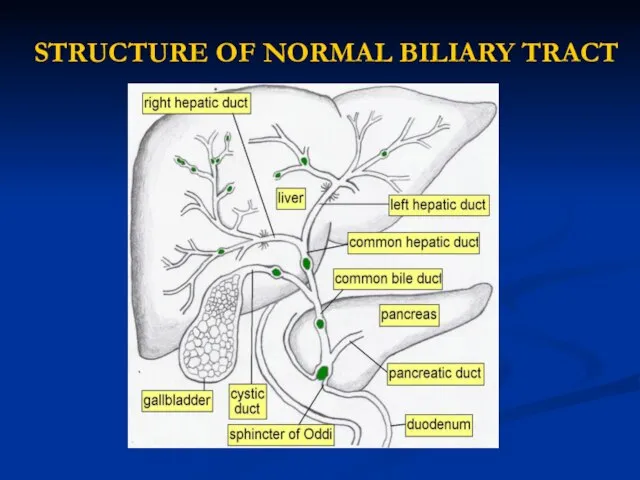
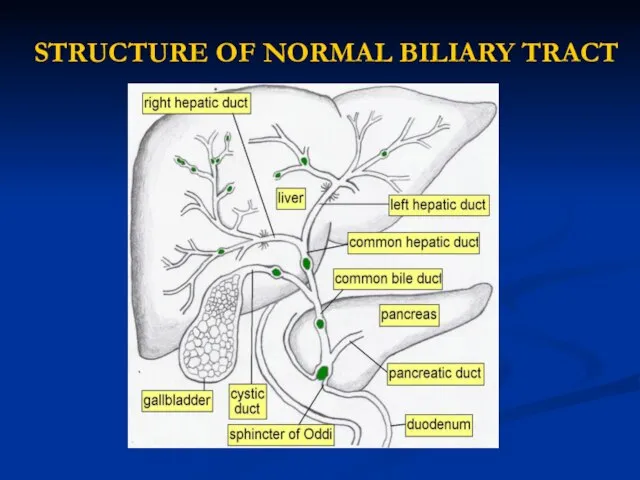
Слайд 2STRUCTURE OF NORMAL BILIARY TRACT
Слайд 3LIST OF DISEASES OF THE GALLBLADDER
CONGENITAL ANOMALIES
GALLSTONES
ACUTE CHOLECYSTITIS
ACALCULOUS CHOLECYSTITIS
EMPHYSEMATOUS CHOLECYSTITIS
CHRONIC CHOLECYSTITIS
GALLBLADDER CANCER
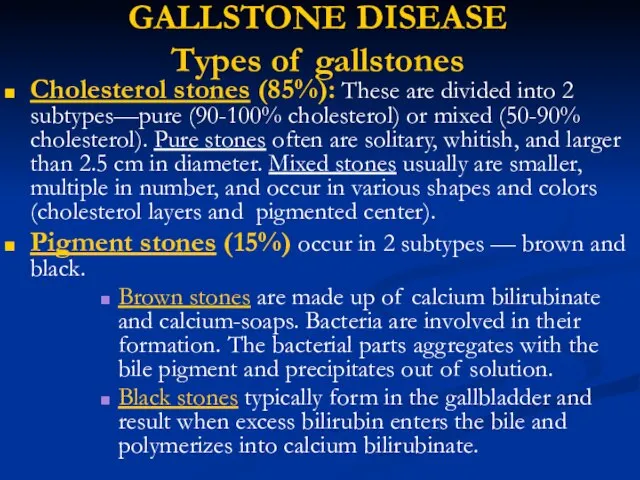
Слайд 4GALLSTONE DISEASE
Types of gallstones
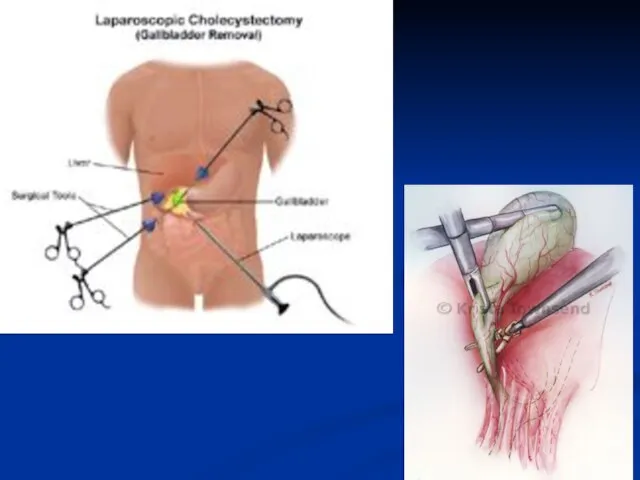
Cholesterol stones (85%): These are divided into 2
subtypes—pure (90-100% cholesterol) or mixed (50-90% cholesterol). Pure stones often are solitary, whitish, and larger than 2.5 cm in diameter. Mixed stones usually are smaller, multiple in number, and occur in various shapes and colors (cholesterol layers and pigmented center).
Pigment stones (15%) occur in 2 subtypes — brown and black.
Brown stones are made up of calcium bilirubinate and calcium-soaps. Bacteria are involved in their formation. The bacterial parts aggregates with the bile pigment and precipitates out of solution.
Black stones typically form in the gallbladder and result when excess bilirubin enters the bile and polymerizes into calcium bilirubinate.
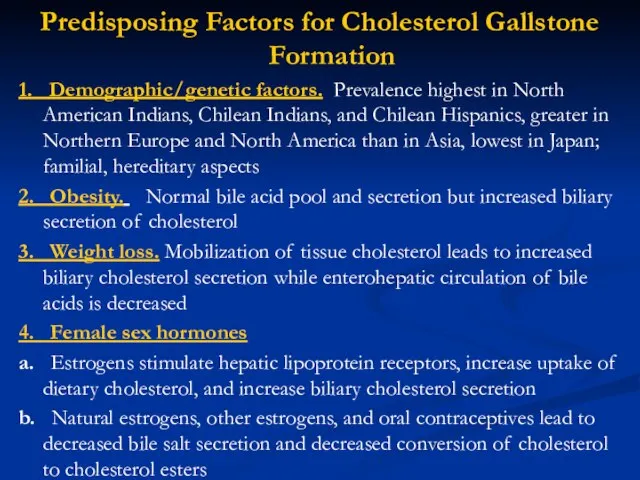
Слайд 5Predisposing Factors for Cholesterol Gallstone Formation
1. Demographic/genetic factors. Prevalence highest in North American
Indians, Chilean Indians, and Chilean Hispanics, greater in Northern Europe and North America than in Asia, lowest in Japan; familial, hereditary aspects
2. Obesity. Normal bile acid pool and secretion but increased biliary secretion of cholesterol
3. Weight loss. Mobilization of tissue cholesterol leads to increased biliary cholesterol secretion while enterohepatic circulation of bile acids is decreased
4. Female sex hormones
a. Estrogens stimulate hepatic lipoprotein receptors, increase uptake of dietary cholesterol, and increase biliary cholesterol secretion
b. Natural estrogens, other estrogens, and oral contraceptives lead to decreased bile salt secretion and decreased conversion of cholesterol to cholesterol esters
