Содержание
- 2. History of epigastric pain present in 80-90 % of patient, but is nonspecific. Burning epigastric pain
- 3. PEPTIC ULCER DISEASE The term 'peptic ulcer' refers to an ulcer in the lower oesophagus, stomach
- 4. Ulcers are defined as a break in the mucosal surface >5 mm in size, with depth
- 5. Why does the ulcer appear ? Let’s remember the physiology of gastric secretion. Hydrochloric acid and
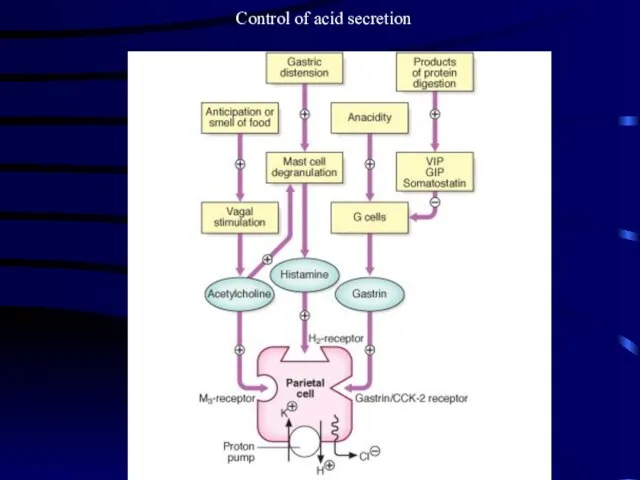
- 6. Control of acid secretion
- 7. The gastric epithelium is under a constant assault by a series of endogenous noxious factors including
- 8. The mucosal defense system can be envisioned as a three-level barrier, composed of preepithelial, epithelial, and
- 9. Surface epithelial cells provide the next line of defense through several factors, including mucus production, epithelial
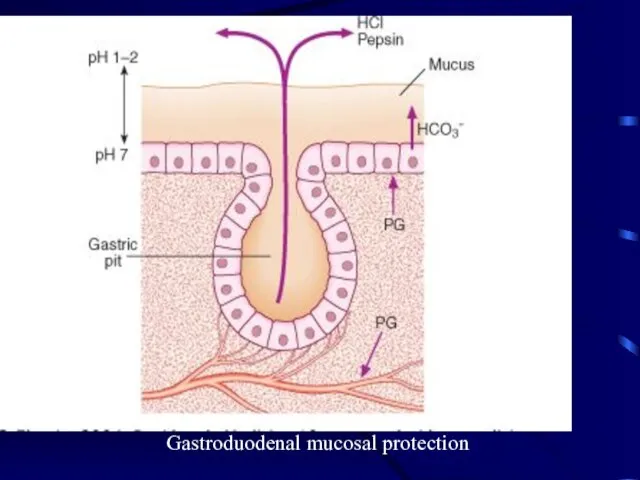
- 10. Prostaglandins play a central role in gastric epithelial defense/repair. The gastric mucosa contains abundant levels of
- 11. Gastroduodenal mucosal protection
- 12. GASTRIC AND DUODENAL ULCER Although the prevalence of peptic ulcer is decreasing in many Western communities,
- 13. Etiology: Helicobacter pylori In the industrialised world the prevalence of H. pylori infection in the general
- 14. The Bacterium initially named Campylobacter pyloridis, is a gram-negative microaerophilic rod found most commonly in the
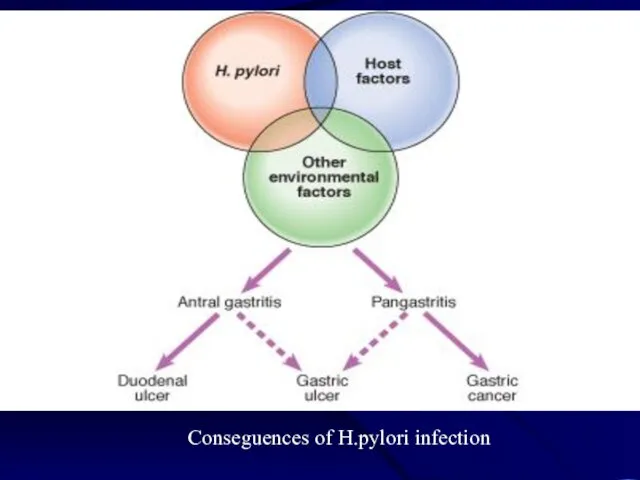
- 15. Conseguences of H.pylori infection
- 16. Pathogenesis and pathophysiology of infection
- 17. In most people H. pylori causes antral gastritis associated with depletion of somatostatin (from D cells)
- 18. In approximately 1% of infected people, H. pylori causes a pangastritis leading to gastric atrophy and
- 19. MISCELLANEOUS PATHOGENETIC FACTORS IN PEPTIC ULCER DISEASE Cigarette smoking Genetic predisposition Psychological stress Diet NSAID
- 20. Cigarette smoking has been implicated in the pathogenesis of PUD. Not only have smokers been found
- 21. Genetic predisposition has also been considered to play a role in ulcer development. First-degree relatives of
- 22. Psychological stress has been thought to contribute to PUD, but studies examining the role of psychological
- 23. Diet has also been thought to play a role in peptic diseases. Certain foods can cause
- 24. NSAIDs About 20,000 patients die each year from serious gastrointestinal complications from NSAIDs. Unfortunately, dyspeptic symptoms
- 25. Multiple factors play a role in the pathogenesis of PUD. The two predominant causes are H.
