Содержание
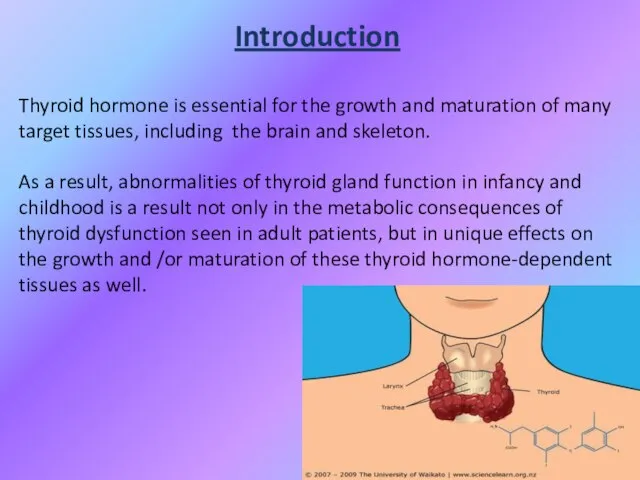
- 3. Introduction Thyroid hormone is essential for the growth and maturation of many target tissues, including the
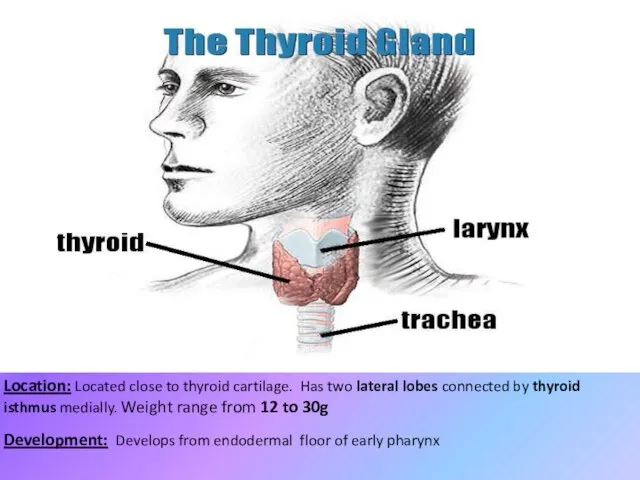
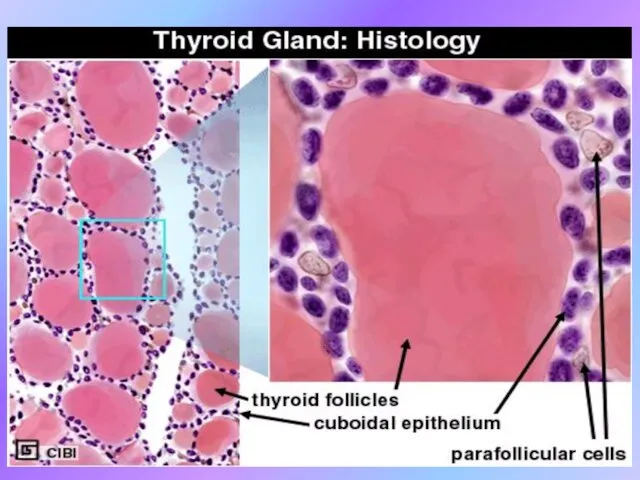
- 4. Location: Located close to thyroid cartilage. Has two lateral lobes connected by thyroid isthmus medially. Weight
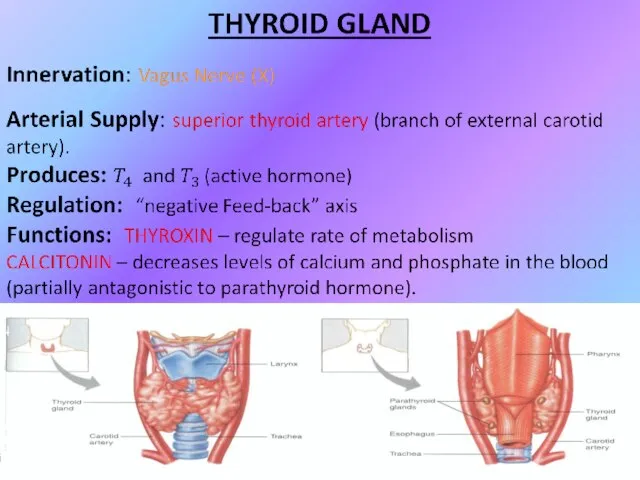
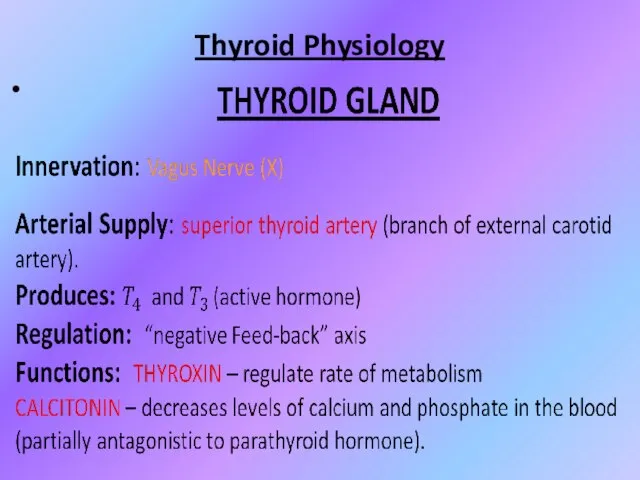
- 7. Thyroid Physiology
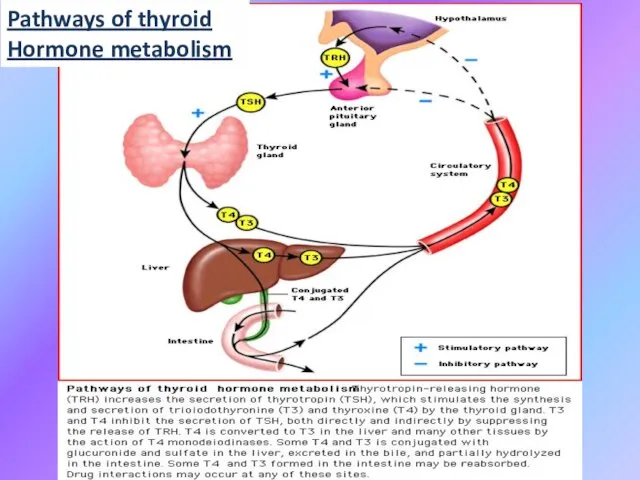
- 8. Pathways of thyroid Hormone metabolism
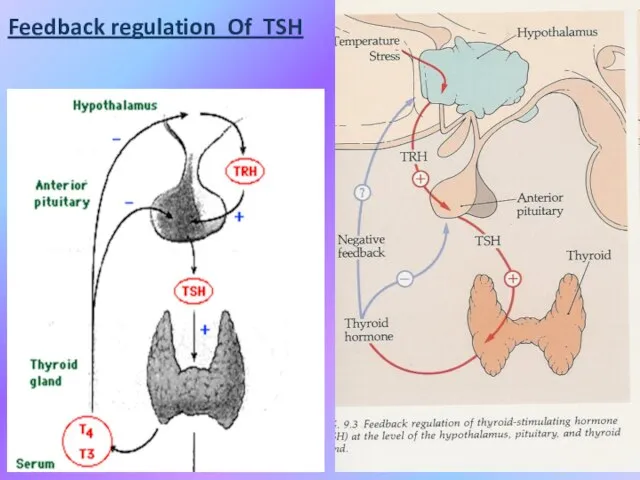
- 9. Feedback regulation Of TSH
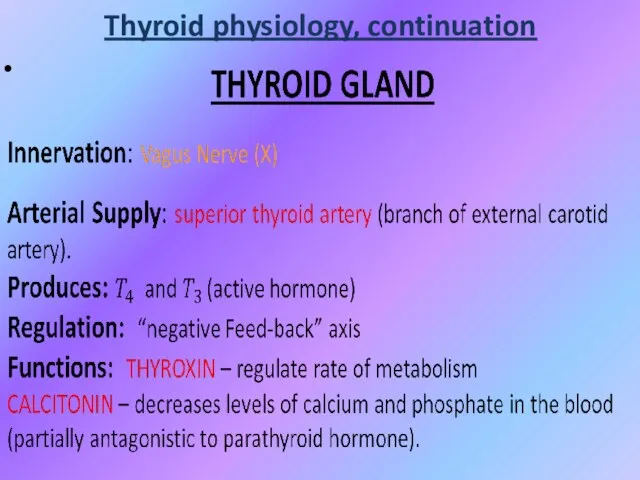
- 10. Thyroid physiology, continuation
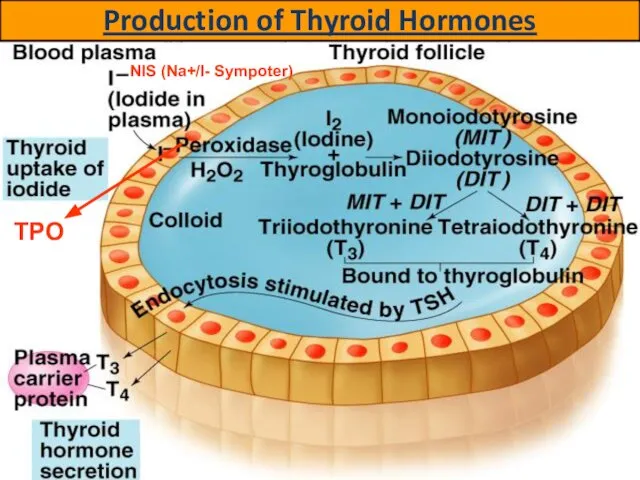
- 11. Production of Thyroid Hormones NIS (Na+/I- Sympoter) TPO
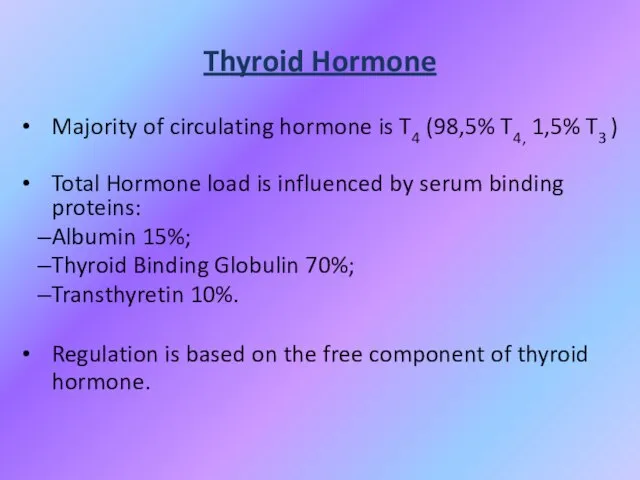
- 12. Thyroid Hormone Majority of circulating hormone is T4 (98,5% T4, 1,5% T3 ) Total Hormone load
- 13. Effects of thyroid hormones Fetal brain and skeletal maturation; Increase in basal metabolic rate; Inotropic and
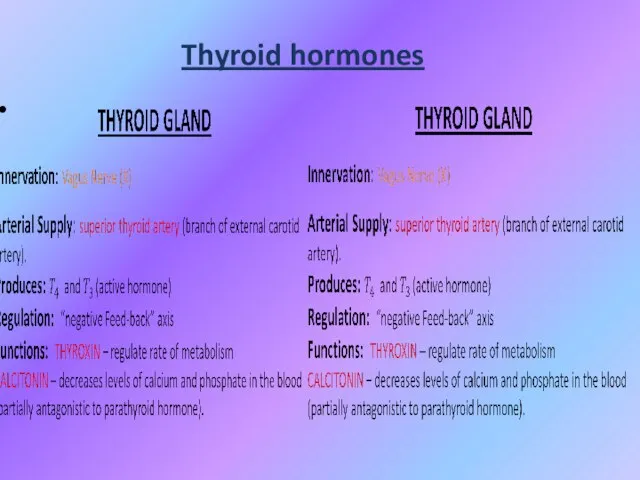
- 14. Thyroid hormones
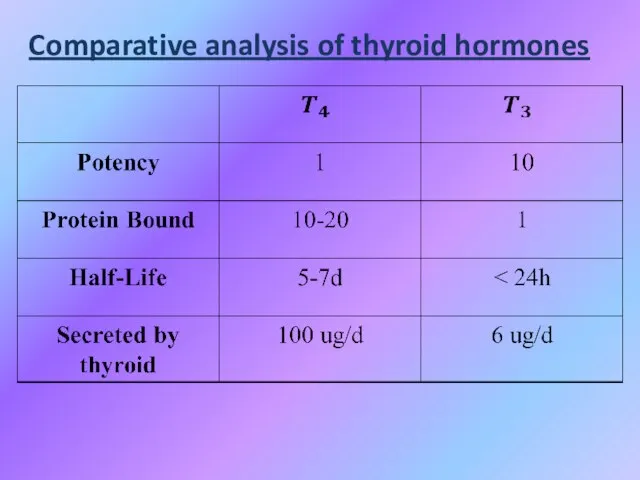
- 15. Comparative analysis of thyroid hormones
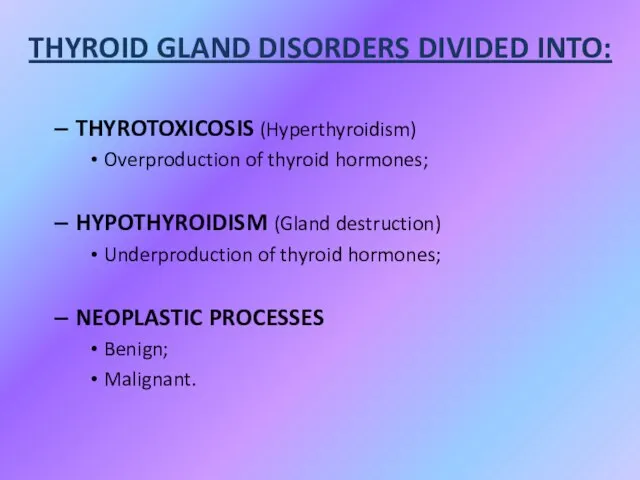