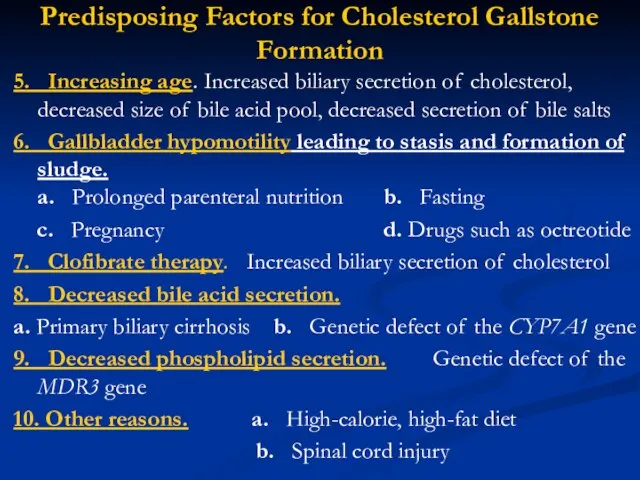
Слайд 6Predisposing Factors for Cholesterol Gallstone Formation
5. Increasing age. Increased biliary secretion of cholesterol,
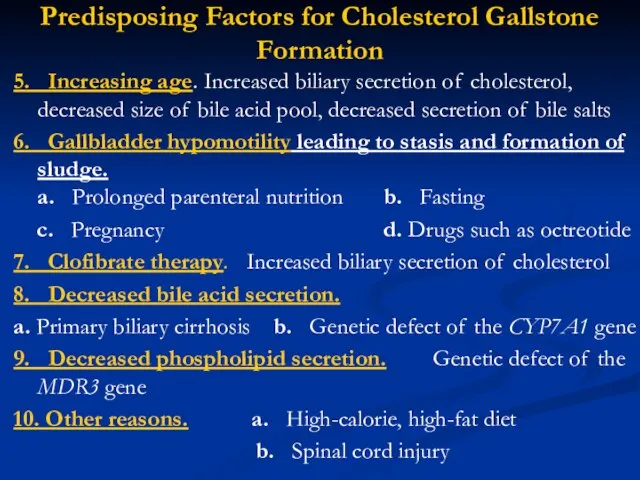
decreased size of bile acid pool, decreased secretion of bile salts
6. Gallbladder hypomotility leading to stasis and formation of sludge. a. Prolonged parenteral nutrition b. Fasting
c. Pregnancy d. Drugs such as octreotide
7. Clofibrate therapy. Increased biliary secretion of cholesterol
8. Decreased bile acid secretion.
a. Primary biliary cirrhosis b. Genetic defect of the CYP7A1 gene
9. Decreased phospholipid secretion. Genetic defect of the MDR3 gene
10. Other reasons. a. High-calorie, high-fat diet
b. Spinal cord injury
Слайд 7 Predisposing Factors for Pigment Gallstone Formation
1. Demographic/genetic factors: Asia, rural setting
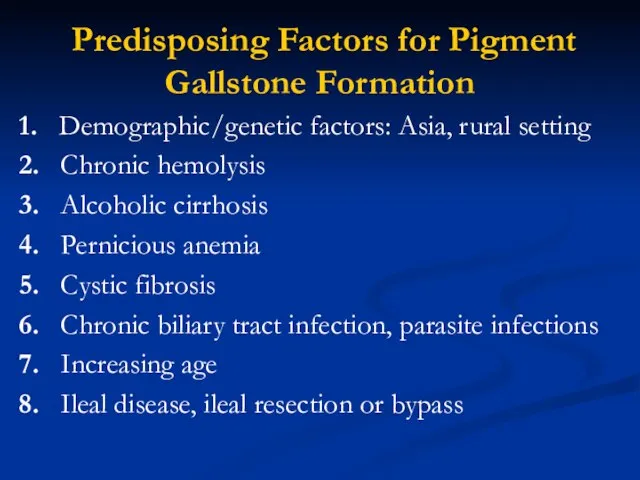
2. Chronic hemolysis
3. Alcoholic cirrhosis
4. Pernicious anemia
5. Cystic fibrosis
6. Chronic biliary tract infection, parasite infections
7. Increasing age
8. Ileal disease, ileal resection or bypass
Слайд 8STAGES OF STONE FORMATION
Cholesterol supersaturation in bile. Cholesterol is held in solution
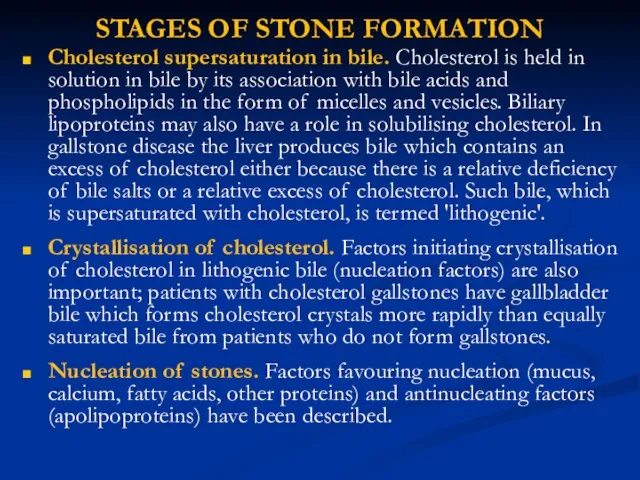
in bile by its association with bile acids and phospholipids in the form of micelles and vesicles. Biliary lipoproteins may also have a role in solubilising cholesterol. In gallstone disease the liver produces bile which contains an excess of cholesterol either because there is a relative deficiency of bile salts or a relative excess of cholesterol. Such bile, which is supersaturated with cholesterol, is termed 'lithogenic'.
Crystallisation of cholesterol. Factors initiating crystallisation of cholesterol in lithogenic bile (nucleation factors) are also important; patients with cholesterol gallstones have gallbladder bile which forms cholesterol crystals more rapidly than equally saturated bile from patients who do not form gallstones.
Nucleation of stones. Factors favouring nucleation (mucus, calcium, fatty acids, other proteins) and antinucleating factors (apolipoproteins) have been described.
Слайд 9Symptoms of Gallstone Disease
Gallstones usually produce symptoms by causing inflammation or obstruction
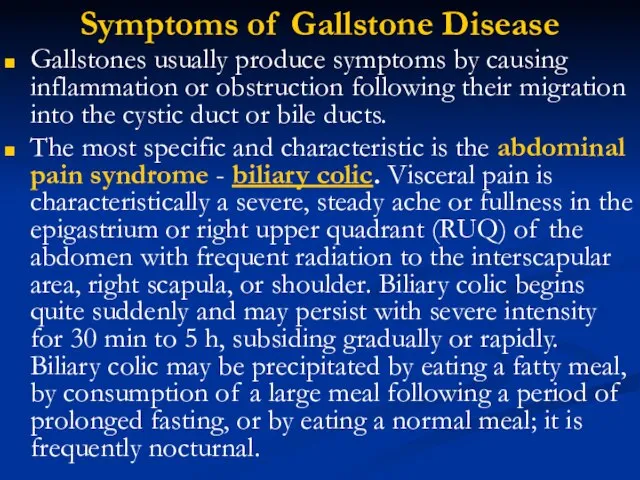
following their migration into the cystic duct or bile ducts.
The most specific and characteristic is the abdominal pain syndrome - biliary colic. Visceral pain is characteristically a severe, steady ache or fullness in the epigastrium or right upper quadrant (RUQ) of the abdomen with frequent radiation to the interscapular area, right scapula, or shoulder. Biliary colic begins quite suddenly and may persist with severe intensity for 30 min to 5 h, subsiding gradually or rapidly. Biliary colic may be precipitated by eating a fatty meal, by consumption of a large meal following a period of prolonged fasting, or by eating a normal meal; it is frequently nocturnal.
Слайд 10Symptoms of Gallstone Disease
Dyspeptic syndrome (Nausea and vomiting) frequently accompany episodes of
biliary pain.
General intoxication (Fever or chills) (rigors) with biliary pain usually imply a complication, i.e., cholecystitis, pancreatitis, or cholangitis.
Complaints of vague epigastric fullness, dyspepsia, eructation, or flatulence, especially following a fatty meal, should not be confused with biliary pain. Such symptoms are not specific for biliary calculi.
Слайд 11 EXAMINATION
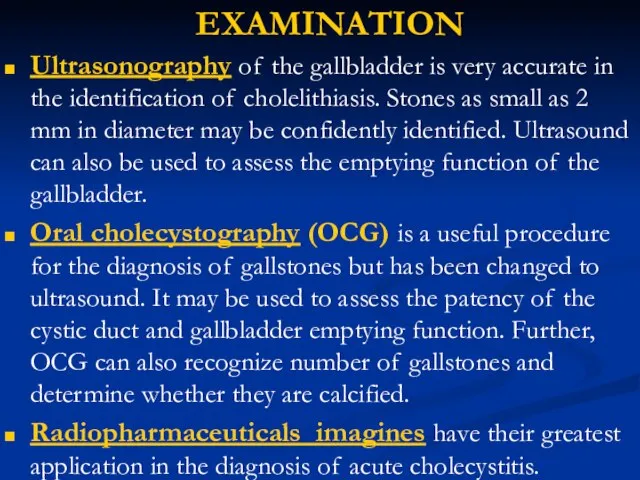
Ultrasonography of the gallbladder is very accurate in the identification of
cholelithiasis. Stones as small as 2 mm in diameter may be confidently identified. Ultrasound can also be used to assess the emptying function of the gallbladder.
Oral cholecystography (OCG) is a useful procedure for the diagnosis of gallstones but has been changed to ultrasound. It may be used to assess the patency of the cystic duct and gallbladder emptying function. Further, OCG can also recognize number of gallstones and determine whether they are calcified.
Radiopharmaceuticals imagines have their greatest application in the diagnosis of acute cholecystitis.
