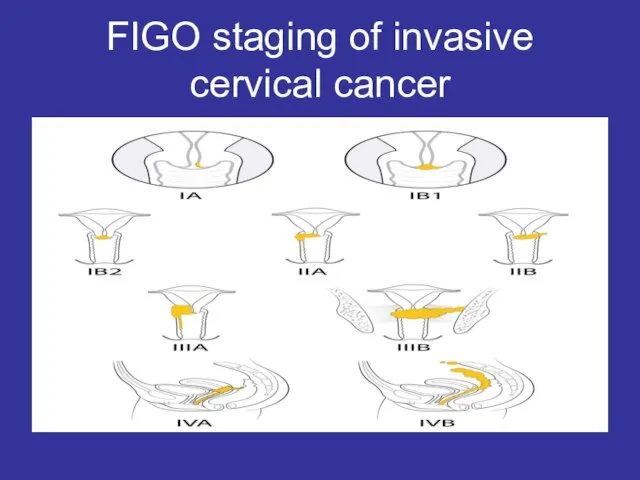
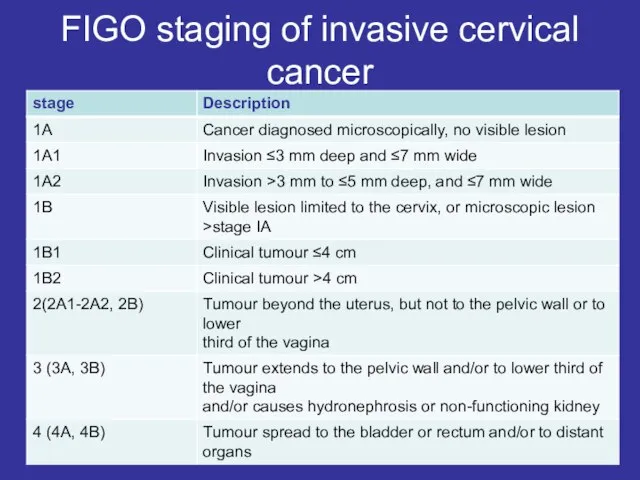
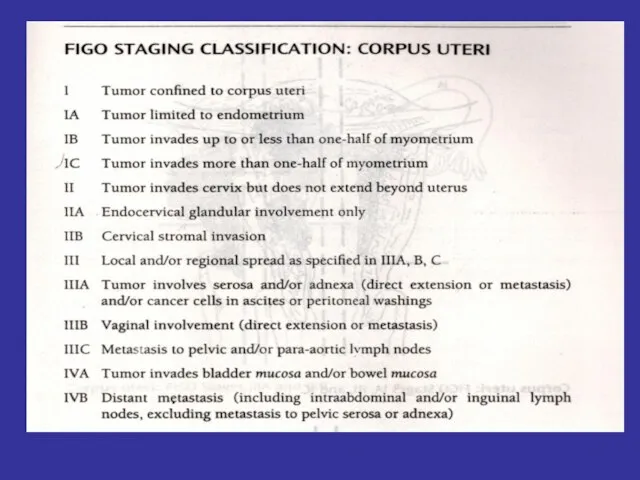
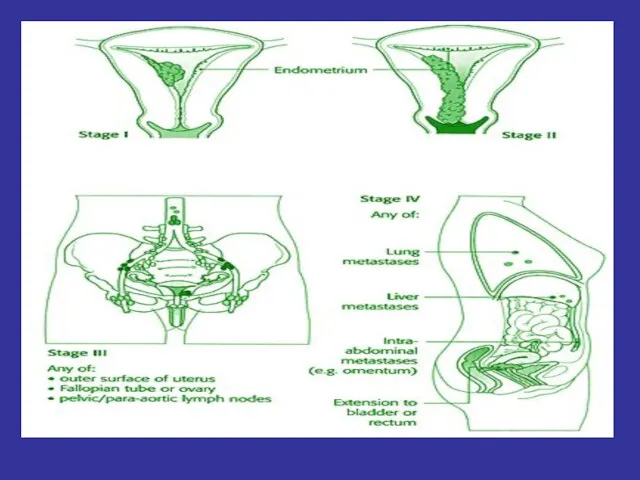
Слайд 5FIGO staging of invasive cervical cancer
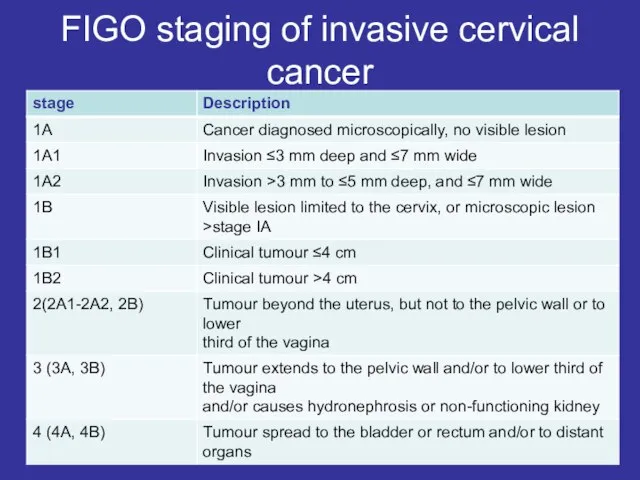
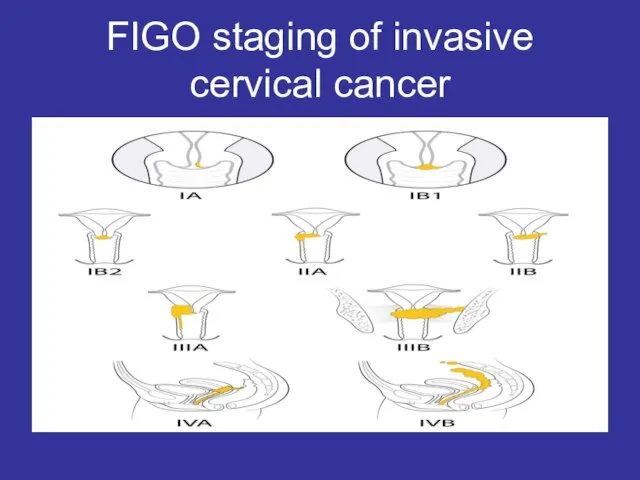
Слайд 6FIGO staging of invasive cervical cancer
Слайд 7Treatment of cervical cancer during pregnancy
The decision to continue the pregnancy should
be based on careful discussion of the cancer prognosis, treatment and future fertility with the woman and her partner and multidisciplinary team
