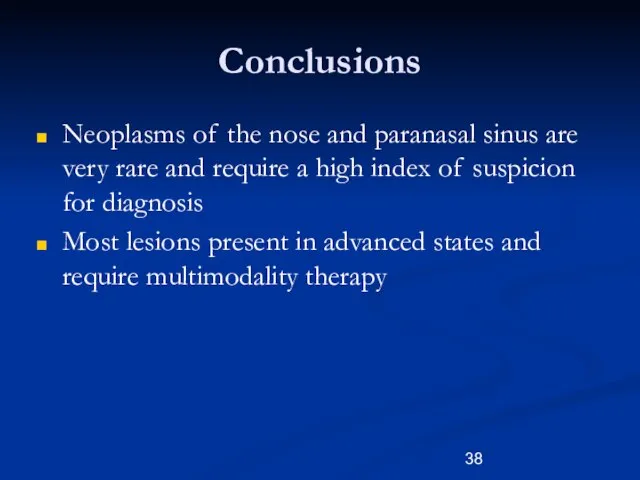
Слайд 2Neoplasms of Nose and Paranasal Sinuses
Very rare 3%
Delay in diagnosis due to
similarity to benign conditions
Nasal cavity
½ benign
½ malignant
Paranasal Sinuses
Malignant
Слайд 3Neoplasms of Nose and Paranasal Sinuses
Multimodality treatment
Orbital Preservation
Minimally invasive surgical techniques
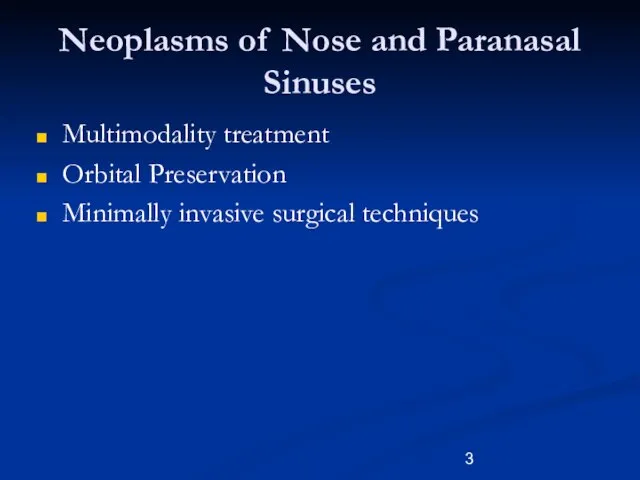
Слайд 4
Epidemiology
Predominately of older males
Exposure:
Wood, nickel-refining processes
Industrial fumes, leather tanning
Cigarette and Alcohol
consumption
No significant association has been shown
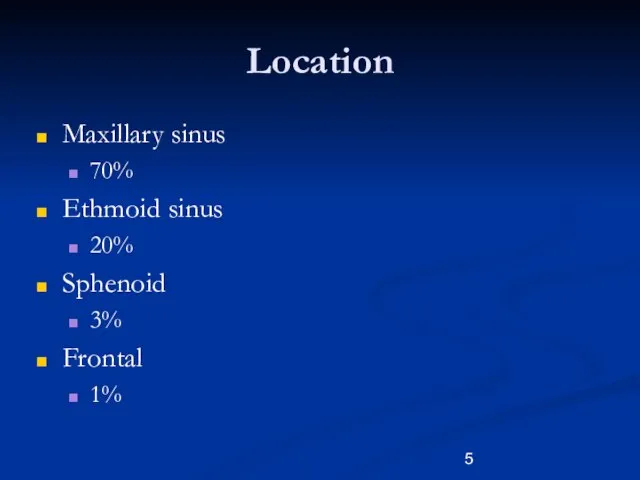
Слайд 5Location
Maxillary sinus
70%
Ethmoid sinus
20%
Sphenoid
3%
Frontal
1%
Слайд 6Presentation
Oral symptoms: 25-35%
Pain, trismus, alveolar ridge fullness, erosion
Nasal findings: 50%
Obstruction, epistaxis, rhinorrhea
Ocular
findings: 25%
Epiphora, diplopia, proptosis
Facial signs
Paresthesias, asymmetry
Слайд 7Radiography
CT
Bony erosion
Limitations with periorbita involvement
MRI
94 -98% correlation with surgical findings
Inflammation/retained secretions: low
T1, high T2
Hypercellular malignancy: low/intermediate on both
Enhancement with Gadolinium
Слайд 8Benign Lesions
Papillomas
Osteomas
Fibrous Dysplasia
Neurogenic tumors
Слайд 9Papilloma
Vestibular papillomas
Schneiderian papillomas derived from schneiderian mucosa (squamous)
Fungiform: 50%, nasal septum
Cylindrical: 3%,
lateral wall/sinuses
Inverted: 47%, lateral wall
Слайд 10Inverted Papilloma
4% of sinonasal tumors
Site of Origin: lateral nasal wall
Unilateral
Malignant degeneration in
2-13% (avg 10%)
Слайд 11Inverted Papilloma
Resection
Initially via transnasal resection:
50-80% recurrence
Medial Maxillectomy via lateral rhinotomy:
Gold Standard
10-20%
Endoscopic medial
maxillectomy:
Key concepts:
Identify the origin of the papilloma
Bony removal of this region
Recurrent lesions:
Via medial maxillectomy vs. Endoscopic resection
22%
Слайд 12Osteomas
Benign slow growing tumors of mature bone
Location:
Frontal, ethmoids, maxillary sinuses
When obstructing mucosal
flow can lead to mucocele formation
