Слайд 2Labour is the expulsion of the fetus and placenta from the uterus
and is traditionally divided into three stages, unequal in length
Слайд 3Mechanism of labour
In humans, the cause of labour is unknown. The following
facts are accepted:
Oestrogens increase uterine muscle activity
whilst progesterone suppresses it.
• In late pregnancy the fetal adrenal glands produce much more dehydroepiandrosterone sulphate (DHEAS) which is converted by the placenta into oestrogen. This encourages uterine
contractions.
Слайд 4Mechanism of labour
• The decidua releases prostaglandins (PGs), mainly PGE2 and PGF2a.
Such PGs cause minor uterine contractions which result in further hypoxia of the decidua and so further PG production.
• The final common pathway for a contraction
is an increase in the cytosol-free calcium which
causes a joining together of actin and myosin.
This is common to all involuntary muscle contractions.
Слайд 5Mechanism of labour
• Oxytocin, released from the posterior pituitary, cannot be detected
in the blood in early normal labour. The release of oxytocin is dependent upon a monosynaptic reflex, initiated when the presenting part presses on the pelvic floor
Слайд 6Uterine action
The fetus is propelled down the birth canal by the action
of the myometrium. Normal uterine activity is fundally dominant, so waves of contraction pass down from each cornu to the lower uterine segment.
Слайд 7Uterine action
During labour, contractions increase in frequency
and strength. Contractions are painful
and this
may be due to:
• Hypoxia because of the duration of the
contraction.
• Compression of the nerve endings in the
myometrium.
• Cervical stretch and dilatation.
Слайд 8Uterine action
Labour starts with contractions about one in
every 10 minutes increasing
to one in every
2–3 minutes. The upper uterine segment contracts and retracts so that the lower segment and later, the cervix, is pulled over the baby’s head rather like putting on a tight polo-neck sweater.
Слайд 9Stages
1 The first stage, dilatation —from the onset of labour until the
cervix is fully dilated. More recently it has been divided into two phases:
• The latent phase of effacement of the cervix:
to 3cm dilation.
• The active phase of active cervical dilatation:
from 3cm to full dilation.
2 The second stage, expulsive —from full cervical
dilatation to birth of the baby.
3 The third stage, placental —from birth of the baby
to the delivery of the placenta.
Слайд 10The uterus in the first stage
1 Uterine muscle fibres contract and retract,
so they do not return to their original length after contraction but remain shorter.
2 There is a heaping up and thickening of the upper uterine segment while the lower uterine segment becomes thinner and stretched.
3 The cervix is pulled up and the canal is effaced so its length diminishes.
4 The cervix is pulled up and open and so the os is dilated.
Слайд 11The uterus in the second stage
1 A diminution in the transverse diameters
because of:
• Pulling up of the lower segment.
• Straightening out of the fetus.
2 The fetal head is forced into the upper vagina which now forms a continuous tube with the uterus and a fully effaced cervix.
3 As well as uterine contractions, expulsive efforts are made by the mother using:
• The abdominal wall muscles.
• The fixed diaphragm, thus raising intra-abdominal pressure.
4 Voluntary efforts are not essential; paraplegic women and those with epidural analgesia have normal deliveries. Pushing is instinctive, and very satisfying to the woman who then assists at her own delivery.
Слайд 12The uterus in the third stage
1 The uterine muscles contract so constricting
the
blood vessels passing between the fibres, and thus
preventing excessive bleeding.
2 The placenta separates at the delivery of the
fetus when the uterus contracts sharply in size. Haemostasis is mostly mechanical immediately after delivery, with muscle fibres kinking bloodvessels. During pregnancy and most of the labour the placental bed and the placenta are roughly the same size. With the fetus removed, the area of the placental bed is reduced to about half that of the placenta
Слайд 13The uterus in the third stage
The placenta is therefore sheared off and
is finally expelled from the uterus by contractions passing down into the lower segment.
The signs of descent of the placenta in the uterus
are:
• The uterus becomes hard.
• The umbilical cord lengthens.
• There is a show of blood.
