Содержание
- 2. Use of this Slide Set Presentation information is listed in the notes section below the slide
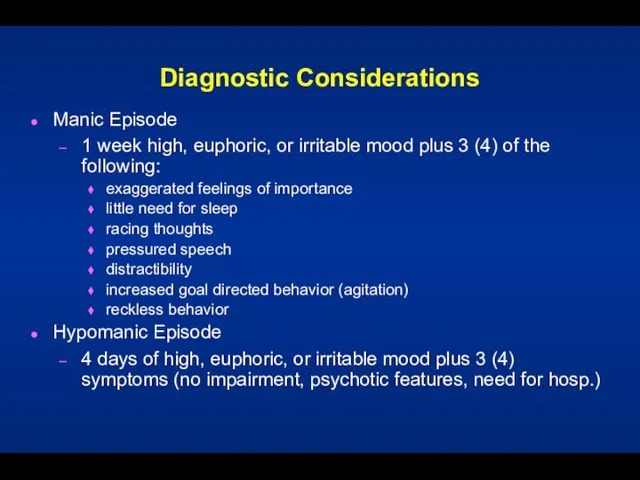
- 3. Diagnostic Considerations Manic Episode 1 week high, euphoric, or irritable mood plus 3 (4) of the
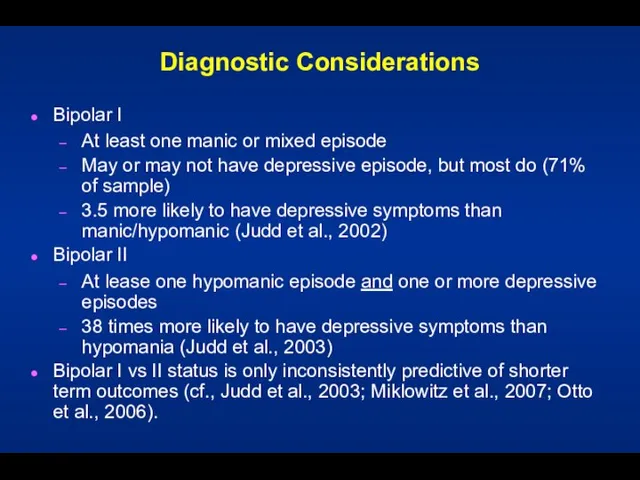
- 4. Diagnostic Considerations Bipolar I At least one manic or mixed episode May or may not have
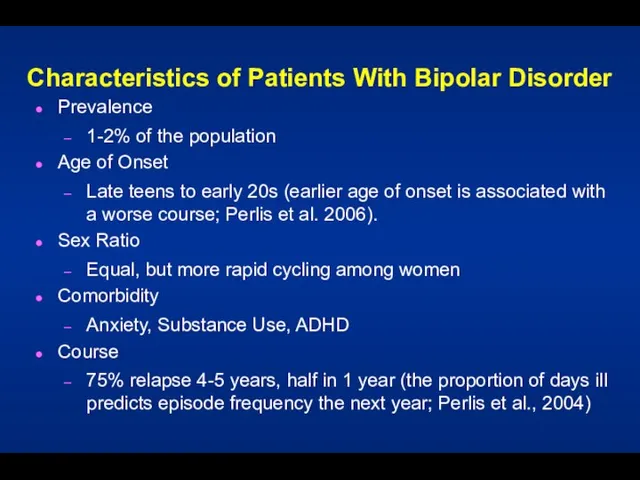
- 5. Characteristics of Patients With Bipolar Disorder Prevalence 1-2% of the population Age of Onset Late teens
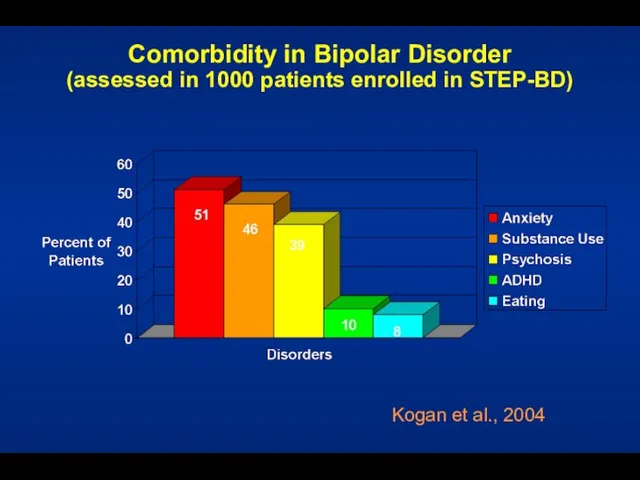
- 6. Comorbidity in Bipolar Disorder (assessed in 1000 patients enrolled in STEP-BD) Kogan et al., 2004
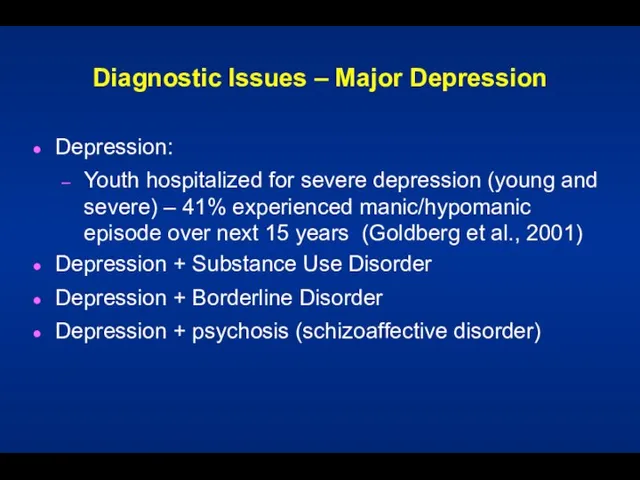
- 7. Diagnostic Issues – Major Depression Depression: Youth hospitalized for severe depression (young and severe) – 41%
- 8. Presentation with Psychosis Is it mania? Schizophrenia? Substance Induced? Schizoaffective? History and family help
- 9. An Abundance of Distress and Disability Family, job, personal Post-episode studies 6 months after: 30% unable
- 10. Psychosocial Treatment
- 11. Topics What is the evidence for the efficacy of psychotherapy for bipolar disorder? What are the
- 12. Psychosocial Treatment for Bipolar Disorder Initial Encouragement: Psychosocial Predictors of Bipolar Course Incomplete Efficacy of Mood
- 13. Role of Psychosocial Factors in Bipolar Disorder Psychosocial stressors impact the course of bipolar disorder: Family
- 14. Pharmacotherapy for Bipolar Disorder Advances in the field, but among patients taking medications: Half relapse first
- 15. Focused Psychosocial Treatments for Bipolar Disorder The product of diverse theoretical orientations, but with a high
- 16. Common Treatment Elements Among CBT, IPSRT, FFT Psychoeducation providing a model of the disorder and risk
- 17. 1. Cochran (1983) 2. Perry et al. (1999) 3. Lam et al. (2000), Lam et al.