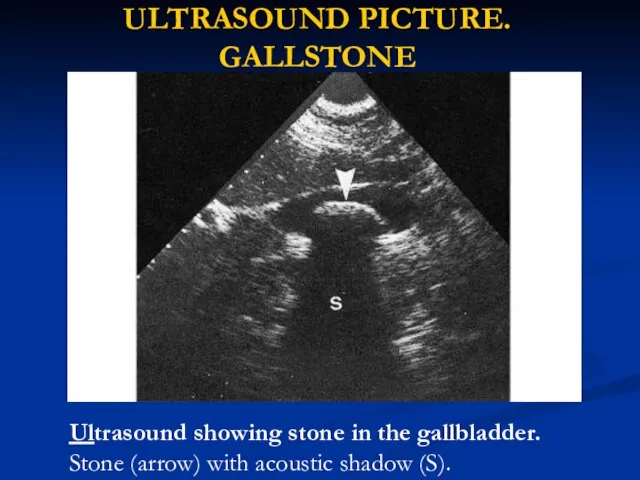
Слайд 12ULTRASOUND PICTURE. GALLSTONE
Ultrasound showing stone in the gallbladder. Stone (arrow) with acoustic
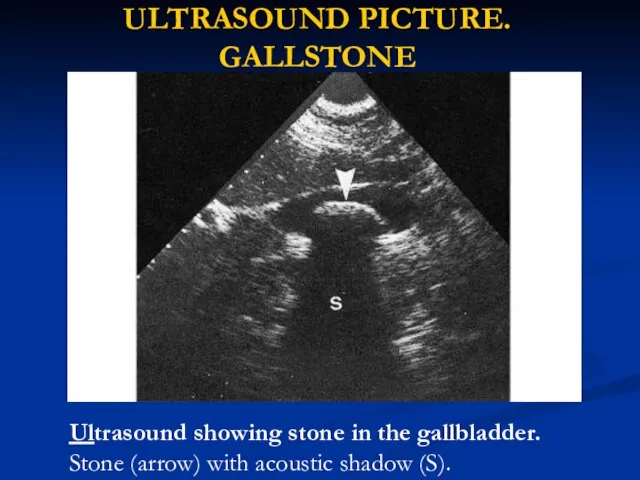
shadow (S).
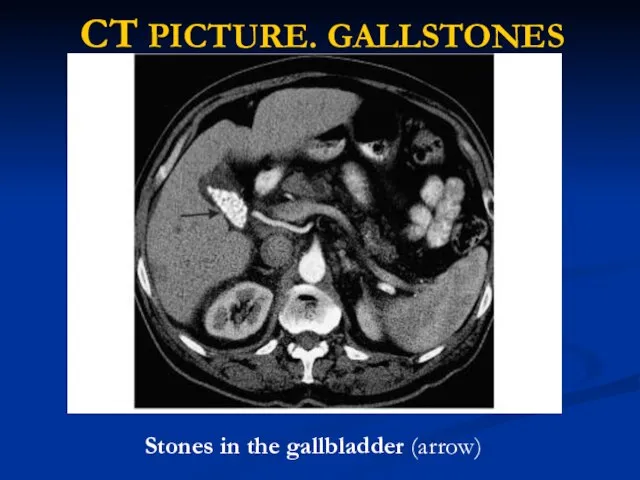
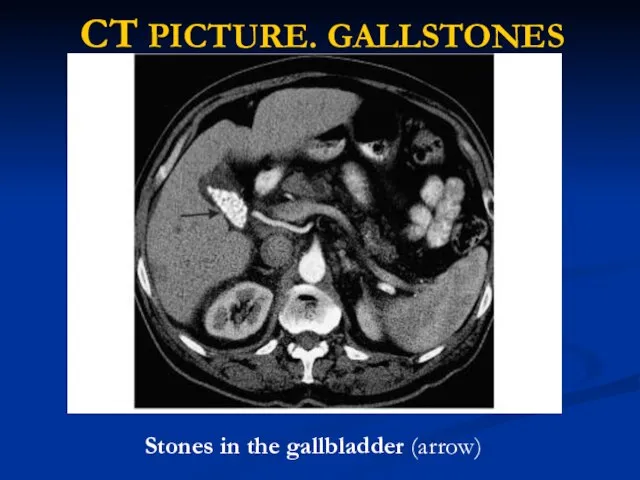
Слайд 14CT PICTURE. GALLSTONES
Stones in the gallbladder (arrow)
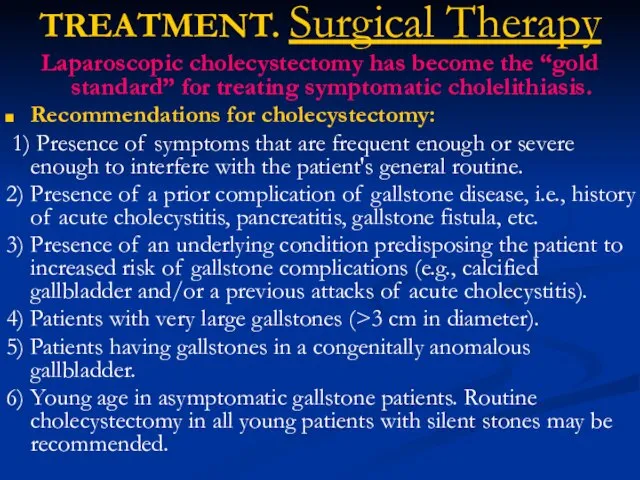
Слайд 15TREATMENT. Surgical Therapy
Laparoscopic cholecystectomy has become the “gold standard” for treating symptomatic
cholelithiasis.
Recommendations for cholecystectomy:
1) Presence of symptoms that are frequent enough or severe enough to interfere with the patient's general routine.
2) Presence of a prior complication of gallstone disease, i.e., history of acute cholecystitis, pancreatitis, gallstone fistula, etc.
3) Presence of an underlying condition predisposing the patient to increased risk of gallstone complications (e.g., calcified gallbladder and/or a previous attacks of acute cholecystitis).
4) Patients with very large gallstones (>3 cm in diameter).
5) Patients having gallstones in a congenitally anomalous gallbladder.
6) Young age in asymptomatic gallstone patients. Routine cholecystectomy in all young patients with silent stones may be recommended.
Слайд 18TREATMENT
Medical Therapy—Gallstone Dissolution
UDCA (Actigall, URSO 250, URSO, Ursofalk, ursodeoxycholic acid) decreases cholesterol
saturation of bile and also help to dispersion of cholesterol from stones. UDCA may also retard cholesterol crystal nucleation. In carefully selected patients with a functioning gallbladder and with stones <10 mm in diameter, complete dissolution can be achieved in about 50% of patients within 6 months to 2 years with UDCA at a dose of 8 to 10 mg/kg per day. The highest success rate (i.e., >70%) occurs in patients with small (<5 mm) floating radiolucent gallstones.
Extracorporeal shock waves. While such shock wave lithotripsy combined with medical litholytic therapy is safe and effective in carefully selected patients with gallbladder calculi (radiolucent, solitary stone <2 cm in well-contracting gallbladder).
Слайд 19Medical Therapy—Gallstone Dissolution

Слайд 20ACUTE CHOLECYSTITIS
ETHIOLOGY
Acute inflammation of the gallbladder wall usually follows obstruction of
the cystic duct by a stone.
Inflammatory response can be evoked by 3 factors:
(1) mechanical inflammation produced by increased intraluminal pressure and distention with resulting ischemia of the gallbladder mucosa and wall,
(2) chemical inflammation caused by the release of lysolecithin (due to the action of phospholipase on lecithin in bile) and other local tissue factors,
(3) bacterial inflammation, which may play a role in 50 to 85% of patients with acute cholecystitis. The organisms most frequently isolated by culture of gallbladder bile include Escherichia coli, Klebsiella spp., Streptococcus spp., and Clostridium spp.
Слайд 21ACUTE CHOLECYSTITIS. SYMPTOMS AND SIGHNS
Acute cholecystitis often begins as an attack
of biliary pain (abdominal pain syndrome) that progressively worsens. Approximately 60 to 70% of patients report having experienced prior attacks that resolved spontaneously. As the episode progresses, however, the pain of acute cholecystitis becomes more generalized in the right upper abdomen. The pain may radiate to the interscapular area, right scapula, or shoulder.
Peritoneal signs of inflammation such as increased pain with jarring or on deep respiration may be apparent.
Dyspeptic syndrome - the patient is anorectic and often nauseated. Vomiting is relatively common and may produce symptoms and signs of vascular and extracellular volume depletion.
Слайд 22ACUTE CHOLECYSTITIS. SYMPTOMS AND SIGHNS
Jaundice is unusual early in the course of
acute cholecystitis but may occur when edematous inflammatory changes involve the bile ducts and surrounding lymph nodes.
A low-grade fever is characteristically present, but shaking chills or rigors are not uncommon.
The right upper quadrant of the abdomen is almost invariably tender to palpation (Kerr’s sign).
An enlarged, tense gallbladder is palpable in one-quarter to one-half of patients.
Deep inspiration or cough during subcostal palpation of the RUQ usually produces increased pain and inspiratory arrest (Murphy's sign).
A light thump delivered to the right subcostal area may markedly increase the pain (Orthner’s sign).
Localized rebound tenderness in the RUQ is common, as a abdominal distention and hypoactive bowel sounds from paralytic ileus, but without generalized peritoneal signs and abdominal rigidity, in the absence of perforation.