Treatment is local excision
Слайд 13Fibrous dysplasia
Dysplastic transformation of normal bone with collagen, fibroblasts, and osteoid material
Monostotic
vs Polyostotic
Surgical excision for obstructing lesions
Malignant transformation to rhabdomyosarcoma has been seen with radiation
Слайд 14Neurogenic tumors
4% are found within the paranasal sinuses
Schwannomas
Neurofibromas
Treatment via surgical resection
Neurogenic Sarcomas
are very aggressive and require surgical excision with post op chemo/XRT for residual disease.
When associated with Von Recklinghausen’s syndrome: more aggressive (30% 5yr survival).
Слайд 15Malignant lesions
Squamous cell carcinoma
Adenoid cystic carcinoma
Mucoepidermoid carcinoma
Adenocarcinoma
Hemangiopericytoma
Melanoma
Olfactory neuroblastoma
Osteogenic sarcoma, fibrosarcoma, chondrosarcoma, rhabdomyosarcoma
Lymphoma
Metastatic
tumors
Sinonasal undifferentiated carcinoma
Слайд 16Squamous cell carcinoma
Most common tumor (80%)
Location:
Maxillary sinus (70%)
Nasal cavity (20%)
90% have local
invasion by presentation
Lymphatic drainage:
First echelon: retropharyngeal nodes
Second echelon: subdigastric nodes
Слайд 17Treatment
88% present in advanced stages (T3/T4)
Surgical resection with postoperative radiation
Complex 3-D anatomy
makes margins difficult
Слайд 18Adenoid Cystic Carcinoma
3rd most common site is the nose/paranasal sinuses
Perineural spread
Anterograde and
retrograde
Despite aggressive surgical resection and radiotherapy, most grow insidiously.
Neck metastasis is rare and usually a sign of local failure
Postoperative XRT is very important
Слайд 19Mucoepidermoid Carcinoma
Extremely rare
Widespread local invasion makes resection difficult, therefore radiation is often
indicated
Слайд 20Adenocarcinoma
2nd most common malignant tumor in the maxillary and ethmoid sinuses
Present most
often in the superior portions
Strong association with occupational exposures
High grade: solid growth pattern with poorly defined margins. 30% present with metastasis
Low grade: uniform and glandular with less incidence of perineural invasion/metastasis.