- 16. THYROTOXICOSIS (Hyperthyroidism) Overproduction of thyroid hormones; HYPOTHYROIDISM (Gland destruction) Underproduction of thyroid hormones; NEOPLASTIC PROCESSES Benign;
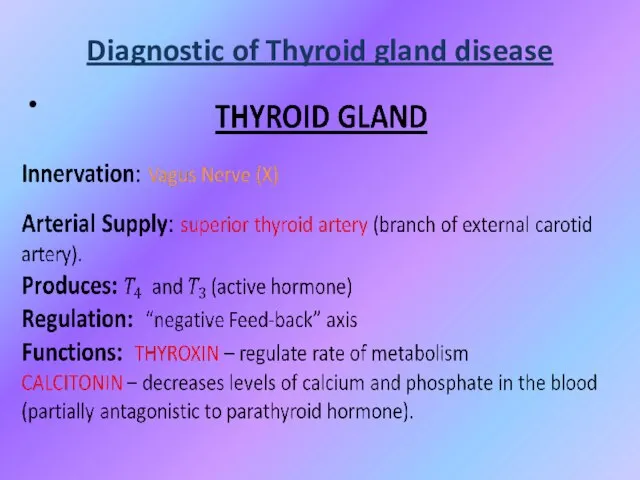
- 17. Diagnostic of Thyroid gland disease
- 18. LABORATORY EVALUATION TSH (thyroid-stimulating hormone) normal, practically excludes abnormality
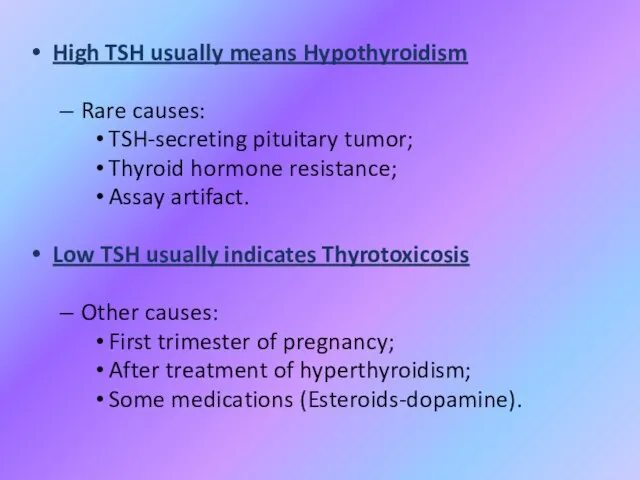
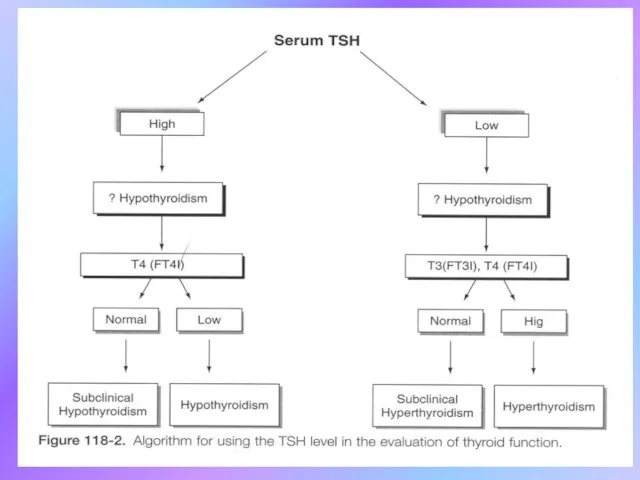
- 19. High TSH usually means Hypothyroidism Rare causes: TSH-secreting pituitary tumor; Thyroid hormone resistance; Assay artifact. Low
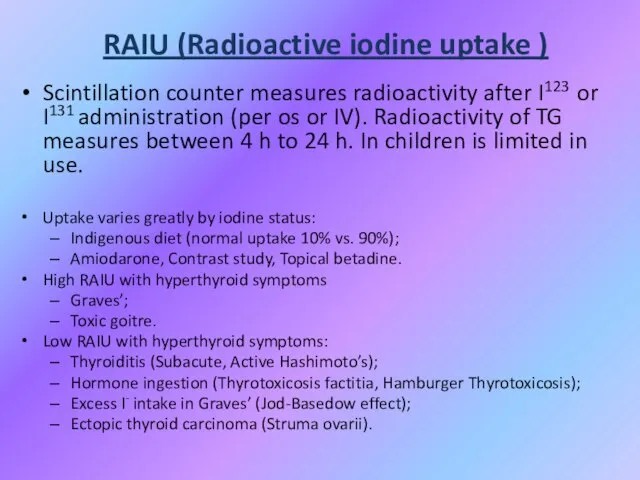
- 21. RAIU (Radioactive iodine uptake ) Scintillation counter measures radioactivity after I123 or I131 administration (per os
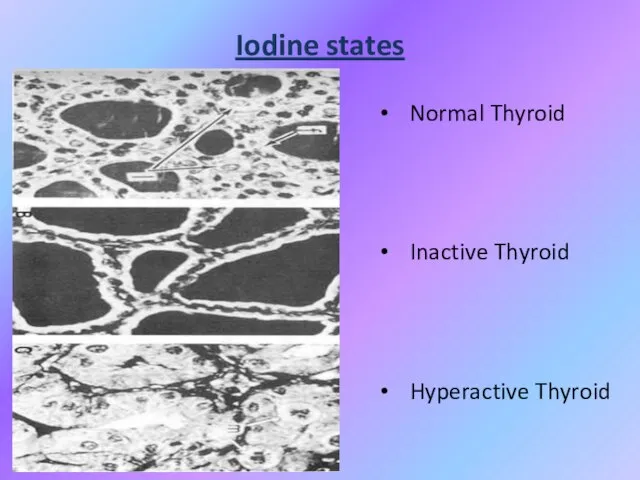
- 22. Iodine states Normal Thyroid Inactive Thyroid Hyperactive Thyroid
- 23. Thyrotoxicosis Primary; Secondary; Without Hyperthyroidism; Exogenous or factitious. Hypothyroidism Primary; Secondary; Peripheral.
- 24. HYPERTHYROIDISM or THYROTOXICOSIS: - is the result of excessive thyroid gland function because is defined as
- 25. Primary Hyperthyroidism: Graves’; Toxic Multinodular Goitre; Toxic adenoma; Functioning thyroid carcinoma metastases; Activating mutation of TSH
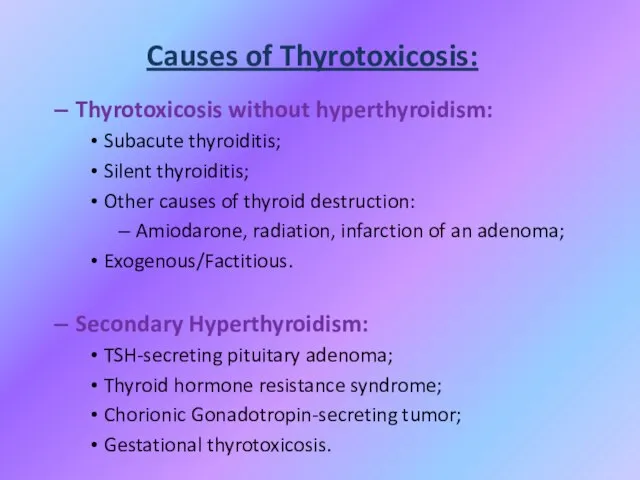