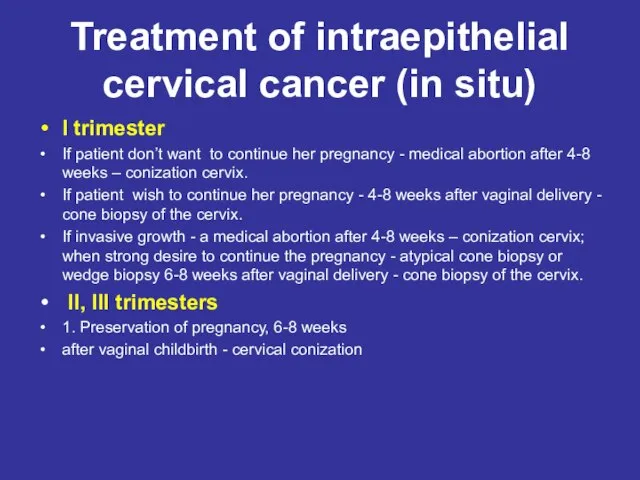
Слайд 8Treatment of intraepithelial cervical cancer (in situ)
I trimester
If patient don’t want to
continue her pregnancy - medical abortion after 4-8 weeks – conization cervix.
If patient wish to continue her pregnancy - 4-8 weeks after vaginal delivery - cone biopsy of the cervix.
If invasive growth - a medical abortion after 4-8 weeks – conization cervix; when strong desire to continue the pregnancy - atypical cone biopsy or wedge biopsy 6-8 weeks after vaginal delivery - cone biopsy of the cervix.