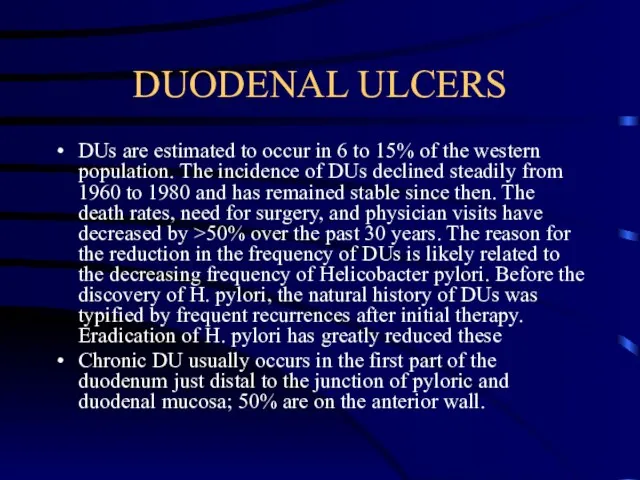
- 26. DUODENAL ULCERS DUs are estimated to occur in 6 to 15% of the western population. The
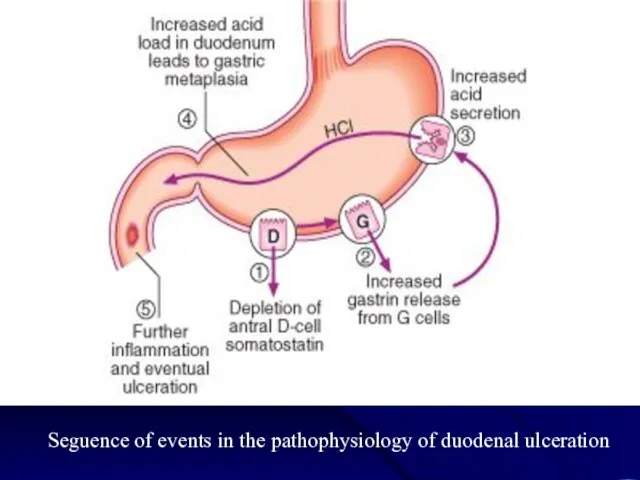
- 27. Seguence of events in the pathophysiology of duodenal ulceration
- 28. GASTRIC ULCERS As in DUs, the majority of GUs can be attributed to either H. pylori
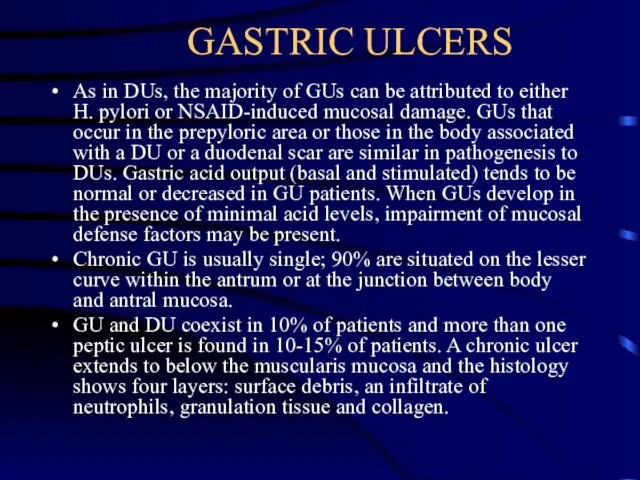
- 29. Clinical features Abdominal pain is common to many gastrointestinal disorders, including DU and GU, but has
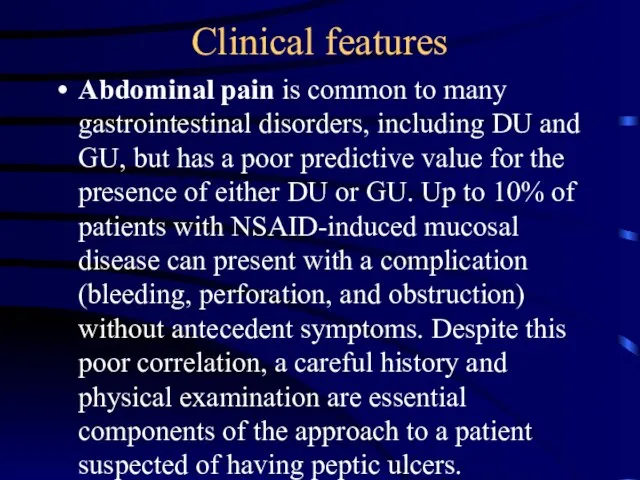
- 30. Epigastric pain described as a burning or gnawing discomfort can be present in both DU and
- 31. Variation in the intensity or distribution of the abdominal pain, as well as the onset of
- 32. Diagnostic Evaluation Including such methods as Barium studies of the proximal gastrointestinal tract, Endoscopy Several biopsy
- 33. Investigations The diagnosis can be made by double-contrast barium meal examination or by endoscopy. - Endoscopy
- 34. Tests for H. pylori Tests for H. pylori can be divided into two groups: invasive tests,
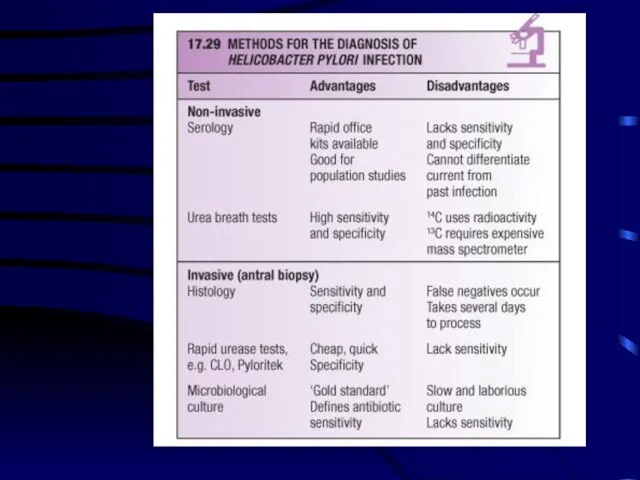
- 36. If endoscopy is performed, the most convenient biopsy-based test is the biopsy urease test, in which
