Содержание
- 2. Crohn’s Disease Aim of this module To increase the understanding of Crohn’s disease by looking at
- 3. How to use this module This module is designed by a student for students. The data
- 4. Epidemiology & Pathology of Crohn’s Disease
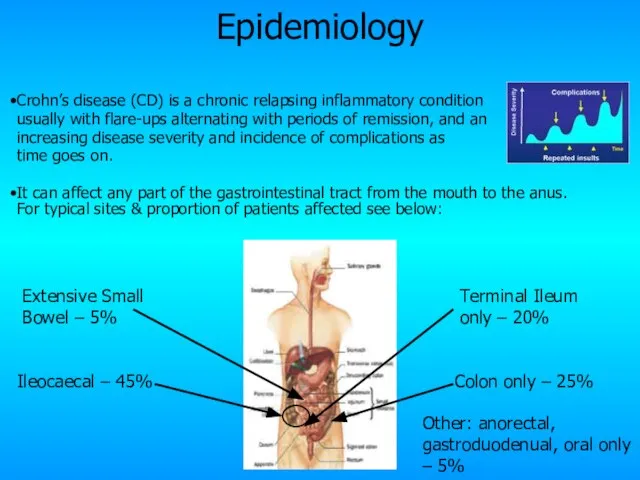
- 5. Crohn’s disease (CD) is a chronic relapsing inflammatory condition usually with flare-ups alternating with periods of
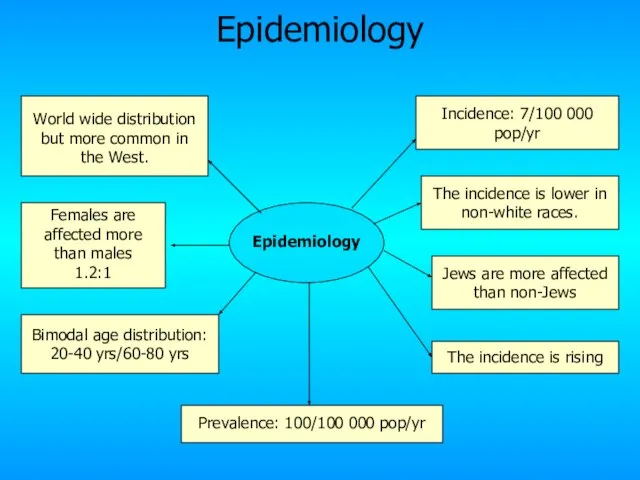
- 6. Epidemiology Incidence: 7/100 000 pop/yr Prevalence: 100/100 000 pop/yr World wide distribution but more common in
- 7. Pathology It is characterised by patchy transmural inflammation. The chronic inflammatory process leads of thickening of
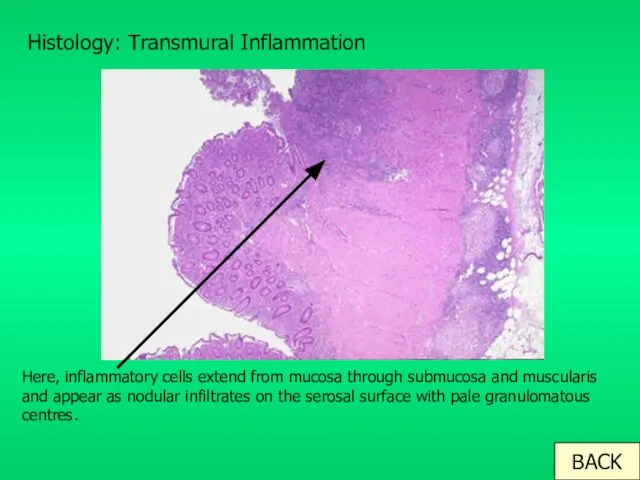
- 8. Histology: Transmural Inflammation Here, inflammatory cells extend from mucosa through submucosa and muscularis and appear as
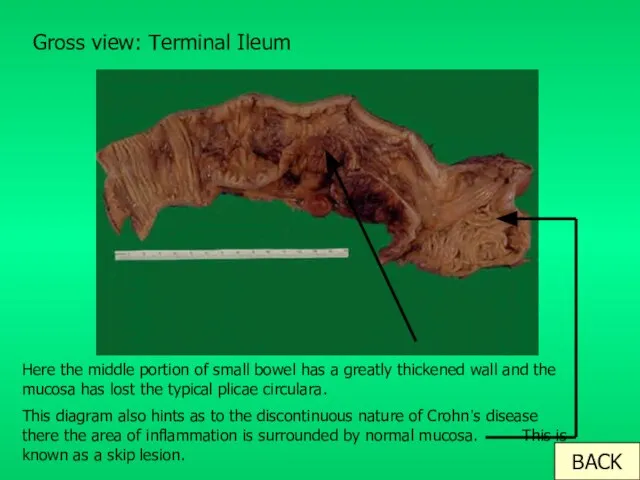
- 9. Gross view: Terminal Ileum Here the middle portion of small bowel has a greatly thickened wall