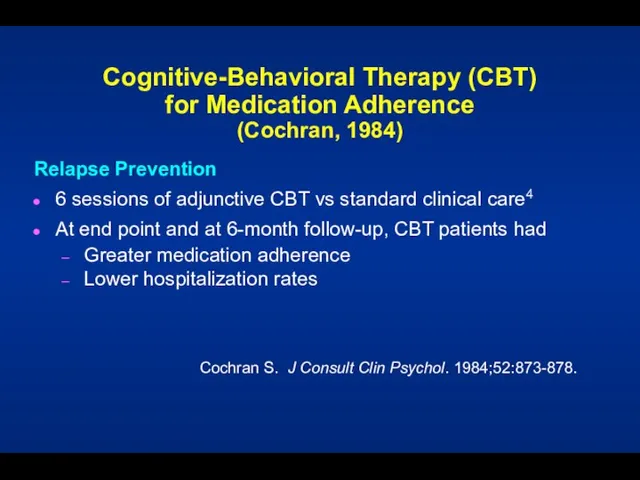
- 18. Cochran S. J Consult Clin Psychol. 1984;52:873-878. Cognitive-Behavioral Therapy (CBT) for Medication Adherence (Cochran, 1984) Relapse
- 19. Lam et al. - An Early CBT Success 103 bipolar patients randomized to CBT or TAU
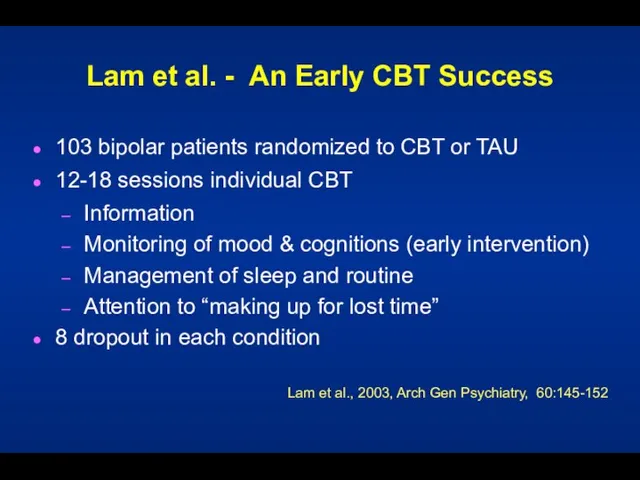
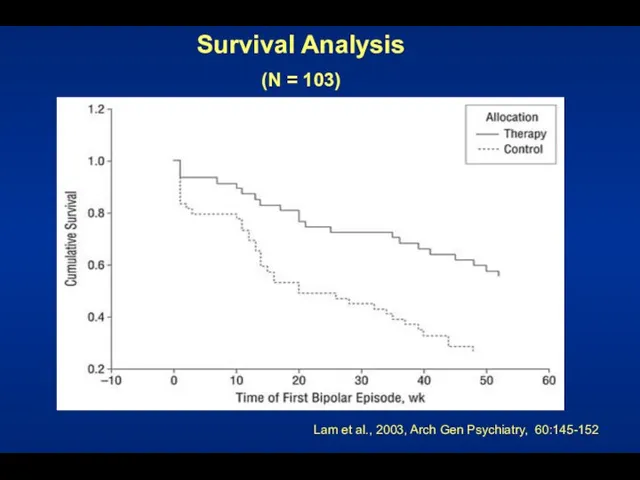
- 20. Medication Adherence Lam et al., 2003, Arch Gen Psychiatry, 60:145-152 Percent of Patients
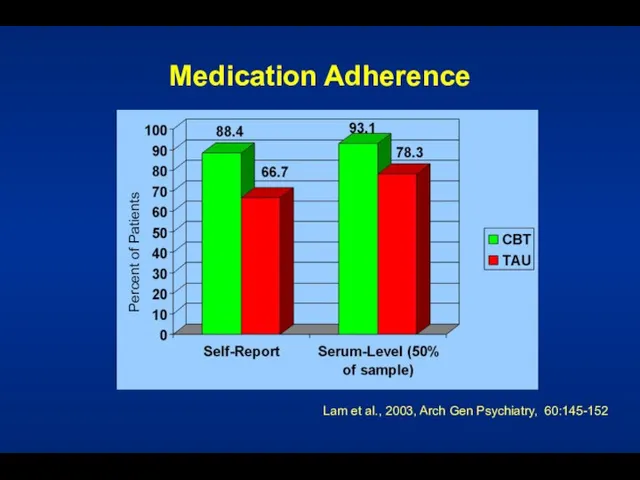
- 21. Clinical Outcome (days ill over 1 year) Lam et al., 2003, Arch Gen Psychiatry, 60:145-152 Mean
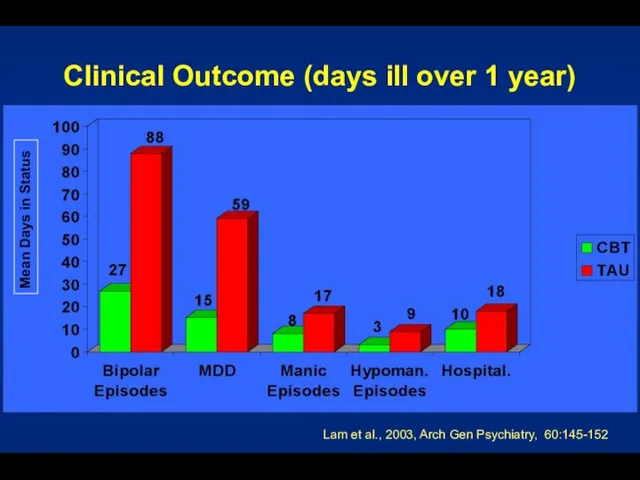
- 22. Survival Analysis (N = 103) Lam et al., 2003, Arch Gen Psychiatry, 60:145-152
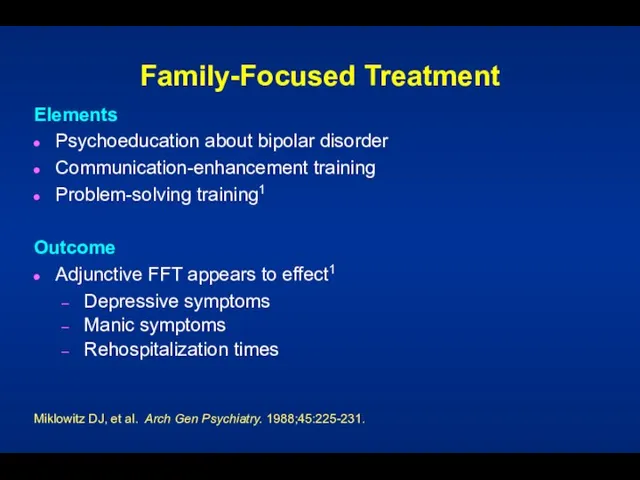
- 23. Family-Focused Treatment Elements Psychoeducation about bipolar disorder Communication-enhancement training Problem-solving training1 Outcome Adjunctive FFT appears to