- 37. The most consistently accurate test is the urea breath test. In this simple test, the patient
- 38. Management The aims of management are: - to relieve symptoms, - induce ulcer healing in the
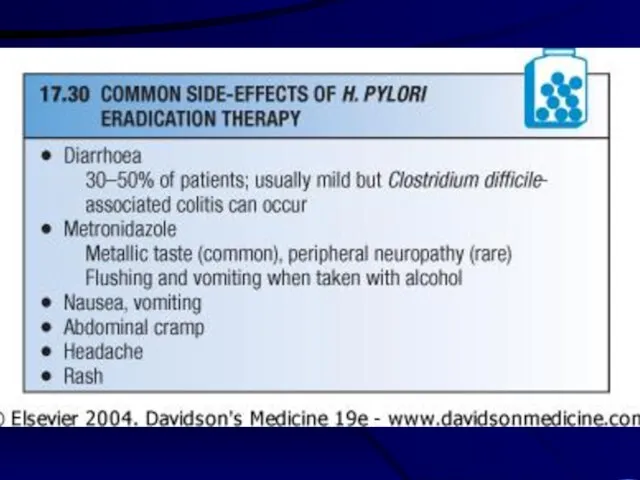
- 39. H. pylori eradication First-line (triple) therapy: IPP at standart dose (12-hourly) for eg. - rabeprasol Amoxicillin
- 40. H. pylori eradication Second-line (quadruple) therapy: IPP at standart dose (12-hourly) bismuth 120 mg 6-hourly tetracicline
- 43. General measures Cigarette smoking, aspirin and NSAIDs should be avoided. Alcohol in moderation is not harmful
- 44. Short-term management Many different drugs are available for the short-term management of acid peptic symptoms -
- 45. Histamine H2-receptor antagonist drugs. These are competitive inhibitors of histamine at the H2-receptor on the parietal
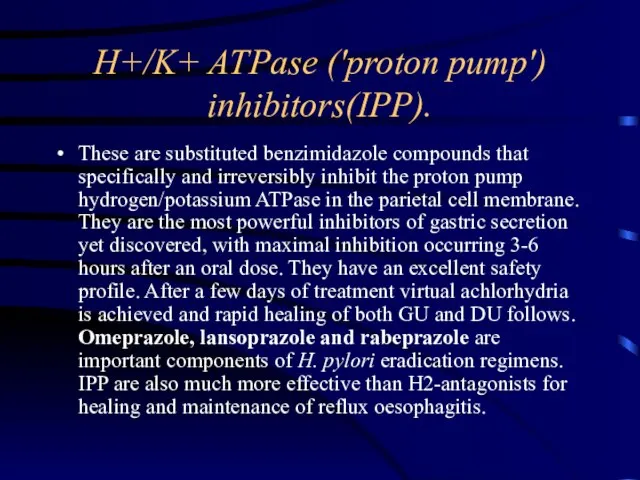
- 46. H+/K+ ATPase ('proton pump') inhibitors(IPP). These are substituted benzimidazole compounds that specifically and irreversibly inhibit the
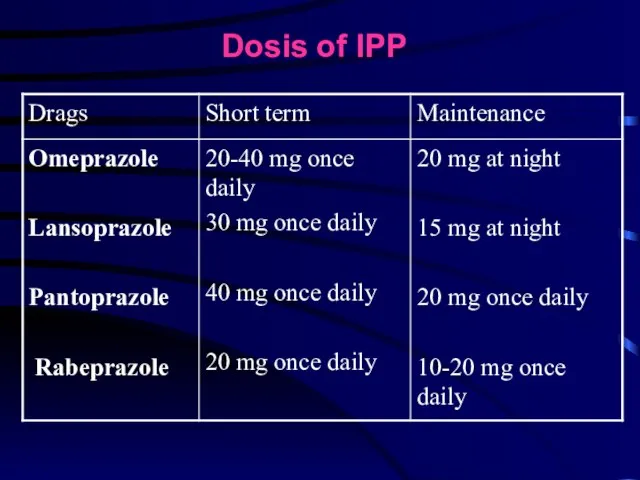
- 47. Dosis of IPP
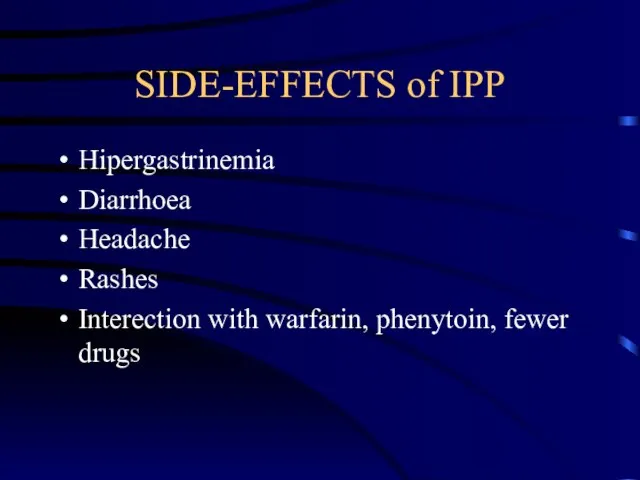
- 48. SIDE-EFFECTS of IPP Hipergastrinemia Diarrhoea Headache Rashes Interection with warfarin, phenytoin, fewer drugs