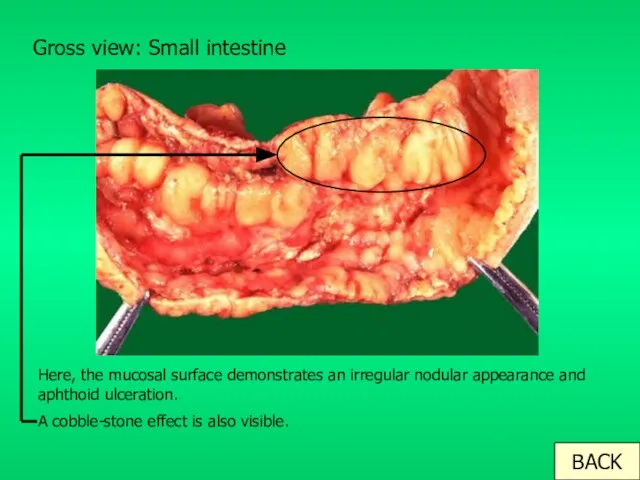
- 10. Gross view: Small intestine Here, the mucosal surface demonstrates an irregular nodular appearance and aphthoid ulceration.
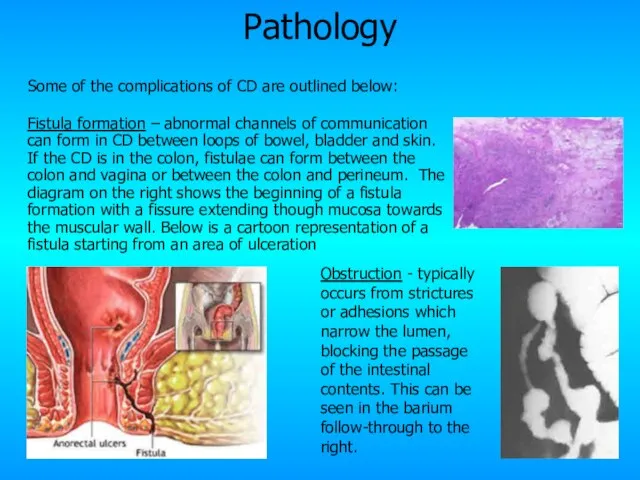
- 11. Pathology Some of the complications of CD are outlined below: Fistula formation – abnormal channels of
- 12. Aetiology and Pathogenesis of Crohn’s Disease
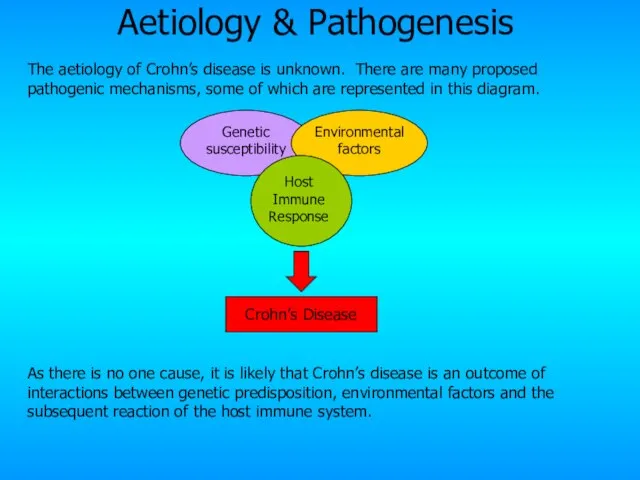
- 13. Aetiology & Pathogenesis The aetiology of Crohn’s disease is unknown. There are many proposed pathogenic mechanisms,
- 14. Genetic Factors There are 3 mutations on the CARD15 gene on Chromosome 16 that are associated
- 15. Environmental Factors A wide range of environmental factors have been found to play a role: Smoking
- 16. Immune response Host Immune Response Both the potential genetics underlying CD and the environmental and host
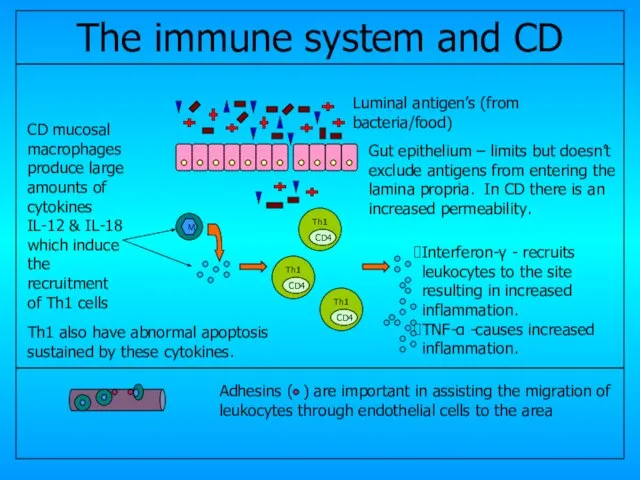
- 17. CD4 CD4 CD4 Gut epithelium – limits but doesn’t exclude antigens from entering the lamina propria.