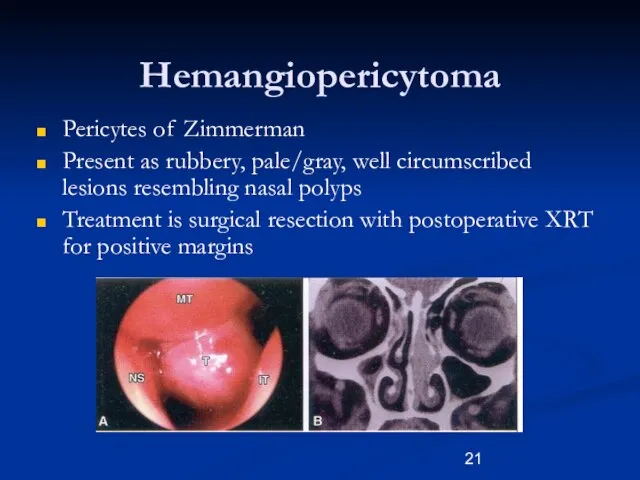
Слайд 21Hemangiopericytoma
Pericytes of Zimmerman
Present as rubbery, pale/gray, well circumscribed lesions resembling nasal polyps
Treatment
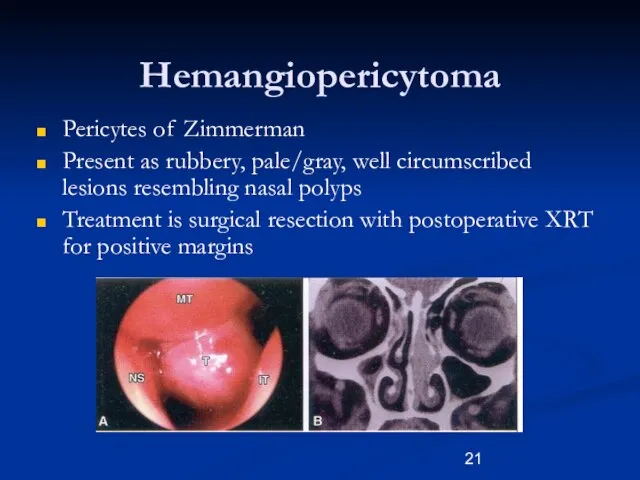
is surgical resection with postoperative XRT for positive margins
Слайд 22Melanoma
0.5- 1.5% of melanoma originates from the nasal cavity and paranasal sinus.
Anterior
Septum: most common site
Treatment is wide local excision with/without postoperative radiation therapy
END not recommended
AFIP: Poor prognosis
5yr: 11%
20yr: 0.5%
Слайд 23Olfactory Neuroblastoma
Esthesioneuroblastoma
Originate from stem cells of neural crest origin that differentiate into
olfactory sensory cells.
Kadish Classification
A: confined to nasal cavity
B: involving the paranasal cavity
C: extending beyond these limits
Слайд 24Olfactory Neuroblastoma
Esthesioneuroblastoma
UCLA Staging system
T1: Tumor involving nasal cavity and/or paranasal sinus, excluding
the sphenoid and superior most ethmoids
T2: Tumor involving the nasal cavity and/or paranasal sinus including sphenoid/cribriform plate
T3: Tumor extending into the orbit or anterior cranial fossa
T4: Tumor involving the brain
Слайд 25Olfactory Neuroblastoma
Esthesioneuroblastoma
Aggressive behavior
Local failure: 50-75%
Metastatic disease develops in 20-30%
Treatment:
En bloc surgical resection
with postoperative XRT
Слайд 26Sarcomas
Osteogenic Sarcoma
Most common primary malignancy of bone.
Mandible > Maxilla
Sunray radiographic appearance
Fibrosarcoma
Chondrosarcoma
Слайд 27Rhabdomyosarcoma
Most common paranasal sinus malignancy in children
Non-orbital, parameningeal
Triple therapy is often necessary
Aggressive
chemo/XRT has improved survival from 51% to 81% in patients with cranial nerve deficits/skull/intracranial involvement.
Adults, Surgical resection with postoperative XRT for positive margins.