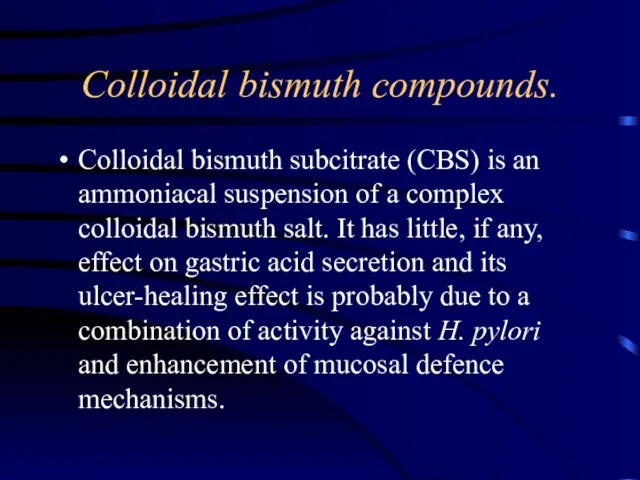
- 49. Colloidal bismuth compounds. Colloidal bismuth subcitrate (CBS) is an ammoniacal suspension of a complex colloidal bismuth
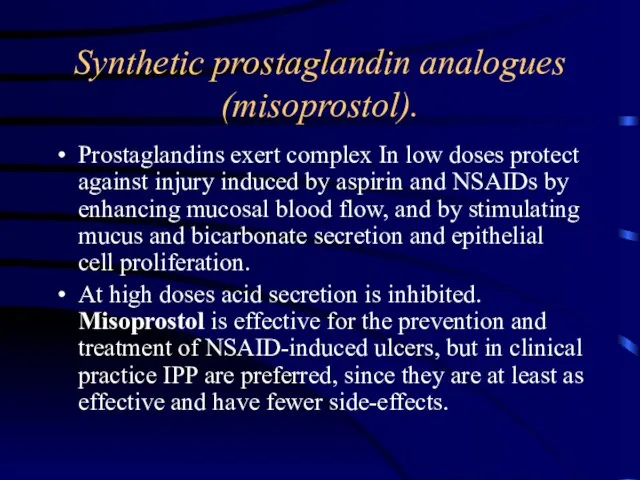
- 50. Synthetic prostaglandin analogues (misoprostol). Prostaglandins exert complex In low doses protect against injury induced by aspirin
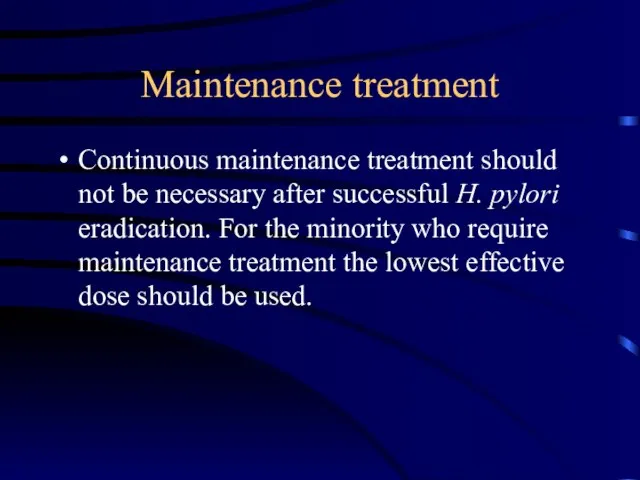
- 51. Maintenance treatment Continuous maintenance treatment should not be necessary after successful H. pylori eradication. For the
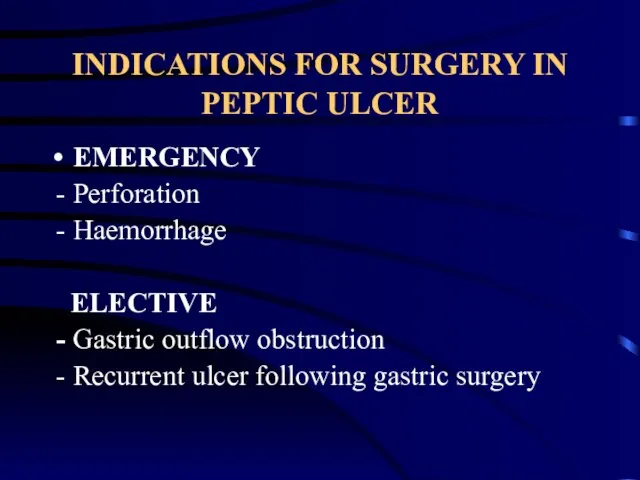
- 52. INDICATIONS FOR SURGERY IN PEPTIC ULCER EMERGENCY - Perforation - Haemorrhage ELECTIVE - Gastric outflow obstruction
- 54. Скачать презентацию
 Инфраструктурные инвестиции
Инфраструктурные инвестиции Културен туризъм: международен маркетинг Бележки към кръглата маса организирана от ПП ГЕРБ Асеновград, 23.06.09
Културен туризъм: международен маркетинг Бележки към кръглата маса организирана от ПП ГЕРБ Асеновград, 23.06.09 Pos материалы гербион
Pos материалы гербион Презентация на тему Неофициальные символы России
Презентация на тему Неофициальные символы России CPA launches FOD
CPA launches FOD Методы и приборы разрушающего контроля, применяемые при обследовании