- 18. Clinical features of Crohn’s Disease
- 19. Clinical Features The clinical presentation can be very variable depending upon the site and predominant pathology
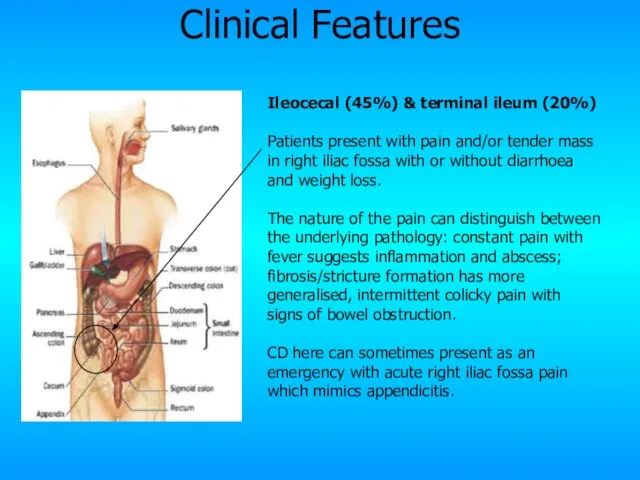
- 20. Ileocecal (45%) & terminal ileum (20%) Patients present with pain and/or tender mass in right iliac
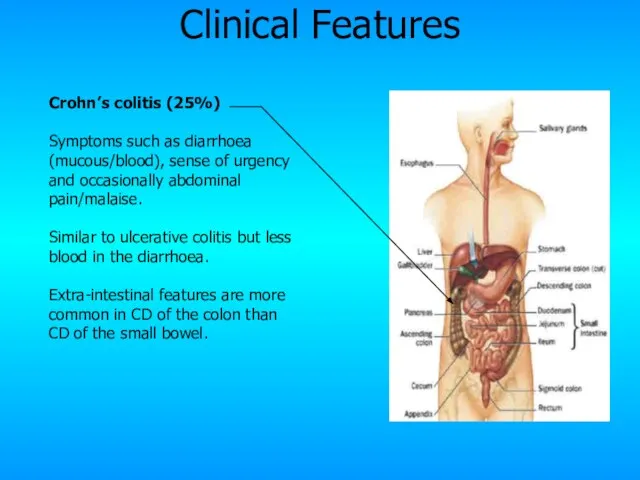
- 21. Crohn’s colitis (25%) Symptoms such as diarrhoea (mucous/blood), sense of urgency and occasionally abdominal pain/malaise. Similar
- 22. Gastroduodenal & oral (5%) Very rare. The former presents with upper abdominal pain or dyspepsia with
- 23. Extensive small bowel (5%) Presents with typical pain, diarrhoea and weight loss in addition to features
- 24. Perianal CD – complication Characterised by perianal pain and/or discharge. It’s due to fistula, fissure or
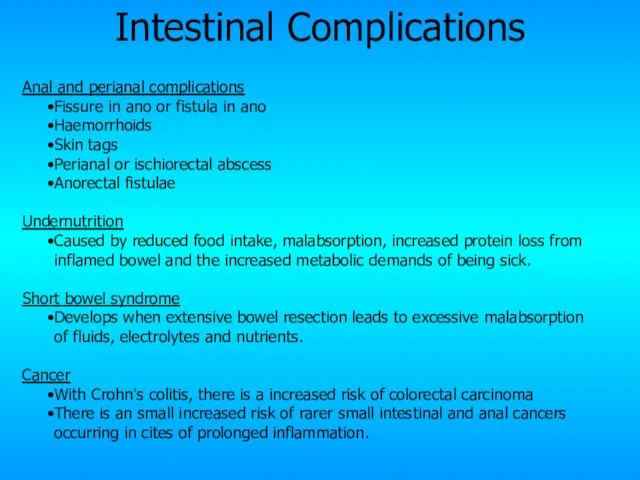
- 25. Intestinal Complications Anal and perianal complications Fissure in ano or fistula in ano Haemorrhoids Skin tags
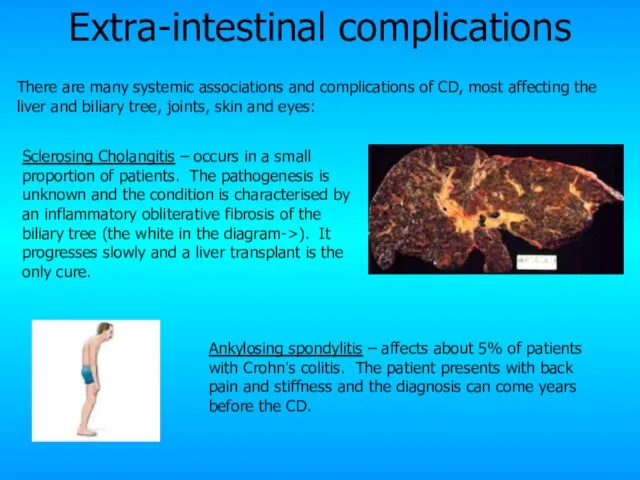
