Содержание
- 2. Case . מטופלת בשם גיל, בת 23, פרופיל 97. עובדת בעבודה משרדית אשקנזיה, שוללת תרופות קבוע.
- 3. בדיקה פיזיקלית תקינה בדיקת שתן כללית תקין, תרבית שתן תקין. STD תקין נבדקה אצל רופא נשים
- 4. What is it? URINARY INCONTINENCE Neurogenic Bladder ANXIETY Nicturia Enuresis
- 5. Definitions Dysuria is a symptom of pain, discomfort, or burning when urinating Nocturia is “the complaint
- 9. Epidemiology Urinary incontinence affects millions of persons, and the prevalence increases with age. Roughly 20 million
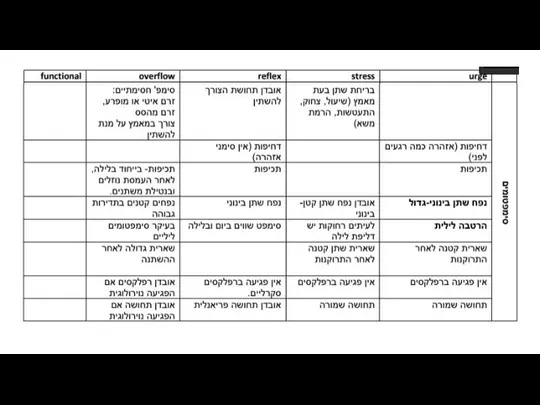
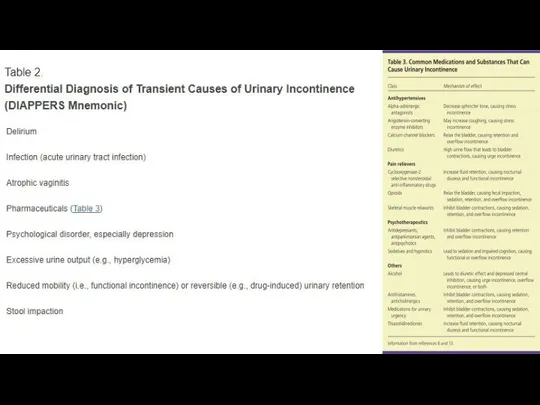
- 10. Classification Incontinence can be classified as transient - spontaneously reverses after the underlying cause is resolved
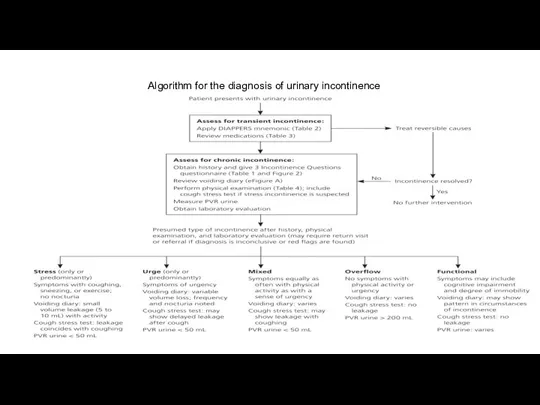
- 14. Algorithm for the diagnosis of urinary incontinence
- 16. Chronic Urinary Incontinence The 3 Incontinence Questions is a reliable questionnaire available free of charge- It
- 17. ASSESSMENT OF MEDICAL PROBLEMS The patient history should include an assessment of other medical conditions and
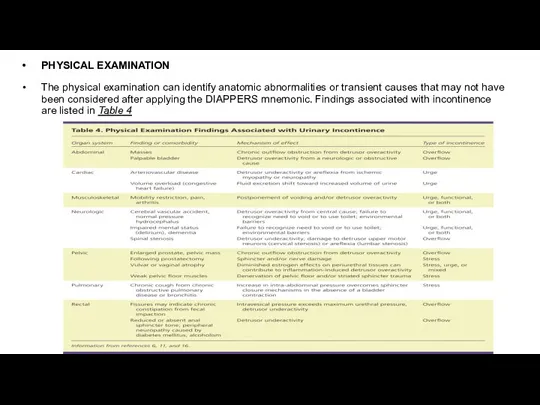
- 18. PHYSICAL EXAMINATION The physical examination can identify anatomic abnormalities or transient causes that may not have
- 19. COUGH STRESS TEST If stress incontinence is suspected, the cough stress test is the most reliable
- 20. LABORATORY TESTS a serum creatinine level - may be elevated if there is urinary retention (overflow
- 21. POSTVOID RESIDUAL URINE A measurement of postvoid residual (PVR) urine is recommended to diagnose overflow incontinence.Although
- 22. If the cause of urinary incontinence is unclear after the assessment, referral to a urologist or
- 23. Routine referral for urodynamic testing is not recommended, even if a patient is a candidate for
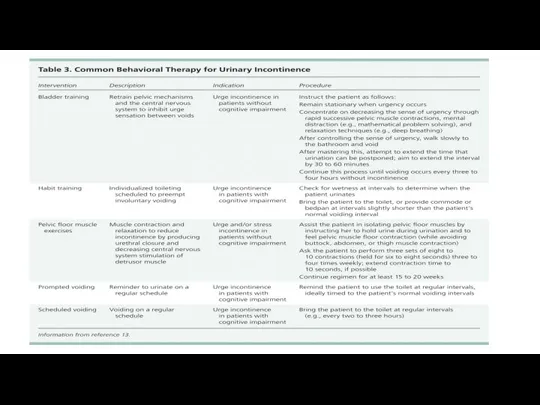
- 26. Pelvic floor muscle (Kegel) exercises — Consistent with guidelines from the American College of Physicians, we
- 27. PHARMACOLOGIC THERAPY Medications can be used to treat urge and mixed incontinence if behavioral therapy is
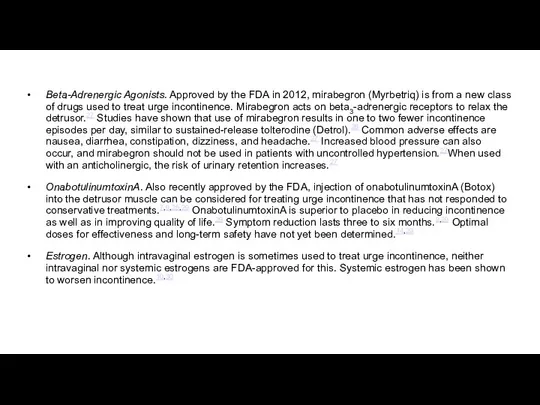
- 30. Beta-Adrenergic Agonists. Approved by the FDA in 2012, mirabegron (Myrbetriq) is from a new class of
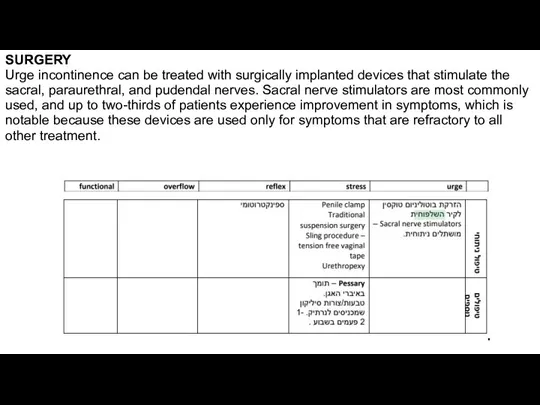