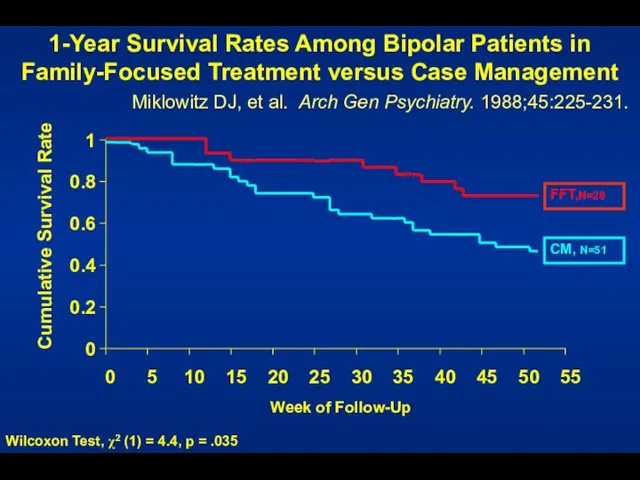
- 24. 0 0.2 0.4 0.6 0.8 1 0 5 10 15 20 25 30 35 40 45
- 25. Six Objectives of FFT Help the patient and her or his relatives to: Understand the nature
- 26. Interpersonal and Social Rhythm Therapy Educate patient about bipolar disorder Identify current interpersonal problem areas (e.g.,
- 27. Colom F, et al. Arch Gen Psychiatry. 2003;60:402-407. Group Psychoeducation vs. Standard Care 21 Weeks of
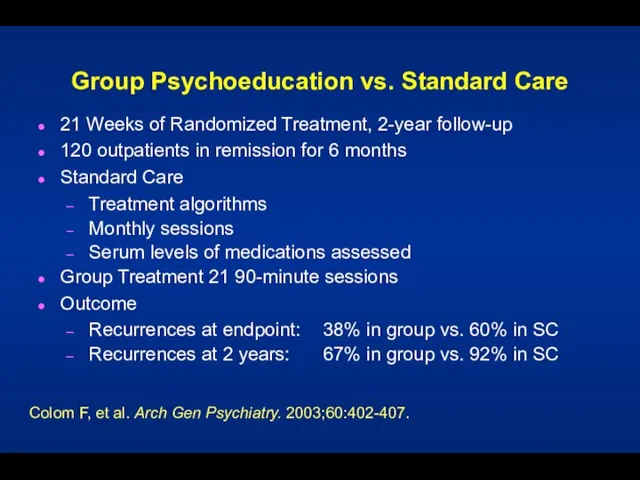
- 28. Colom F, et al. Arch Gen Psychiatry. 2003;60:402-407. Psychoeducation? Psychoeducation What is bipolar illness Symptoms Treatments
- 29. CBT, IPSRT, FFT vs. Collab Care for Bipolar Depression Miklowitz et al., 2007, Archives Gen Psychiatry
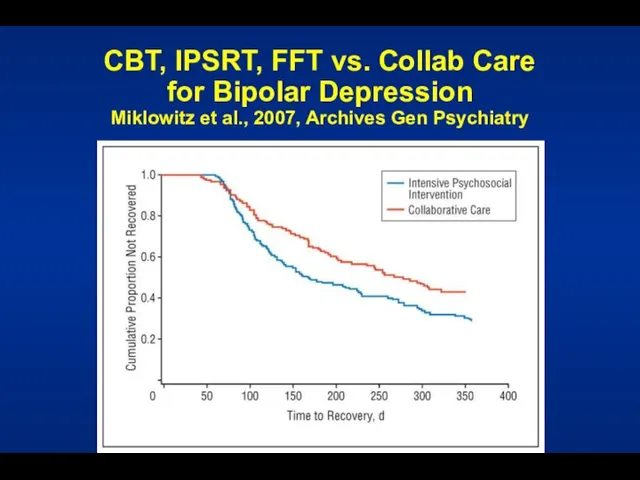
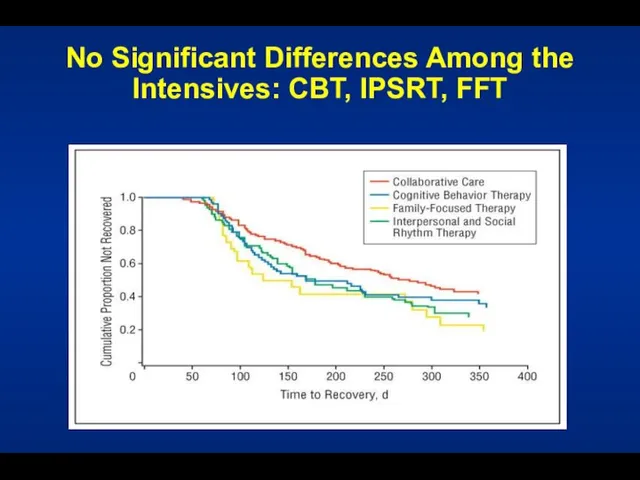