Слайд 23ACUTE CHOLECYSTITIS. Diagnosis
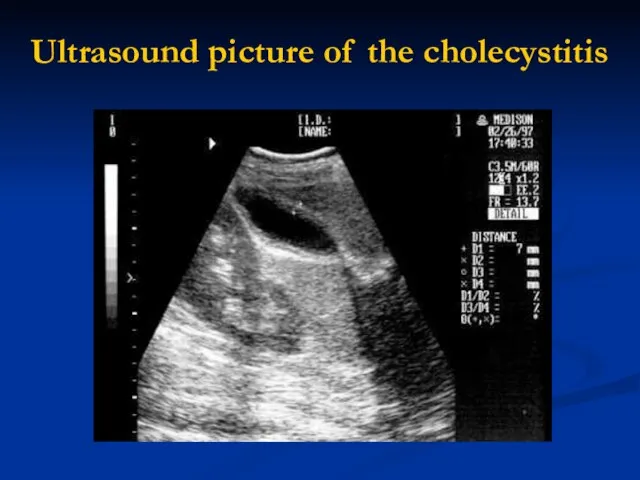
The diagnosis of acute cholecystitis is usually made on the
basis of a characteristic history and physical examination.
The triad of sudden onset of RUQ tenderness, fever, and leukocytosis is highly suggestive.
The serum bilirubin is mildly elevated [<85.5 µmol/L (5 mg/dL)] in half of patients.
About one-fourth have modest elevations in serum aminotransferases (usually less than a fivefold elevation).
The radionuclide (e.g., HIDA) biliary scan may be confirmatory if bile duct imaging is seen without visualization of the gallbladder.
Ultrasound demonstrates calculi in 90 - 95% of cases.
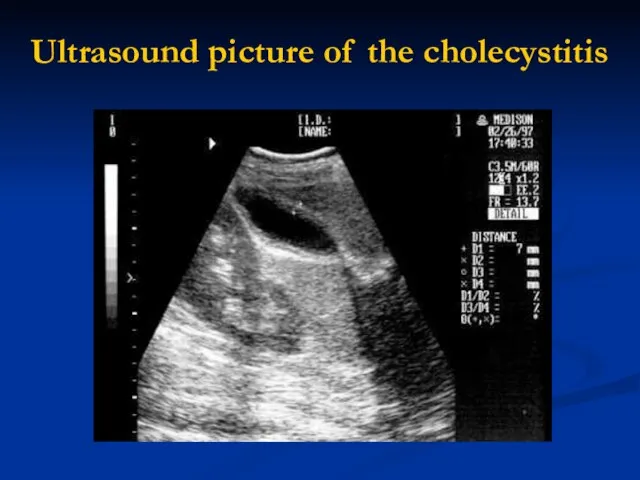
Слайд 24Ultrasound picture of the cholecystitis
Слайд 25ACUTE CHOLECYSTITIS. Outcomes.
Approximately 75% of patients treated medically have remission of acute
symptoms within 2 to 7 days following hospitalization.
In 25%, however, a complication of acute cholecystitis will occur despite conservative. In this setting, prompt surgical intervention is required.
Of the 75% of patients with acute cholecystitis who undergo remission of symptoms, approximately one-quarter will experience a recurrence of cholecystitis within 1 year, and 60% will have at least one recurrence within 6 years.
In view of the natural history of the disease, acute cholecystitis is best treated by early surgery whenever possible.
Слайд 26ACALCULOUS CHOLECYSTITIS
ETHIOLOGY. In 5 to 10% of patients with acute cholecystitis, calculi
obstructing the cystic duct are not found.
An increased risk is especially associated with serious trauma or burns, the postpartum period following prolonged labor, and with orthopedic and other nonbiliary major surgical operations in the postoperative period.
It may possibly complicate periods of prolonged parenteral hyperalimentation. For some of these cases, biliary sludge in the cystic duct may be responsible.
Other precipitating factors include vasculitis, obstructing adenocarcinoma of the gallbladder, diabetes mellitus, torsion of the gallbladder, “unusual” bacterial infections of the gallbladder (e.g., Leptospira, Streptococcus, Salmonella, or Vibrio cholerae), and parasitic infestation of the gallbladder.
Acalculous cholecystitis may also be seen with a variety of other systemic disease processes (sarcoidosis, cardiovascular disease, tuberculosis, syphilis, actinomycosis, etc.).
Слайд 27ACALCULOUS CHOLECYSTITIS
CLINICAL PICTURE. The clinical manifestations of acalculous cholecystitis are the same
as calculous cholecystitis, with the symptoms of underlying illness.
DIAGNOSIS. Ultrasound, computed tomography (CT) scanning, or radionuclide examinations demonstrating a large, tense, static gallbladder without stones and with evidence of poor emptying over a prolonged period may be diagnostically useful.
The COMPLICATION rate for acalculous cholecystitis exceeds that for calculous cholecystitis.
Successful MANAGEMENT of acute acalculous cholecystitis bases on early diagnosis and surgical intervention, with special attention to postoperative care.
Слайд 28CHRONIC CHOLECYSTITIS
ETHIOLOGY, CLINICAL PICTURE
Chronic inflammation of the gallbladder wall is almost always
associated with the presence of gallstones and is thought to result from repeated occurring of subacute or acute cholecystitis or from persistent mechanical irritation of the gallbladder wall by gallstones.
The presence of bacteria in the bile occurs in more than one-quarter of patients with chronic cholecystitis.
Chronic cholecystitis may be asymptomatic for years, may progress to symptomatic gallbladder disease or to acute cholecystitis, or may present with complications.
Слайд 29CHRONIC CHOLECYSTITIS. Complications
EMPYEMA of the gallbladder usually results from progression of acute
cholecystitis with persistent cystic duct obstruction to superinfection of the stagnant bile with a pus-forming bacterial organism.
The clinical picture resembles that of cholangitis with high fever, severe RUQ pain, marked leukocytosis, and often, prostration. Empyema of the gallbladder carries a high risk of gram-negative sepsis and/or perforation.
Management. Emergency surgical intervention with proper antibiotic coverage is required as soon as the diagnosis is suspected.
Слайд 30CHRONIC CHOLECYSTITIS. Complications
HYDROPS or MUCOCELE of the gallbladder may also result from
prolonged obstruction of the cystic duct, usually by a large solitary calculus. In this instance, the obstructed gallbladder lumen is progressively distended, over a period of time, by mucus (mucocele) or by a clear transudate (hydrops) produced by mucosal epithelial cells.
Clinical picture. A visible, easily palpable, nontender mass sometimes extending from the RUQ into the right iliac fossa may be found on physical examination. The patient with hydrops of the gallbladder frequently remains asymptomatic, although chronic RUQ pain may also occur.
Management. Cholecystectomy is indicated, since empyema, perforation, or gangrene may complicate the condition.
Слайд 31CHRONIC CHOLECYSTITIS. Complications
GANGRENE of the gallbladder results from ischemia of the wall
and patchy or complete tissue necrosis. Underlying conditions often include marked distention of the gallbladder, vasculitis, diabetes mellitus, Empyema, or torsion resulting in arterial occlusion.
PERFORATION. Gangrene usually predisposes to perforation of the gallbladder, but perforation may also occur in chronic cholecystitis without premonitory warning symptoms. Localized perforations are usually contained by the omentum or by adhesions produced by recurrent inflammation of the gallbladder. Bacterial superinfection of the walled-off gallbladder contents results in abscess formation.
Most patients are best treated with cholecystectomy, but some seriously ill patients may be managed with cholecystostomy and drainage of the abscess.
Free perforation is less common but is associated with a mortality rate of approximately 30%.
Such patients may experience a sudden transient relief of RUQ pain as the distended gallbladder decompresses; this is followed by signs of generalized peritonitis.
FISTULA FORMATION AND GALLSTONE ILEUS
PANCREATITIS
Слайд 32CHRONIC CHOLECYSTITIS. MEDICAL TREATMENT
Although surgical intervention remains the mainstay of therapy for
acute cholecystitis and its complications, a period of in-hospital stabilization may be required before cholecystectomy.
Oral intake is eliminated, nasogastric suction may be indicated, and extracellular volume depletion and electrolyte abnormalities are repaired.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually employed for analgesia because they may produce less spasm of the sphincter of Oddi than drugs such as morphine.
Слайд 33CHRONIC CHOLECYSTITIS. MEDICAL TREATMENT
Intravenous antibiotic therapy is usually indicated in patients with
severe acute cholecystitis even though bacterial superinfection of bile may not have occurred in the early stages of the inflammatory process. Antibiotic therapy is guided by the most common organisms likely to be present, which are E. coli, Klebsiella spp., and Streptococcus spp. Effective antibiotics include ureidopenicillins such as piperacillin or mezlocillin, ampicillin sulbactam, and third-generation cephalosporins.