- 26. Extra-intestinal complications Sclerosing Cholangitis – occurs in a small proportion of patients. The pathogenesis is unknown
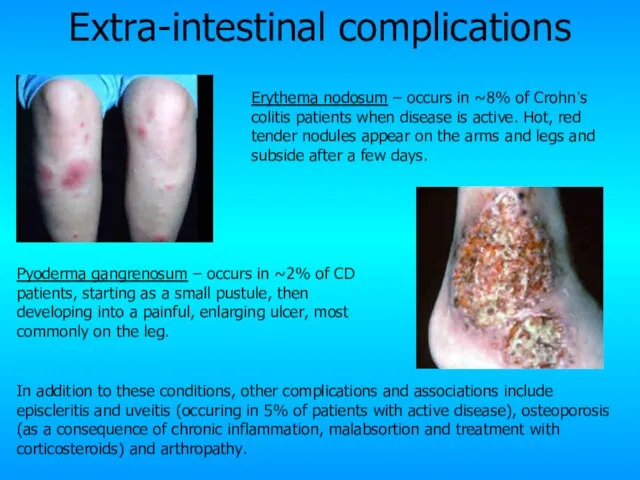
- 27. Extra-intestinal complications Pyoderma gangrenosum – occurs in ~2% of CD patients, starting as a small pustule,
- 28. Diagnosis and Management of Crohn’s Disease
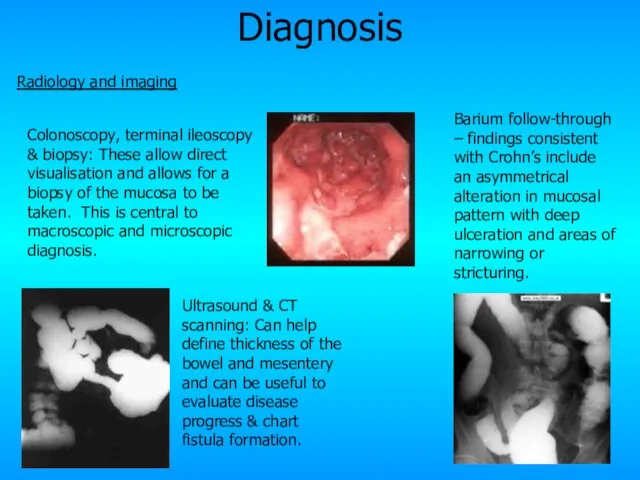
- 29. Diagnosis Radiology and imaging Ultrasound & CT scanning: Can help define thickness of the bowel and
- 30. Diagnosis Blood tests Haematology: results suggesting anaemia, ? platelet count & ? ESR suggests an inflammatory
- 31. Differential Diagnosis There are many differential diagnosis for Crohn’s disease, complicated further by the differing presentations
- 32. Management Management is best if a MDT approach is adopted, including physicians, surgeons, specialist nurses, dieticians
- 33. Medical management Dietary advice and nutritional support including vitamin supplementation to counter-act any deficiencies that develop.