- 26. Causes of Thyrotoxicosis: Thyrotoxicosis without hyperthyroidism: Subacute thyroiditis; Silent thyroiditis; Other causes of thyroid destruction: Amiodarone,
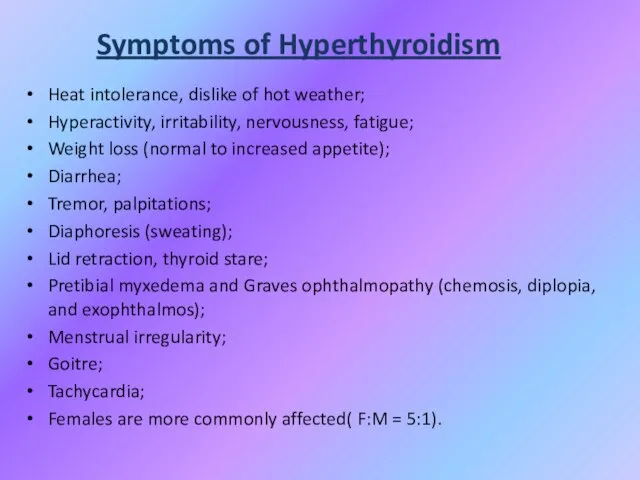
- 27. Symptoms of Hyperthyroidism Heat intolerance, dislike of hot weather; Hyperactivity, irritability, nervousness, fatigue; Weight loss (normal
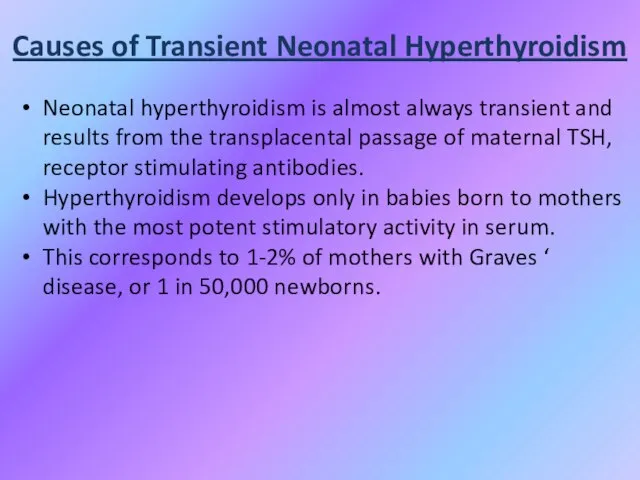
- 28. Causes of Transient Neonatal Hyperthyroidism Neonatal hyperthyroidism is almost always transient and results from the transplacental
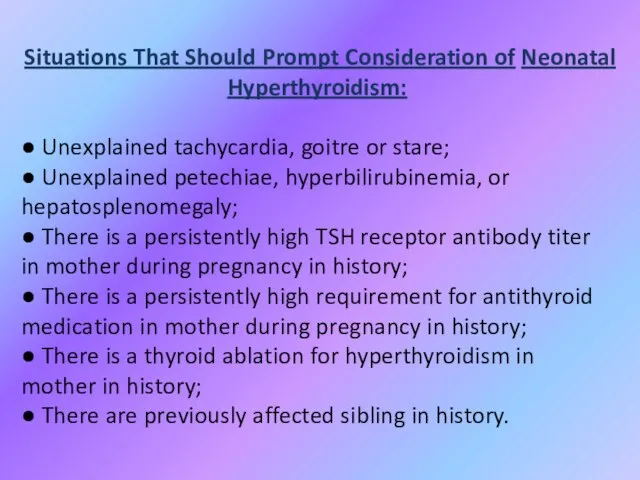
- 29. Situations That Should Prompt Consideration of Neonatal Hyperthyroidism: ● Unexplained tachycardia, goitre or stare; ● Unexplained
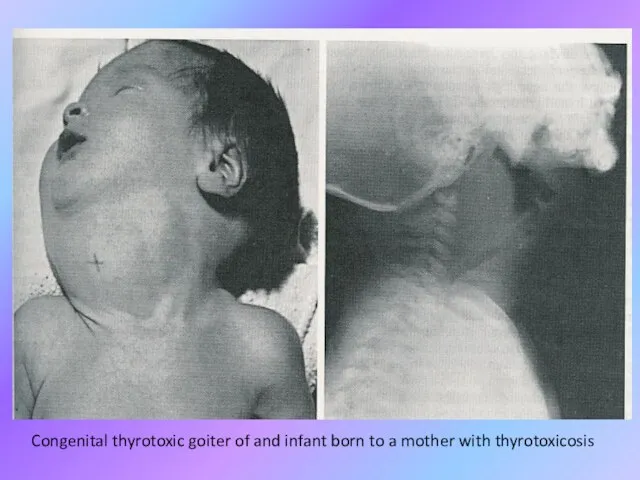
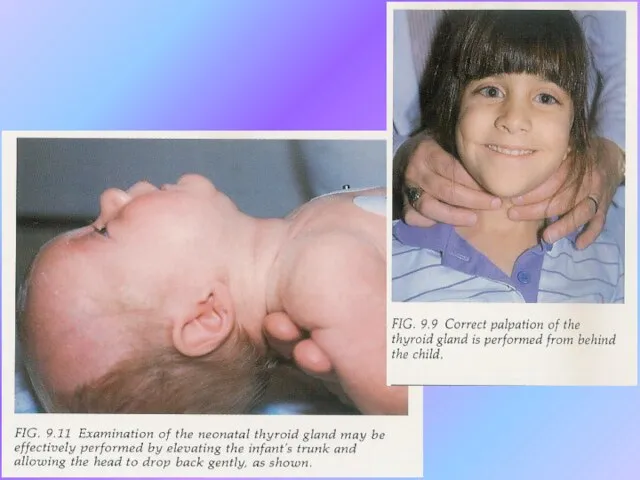
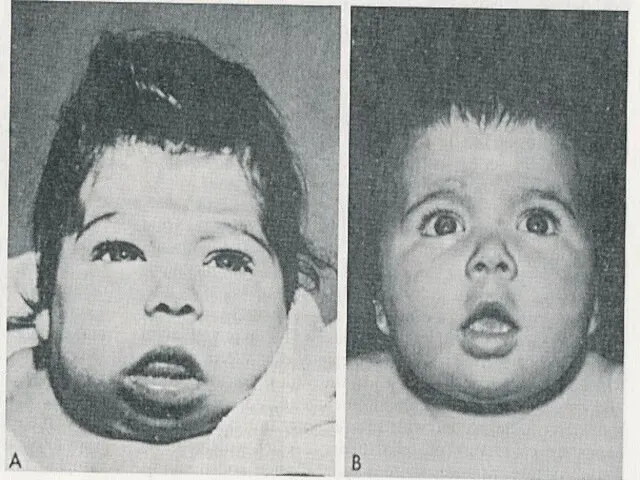
- 30. Congenital thyrotoxic goiter of and infant born to a mother with thyrotoxicosis
- 31. Therapy of Transient neonatal hyperthyroidism Treatment is accomplished by maternal administration of antithyroid medication in fetus.
- 32. Therapy of Transient neonatal hyperthyroidism In the neonate, treatment is the follows: either PTU (5 to10
- 33. Therapy of Transient neonatal hyperthyroidism Propranolol (2 mg/kg/day in 2 or 3 divided doses) is added