- 31. SURGERY Urge incontinence can be treated with surgically implanted devices that stimulate the sacral, paraurethral, and
- 33. Скачать презентацию
Слайд 2Case
. מטופלת בשם גיל, בת 23, פרופיל 97. עובדת בעבודה משרדית
אשקנזיה, שוללת
Case
. מטופלת בשם גיל, בת 23, פרופיל 97. עובדת בעבודה משרדית
אשקנזיה, שוללת
שוללת ניתוחים והריונות
מתלוננת על דחיפות במתן שתן בכמות מספר טיפות בזמן שיעול או אימון גופני במשך שנתיים.
שוללת צריבת במתן שתן
מציינת עליה במתן שתן בזמן שכיס השתן ריק
Слайд 3בדיקה פיזיקלית תקינה
בדיקת שתן כללית תקין, תרבית שתן תקין.
STD תקין
נבדקה
בדיקה פיזיקלית תקינה
בדיקת שתן כללית תקין, תרבית שתן תקין.
STD תקין
נבדקה
Слайд 4What is it?
URINARY INCONTINENCE
Neurogenic Bladder
ANXIETY
Nicturia
Enuresis
What is it?
URINARY INCONTINENCE
Neurogenic Bladder
ANXIETY
Nicturia
Enuresis
Слайд 5Definitions
Dysuria is a symptom of pain, discomfort, or burning when urinating
Nocturia is “the
Definitions
Dysuria is a symptom of pain, discomfort, or burning when urinating
Nocturia is “the
Enuresis - is a repeated inability to control urination
URINARY INCONTINENCE - any uncontrolled leakage of urine
Neurogenic bladder is a condition that causes problems with bladder control
Guidelines for diagnosis and treatment of urinary incontinence were published in 2012 by the American Urological Association
Слайд 9Epidemiology
Urinary incontinence affects millions of persons, and the prevalence increases with age.
Epidemiology
Urinary incontinence affects millions of persons, and the prevalence increases with age.
Although women report incontinence more often than men,2,3 after 80 years of age, both sexes are affected equally.3 Women commonly experience stress or urge incontinence (i.e., overactive bladder), or a combination of the two, with approximately equal frequency.4 In men, prostate problems, which lead to overflow incontinence, and their treatments, which lead to stress incontinence, are the most common causes.5
1. Fantl AJ. Urinary incontinence in adults: acute and chronic management/urinary incontinence in adults. Guideline Panel Update. Rockville, Md.: U.S. Department of Health and Human Services, 1996; Agency for Health Care Policy and Research; Clinical Practice Guideline Number 2: AHCPR publication no. 96-0682.