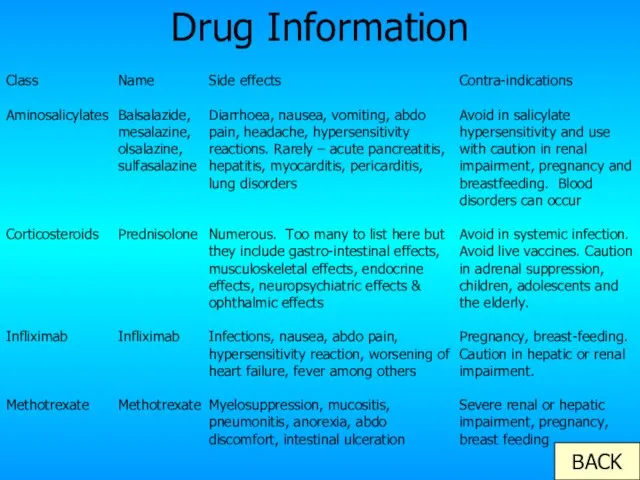
- 34. Drug Information BACK Class Aminosalicylates Corticosteroids Infliximab Methotrexate Name Balsalazide, mesalazine, olsalazine, sulfasalazine Prednisolone Infliximab Methotrexate
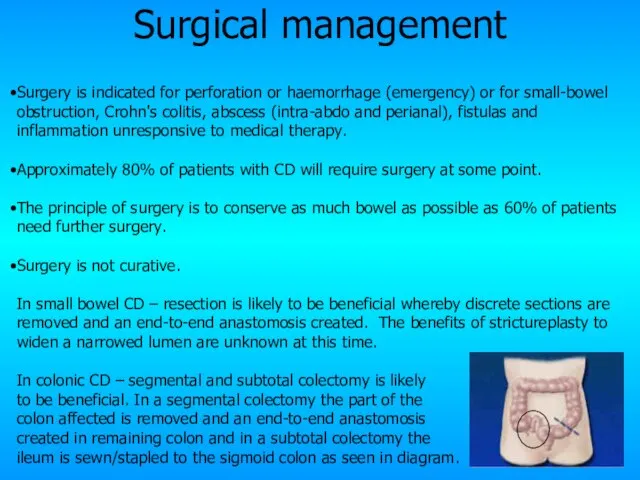
- 35. Surgical management Surgery is indicated for perforation or haemorrhage (emergency) or for small-bowel obstruction, Crohn's colitis,
- 36. Prognosis Mortality The cumulative mortality is approximately twice that of the general population. Death is primarily
- 37. Summary Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract characterised by transmural inflammation,
- 38. The different sections If you want to revisit any of the sections of this module please
- 39. Case Study 30-year-old woman was admitted with a 4-week history of increasing bloody diarrhoea and abdominal
- 40. Case Study The rectal biopsy taken at sigmoidoscopy showed a small area of ulceration of the
- 41. Thank you I hope this has been of some help to your studies!