- 34. Permanent neonatal hyperthyroidism Rarely, neonatal hyperthyroidism is inconvertible and is due to a germline mutation in
- 35. Permanent neonatal hyperthyroidism Early recognition is important because the thyroid function of affected infants is frequently
- 37. Goitre Endemic goitre: Areas where > 5% of children 6-12 years old have goiter Common in
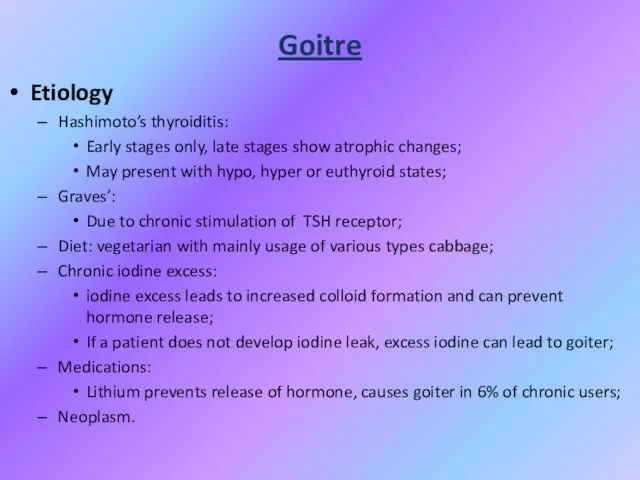
- 38. Goitre Etiology Hashimoto’s thyroiditis: Early stages only, late stages show atrophic changes; May present with hypo,
- 39. Goitre
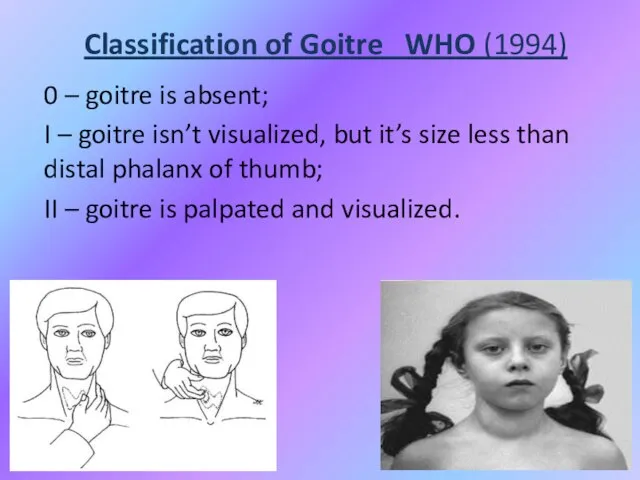
- 40. Classification of Goitre WHO (1994) 0 – goitre is absent; I – goitre isn’t visualized, but
- 41. Functional condition of Thyroid influence may be as Euthyroidism; Hypothyroidism; Hyperthyroidism.
- 42. Non-Toxic Goitre Cancer screening in non-toxic MNG (Multinodular goitre ) Longstanding MNG has a risk of
- 43. Non-Toxic Goitre Treatment options (no compressive symptoms): Use follow-up to monitor for progression; Thyroid suppression therapy:
- 44. Non-Toxic Goitre Treatment options (compressive symptoms): Radioactive iodine (RAI) ablation: Volume reduction 33% - 66% in
- 45. Toxic Goitre Treatment for Toxic MNG: Thionamide medications: Not indicated for long-term use due to complications;