Слайд 28Lymphoma
Non-Hodgkins type
Treatment is by radiation, with or without chemotherapy
Survival drops to 10%
for recurrent lesions
Слайд 29Sinonasal Undifferentiated Carcinoma
Aggressive locally destructive lesion
Dependent on pathological differentiation from melanoma, lymphoma,
and olfactory neuroblastoma
Preoperative chemotherapy and radiation may offer improved survival
Слайд 30Metastatic Tumors
Renal cell carcinoma is the most common
Palliative treatment only
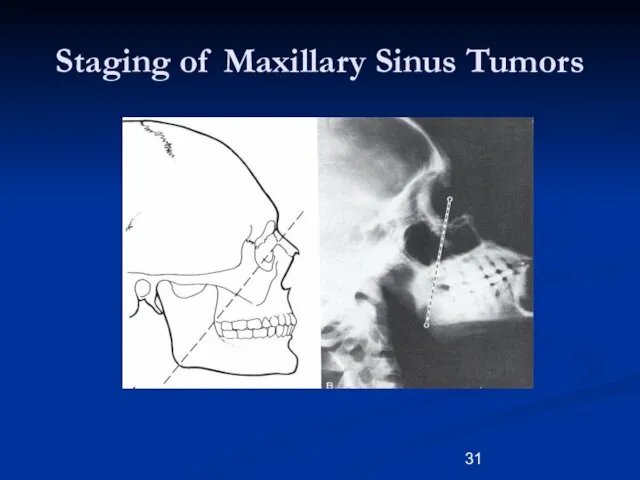
Слайд 31Staging of Maxillary Sinus Tumors
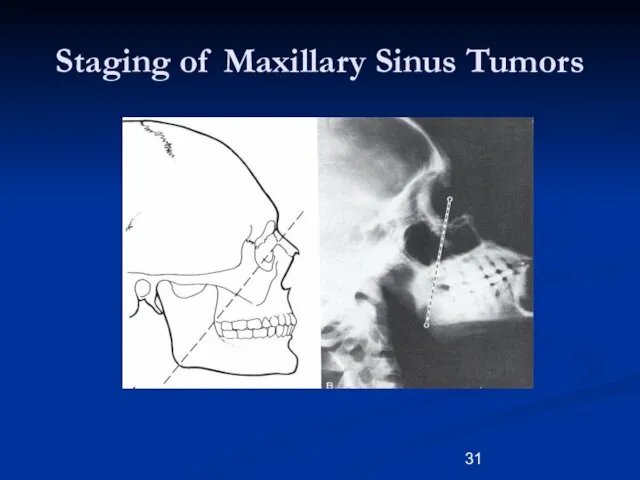
Слайд 32Staging of Maxillary Sinus Tumors
T1: limited to antral mucosa without bony erosion
T2:
erosion or destruction of the infrastructure, including the hard palate and/or middle meatus
T3: Tumor invades: skin of cheek, posterior wall of sinus, inferior or medial wall of orbit, anterior ethmoid sinus
T4: tumor invades orbital contents and/or: cribriform plate, post ethmoids or sphenoid, nasopharynx, soft palate, pterygopalatine or infratemporal fossa or base of skull
Слайд 33Surgery
Unresectable tumors:
Superior extension: frontal lobes
Lateral extension: cavernous sinus
Posterior extension: prevertebral fascia
Bilateral optic
nerve involvement
Слайд 34Surgery
Surgical approaches:
Endoscopic
Lateral rhinotomy
Transoral/transpalatal
Midfacial degloving
Weber-Fergusson
Combined craniofacial approach
Extent of resection
Medial maxillectomy
Inferior maxillectomy
Total maxillectomy
Слайд 35Tracheostomy
130 maxillectomies only 7.7% required tracheostomy
Of those not receiving tracheostomy during surgery,
only 0.9% experienced postoperative airway complications
Tracheostomy is unnecessary except in certain circumstances (bulky packing/flaps, mandibulectomy)
Слайд 36Treatment of the Orbit
Before 1970’s orbital exenteration was included in the radical
resection
Preoperative radiation reduced tumor load and allowed for orbital preservation with clear surgical margins
Currently, the debate is centered on what “degree” of orbital invasion is allowed.