- 30. No Significant Differences Among the Intensives: CBT, IPSRT, FFT
- 31. Given this Evidence... ...What are Some Targets for Psychotherapy? Medication adherence Early detection and intervention Stress
- 32. Medication Non-Adherence in Mood Disorder 98 patients taking mood stabilizers (80% bipolar) 50% non-adherence rate last
- 33. Relapse Prevention Patient as cotherapist Treatment contract Training in early detection Use of treatment team
- 34. Individualized Treatment Contract Why contract? Formulate a plan for the future How I know I am
- 35. Mood Charting Enables early and accurate identification of changes in mood Allows for early intervention prior
- 36. Strategies for Hypomania Explore medical solutions (e.g., dosage or medication changes) Counteract impulsivity Give car keys
- 37. Cognitive-Behavioral Therapy for Bipolar Depression/Relapse Prevention Structure of Sessions Review of symptoms, progress, and problems Construction
- 38. Cognitive Restructuring and Skill Acquisition Restructuring Education (role and nature of thoughts) Self-monitoring of thoughts Identification
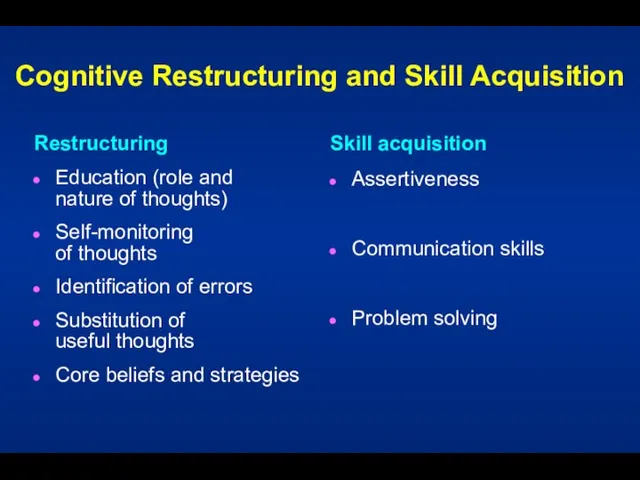
- 39. Cognitive Restructuring Examine the evidence for the thought Generate alternative explanations De-catastrophize Debunk “shoulds” Find the
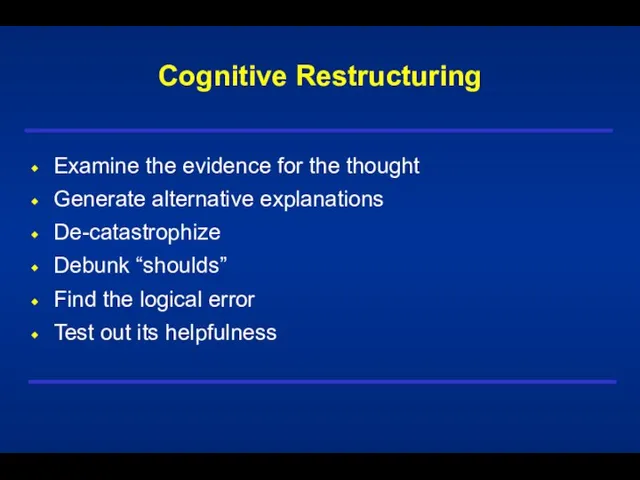
- 40. Questions Used to Formulate Rational Response What is the evidence that the automatic thought is true?
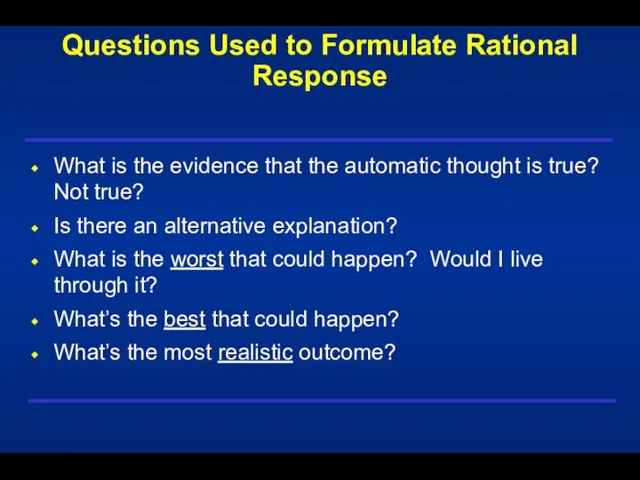
- 41. Questions Used to Formulate Rational Response (Cont’d) What is the effect of my believing the automatic
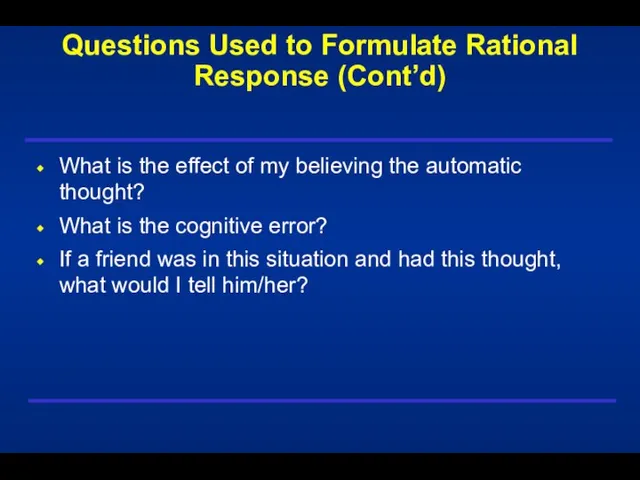
- 42. Respecting Hot Emotions Interventions are in relation to, not in spite of, the patient’s current mood.