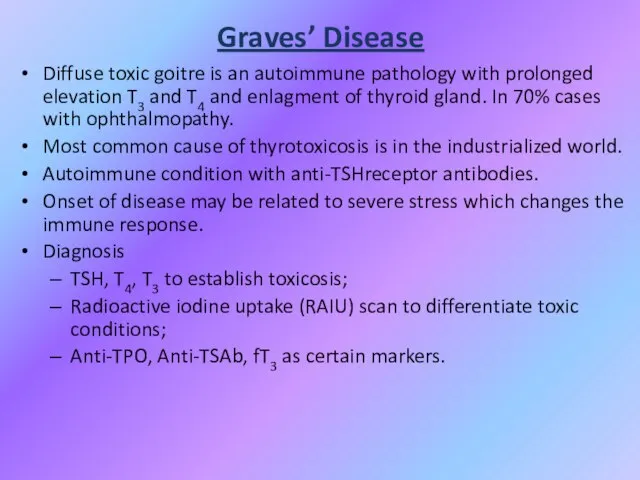
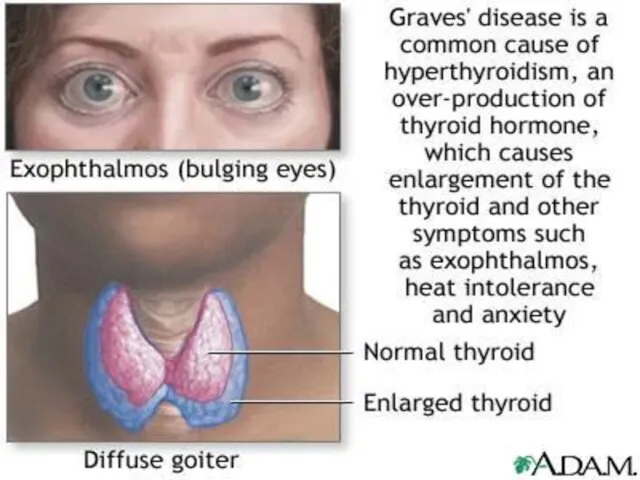
- 46. Graves’ Disease Diffuse toxic goitre is an autoimmune pathology with prolonged elevation T3 and T4 and
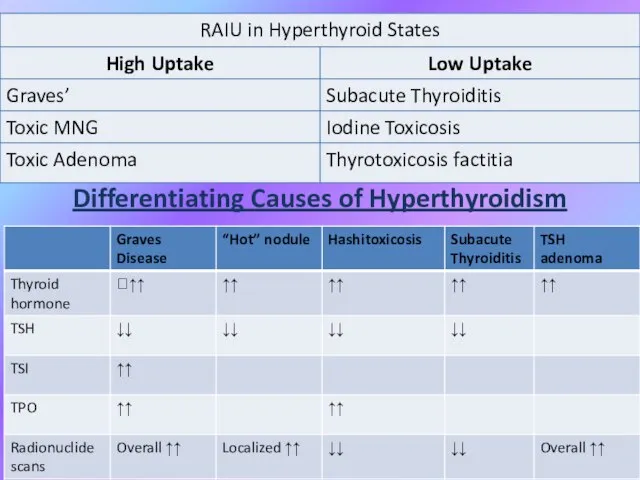
- 48. Differentiating Causes of Hyperthyroidism
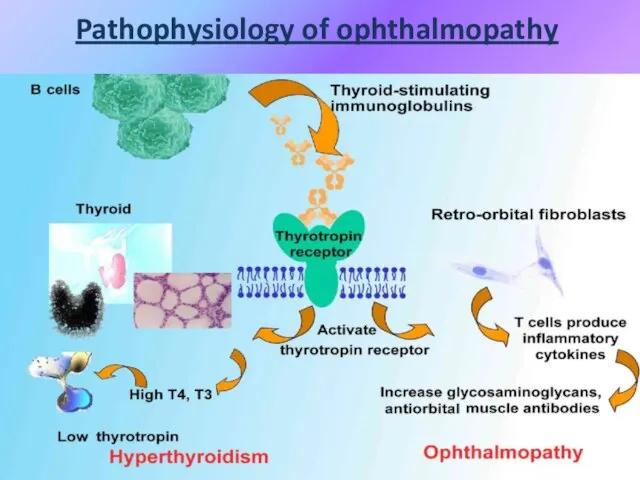
- 49. Pathophysiology of ophthalmopathy
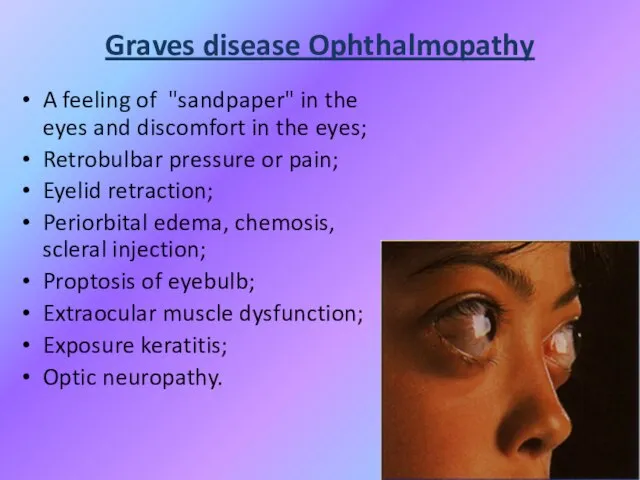
- 50. Graves disease Ophthalmopathy A feeling of "sandpaper" in the eyes and discomfort in the eyes; Retrobulbar
- 51. Graves Disease: Treatment • Medications: – Beta-blockers for symptoms – can be discontinued as thyroid function
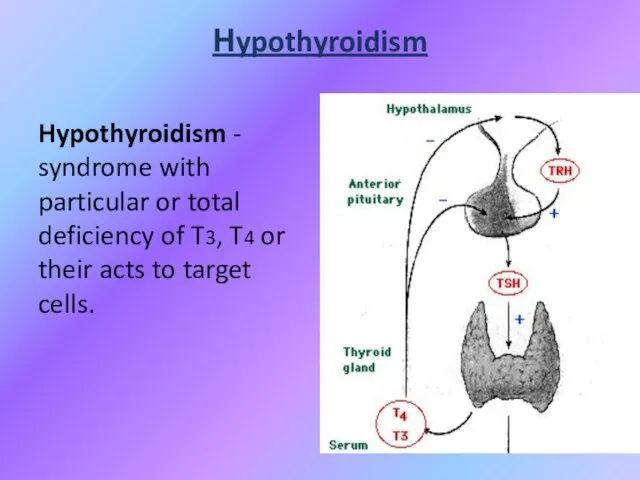
- 52. Нypothyroidism Hypothyroidism - syndrome with particular or total deficiency of T3, T4 or their acts to
- 53. Classification of hypothyroidism PRIMARY - defects of biosynthesis of T3, T4 due to pathology of thyroid
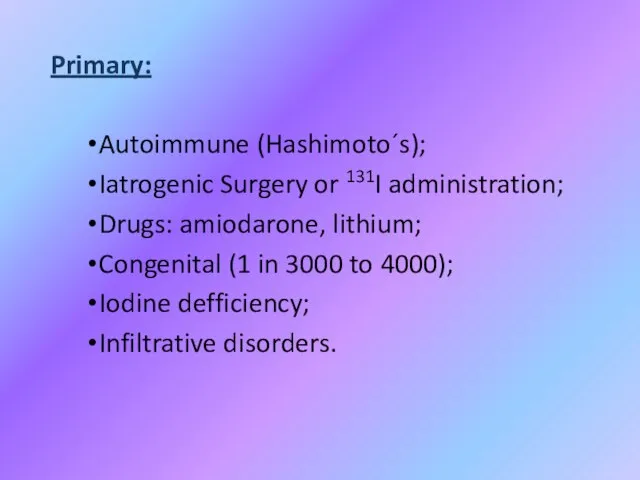
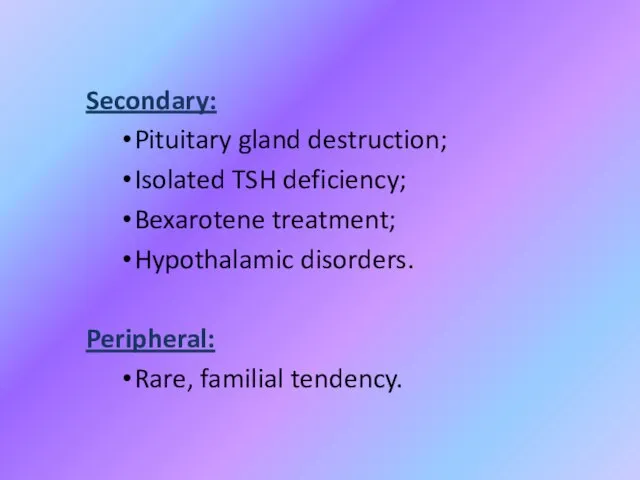
- 54. Primary: Autoimmune (Hashimoto´s); Iatrogenic Surgery or 131I administration; Drugs: amiodarone, lithium; Congenital (1 in 3000 to
- 55. Secondary: Pituitary gland destruction; Isolated TSH deficiency; Bexarotene treatment; Hypothalamic disorders. Peripheral: Rare, familial tendency.
