Содержание
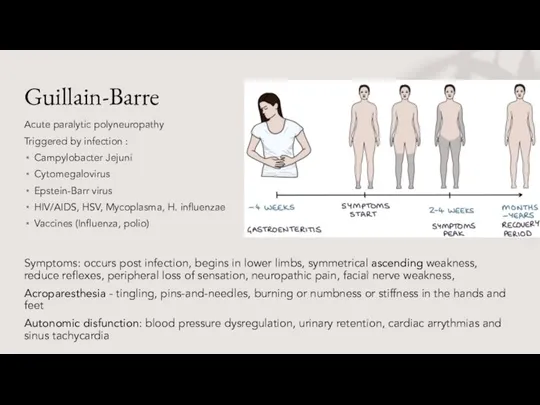
- 2. Guillain-Barre Acute paralytic polyneuropathy Triggered by infection : Campylobacter Jejuni Cytomegalovirus Epstein-Barr virus HIV/AIDS, HSV, Mycoplasma,
- 3. Guillain-Barre syndrome Diagnosis: Clinical The most accurate is Electromyography (EMG) and Nerve conduction test (reduced signal)
- 4. An 11-years-old boy is brought to your practice with progressive difficulty climbing stairs, walking, or running
- 5. A child was recently vaccinated for polio, now presents with 1-week history of fever, flaccid paralysis
- 6. Infection with wild poliomyelitis Initial symptoms are fever, fatigue, headache, vomiting, stiffness of the neck and
- 7. A 32-year-old woman suddenly develops abdominal pain and diarrhea. The abdominal pain is periumbilical and crampy,
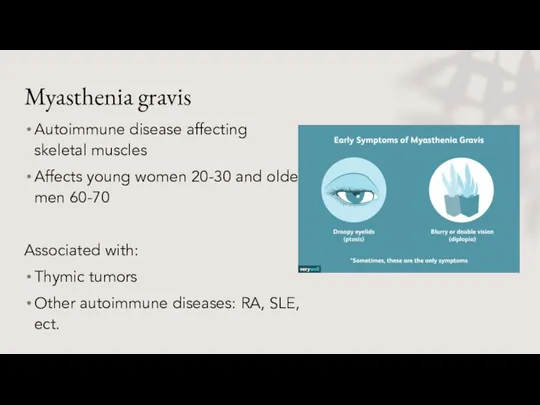
- 8. Myasthenia gravis Autoimmune disease affecting skeletal muscles Affects young women 20-30 and older men 60-70 Associated
- 9. Myasthenia gravis Symptoms: Weakness neck, face, arms Eyelid drooping “Ptosis” Appearance mask-like (very sleepy look) Keep
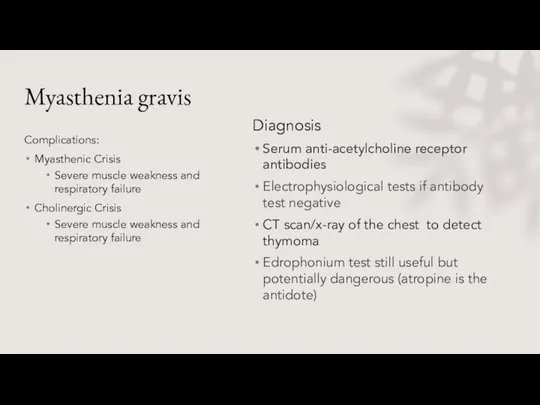
- 10. Myasthenia gravis Complications: Myasthenic Crisis Severe muscle weakness and respiratory failure Cholinergic Crisis Severe muscle weakness
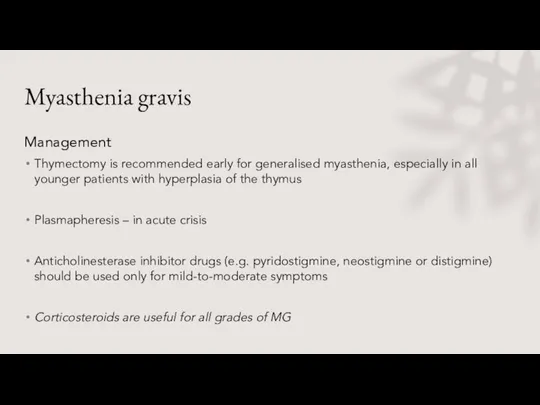
- 11. Myasthenia gravis Management Thymectomy is recommended early for generalised myasthenia, especially in all younger patients with
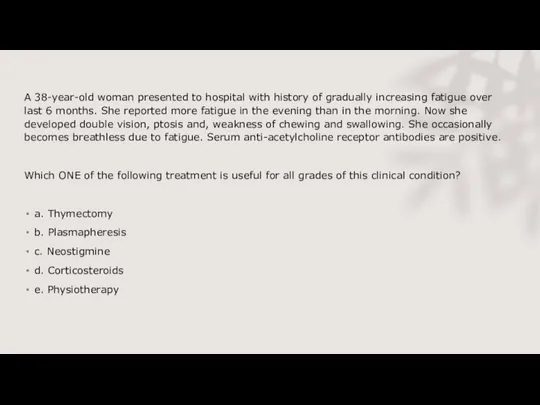
- 12. A 38-year-old woman presented to hospital with history of gradually increasing fatigue over last 6 months.