Методы и приборы разрушающего контроля, применяемые при обследовании ЖИЗНЬ И БЫТ В СРЕДНЕВЕКОВОМ ЗАМКЕ
ЖИЗНЬ И БЫТ В СРЕДНЕВЕКОВОМ ЗАМКЕ Презентация компании MOST Marketing«Франчайзинговый пакет: как разработать,чтобы привлечь франчайзи»
Презентация компании MOST Marketing«Франчайзинговый пакет: как разработать,чтобы привлечь франчайзи» Колористика при окрашивании волос. Тест
Колористика при окрашивании волос. Тест Предложение по летнему корпоративному отдыху на стадионе «Труд» (пос. «Старая Купавна»)
Предложение по летнему корпоративному отдыху на стадионе «Труд» (пос. «Старая Купавна»)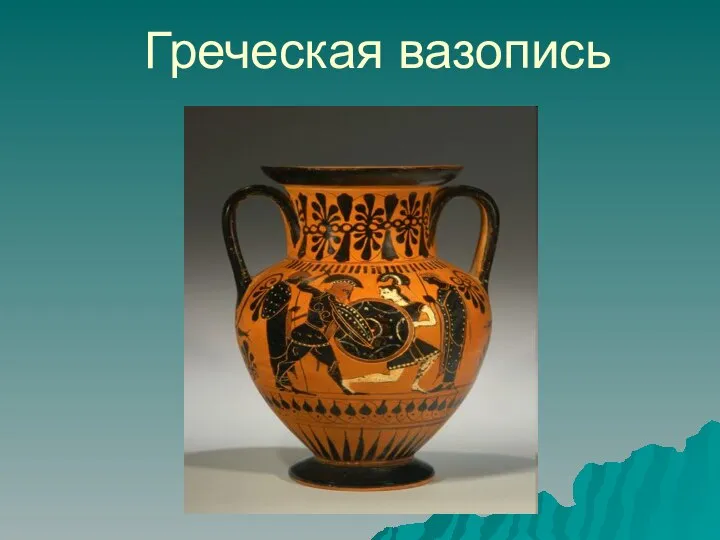 Греческая вазопись
Греческая вазопись Холод в нефтянной промышленности
Холод в нефтянной промышленности Урок-путешествие по разделу «Были-небылицы». Оценка достижений
Урок-путешествие по разделу «Были-небылицы». Оценка достижений LobbyWorks
LobbyWorks Самоиндукция
Самоиндукция Correct сommunication. Правильное общение
Correct сommunication. Правильное общение Тема: «Положение человека в системе животного мира. Эволюция гоминид».
Тема: «Положение человека в системе животного мира. Эволюция гоминид». Презентация на тему Выживание в природных условиях после аварии