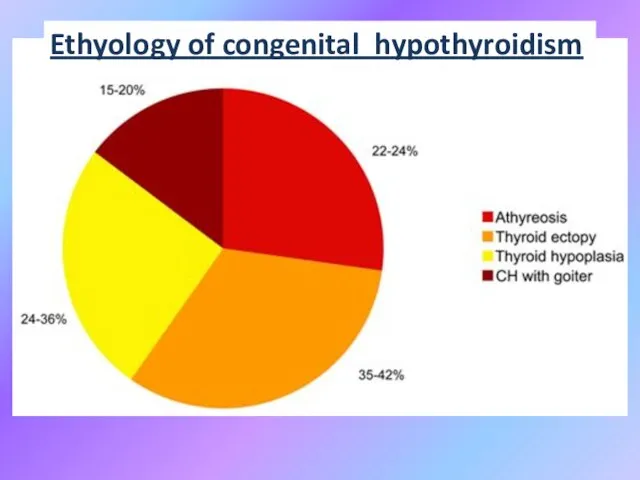
- 56. Ethyology of congenital hypothyroidism
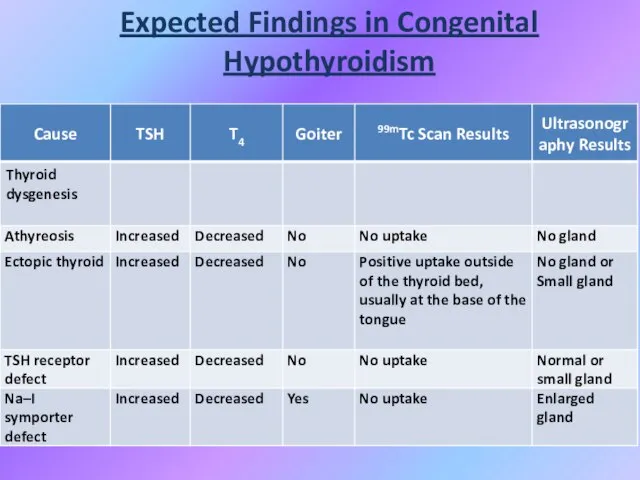
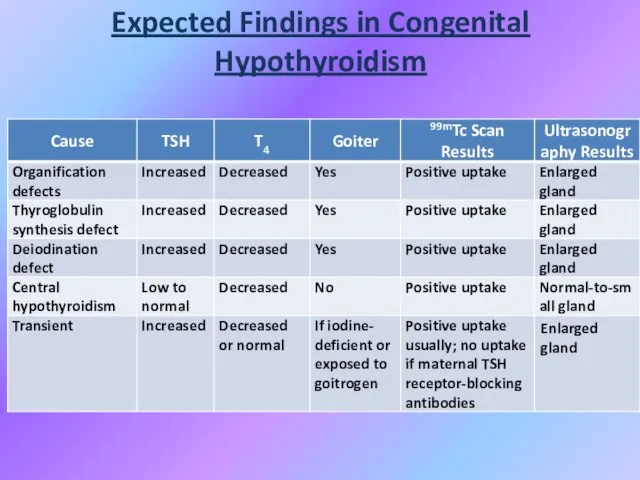
- 57. Expected Findings in Congenital Hypothyroidism
- 58. Expected Findings in Congenital Hypothyroidism
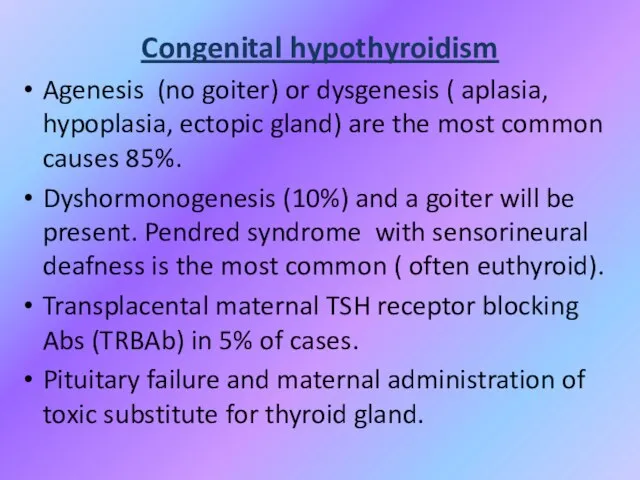
- 59. Congenital hypothyroidism Agenesis (no goiter) or dysgenesis ( aplasia, hypoplasia, ectopic gland) are the most common
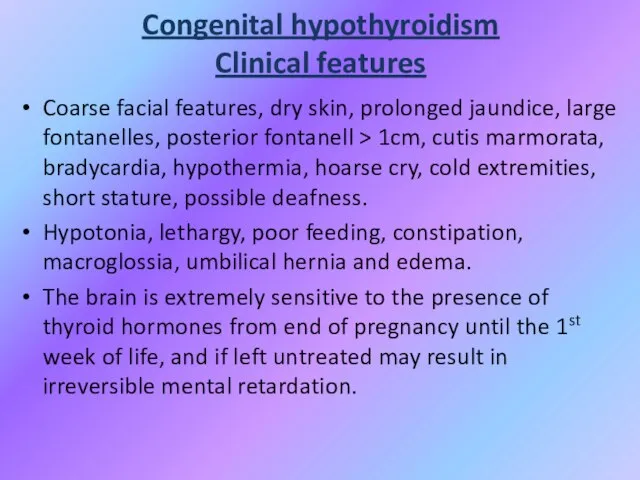
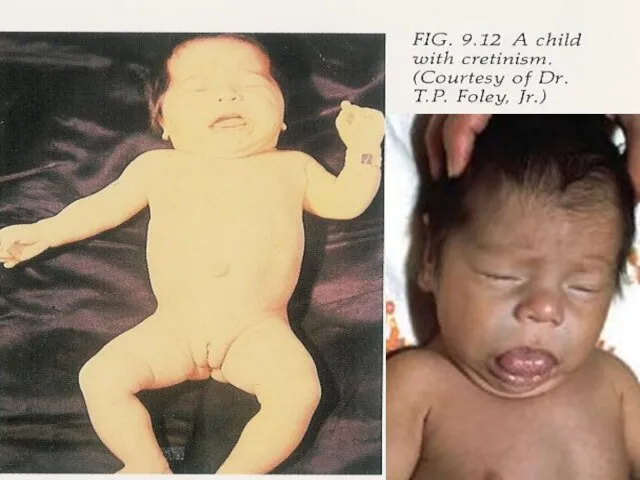
- 60. Congenital hypothyroidism Clinical features Coarse facial features, dry skin, prolonged jaundice, large fontanelles, posterior fontanell >
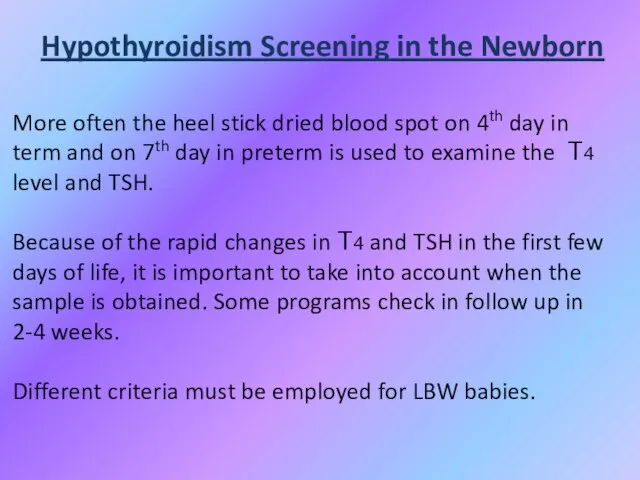
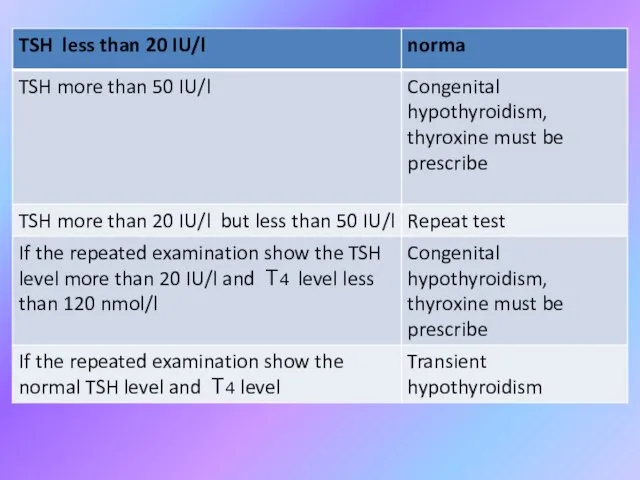
- 63. Hypothyroidism Screening in the Newborn More often the heel stick dried blood spot on 4th day
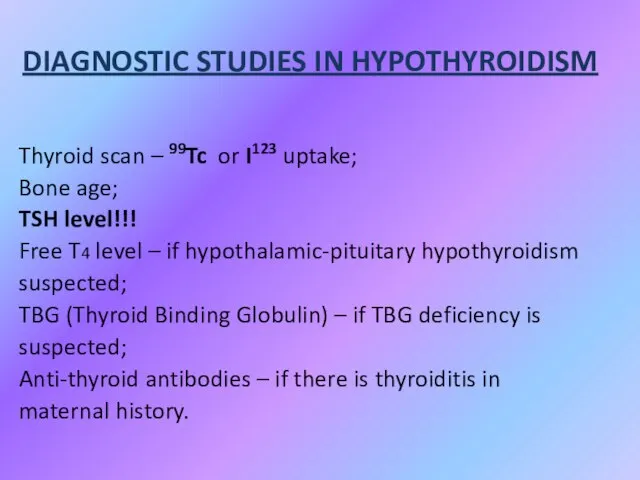
- 66. DIAGNOSTIC STUDIES IN HYPOTHYROIDISM Thyroid scan – 99Tc or I123 uptake; Bone age; TSH level!!! Free
- 67. Biochemical markers of CH Low serum T4 level and T3 level with evaluated TSH (primary) level;
- 68. Biochemical markers of CH Other: Elevated serum cholesterol; Elevated creatinphosphokinase; Hyponatriemia.