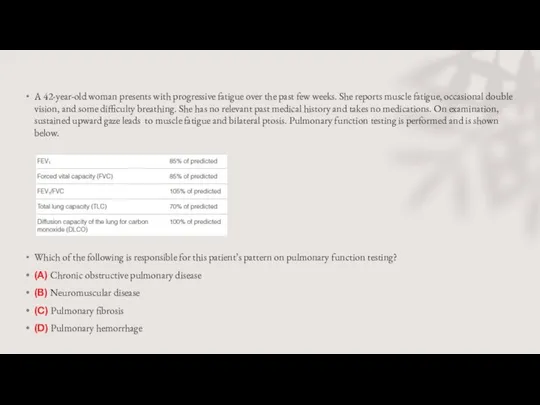
- 13. A 42-year-old woman presents with progressive fatigue over the past few weeks. She reports muscle fatigue,
- 14. Neuromuscular disease. Myasthenia gravis is a neuromuscular disease caused by autoantibodies directed against postsynaptic acetylcholine receptors.
- 15. A 75 year old lady is admitted in an acute confusional state secondary to a urinary
- 16. Which ONE of the following condition causes ptosis and dilated pupil? a. Myasthenia gravis b. Mitochondrial
- 18. Скачать презентацию
 Чума. 8 класс
Чума. 8 класс Топическая диагностика поражений нервной системы
Топическая диагностика поражений нервной системы Нарушение кровообращения
Нарушение кровообращения Кровотечение. Классификация по локализации излившейся крови, по характеру поврежденных сосудов, по скорости истечения
Кровотечение. Классификация по локализации излившейся крови, по характеру поврежденных сосудов, по скорости истечения Артериальды гипертензиясы бар инфаркт миокардты басынан өткерген науқастарда комплексті емнің эффективтілігін бағалау
Артериальды гипертензиясы бар инфаркт миокардты басынан өткерген науқастарда комплексті емнің эффективтілігін бағалау Блокада плечевого сплетения
Блокада плечевого сплетения Кардиоверсия при ФП - электрическая или фармакологическая
Кардиоверсия при ФП - электрическая или фармакологическая Резиденттің өзіндік жұмысы
Резиденттің өзіндік жұмысы Вульвовагенит. Симптомы
Вульвовагенит. Симптомы Физические основы работы рентгеновских установок
Физические основы работы рентгеновских установок Полисемия клинических терминоэлементов
Полисемия клинических терминоэлементов xGenCloud - облачный сервис для автоматической интерпретации результатов генетических анализов и формирования заключения
xGenCloud - облачный сервис для автоматической интерпретации результатов генетических анализов и формирования заключения Пищевые отравления
Пищевые отравления Врождённые наследственные заболевания
Врождённые наследственные заболевания General principles of anaesthesiology
General principles of anaesthesiology Оценка состояния сознание при воспалении челюстно-лицевой области
Оценка состояния сознание при воспалении челюстно-лицевой области Ларингит – воспалительное заболевание слизистой оболочки гортани
Ларингит – воспалительное заболевание слизистой оболочки гортани Система учета донорских органов и тканей человека, доноров органов и тканей человека, пациентов (реципиентов) в РФ
Система учета донорских органов и тканей человека, доноров органов и тканей человека, пациентов (реципиентов) в РФ 의약품의 복용법
의약품의 복용법 Сыпи у детей (1)
Сыпи у детей (1) Лекарственные растения и травы в ветеринарии
Лекарственные растения и травы в ветеринарии Телемедецина. Предрейсовый, предсменный медосмотр сотрудников в любом месте и в любое время
Телемедецина. Предрейсовый, предсменный медосмотр сотрудников в любом месте и в любое время Шымкент қаласының мектеп жасына дейінгі балаларының сілекейіндегі, липидтердің, асқын тотық өнімдерінің, ауыз қуысының
Шымкент қаласының мектеп жасына дейінгі балаларының сілекейіндегі, липидтердің, асқын тотық өнімдерінің, ауыз қуысының Секреты долголетия
Секреты долголетия Здоровье дошкольника
Здоровье дошкольника Образец. Физическая реабилитация женщин 40-45 лет при остеохондрозе шейно - грудного отдела позвоночника
Образец. Физическая реабилитация женщин 40-45 лет при остеохондрозе шейно - грудного отдела позвоночника Опухоль Клатскина
Опухоль Клатскина _ _Правила проведения непрямого массажа сердца. Искусственная вентиляция легких. Правила сердечно-легочной реанимации_
_ _Правила проведения непрямого массажа сердца. Искусственная вентиляция легких. Правила сердечно-легочной реанимации_