Anaerobic coverage by a drug such as metronidazole should be added if gangrenous or emphysematous cholecystitis is suspected.
Similarly, combination therapy with an aminoglycoside and other antibiotics may be considered in diabetic or debilitated patients and in those with signs of gram-negative sepsis. Postoperative complications of wound infection, abscess formation, or sepsis are reduced in antibiotic-treated patients.
Слайд 34CHRONIC CHOLECYSTITIS. SURGICAL TREATMENT
The optimal timing of surgical intervention in patients with
acute cholecystitis depends on stabilization of the patient.
Urgent (emergency) cholecystectomy or cholecystostomy is probably appropriate in most patients in whom a complication of acute cholecystitis such as empyema, emphysematous cholecystitis, or perforation is suspected or confirmed. In uncomplicated cases of cholecystitis, up to 30% of patients fail to resolve their symptoms on appropriate medical therapy, and progression of the attack or occurring of complication leads to the performance of early operation (within 24 to 72 h).
Early cholecystectomy is the treatment of choice for most patients with exacerbation of chronic calculous cholecystitis.
Слайд 35CHRONIC CHOLECYSTITIS. SURGICAL TREATMENT
Delayed surgical intervention is probably best reserved for
(1)
patients with very high risk for early surgery
(2) patients in whom the diagnosis of cholecystitis is in doubt.
Mortality figures for emergency cholecystectomy in most centers approach 0.5% - 3%.
Of course, the operative risks increase with age-related diseases of other organ systems and with the presence of long- or short-term complications of gallbladder disease.
Seriously ill or debilitated patients with cholecystitis may be managed with cholecystostomy and tube drainage of the gallbladder.
Elective cholecystectomy may then be done at a later date.
Слайд 36Postcholecystectomy Complications
Early complications following cholecystectomy include atelectasis and other pulmonary disorders, abscess
formation (often subphrenic), external or internal hemorrhage, biliary-enteric fistula, and bile leaks.
Jaundice may indicate absorption of bile from an intraabdominal collection following a biliary leak or mechanical obstruction of the CBD by retained calculi, intraductal blood clots, or extrinsic compression. Routine performance of intraoperative cholangiography during cholecystectomy has helped to reduce the incidence of these early complications.
In a small percentage of patients, however, a disorder of the extrahepatic bile ducts may result in persistent symptomatology. These so-called postcholecystectomy syndromes may be due to
(1) biliary strictures,
(2) retained biliary calculi,
(3) cystic duct stump syndrome,
(4) stenosis or dyskinesia of the sphincter of Oddi,
(5) bile salt–induced diarrhea or gastritis.
Слайд 37LIST OF DISEASES OF THE BILE DUCTS
CONGENITAL ANOMALIES
CHOLEDOCHOLITHIASIS
CHOLANGITIS
PAPILLARY DYSFUNCTION
PAPILLARY STENOSIS
SPASM OF THE
SPHINCTER OF ODDI
BILIARY DYSKINESIA
PRIMARY BILIARY CIRRHOSIS
AUTOIMMUNE CHOLANGITIS
NEOPLASMS OF THE BILIARY TRACT
HEPATOBILIARY PARASITISM
SCLEROSING CHOLANGITIS
Слайд 38DISEASES OF THE BILE DUCTS. CONGENITAL ANOMALIES
Biliary Atresia and Hypoplasia
Atretic and hypoplastic
lesions of the extrahepatic and major intrahepatic bile ducts are the most common biliary anomalies in infancy. The clinical picture is obstructive jaundice during the first month of life, with pale stools. The diagnosis is confirmed by operative cholangiography. Approximately 10% of cases are treatable with choledochojejunostomy, with hepatic portoenterostomy. Most patients, even with successful biliary-enteric anastomoses, develop chronic cholangitis, extensive hepatic fibrosis, and portal hypertension.
Choledochal Cysts
Cystic dilatation may involve the free portion of the CBD, i.e., choledochal cyst, or may present as diverticulum formation in the intraduodenal segment. Chronic reflux of pancreatic juice into the biliary tree can produce inflammation and stenosis of the extrahepatic bile ducts leading to cholangitis or biliary obstruction. The diagnosis may be made by ultrasound, abdominal CT, MRI, or cholangiography. Only one-third of patients show the classic triad of abdominal pain, jaundice, and an abdominal mass. Surgical treatment involves excision of the “cyst” and biliary-enteric anastomosis. Patients with choledochal cysts are at increased risk for the subsequent development of Cholangiocarcinoma.
Слайд 39DISEASES OF THE BILE DUCTS. CONGENITAL ANOMALIES
Congenital Biliary Ectasia
Dilatation of intrahepatic bile
ducts may involve either the major intrahepatic radicles (Caroli's disease), the inter- and intralobular ducts (congenital hepatic fibrosis), or both. In Caroli's disease, clinical manifestations include recurrent cholangitis, abscess formation in and around the affected ducts, and, often, gallstone formation within portions of ectatic intrahepatic biliary radicles. Ultrasound, MRI, and CT are of great diagnostic value in demonstrating cystic dilatation of the intrahepatic bile ducts. Treatment with ongoing antibiotic therapy is usually undertaken in an effort to limit the frequency and severity of cholangitis. Progression to secondary biliary cirrhosis with portal hypertension, extrahepatic biliary obstruction, Cholangiocarcinoma, or recurrent episodes of sepsis with hepatic abscess formation is common.
Слайд 40DISEASES OF THE BILE DUCTS.
CHOLEDOCHOLITHIASIS
Passage of gallstones into the CBD occurs in
approximately 10 to 15% of patients with cholelithiasis.
The incidence of common duct stones increases with increasing age of the patient.
Undetected duct stones are in approximately 1 - 5% of cholecystectomy patients.
The majority of bile duct stones are cholesterol stones formed in the gallbladder, which then migrate into the extrahepatic biliary tree through the cystic duct.
Слайд 41DISEASES OF THE BILE DUCTS
CHOLEDOCHOLITHIASIS
Primary calculi arising de novo in the ducts
are usually pigment stones developing in patients with
hepatobiliary parasitism or chronic, recurrent cholangitis;
congenital anomalies of the bile ducts (especially Caroli's disease);
dilated, sclerosed, or strictured ducts;
an MDR3 gene defect leading to impaired biliary phospholipids secretion.
Common duct stones may remain asymptomatic for years, may pass spontaneously into the duodenum, or most often may present with biliary colic or a complication.
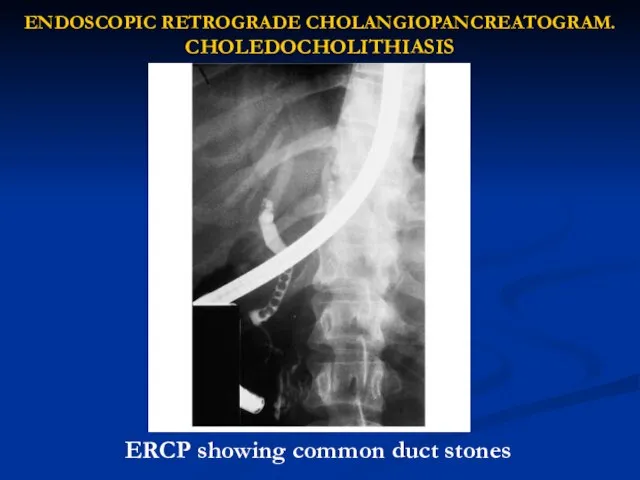
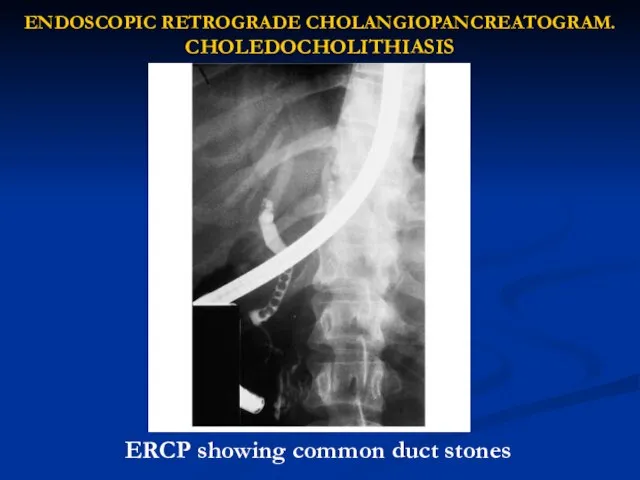
Слайд 42ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAM. CHOLEDOCHOLITHIASIS
ERCP showing common duct stones
Слайд 43CHOLEDOCHOLITHIASIS. Complications
CHOLANGITIS
Cholangitis may be acute or chronic, and symptoms result from
inflammation, which usually requires at least partial obstruction to the flow of bile. Bacteria are present on bile culture in approximately 75% of patients with acute cholangitis early in the symptomatic course.