- 69. Instrumental data Slightly decrease heart rate and amplitude of R wave (ECG); Increased left ventricular wall
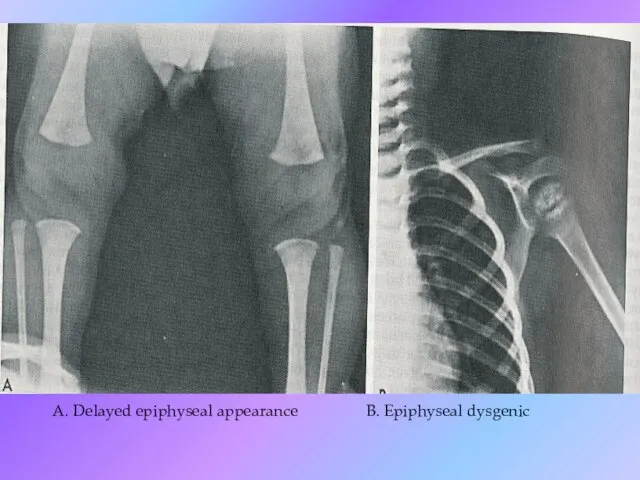
- 70. A. Delayed epiphyseal appearance B. Epiphyseal dysgenic
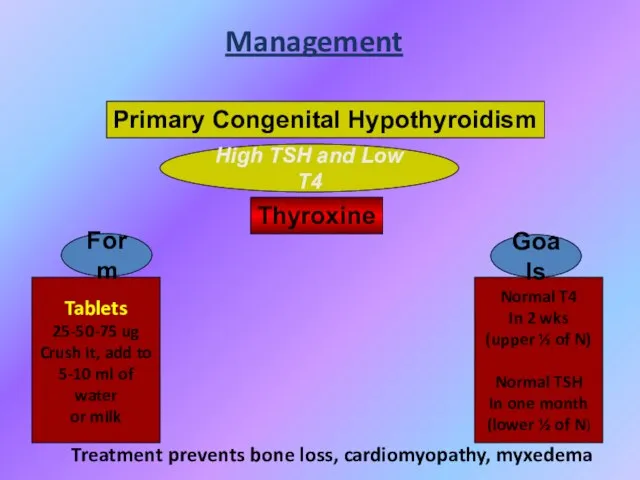
- 71. High TSH and Low T4 Management Primary Congenital Hypothyroidism Thyroxine Tablets 25-50-75 ug Crush it, add
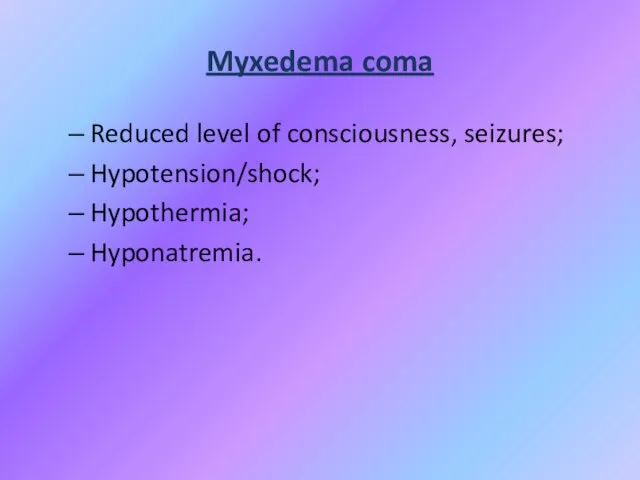
- 72. Myxedema coma Reduced level of consciousness, seizures; Hypotension/shock; Hypothermia; Hyponatremia.
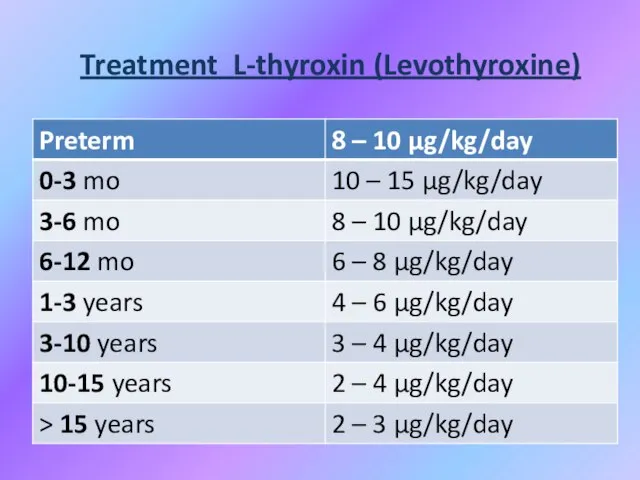
- 73. Treatment L-thyroxin (Levothyroxine)
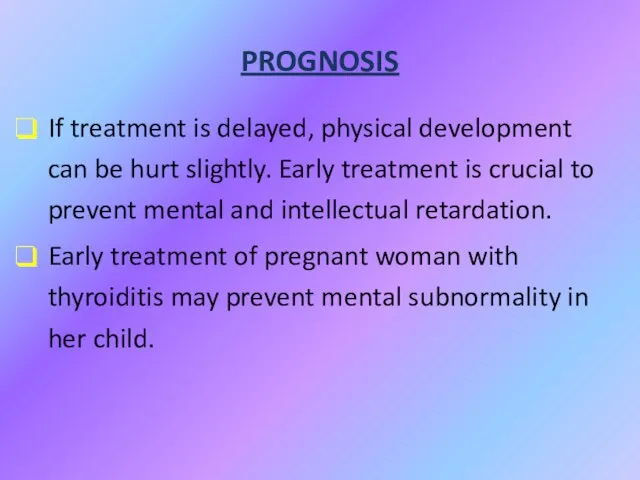
- 74. PROGNOSIS If treatment is delayed, physical development can be hurt slightly. Early treatment is crucial to
- 75. Juvenile hypothyroidism A child with growth retardation, constipation, becomes less sociable, gain weight; his school performance
- 76. Causes of juvenile hypothyroidism Hashimoto thyroiditis. More common in girls who may have initial thyrotoxicosis or
- 77. JH investigations Antithyroglobulin and antimicrosomal antibodies are found. Serum T4 is low (earlier than T3). Bone
- 78. ETIOLOGY OF ACQUIRED HYPOTHYROIDISM Chronic lymphocytic (Hashimoto`s) thyroiditis (CLT); Subacute thyroiditis (De Quervain`s); Goitrogens (iodide, thiouracil,
- 79. SYMPTOMS OF ACQUIRED HYPOTHYROIDISM Slow growth; Edema; Decreased appetite; Constipation; Swollen thyroid gland; Lethargy; Drop in
- 80. SIGNS OF ACQUIRED HYPOTHYROIDISM Delayed reflex return; Mental depression; Pale, thick, or cool skin; Muscle pseudohypertrophy;
- 81. Chronic thyroiditis Hashimoto disease Clinical presentation: Painless diffuse goiter; Goiter with euthyroidism; Toxic thyroiditis; Hypothyroidism with
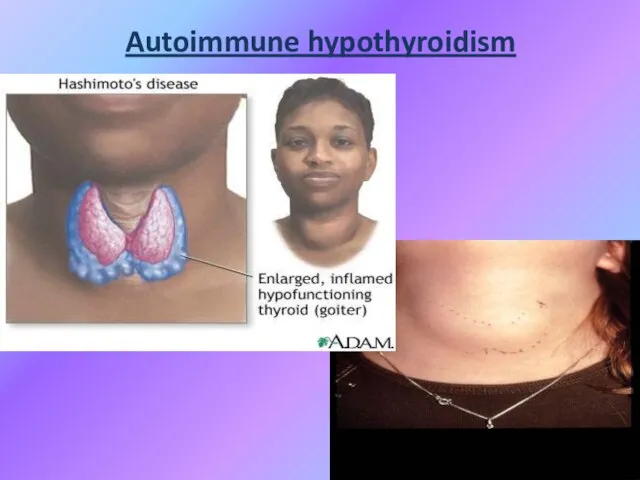
- 82. Autoimmune hypothyroidism
- 83. Diagnosis Hashimoto disease T4 total and free, serum TSH; Biopsy; Antibodies test: antithyroglobulin antibodies to thyroperoxidase,
- 84. Treatment Levothyroxine if hypothyroid; Triiodothyronine (for myxedema coma); Thyroid suppression (levothyroxine) to decrease goiter size; Surgery
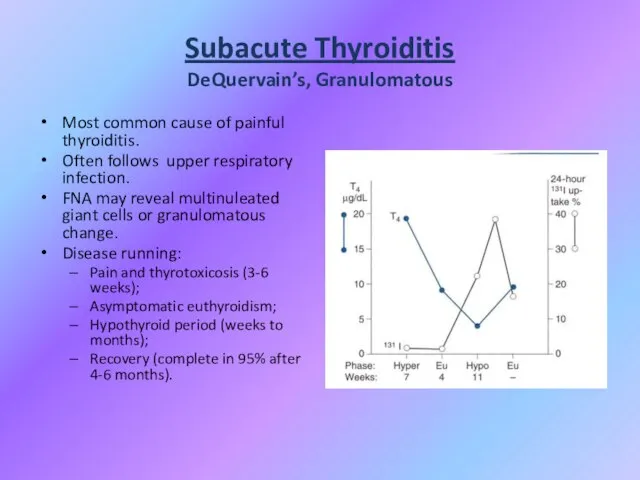
- 85. Subacute Thyroiditis DeQuervain’s, Granulomatous Most common cause of painful thyroiditis. Often follows upper respiratory infection. FNA
- 86. Subacute Thyroiditis DeQuervain’s, Granulomatous
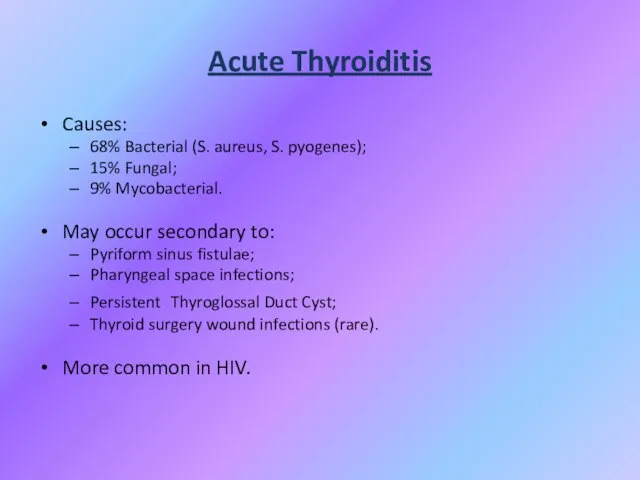
- 87. Acute Thyroiditis Causes: 68% Bacterial (S. aureus, S. pyogenes); 15% Fungal; 9% Mycobacterial. May occur secondary
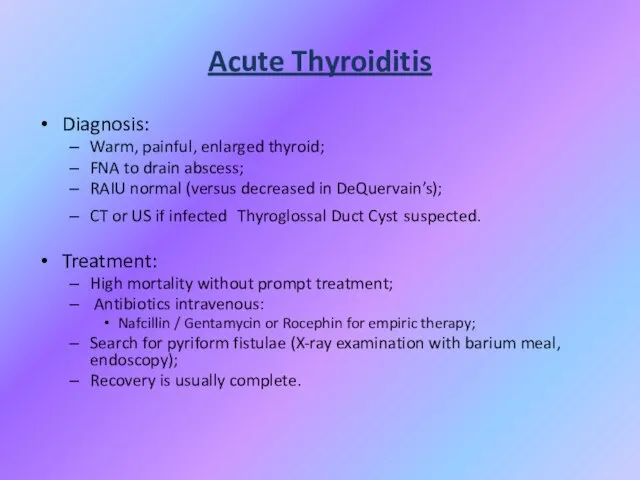