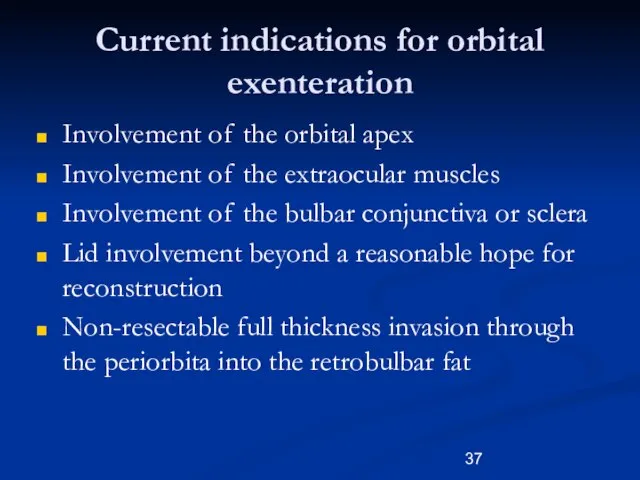
Слайд 37Current indications for orbital exenteration
Involvement of the orbital apex
Involvement of the extraocular
muscles
Involvement of the bulbar conjunctiva or sclera
Lid involvement beyond a reasonable hope for reconstruction
Non-resectable full thickness invasion through the periorbita into the retrobulbar fat
Слайд 38Conclusions
Neoplasms of the nose and paranasal sinus are very rare and require
a high index of suspicion for diagnosis
Most lesions present in advanced states and require multimodality therapy
 Определение процентного содержания вязкой составляющей в изломах ударных образцов, после испытаний при низких температурах
Определение процентного содержания вязкой составляющей в изломах ударных образцов, после испытаний при низких температурах ZF Aftermarket определяет мобильность будущего
ZF Aftermarket определяет мобильность будущего Тексты зрительных диктантов
Тексты зрительных диктантов Презентация на тему Формы организации учебно-познавательной деятельности на уроке
Презентация на тему Формы организации учебно-познавательной деятельности на уроке  Дома в Англии
Дома в Англии Архетипы
Архетипы Процедуры
Процедуры Требования к проекту
Требования к проекту Презентация "Струнно-смычковые" - скачать презентации по МХК
Презентация "Струнно-смычковые" - скачать презентации по МХК Гигиена и экология человека
Гигиена и экология человека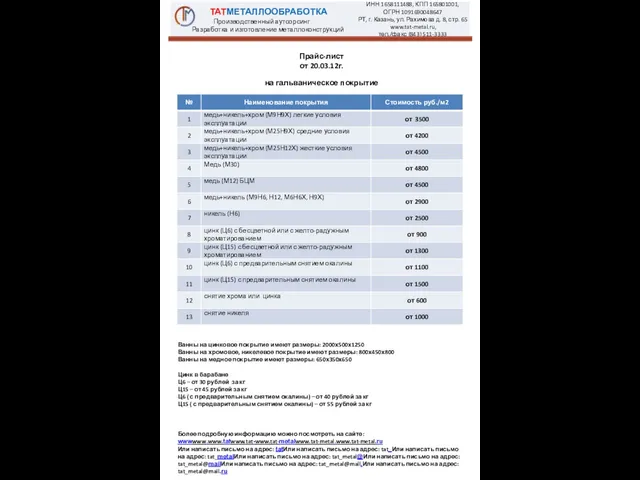 Прайс-лист от 20.03.12г. на гальваническое покрытие Ванны на цинковое покрытие имеют размеры: 2000х500х1250 Ванны на
Прайс-лист от 20.03.12г. на гальваническое покрытие Ванны на цинковое покрытие имеют размеры: 2000х500х1250 Ванны на  Презентация на тему Чарльз Дарвин и Эволюционное учение
Презентация на тему Чарльз Дарвин и Эволюционное учение  Основы логики - построение таблиц истинности
Основы логики - построение таблиц истинности Основы маркетинга
Основы маркетинга Сосновому бору – экологическую чистоту!
Сосновому бору – экологическую чистоту! Группа 1
Группа 1 Национальные директивы по фортификации муки Ибрахим Парванта Директор, Программа IMMPaCt Центр по Профилактике и Контролю за Заболе
Национальные директивы по фортификации муки Ибрахим Парванта Директор, Программа IMMPaCt Центр по Профилактике и Контролю за Заболе Конвенции о правах ребёнка!
Конвенции о правах ребёнка! Как празднуют Новый год в разных странах мира
Как празднуют Новый год в разных странах мира Опыт внедрения пилотных проектов по АСУДД в регионах и знаков обратной связи с водителями
Опыт внедрения пилотных проектов по АСУДД в регионах и знаков обратной связи с водителями Налогообложение на выбросы СО2
Налогообложение на выбросы СО2 Презентация на тему Химическое загрязнение окружающей среды
Презентация на тему Химическое загрязнение окружающей среды  П.И. Чайковский Опера "Черевички"
П.И. Чайковский Опера "Черевички" Построение экспликации помещений
Построение экспликации помещений Ниобий и тантал.Свойства элементов и их соединений
Ниобий и тантал.Свойства элементов и их соединений Классы неорганических веществ
Классы неорганических веществ Вовлечение волонтеров в оказание паллиативной помощи пациентам и их близким
Вовлечение волонтеров в оказание паллиативной помощи пациентам и их близким Общие контуры политической системы. Конституция Бразилии
Общие контуры политической системы. Конституция Бразилии