The characteristic presentation of acute cholangitis involves biliary pain, jaundice, and fevers with chills (Charcot's triad). Blood cultures are frequently positive, and leukocytosis is typical.
Слайд 44CHOLEDOCHOLITHIASIS. Complications
Nonsuppurative acute cholangitis is most common and may respond relatively rapidly
to supportive measures and to treatment with antibiotics.
In suppurative acute cholangitis the presence of pus under pressure in a completely obstructed ductal system leads to symptoms of severe toxicity — mental confusion, bacteremia, and septic shock. Response to antibiotics alone is relatively poor, multiple hepatic abscesses are often present, and the mortality rate approaches 100% without endoscopic or surgical relief of the obstruction and drainage of infected bile.
Endoscopic management of bacterial cholangitis is as effective as surgical intervention. In combination with endoscopic sphincterotomy it is safe and the preferred initial procedure for diagnosis and effective therapy.
Слайд 45CHOLEDOCHOLITHIASIS
Complications. OBSTRUCTIVE JAUNDICE
Gradual obstruction of the CBD over a period of weeks
or months usually leads to initial manifestations of jaundice or pruritus without associated symptoms of biliary colic or cholangitis.
Painless jaundice may occur in patients with choledocholithiasis, but this manifestation is much more characteristic of biliary obstruction secondary to malignancy of the head of the pancreas, bile ducts, or ampoule of Vater.
The presence of a palpably enlarged gallbladder suggests that the biliary obstruction is secondary to an underlying malignancy rather than to calculous disease - Courvoisier's law
Biliary obstruction causes progressive dilatation of the intrahepatic bile ducts, hepatic bile flow is suppressed, and reabsorption and regurgitation of conjugated bilirubin into the bloodstream lead to jaundice accompanied by dark urine (bilirubinuria) and light-colored (acholic) stools.
Слайд 46CHOLEDOCHOLITHIASIS
Complications. OBSTRUCTIVE JAUNDICE
CBD stones should be suspected in any patient with cholecystitis
whose serum bilirubin level exceeds 85.5 µmol/L (5 mg/dL). The maximum bilirubin level is seldom over 256.5 µmol/L (15.0 mg/dL) in patients with choledocholithiasis without concomitant hepatic disease or another factor leading to marked hyperbilirubinemia. Serum bilirubin levels of 342.0 µmol/L (20 mg/dL) or more should suggest the possibility of neoplastic obstruction.
The serum alkaline phosphatase level is almost always elevated in biliary obstruction. A rise in alkaline phosphatase often precedes clinical jaundice and may be the only abnormality in routine liver function tests. There may be a two- to tenfold elevation of serum aminotransferases, especially in association with acute obstruction.
Following relief of the obstructing process, serum aminotransferase elevations usually return rapidly to normal, while the serum bilirubin level may take 1 to 2 weeks to return to normal. The alkaline phosphatase level usually falls slowly, lagging behind the decrease in serum bilirubin.
Слайд 47PAPILLARY DYSFUNCTION, STENOSIS, SPASM OF THE SPHINCTER OF ODDI, BILIARY DYSKINESIA
Symptoms of
biliary colic accompanied by signs of recurrent, intermittent biliary obstruction may be produced by papillary stenosis, papillary dysfunction, spasm of the sphincter of Oddi, and biliary dyskinesia.
Papillary stenosis is result from acute or chronic inflammation of the papilla of Vater or from glandular hyperplasia of the papillary segment.
Five criteria have been used to define papillary stenosis:
(1) upper abdominal pain, usually RUQ or epigastric;
(2) abnormal liver tests;
(3) dilatation of the common bile duct upon ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAM examination;
(4) delayed (>45 min) drainage of contrast material from the duct;
(5) increased basal pressure of the sphincter of Oddi.
Слайд 48PAPILLARY DYSFUNCTION, STENOSIS, SPASM OF THE SPHINCTER OF ODDI, BILIARY DYSKINESIA
An alternative
to ERCP is magnetic resonance cholangiography (MRC). In patients with papillary stenosis, quantitative hepatobiliary scintigraphy has revealed delayed transit from the common bile duct to the bowel, ductal dilatation, and abnormal time-activity dynamics.
Treatment consists of endoscopic or surgical sphincteroplasty to ensure wide patency of the distal portions of both the bile and pancreatic ducts.
The factors usually considered as indications for sphincterotomy include
(1) prolonged duration of symptoms,
(2) lack of response to symptomatic treatment,
(3) presence of severe disability,
(4) the patient's choice of sphincterotomy over surgery.
Слайд 49 Proposed mechanisms of Dyskinesia of the sphincter of Oddi include spasm
of the sphincter, denervation sensitivity resulting in hypertonicity, and abnormalities in the sphincteric contraction waves.
Endoscopic biliary sphincterotomy (EBS) or surgical sphincteroplasty may be indicated in patients who fail to respond to a 2- to 3-month trial of medical therapy (medical treatment with nitrites or anticholinergics to attempt pharmacologic relaxation of the sphincter), especially if basal sphincter of Oddi pressures are elevated.
EBS has become the procedure of choice for removing bile duct stones and for other biliary and pancreatic problems.
Слайд 50Neoplasms of the biliary tract: Carcinoma of the biliary system manifests with
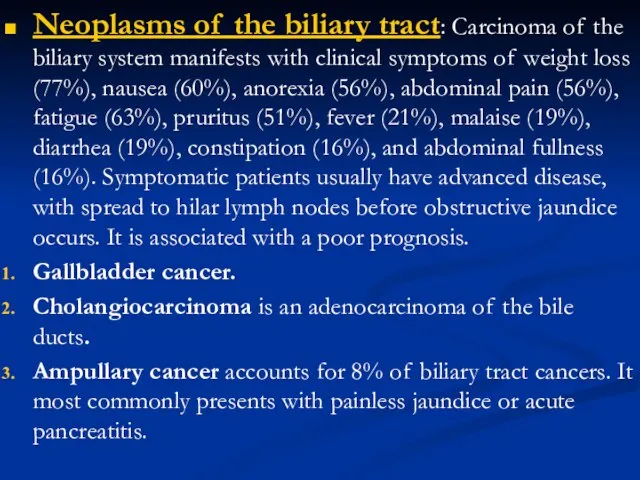
clinical symptoms of weight loss (77%), nausea (60%), anorexia (56%), abdominal pain (56%), fatigue (63%), pruritus (51%), fever (21%), malaise (19%), diarrhea (19%), constipation (16%), and abdominal fullness (16%). Symptomatic patients usually have advanced disease, with spread to hilar lymph nodes before obstructive jaundice occurs. It is associated with a poor prognosis.
Gallbladder cancer.
Cholangiocarcinoma is an adenocarcinoma of the bile ducts.
Ampullary cancer accounts for 8% of biliary tract cancers. It most commonly presents with painless jaundice or acute pancreatitis.
Слайд 51SCLEROSING CHOLANGITIS
Definition. Primary or idiopathic sclerosing cholangitis is characterized by a progressive,
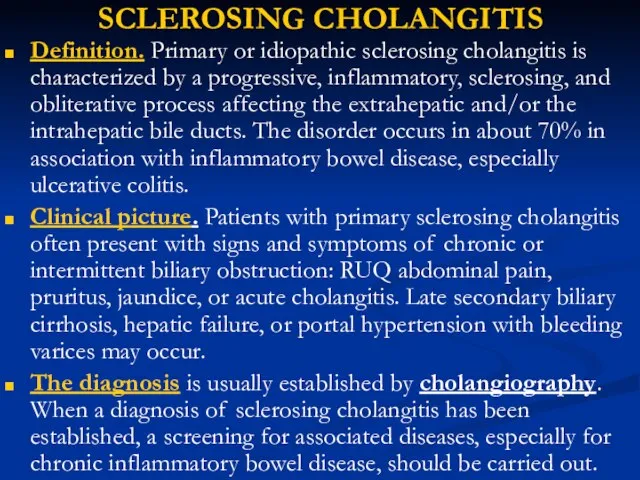
inflammatory, sclerosing, and obliterative process affecting the extrahepatic and/or the intrahepatic bile ducts. The disorder occurs in about 70% in association with inflammatory bowel disease, especially ulcerative colitis.
Clinical picture. Patients with primary sclerosing cholangitis often present with signs and symptoms of chronic or intermittent biliary obstruction: RUQ abdominal pain, pruritus, jaundice, or acute cholangitis. Late secondary biliary cirrhosis, hepatic failure, or portal hypertension with bleeding varices may occur.
The diagnosis is usually established by cholangiography. When a diagnosis of sclerosing cholangitis has been established, a screening for associated diseases, especially for chronic inflammatory bowel disease, should be carried out.