- 88. Acute Thyroiditis Diagnosis: Warm, painful, enlarged thyroid; FNA to drain abscess; RAIU normal (versus decreased in
- 90. Скачать презентацию

 Технологическое предпринимательство для школьников: от изобретения к бизнесу! Занятие 2
Технологическое предпринимательство для школьников: от изобретения к бизнесу! Занятие 2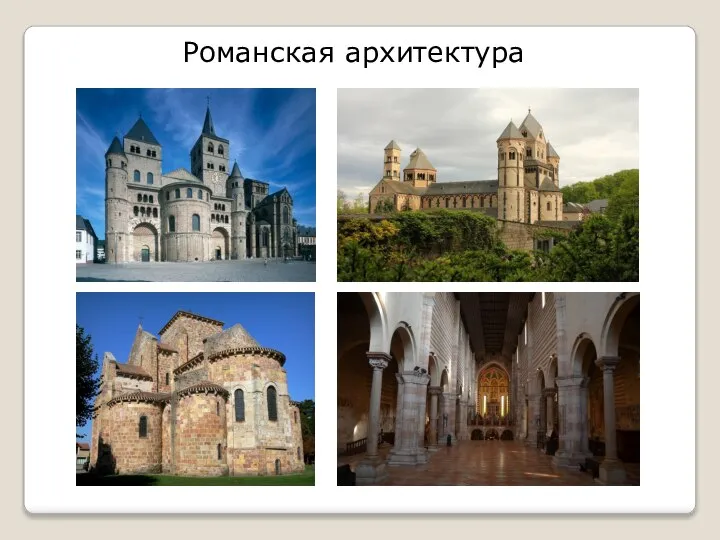 Романская архитектура
Романская архитектура Выборы Лидера совета старшеклассников
Выборы Лидера совета старшеклассников Роботы в древней греции
Роботы в древней греции Функция
Функция Поисковое продвижение: как увеличить его эффективность?
Поисковое продвижение: как увеличить его эффективность? Рекламные решения
Рекламные решения Мегалитическая архитектура 8 класс
Мегалитическая архитектура 8 класс Планета дорог
Планета дорог Забота о ближнем - призвание христианина
Забота о ближнем - призвание христианина МОДЕЛИ ПЕДАГОГИЧЕСКОГО ОБЩЕНИЯ
МОДЕЛИ ПЕДАГОГИЧЕСКОГО ОБЩЕНИЯ Презентация на тему Правила поведения при пожаре
Презентация на тему Правила поведения при пожаре  Викторина по произведению А.С. Пушкина "Капитанская дочка"
Викторина по произведению А.С. Пушкина "Капитанская дочка" Конструирование и моделирование одежды
Конструирование и моделирование одежды Медиабезопасность
Медиабезопасность Агатэ Элерс, отдел Международного сотрудничества Услуги и опыт Немецкого Энергетического Агентства в реализации СО- и МЧР-проект
Агатэ Элерс, отдел Международного сотрудничества Услуги и опыт Немецкого Энергетического Агентства в реализации СО- и МЧР-проект ВСЕМ! ВСЕМ! ВСЕМ! 7 ФЕВРАЛЯ, В 17 ЧАСОВ ГИМНАЗИЯ № 3 ЖДЁТ СВОИХ ВЫПУСКНИКОВ
ВСЕМ! ВСЕМ! ВСЕМ! 7 ФЕВРАЛЯ, В 17 ЧАСОВ ГИМНАЗИЯ № 3 ЖДЁТ СВОИХ ВЫПУСКНИКОВ  Что нас окружает ?
Что нас окружает ? НИД кафедры ЭиУ в 2020/21 уч. году Проблемы, задачи, пути развития
НИД кафедры ЭиУ в 2020/21 уч. году Проблемы, задачи, пути развития Британские художники
Британские художники Год театра в России. Научно-практическая конференция
Год театра в России. Научно-практическая конференция Презентация3
Презентация3 Винтовые лестницы
Винтовые лестницы Экспорт нефти и нормативно-правовое регулирование
Экспорт нефти и нормативно-правовое регулирование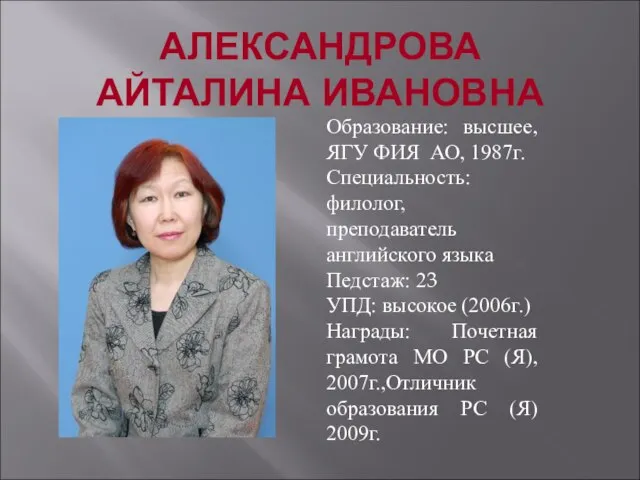 Александрова Айталина Ивановна
Александрова Айталина Ивановна Готовность первоклассника к школе
Готовность первоклассника к школе Отклонение в поведении ребенка как социально-педагогическая проблема
Отклонение в поведении ребенка как социально-педагогическая проблема Презентация на тему Миграции населения России (8 класс)
Презентация на тему Миграции населения России (8 класс)