Слайд 14Diagnosis of labour
The onset of labour is defined as regular painful uterine
contractions that cause cervical change. By definition it is often a retrospective diagnosis
Слайд 15First stage of labour
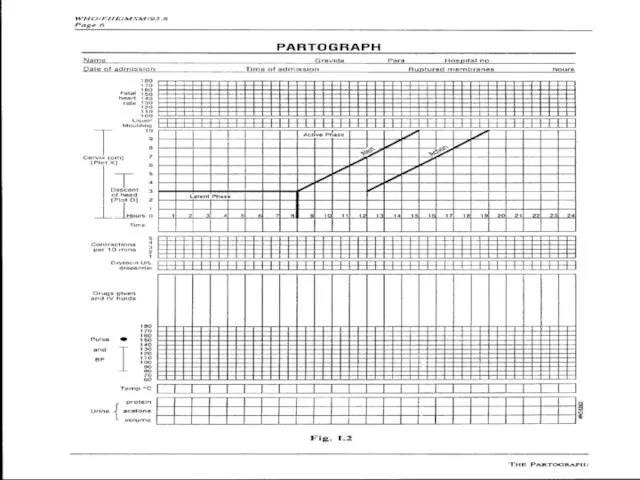
Progress in labour is monitored by descent of the
fetal head together with dilatation of the cervix. As little or nothing is known about the rate of cervical dilatation prior to admission to the labour ward,the partogram is started on admission.The partogram used by most maternity units, is an easy, graphical method of assessing the progress of labour and helps facilitate handover between midwives. It contains the following information:
Слайд 161 High-risk factors—obstetric, paediatric or anaesthetic.
2 A record of the fetal heart
rate. Higher risk
women have continuous electronic fetal heart rate monitoring (EFM) by the cardiotocograph. Lowrisk women usually have the fetal heart rate measured with a Pinard’s stethoscope every 15 minutes, immediately following contractions. These records are plotted on the partogram.
Слайд 173 The cervicogram: graphical record of the rate of cervical dilatation.
4 Descent
of fetal head.
5 Frequency, duration and strength of uterine contractions are recorded.
6 If membranes are ruptured, the amniotic fluid colour.
7 The volume of maternal urine that is produced, tested for ketones and protein.
8 A record of the drugs given, in particular analgesics.
9 Maternal blood pressure, pulse and temperature
Слайд 18After the first examination the following should be plotted:
1 The amount of
the fetal head that can be palpated per abdomen in terms of fifths of the head descent.
2 The cervical dilatation (1cm/hour beyond 3cm).
Слайд 193 A line of expected cervical dilatation should then also be plotted.
The WHO have produced an international partogram with two parallel straight lines plotted at 1cm/hour. The first line represents the expected progress of a normal labour. If cervical dilatation falls below the first line and reaches/crosses the action line then an artificial rupture of the membranes (ARM) should be performed. If progress after 2 hours is not parallel to the action line then syntocinon should be started to make the contractions stronger and more frequent. Labour should then follow the action line, if it does not then a Caesarean section is indicated.
Слайд 20The level of descent of the presenting part should be checked and
plotted every hour, whilst vaginal examinations may be performed every 4 hours. As long as the rate of cervical dilatation stays on or to the left of the nomogram, labour progress is considered to be normal.
Слайд 22A partogram used to assess the progress of labour. The lines in
the cervical dilated section are the expected patterns of cervical dilatation in labour showing a slow latent phase and faster active phase. If dilatation crosses the action line then the patient should be reviewed and syntocinon infusion started to accelerate labour.
Слайд 23Care of the patient
• The woman should not be left alone during
labour. Ideally there should be a midwife present with her throughout. In addition, many women choose to have their partner, companion or relative present.
• Analgesia should be given sufficient for the woman’s need.
• She should be encouraged to pass urine frequently.
• Light snacks, soup or cool fluids are offered
Слайд 24Бажано забезпечити
співвідношення
одна роділля –
одна акушерка

Слайд 26Second stage of labour
1 During the expulsive stage, the woman is encouraged
to push with uterine contractions. If she is sitting propped up, this is done, by taking a deep breath and holding it, putting her chin on her chest, and pulling on the backs of her knees.Women usually achieve two or three expulsive pushes during each uterine contraction.