Слайд 52SCLEROSING CHOLANGITIS
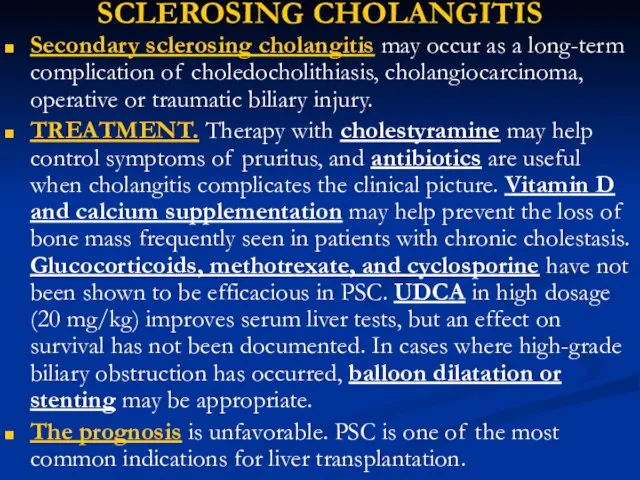
Secondary sclerosing cholangitis may occur as a long-term complication of choledocholithiasis,
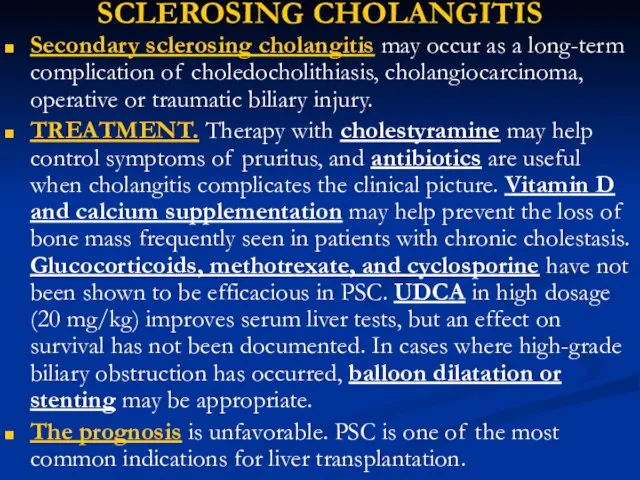
cholangiocarcinoma, operative or traumatic biliary injury.
TREATMENT. Therapy with cholestyramine may help control symptoms of pruritus, and antibiotics are useful when cholangitis complicates the clinical picture. Vitamin D and calcium supplementation may help prevent the loss of bone mass frequently seen in patients with chronic cholestasis. Glucocorticoids, methotrexate, and cyclosporine have not been shown to be efficacious in PSC. UDCA in high dosage (20 mg/kg) improves serum liver tests, but an effect on survival has not been documented. In cases where high-grade biliary obstruction has occurred, balloon dilatation or stenting may be appropriate.
The prognosis is unfavorable. PSC is one of the most common indications for liver transplantation.
Слайд 53DIFFERENTIAL DIAGNOSIS OF JAUNDICE AND HYPERBILIRUBINEMIA
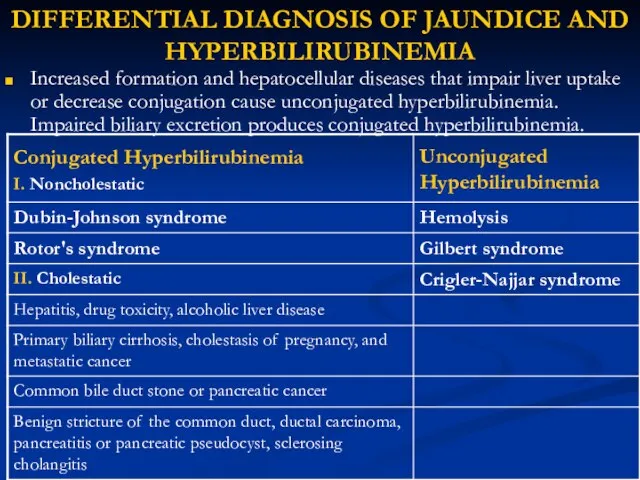
Increased formation and hepatocellular diseases that impair
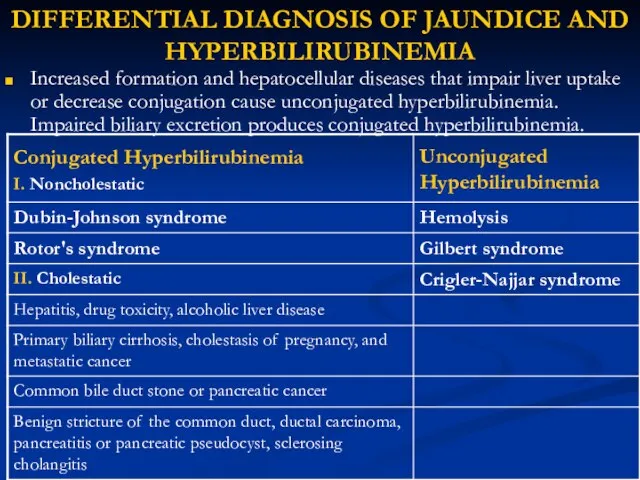
liver uptake or decrease conjugation cause unconjugated hyperbilirubinemia. Impaired biliary excretion produces conjugated hyperbilirubinemia.
Слайд 54Noncholestatic Conjugated Hyperbilirubinemia
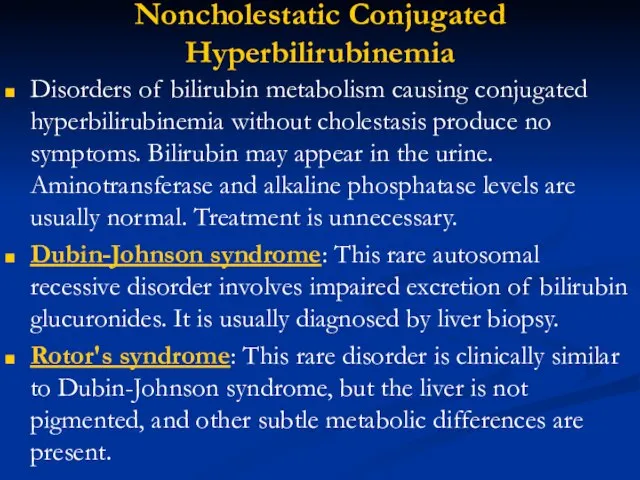
Disorders of bilirubin metabolism causing conjugated hyperbilirubinemia without cholestasis produce
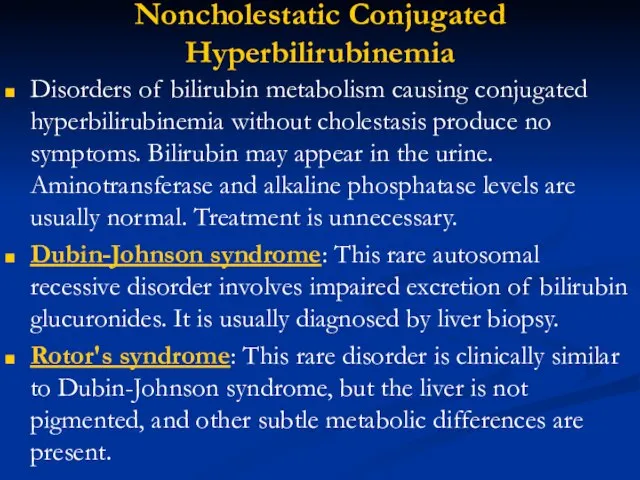
no symptoms. Bilirubin may appear in the urine. Aminotransferase and alkaline phosphatase levels are usually normal. Treatment is unnecessary.
Dubin-Johnson syndrome: This rare autosomal recessive disorder involves impaired excretion of bilirubin glucuronides. It is usually diagnosed by liver biopsy.
Rotor's syndrome: This rare disorder is clinically similar to Dubin-Johnson syndrome, but the liver is not pigmented, and other subtle metabolic differences are present.