II, III trimesters
1. Preservation of pregnancy, 6-8 weeks
after vaginal childbirth - cervical conization
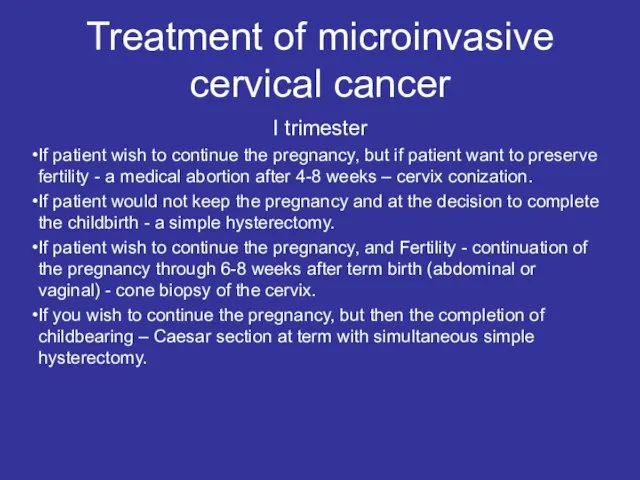
Слайд 9Treatment of microinvasive cervical cancer
I trimester
If patient wish to continue the
pregnancy, but if patient want to preserve fertility - a medical abortion after 4-8 weeks – cervix conization.
If patient would not keep the pregnancy and at the decision to complete the childbirth - a simple hysterectomy.
If patient wish to continue the pregnancy, and Fertility - continuation of the pregnancy through 6-8 weeks after term birth (abdominal or vaginal) - cone biopsy of the cervix.
If you wish to continue the pregnancy, but then the completion of childbearing – Caesar section at term with simultaneous simple hysterectomy.
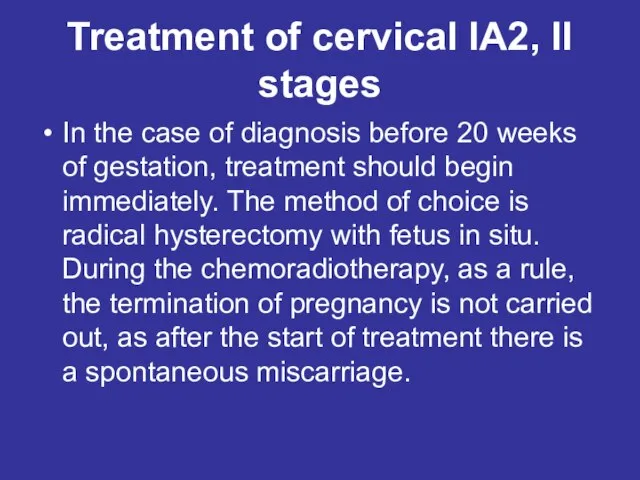
Слайд 10Treatment of cervical IA2, II stages
In the case of diagnosis before 20
weeks of gestation, treatment should begin immediately. The method of choice is radical hysterectomy with fetus in situ. During the chemoradiotherapy, as a rule, the termination of pregnancy is not carried out, as after the start of treatment there is a spontaneous miscarriage.
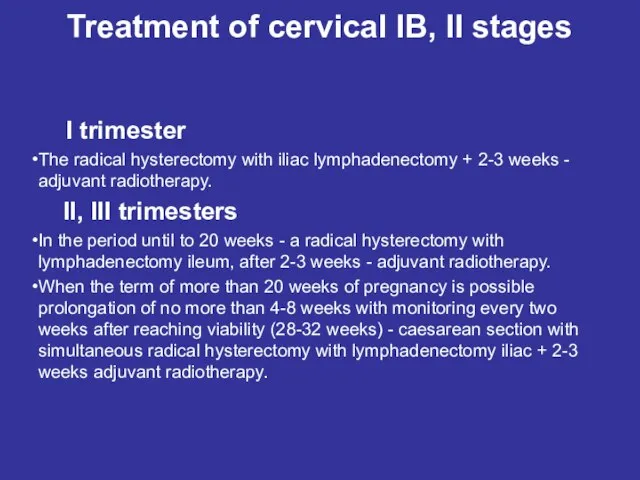
Слайд 11Treatment of cervical IB, II stages
I trimester
The radical hysterectomy with
iliac lymphadenectomy + 2-3 weeks - adjuvant radiotherapy.
II, III trimesters
In the period until to 20 weeks - a radical hysterectomy with lymphadenectomy ileum, after 2-3 weeks - adjuvant radiotherapy.