Презентация на тему Выживание в природных условиях после аварии  ангелы
ангелы Интеллектуально-познавательная игра
Интеллектуально-познавательная игра Анализ применимости ПИК «СтОФ» для массовой оценки стоимости движимого имущества Тевелева Оксана Валерьевна тел: (499) 724-15-14, 8(903)208-
Анализ применимости ПИК «СтОФ» для массовой оценки стоимости движимого имущества Тевелева Оксана Валерьевна тел: (499) 724-15-14, 8(903)208- Fruit and vegetables
Fruit and vegetables Ты подвиг совершил во имя жизни на земле
Ты подвиг совершил во имя жизни на земле Обязательства из односторонних сделок и из действий в чужом интересе. Обязательства из договоров, не подлежащие судебной защите
Обязательства из односторонних сделок и из действий в чужом интересе. Обязательства из договоров, не подлежащие судебной защите ТВ - тюнеры
ТВ - тюнеры Применение программного комплекса CorPos (FORCE Technology Norway AS) для диагностики и прогнозирования коррозии на внутренних стенках газопров
Применение программного комплекса CorPos (FORCE Technology Norway AS) для диагностики и прогнозирования коррозии на внутренних стенках газопров Евгений Замятин
Евгений Замятин Characteristic of grain mass
Characteristic of grain mass