Слайд 27Second stage of labour
2 Monitoring progress in the second stage of labour
is by vaginal assessment of the lowest part of the presenting pole related to the ischeal spines. This applies until the presenting part becomes visible.
3 When the head is delivered, it is allowed to rotate (restitute) and then lateral traction is applied in the direction of the mother’s anus which allows the birth of the fetal anterior shoulder.
4 Now give 2.0mg of Syntometrine intramuscularly (i.m.) to aid delivery of the placenta.
5 The baby’s head is raised towards the mother’s abdomen so the posterior shoulder passes over the perineum and the rest of the baby usually then slips out.
Слайд 28Second stage of labour
6 The baby’s mouth and nasal passages are usually
sucked free of mucus with a mechanical mucus extractor. The mouth should be cleared before the nose as aspirating the nose often causes the baby to inhale.
7 The umbilical cord is clamped twice, and divided between the clamps. In developed countries, hospital units now use disposable plastic umbilical clamps, although Spencer Wells forceps suffice.
8 The baby usually starts breathing within 1 minute of delivery. The baby may be given to the mother immediately if she so wishes but should be wrapped in a prewarmed blanket first
Слайд 30Third stage of labour
1 Syntometrine has been given with the delivery. Signs
of placental separation are now no longer awaited before applying controlled cord traction.
2 The operator’s left hand is placed above the symphysis pubis and guards the front wall of the uterus to prevent uterine inversion.
3 The umbilical cord is grasped in the operator’s right hand and steady traction is applied until the placenta is delivered down into the vagina and
into a kidney dish.
Слайд 31Third stage of labour
4 The membranes usually follow the placenta andcan be
removed by gentle rotation of the placenta helping them to peel off the uterus.
5 The placenta and membranes are checked for
completeness.
6 Blood loss should be estimated; it is normal – 0.5% of mass body.
Слайд 32Pain relief in labour
• Labour is usually painful. Relief of pain is
better
given before the woman feels the pain of the
contractions.
• Careful timing of analgesia is as important as
correct dosage.
Слайд 33Nitrous oxide
This is self-administered, pre-mixed with O2 (50%of each), in Entonox machines.
Inhalation should start as each contraction is felt and before the woman feels pain (Fig. 12.8) for it takes some seconds to work.
Слайд 34Pethidine
Pethidine has been used for many years as an analgesic in labour.
Many units have now withdrawn it because of evidence that it is a poor analgesic and can have a prolonged depressant effect on neonatal respiratory effort.
• Synthetic analgesic and antispasmodic.
• Dose: 50–150mg i.m.; 50–100mg i.v. (slowly, for it can cause nausea).
• Use in first stage. Try to avoid giving within 2 hours of expected delivery if possible because of depression of neonatal respiration.
• Can cause drop of maternal blood pressure.
• Causes nausea in 20%. Give anti-emetic.
Слайд 35Non-drug analgesia
Increasing numbers of women are turning to nonpharmacological methods of pain
relief. Pain is such a subjective symptom that anything which helps a woman and does not put her or her fetus at increased risk should be explored. Maybe these methods cause the release of endorphins and so postpone the need for more formal analgesia; this reduces the total dose, giving the woman a greater sense of self-participation.
Слайд 36Relaxation
The woman should take training in pregnancy. The method works best
if there is a sympathetic attendant to guide in labour (e.g. partner). It is safe for mother and fetus.
Hypnosis
If both woman and attendant are trained, this can give good pain relief. It is expensive on attendant’s time and only works for susceptible women. If it works, it is very safe for the fetus.
Слайд 37Acupuncture
Some women opt for acupuncture in labour. The effects are very variable
from one person to another and the need for several needles in variouspoints of the body limits mobilization which many women find unacceptable.
