Содержание
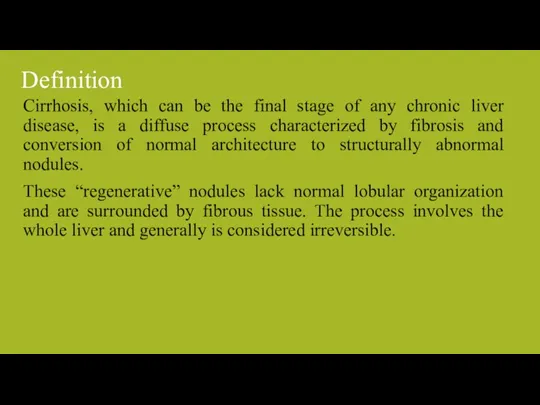
- 2. Definition Cirrhosis, which can be the final stage of any chronic liver disease, is a diffuse
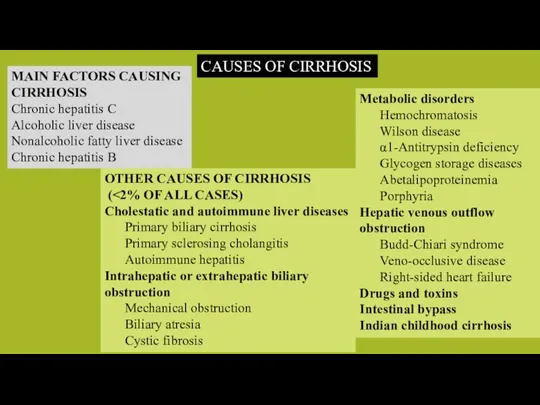
- 3. MAIN FACTORS CAUSING CIRRHOSIS Chronic hepatitis C Alcoholic liver disease Nonalcoholic fatty liver disease Chronic hepatitis
- 4. PATHOBIOLOGY & PATHOGENESIS Liver Fibrosis and Cirrhosis
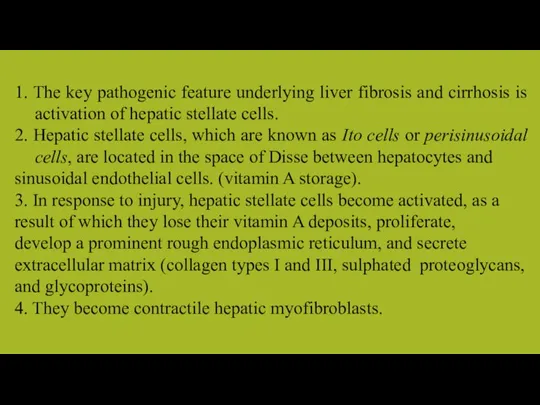
- 5. 1. The key pathogenic feature underlying liver fibrosis and cirrhosis is activation of hepatic stellate cells.
- 6. 5. Liver cells undergo necrosis, the hepatic lobules collapse and this leads to the formation of
- 7. 10. The liver surface becomes nodular. 11. Hepatic vascular bed is distorted, truncated and obstructed, the
- 8. 12. Obstruction to portal venous flow results in the development of portal hypertension. 13. As the
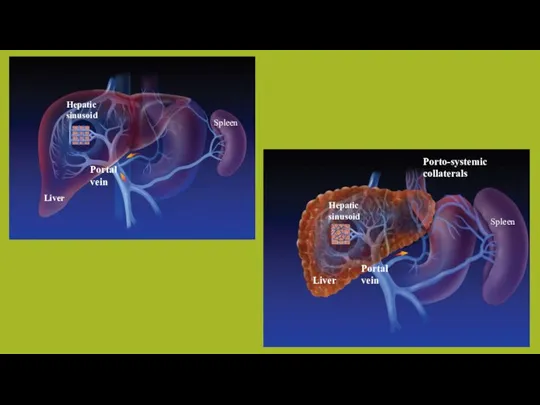
- 9. Hepatic sinusoid Hepatic sinusoid Spleen Spleen Liver Liver Portal vein Portal vein Porto-systemic collaterals
- 10. Morphological Classification The morphological types are: a. micronodular, b. macronodular, and c. mixed.