- 43. Скачать презентацию
 Стресс: это полезно или вредно?
Стресс: это полезно или вредно? Портрет в скульптуре 6 класс
Портрет в скульптуре 6 класс "Лучший классный руководитель"
"Лучший классный руководитель" Итоговый тест по математике за курс 5 класса
Итоговый тест по математике за курс 5 класса Тонкий лед
Тонкий лед Возникновение и эволюция сравнительного менеджмента
Возникновение и эволюция сравнительного менеджмента Президентский Клуб 2012-2013
Президентский Клуб 2012-2013 Типология писем в историческом романе А.С.Пушкина «Капитанская дочка».
Типология писем в историческом романе А.С.Пушкина «Капитанская дочка». Серебряный век русской поэзии
Серебряный век русской поэзии Соблюдение работниками профессиональной и служебной этики, морально-этических норм при проведении экзамена
Соблюдение работниками профессиональной и служебной этики, морально-этических норм при проведении экзамена Презентация на тему Лес и его обитатели
Презентация на тему Лес и его обитатели Презентация на тему Word building
Презентация на тему Word building СТРОИТЕЛЬСТВО СЕТИ МИНИ-ТЭЦ НА БАЗЕ МУНИЦИПАЛЬНЫХ КОТЕЛЬНЫХ ОРЕНБУРГСКОЙ ОБЛАСТИ «Проект 200МВт» ООО «Оренбургская управляющая эн
СТРОИТЕЛЬСТВО СЕТИ МИНИ-ТЭЦ НА БАЗЕ МУНИЦИПАЛЬНЫХ КОТЕЛЬНЫХ ОРЕНБУРГСКОЙ ОБЛАСТИ «Проект 200МВт» ООО «Оренбургская управляющая эн Экосистема цифрового мобильного контента
Экосистема цифрового мобильного контента По следам прочитанного
По следам прочитанного Созвездия талантов. Вокальный кружок
Созвездия талантов. Вокальный кружок Презентация на тему Состав чисел первого десятка
Презентация на тему Состав чисел первого десятка Научно-производственное предприятие «Грант»
Научно-производственное предприятие «Грант» История Олимпийского движения
История Олимпийского движения ИОННЫЕ ИСТОЧНИКИ с замкнутым дрейфом электронов
ИОННЫЕ ИСТОЧНИКИ с замкнутым дрейфом электронов Изменение имён прилагательных по родам и числам 3 класс
Изменение имён прилагательных по родам и числам 3 класс Цифровая и микропроцессорная техника в управлении
Цифровая и микропроцессорная техника в управлении Наши зимние забавы
Наши зимние забавы Занятие № 1 «Необычный взгляд на обычные вещи»
Занятие № 1 «Необычный взгляд на обычные вещи» Артериальная гипертензия эндокринного генеза: Акромегалия, гипертиреоз, гипотиреоз
Артериальная гипертензия эндокринного генеза: Акромегалия, гипертиреоз, гипотиреоз Презентация на тему Вода в природе 3 класс
Презентация на тему Вода в природе 3 класс Операторы организации циклов
Операторы организации циклов  л7 Средневековый Восток
л7 Средневековый Восток