Слайд 38Transcutaneous nerve stimulation (TENS)
Small pulses of electrical vibration to the muscles of
the back, from a portable battery-driven pack, provide distraction therapy. Some find it helpful in the early stages of labour. Even though it might not work for full labour, it could postpone the need for a stronger, more depressant, analgesia and so its use should be encouraged if women want to try it. However, labour ward staff must know how to work the machines and be sympathetic to their use.
Слайд 39Anaesthesia
Depression of the central or peripheral nervous system to prevent transmission and
reception of painful impulses.
General anaesthesia is useful for operations such as an emergency Caesarean section when speed is essential.
Слайд 40Regional
Nerve roots are blocked at their outflow.
Spinal block
• Heavy nupivercaine
into subarachnoid space.
• Give at L3–4, put woman in head-up position.
• Blocks T11–S1.
• Used once only usually for operative delivery
(e.g. Caesarean section).
Слайд 41Epidural block
• Bupivacaine 1% or Marcain 0.25–0.5% through a cannula inserted into
peridural fat. Affects nerve roots T11–S4.
• Pain relief rapid, lasting 2–3 hours.
• Repeated doses can be given; therefore used for pain relief in labour.
• Requires expert anaesthetist .
• Loss of sensation from the uterus means the woman needs help in the second stage to recognize uterine contractions.
• Using a constant infusion of bupivacaine with fentanyl reduces the density of the block and allows some mobilization for the woman (walking epidural).
Слайд 42Complications
• A serious complication of the epidural block is puncture of the
dura and so unwittingly performing a spinal anaesthetic with a big needle. This could lead to nerve blockage and stopping respiration if the anaesthetic agent flows up into the thoracic region. Such a complication is watched for carefully by an experienced anaesthetist; it occurs in 1 : 500 cases.
• A rarer complication is infection which might enter through the skin to the peridural area.
Слайд 43Caudal block
• Localized epidural through sacral hiatus.
• Gives good anaesthesia for operative
deliveries but only 80% effective.
Слайд 44Local
Pudendal
• Block pudendal nerve with Xylocaine 0.5 or 1%
as its two or
three branches circumnavigate the
ischial spine; given either through vagina or
through perineal skin. Numbs the area on the right
only as shown in Fig. 12.10, and therefore needs a
field block as well.
• Used for outlet manipulations in the second
stage of labour, e.g. easy forceps delivery
Слайд 45Field block
A local infiltration of the nerve endings in the vulva and
labia:
• Prior to episiotomy or its repair.
• As an adjunct to pudendal block.
Proper analgesia and anaesthesia in labour work best when the woman and her partner have been instructed antenatally and have had a chance to learn about the methods available. She should talk to other women who have benefited by analgesia. All this is then applied by sympathetic attendants who look to the needs of the individual woman and tailor the therapy to her needs, preferably preventing pain being felt rather than trying to remove it after it has arrived.


 Ислам. Тест
Ислам. Тест Концепция структурных преобразований радиоэлектронной промышленности оборонно-промышленного комплекса
Концепция структурных преобразований радиоэлектронной промышленности оборонно-промышленного комплекса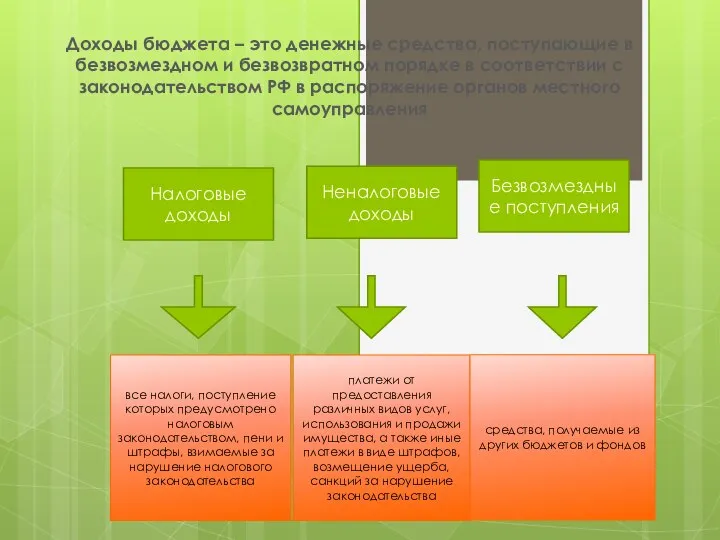 Доходы бюджета Чугунаевского сельского поселения
Доходы бюджета Чугунаевского сельского поселения Деды Морозы в разных странах
Деды Морозы в разных странах Презентация на тему Дорожное движение, безопасность участников дорожного движения (5 класс)
Презентация на тему Дорожное движение, безопасность участников дорожного движения (5 класс) Конкурсная программа «Мы должны быть бережливыми!»