When the term of more than 20 weeks of pregnancy is possible prolongation of no more than 4-8 weeks with monitoring every two weeks after reaching viability (28-32 weeks) - caesarean section with simultaneous radical hysterectomy with lymphadenectomy iliac + 2-3 weeks adjuvant radiotherapy.
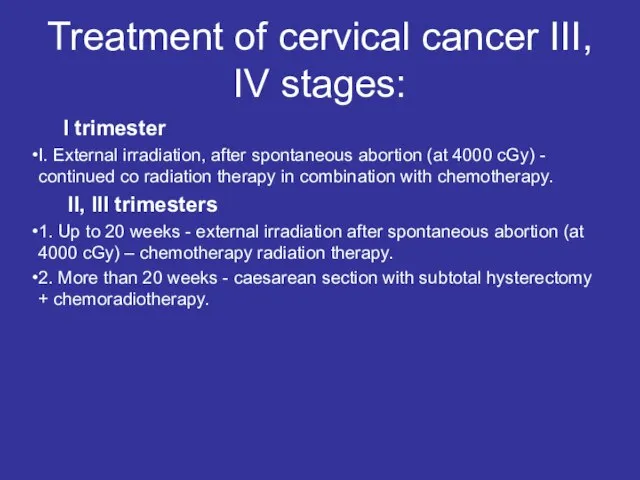
Слайд 12Treatment of cervical cancer III, IV stages:
I trimester
I. External irradiation, after
spontaneous abortion (at 4000 cGy) - continued co radiation therapy in combination with chemotherapy.
II, III trimesters
1. Up to 20 weeks - external irradiation after spontaneous abortion (at 4000 cGy) – chemotherapy radiation therapy.
2. More than 20 weeks - caesarean section with subtotal hysterectomy + chemoradiotherapy.
Слайд 17Cancer During Pregnancy
Cancer during pregnancy is uncommon. It occurs in only about
one out of every 1,000 pregnancies. For many years, both doctors and women were often unsure about how to deal with cancer during pregnancy. But now more women with cancer and their doctors are starting or continuing treatment while pregnant. This means more information about treating and living with cancer during pregnancy is available than ever before.
Слайд 18Diagnosing cancer during pregnancy
Being pregnant may delay a cancer diagnosis. This is
because some cancer symptoms, such as bloating, headaches, breast changes, or rectal bleeding, are also common during pregnancy. On the other hand, pregnancy can sometimes uncover cancer. For example, a Pap test done as part of standard pregnancy care can detect cervical cancer. And an ultrasound performed during pregnancy could find ovarian cancer.
Слайд 19Cancer treatment during pregnancy
When making treatment decisions for cancer during pregnancy, it
is important to consider the best treatment options for the pregnant woman balanced against the possible risks to the growing baby.
Слайд 20Treatment recommendations are based on many factors, including the following
Stage of the
pregnancy
The type, location, size, and stage of the cancer
The woman’s and her family’s wishes
Слайд 21Treatment must be carefully planned to ensure the woman and unborn baby
are safe. In general, treatment during pregnancy requires close teamwork with a multidisciplinary team, including both cancer doctors as well as high-risk obstetricians. These professionals can closely monitor the woman during treatment and make sure the baby is healthy.
Слайд 22Treatments that may be used during pregnancy
Surgery is the removal of the tumor
and some of the surrounding healthy tissue. It poses little risk to the growing baby and is considered the safest cancer treatment during pregnancy.
Слайд 23Chemotherapy.
There is a risk of harm to the fetus if chemotherapy is
given in the first three months of pregnancy. This is when the fetus's organs are still growing. Chemotherapy during the first trimester carries risk of birth defects or pregnancy loss.
Слайд 24During the second and third trimesters, doctors can give several types of
chemotherapy without apparent risk to the fetus. Because the placenta acts as a barrier between the women and the baby, some drugs cannot pass through, or they pass through in very small amounts. Studies have suggested babies exposed to chemotherapy while in the mother’s uterus do not show any abnormalities either immediately after delivery, or during their future growth and development, when compared with children not exposed to chemotherapy.
Слайд 25Radiation therapy.
Radiation therapy is the use of high-energy x-rays to destroy cancer cells.