Слайд 55Unconjugated Hyperbilirubinemia
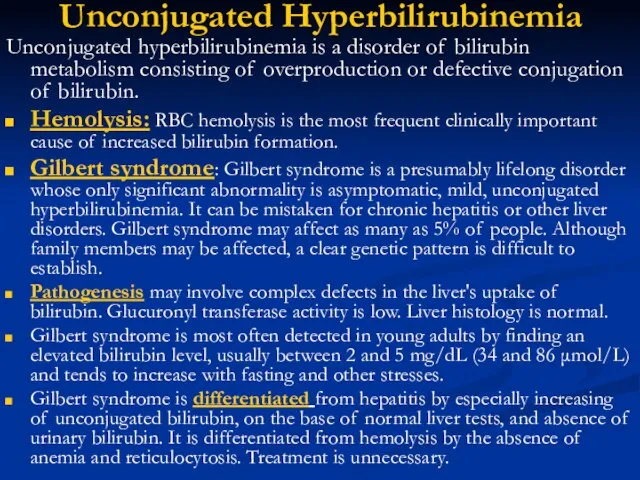
Unconjugated hyperbilirubinemia is a disorder of bilirubin metabolism consisting of overproduction
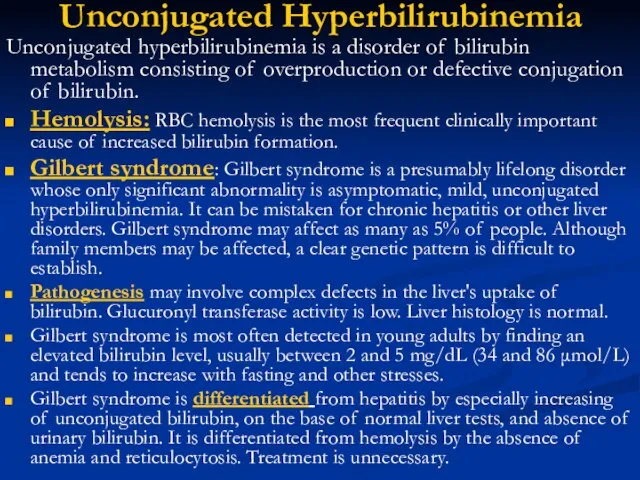
or defective conjugation of bilirubin.
Hemolysis: RBC hemolysis is the most frequent clinically important cause of increased bilirubin formation.
Gilbert syndrome: Gilbert syndrome is a presumably lifelong disorder whose only significant abnormality is asymptomatic, mild, unconjugated hyperbilirubinemia. It can be mistaken for chronic hepatitis or other liver disorders. Gilbert syndrome may affect as many as 5% of people. Although family members may be affected, a clear genetic pattern is difficult to establish.
Pathogenesis may involve complex defects in the liver's uptake of bilirubin. Glucuronyl transferase activity is low. Liver histology is normal.
Gilbert syndrome is most often detected in young adults by finding an elevated bilirubin level, usually between 2 and 5 mg/dL (34 and 86 μmol/L) and tends to increase with fasting and other stresses.
Gilbert syndrome is differentiated from hepatitis by especially increasing of unconjugated bilirubin, on the base of normal liver tests, and absence of urinary bilirubin. It is differentiated from hemolysis by the absence of anemia and reticulocytosis. Treatment is unnecessary.
Слайд 56Unconjugated Hyperbilirubinemia
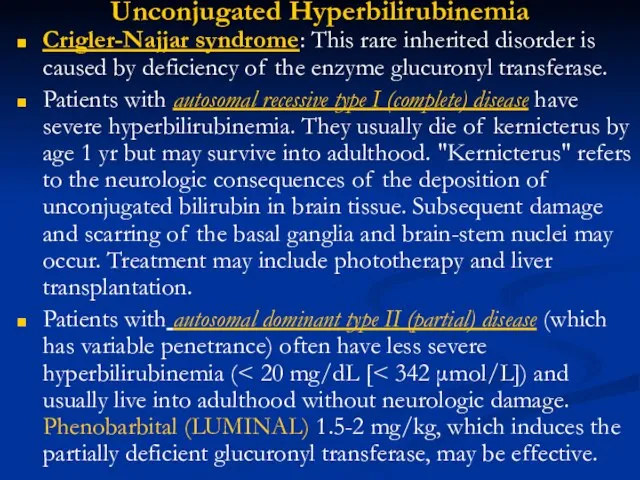
Crigler-Najjar syndrome: This rare inherited disorder is caused by deficiency of
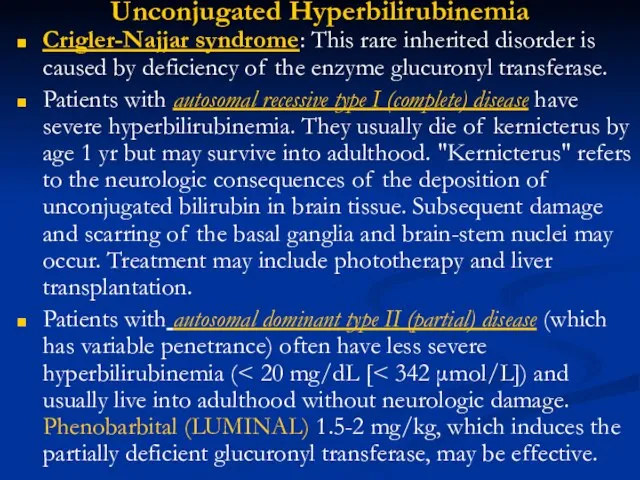
the enzyme glucuronyl transferase.
Patients with autosomal recessive type I (complete) disease have severe hyperbilirubinemia. They usually die of kernicterus by age 1 yr but may survive into adulthood. "Kernicterus" refers to the neurologic consequences of the deposition of unconjugated bilirubin in brain tissue. Subsequent damage and scarring of the basal ganglia and brain-stem nuclei may occur. Treatment may include phototherapy and liver transplantation.
Patients with autosomal dominant type II (partial) disease (which has variable penetrance) often have less severe hyperbilirubinemia (< 20 mg/dL [< 342 μmol/L]) and usually live into adulthood without neurologic damage. Phenobarbital (LUMINAL) 1.5-2 mg/kg, which induces the partially deficient glucuronyl transferase, may be effective.

 Знакомство с миром профессионального труда как одна из составляющих программы развития личности дошкольника
Знакомство с миром профессионального труда как одна из составляющих программы развития личности дошкольника Вера моя крепка
Вера моя крепка Место физкультуры и спорта в моей жизни. Введение
Место физкультуры и спорта в моей жизни. Введение Техническое регулирование деятельности предприятий и организаций нефтегазового комплекса
Техническое регулирование деятельности предприятий и организаций нефтегазового комплекса Азбука в загадках-добавлялках
Азбука в загадках-добавлялках Предпосылки создания Древнерусского Государства
Предпосылки создания Древнерусского Государства Сельский туризм. Западный опыт. Общий обзор.
Сельский туризм. Западный опыт. Общий обзор. Reflection
Reflection Презентация на тему Начало создания колониальных империй
Презентация на тему Начало создания колониальных империй  Загрязнение воздуха
Загрязнение воздуха Летняя математическая школа
Летняя математическая школа Моря, омывающие берега России (8 класс)
Моря, омывающие берега России (8 класс) Практика для студентов в отделе кадров
Практика для студентов в отделе кадров Родительское собрание: «Итоговая аттестация учащихся 11-х классов в 2011-2012 учебном году» 22 ноября 2011 г
Родительское собрание: «Итоговая аттестация учащихся 11-х классов в 2011-2012 учебном году» 22 ноября 2011 г О методических и организационно-технологических аспектах проведения ГИА-9 в новой форме в 2011-2012 г.г.Станченко С.В., заместитель д
О методических и организационно-технологических аспектах проведения ГИА-9 в новой форме в 2011-2012 г.г.Станченко С.В., заместитель д Антикафе Чтец
Антикафе Чтец Бизнес-проект по открытию предприятия по производству и реализации корпусной мебели
Бизнес-проект по открытию предприятия по производству и реализации корпусной мебели Нейтронные звезды
Нейтронные звезды ОРГАНИЗАЦИОННАЯ СТРУКТУРА ПРЕДПРИЯТИЯ (ОРГАНИЗАЦИИ)
ОРГАНИЗАЦИОННАЯ СТРУКТУРА ПРЕДПРИЯТИЯ (ОРГАНИЗАЦИИ) Презентация на тему Владимиро-Суздальское княжество (6 класс)
Презентация на тему Владимиро-Суздальское княжество (6 класс) РЕЗУЛЬТАТЫ ПРОЕКТА«Настройка образовательных программ в российских вузах»(TUNING Educational Programmes in Russian HEIs)
РЕЗУЛЬТАТЫ ПРОЕКТА«Настройка образовательных программ в российских вузах»(TUNING Educational Programmes in Russian HEIs) Лето ягодное Часть 4
Лето ягодное Часть 4 Хозяйство России
Хозяйство России 20170201_baykal_8_klass
20170201_baykal_8_klass HISTORICAL BACKGROUND OF THE UK (Ancient Britain
HISTORICAL BACKGROUND OF THE UK (Ancient Britain Учебно-методический комплект «ИСТОРИЯ РОССИИ 1945-2008 гг.»(Концептуальные основы курса.Авторский коллектив.)
Учебно-методический комплект «ИСТОРИЯ РОССИИ 1945-2008 гг.»(Концептуальные основы курса.Авторский коллектив.) Шенген визы: открой себе Европу
Шенген визы: открой себе Европу Языковой портфолио как инструмент рефлексивной самооценки учащихся
Языковой портфолио как инструмент рефлексивной самооценки учащихся