Конкурсная программа «Мы должны быть бережливыми!» Галерея помещиков Мёртвые души
Галерея помещиков Мёртвые души Искусство второй половины XX века.Ташизм, абстрактный экспрессионизм
Искусство второй половины XX века.Ташизм, абстрактный экспрессионизм Производство ферментных препаратов
Производство ферментных препаратов  Общая физическая подготовка
Общая физическая подготовка Придаточные предложения места
Придаточные предложения места Main changes Tudors
Main changes Tudors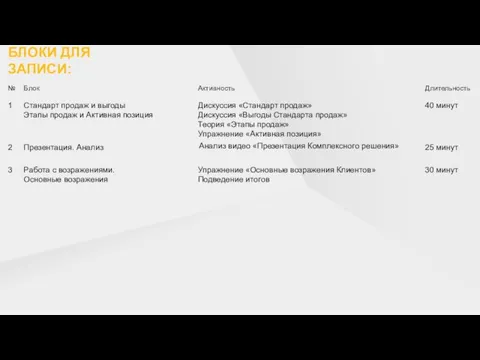 Сертификация (ап)
Сертификация (ап) Презентация к уроку русского языка в 6 классе по теме Прилагательное как часть речи Составитель: Падалко Татьяна Викторовна
Презентация к уроку русского языка в 6 классе по теме Прилагательное как часть речи Составитель: Падалко Татьяна Викторовна  Презентация на тему Характер
Презентация на тему Характер Организация и нормативно-правовое обеспечение государственной (итоговой) аттестации выпускников 9-х классов в 2009-2010 учебном
Организация и нормативно-правовое обеспечение государственной (итоговой) аттестации выпускников 9-х классов в 2009-2010 учебном  Александр Сергеевич Пушкин
Александр Сергеевич Пушкин Ответственность директоров и контролирующего лица
Ответственность директоров и контролирующего лица Организация внеурочной деятельности при реализации федерального государственного образовательного стандарта начального общего
Организация внеурочной деятельности при реализации федерального государственного образовательного стандарта начального общего Презентация на тему Загадки с подвохом
Презентация на тему Загадки с подвохом Век XVIII в истории России
Век XVIII в истории России Законы и нормативно-правовые акты по организации безопасности по условиям РСЧС
Законы и нормативно-правовые акты по организации безопасности по условиям РСЧС БОРТОВАЯ АНАЛИТИЧЕСКАЯ СИСТЕМА УПРАВЛЕНИЯ РИСКАМИ ПОЛЕТА САМОЛЕТА
БОРТОВАЯ АНАЛИТИЧЕСКАЯ СИСТЕМА УПРАВЛЕНИЯ РИСКАМИ ПОЛЕТА САМОЛЕТА ИМИДЖ КАК ФАКТОР КОНКУРЕНТОСПОСОБНОСТИ ВЫСШЕГО УЧЕБНОГО ЗАВЕДЕНИЯ
ИМИДЖ КАК ФАКТОР КОНКУРЕНТОСПОСОБНОСТИ ВЫСШЕГО УЧЕБНОГО ЗАВЕДЕНИЯ Формы ДНК
Формы ДНК Инфекционный перитонит кошек
Инфекционный перитонит кошек Правила выплат нуждающимся в поддержке семьям на детей от 3 до 7 лет
Правила выплат нуждающимся в поддержке семьям на детей от 3 до 7 лет S-Иерархия и атрибуты маршрутов
S-Иерархия и атрибуты маршрутов