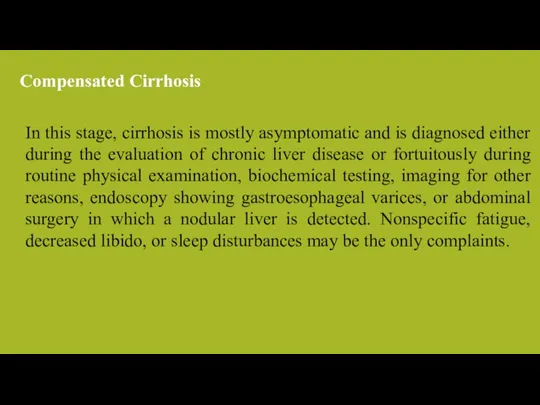
- 11. In this stage, cirrhosis is mostly asymptomatic and is diagnosed either during the evaluation of chronic
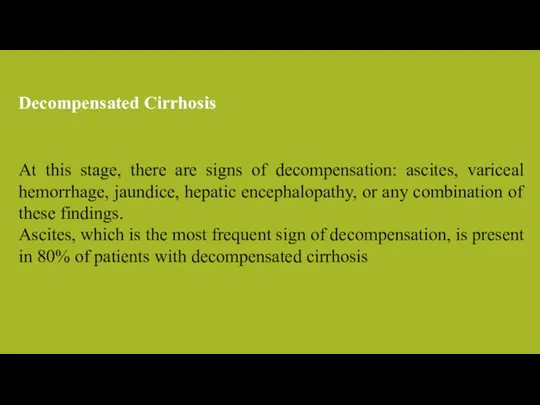
- 12. At this stage, there are signs of decompensation: ascites, variceal hemorrhage, jaundice, hepatic encephalopathy, or any
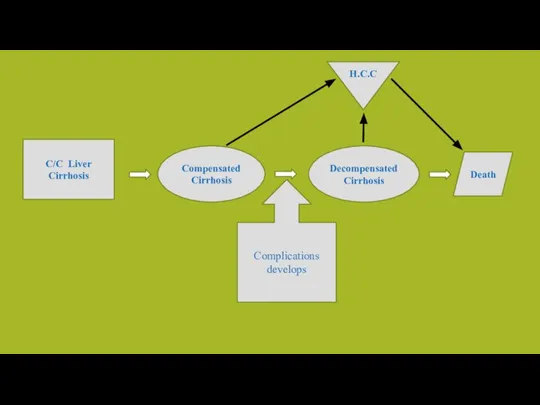
- 13. C/C Liver Cirrhosis Compensated Cirrhosis Decompensated Cirrhosis Death Complications develops H.C.C
- 14. Early stages of the disease are asymptomatic. Vague illhealth, anorexia, loss of weight, loss of libido,
- 15. In the compensated phase, liver synthetic function is mostly normal, and portal pressure, although increased, is
- 16. Variceal Hemorrhage Ascites and Hyponatremia Spontaneous Bacterial Peritonitis Hepatic Encephalopathy Pulmonary Complications Complications
- 18. Скачать презентацию

 Состояние здоровья сельских женщин и их детей
Состояние здоровья сельских женщин и их детей Терапия сопровождения и паллиативная помощь
Терапия сопровождения и паллиативная помощь Крон ауруы
Крон ауруы АІЖ ауруларындағы неврологиялық синдромдар
АІЖ ауруларындағы неврологиялық синдромдар Психопатология памяти (2 часа) (Лекция 4)
Психопатология памяти (2 часа) (Лекция 4) Острые кишечные инфекции у детей
Острые кишечные инфекции у детей Ультразвук в природе и технике
Ультразвук в природе и технике Общемозговые структурно-функциональные объединения стволовых отделов
Общемозговые структурно-функциональные объединения стволовых отделов Санитарный контроль предприятий общественного питания
Санитарный контроль предприятий общественного питания Беседа о гипер и гипогликемических состояниях
Беседа о гипер и гипогликемических состояниях Виды ран и общие правила оказания первой медицинской помощи
Виды ран и общие правила оказания первой медицинской помощи Разработка состава и технологии получения лекарственной формы на основе ЛРС для лечения судорог
Разработка состава и технологии получения лекарственной формы на основе ЛРС для лечения судорог Модуляция аутофагии как мультицелевой подход к терапии нейродегенеративных нарушений болезни Альцгеймера
Модуляция аутофагии как мультицелевой подход к терапии нейродегенеративных нарушений болезни Альцгеймера Всероссийская акция #стопвичспид
Всероссийская акция #стопвичспид Современные вопросы ведения черепно-мозговой травмы
Современные вопросы ведения черепно-мозговой травмы Остеопороз. Подагра
Остеопороз. Подагра ОЗОН – эффективное средство повышения иммунитета!
ОЗОН – эффективное средство повышения иммунитета! Антибиотики. Препарат моксиграм
Антибиотики. Препарат моксиграм Межклеточные взаимодействия через белки суперсемейства иммуноглобулинов
Межклеточные взаимодействия через белки суперсемейства иммуноглобулинов Расту здоровым, сильным, закалённым
Расту здоровым, сильным, закалённым Лазеротерапия
Лазеротерапия ДЦП. Спастическая диплегия
ДЦП. Спастическая диплегия ВРТ / ИКСИ в позднем репродуктивном возрасте
ВРТ / ИКСИ в позднем репродуктивном возрасте XI всероссийская научная конференция студентов и аспирантов Молодая фармация – потенциал будущего
XI всероссийская научная конференция студентов и аспирантов Молодая фармация – потенциал будущего Эвтаназия. Философ Фрэнсис Бэкон
Эвтаназия. Философ Фрэнсис Бэкон Моделирование мигрени на животных
Моделирование мигрени на животных Современные принципы организации акушерско-гинекологической помощи
Современные принципы организации акушерско-гинекологической помощи Основы здорового образа жизни
Основы здорового образа жизни