- 43. Activity Assignments: Bipolar Disorder Management of sleep Management of over/under activity Management of destructive activities (substance
- 44. Activity Assignments - 1 Independent Intervention or used in conjunction with cognitive restructuring Help ensure that
- 45. Activity Assignments - 2 Monitor current Activities For change: Start small (where the patient is) Be
- 46. Activity Assignments - 3 Review performance relative to objective criteria (and the degree of mood disturbance)
- 47. Well-Being Therapy Phase In this phase, therapeutic effort and monitoring is devoted to increasing periods of
- 48. End of Treatment Patient has skills to act as his or her own therapist Patient focuses
- 49. Cognitive-Behavioral Therapy for Comorbid Disorders Anxiety disorders Substance use disorders Eating disorders
- 51. Скачать презентацию
 Отечественная война 1812 года
Отечественная война 1812 года  Система координат
Система координат Роль заместителя директора в процессе внедрения и использования АСУ РСО в образовательном учреждении
Роль заместителя директора в процессе внедрения и использования АСУ РСО в образовательном учреждении Интегрированные занятия учителя логопеда и психологас учащимися с задержкой психического развития.
Интегрированные занятия учителя логопеда и психологас учащимися с задержкой психического развития. 5.4 (2)
5.4 (2) Можно ли оправдать Емельяна Пугачёва?
Можно ли оправдать Емельяна Пугачёва? Vlasova Liudmila V. Slavsk Local Library, methodologist (Kalinigrad Region) Slavsk Local Library, methodologist (Kalinigrad Region)
Vlasova Liudmila V. Slavsk Local Library, methodologist (Kalinigrad Region) Slavsk Local Library, methodologist (Kalinigrad Region) Презентация на тему Неарктическое царство
Презентация на тему Неарктическое царство  Тест “Какой вы родитель?”
Тест “Какой вы родитель?” I-я районная межшкольная конференция
I-я районная межшкольная конференция Урок литературы в 5 классе (по рассказу Л.Н.Толстого «Кавказский пленник»)
Урок литературы в 5 классе (по рассказу Л.Н.Толстого «Кавказский пленник») Способы убийства людей в концлагере Саласпилс
Способы убийства людей в концлагере Саласпилс Особенности проведения ГВЭ-11 в дополнительный сентябрьский период в 2021 году
Особенности проведения ГВЭ-11 в дополнительный сентябрьский период в 2021 году Системы динамометрирования
Системы динамометрирования Мой страх. Занятие 5
Мой страх. Занятие 5 Организация библиотечного обслуживания населения Архангельской области в контексте реформы местн
Организация библиотечного обслуживания населения Архангельской области в контексте реформы местн Небесные гости (2 класс)
Небесные гости (2 класс) СИЛА ТОКА Кл t А q ЗАРЯД Дж U U q НАПРЯЖЕНИЕ А I I t РАБОТА с А q t ВРЕМЯ В q.
СИЛА ТОКА Кл t А q ЗАРЯД Дж U U q НАПРЯЖЕНИЕ А I I t РАБОТА с А q t ВРЕМЯ В q. Узоры на посуде
Узоры на посуде Новые технологии!
Новые технологии! Внешнее строение тела человека
Внешнее строение тела человека 20170829_zagadki
20170829_zagadki Уход за одеждой из хлопчатобумажных и льняных, шерстяных и шелковых, искусственных и синтетических тканей
Уход за одеждой из хлопчатобумажных и льняных, шерстяных и шелковых, искусственных и синтетических тканей Co to jest
Co to jest Публичный доклад муниципального образовательного учреждения средней общеобразовательной школы № 117 Красноармейского района
Публичный доклад муниципального образовательного учреждения средней общеобразовательной школы № 117 Красноармейского района  Йомаклы әлифба
Йомаклы әлифба Moral development
Moral development Группа компаний «МАГНОЛИЯ»
Группа компаний «МАГНОЛИЯ»