Because radiation therapy can harm the fetus in all trimesters, doctors generally avoid using this treatment during pregnancy. The risks to the developing baby depend on the dose of radiation and the area of the body being treated.
Слайд 26Breastfeeding during treatment
Doctors advise women who are receiving chemotherapy after a pregnancy
not to breastfeed. Chemotherapy can transfer to the infant through breast milk.


 IKKOMAX - производитель продукции премиум-класса
IKKOMAX - производитель продукции премиум-класса СОЗДАНИЕ ИНФОРМАЦИОННОГО ПОЛЯ ФИРМЫ
СОЗДАНИЕ ИНФОРМАЦИОННОГО ПОЛЯ ФИРМЫ  Паломництво_до_святинь_Польщі_–
Паломництво_до_святинь_Польщі_– ФОРУМ « СОЗДАЙ СЕБЯ САМ»- представление молодежных инициатив в определении будущей карьеры и развития рынка труда
ФОРУМ « СОЗДАЙ СЕБЯ САМ»- представление молодежных инициатив в определении будущей карьеры и развития рынка труда Voronezh State University
Voronezh State University Тест по пьесе А.Вампилова «Старший сын»
Тест по пьесе А.Вампилова «Старший сын» «Гражданином быть обязан!»
«Гражданином быть обязан!» Лев Николаевич Толстой человек был непростой
Лев Николаевич Толстой человек был непростой Презентация проекта Международный социальный проект об условиях труда и зарплатах в Украине Mojazarplata.com.ua WageIndicator Foundation. - презентаци
Презентация проекта Международный социальный проект об условиях труда и зарплатах в Украине Mojazarplata.com.ua WageIndicator Foundation. - презентаци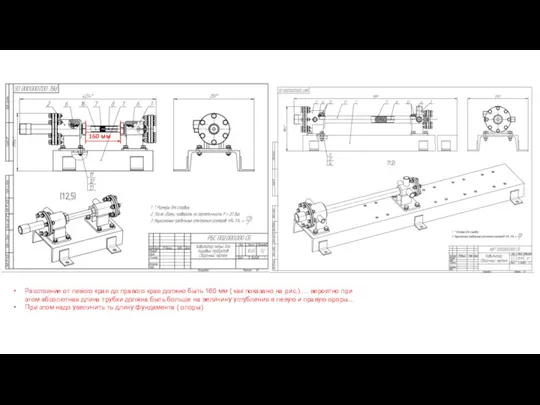 Сравнение и замечания кавитаторов
Сравнение и замечания кавитаторов Презентация на тему Как ориентироваться в лесу
Презентация на тему Как ориентироваться в лесу БЕЛЫЙ МЕДВЕДЬ - КОРОЛЬ СНЕЖНОЙ ПУСТЫНИ
БЕЛЫЙ МЕДВЕДЬ - КОРОЛЬ СНЕЖНОЙ ПУСТЫНИ Подвижные и спортивные игры
Подвижные и спортивные игры Мир профессий
Мир профессий Спостереження за моїм собакою
Спостереження за моїм собакою Презентация на тему Окружающий мир как иерархическая система (9 класс)
Презентация на тему Окружающий мир как иерархическая система (9 класс) Загадки для малышей про посуду
Загадки для малышей про посуду ООО «АвтоПриборМаш»
ООО «АвтоПриборМаш» Российская мечта о «Левиттауне» – опыт американских предпринимателей в массовом строительстве загородного жилья
Российская мечта о «Левиттауне» – опыт американских предпринимателей в массовом строительстве загородного жилья Как начать свой бизнес
Как начать свой бизнес Национально – государственное устройство
Национально – государственное устройство Сайдинг. Виды сайдинга
Сайдинг. Виды сайдинга Аджигардак 1981 март 14-15
Аджигардак 1981 март 14-15 Разработкатестов знаний
Разработкатестов знаний ШЭ ВсОШ 2022-2023 СГ (1)
ШЭ ВсОШ 2022-2023 СГ (1) Градус, транспортир, измерение углов
Градус, транспортир, измерение углов Презентация на тему Имя прилагательное
Презентация на тему Имя прилагательное  Мониторинг воздействия деятельности человека на окружающую среду и Здоровье
Мониторинг воздействия деятельности человека на окружающую среду и Здоровье