2. Holroyd-Leduc JM, Tannenbaum C, Thorpe KE, Straus SE. What type of urinary incontinence does this woman have? JAMA. 2008;299(12):1446–1456.
3. Gibbs CF, Johnson TM II, Ouslander JG. Office management of geriatric urinary incontinence. Am J Med. 2007;120(3):211–220.
4. Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc. 1998;46(4):473–480.
5. DuBeau CE, Kuchel GA, Johnson T II, Palmer MH, Wagg A; Fourth International Consultation on Incontinence. Incontinence in the frail elderly: report from the 4th International Consultation on Incontinence. Neurourol Urodyn. 2010;29(1):165–178.
Слайд 10Classification
Incontinence can be classified as
transient - spontaneously reverses after the underlying
Classification
Incontinence can be classified as
transient - spontaneously reverses after the underlying
chronic - classified into five types:
- stress,
- urge,
- mixed,
- overflow,
- functional
Characteristics of each type are shown in Table 1
Слайд 14Algorithm for the diagnosis of urinary incontinence
Algorithm for the diagnosis of urinary incontinence
Слайд 16Chronic Urinary Incontinence
The 3 Incontinence Questions is a reliable questionnaire available free
Chronic Urinary Incontinence
The 3 Incontinence Questions is a reliable questionnaire available free

Слайд 17ASSESSMENT OF MEDICAL PROBLEMS
The patient history should include an assessment of other
ASSESSMENT OF MEDICAL PROBLEMS
The patient history should include an assessment of other
a history of bowel, back, gynecologic, or bladder surgery could affect the anatomy and innervation of the lower urinary tract, leading to incontinence.
Gynecologic history can assess estrogen status; estrogen deficiency may result in atrophic vaginitis or atrophic urethritis, a potentially reversible cause of urinary incontinence.
about other comorbidities, such as chronic obstructive pulmonary disease (chronic cough can result in stress incontinence); cardiovascular disease (volume status or diuretic therapy can increase urine flow and cause incontinence in patients with an overactive bladder); neurologic conditions (central nervous system dysfunction can impair inhibition of detrusor contractions, or lead to denervation of the detrusor muscle with resultant retention and overflow incontinence); and musculoskeletal conditions (impaired mobility can cause functional incontinence).
ASSESSMENT OF QUALITY OF LIFE
Patients should be asked about the effects of incontinence on work, activities of daily living, sleep, sexual activity, social interactions, interpersonal relationships, and general perception of health and quality of life.
A voiding diary
A voiding diary an also serve as a baseline for comparing the severity of incontinence after treatment, thereby assessing the effectiveness of management. A three-day diary is as informative as a longer-term assessment
Слайд 18PHYSICAL EXAMINATION
The physical examination can identify anatomic abnormalities or transient causes that
PHYSICAL EXAMINATION
The physical examination can identify anatomic abnormalities or transient causes that
Слайд 19COUGH STRESS TEST
If stress incontinence is suspected, the cough stress test is
COUGH STRESS TEST
If stress incontinence is suspected, the cough stress test is
With a full bladder (although not to the point of abrupt urination), the patient should be in the lithotomy position. Women should separate the labia. The patient should relax the pelvic muscles and forcibly cough once.If the test is initially performed supine and no leakage is observed, the test should be repeated in the standing position. The patient stands while wearing a pad or with his or her legs shoulder-width apart over a cloth or paper sheet on the floor to see the leakage. If urine leaks with the onset of the cough and terminates with its cessation, the test is positive for stress incontinence.
A negative test shows no leak or a delayed leak by five to 15 seconds, and rules out most cases of stress incontinence.36 False-negative results may occur if a patient's bladder is empty, if the cough is not forceful enough, if the pelvic floor muscles contract to override urethral sphincter incompetence, or if severe prolapse masks the leakage.
Слайд 20LABORATORY TESTS
a serum creatinine level - may be elevated if there is
LABORATORY TESTS
a serum creatinine level - may be elevated if there is
urinalysis - exclude acute urinary tract infection as a cause of reversible incontinence, a urinalysis should be obtained to rule out hematuria, proteinuria, and glycosuria, any of which require a diagnostic workup.
Слайд 21POSTVOID RESIDUAL URINE
A measurement of postvoid residual (PVR) urine is recommended to
POSTVOID RESIDUAL URINE
A measurement of postvoid residual (PVR) urine is recommended to
To measure PVR urine, the patient empties the bladder, and then the amount of urine remaining in the bladder is measured. This can be performed with a handheld ultrasound unit, which is the preferred method if available. The alternative is in-and-out urethral catheterization.28 In-and-out catheterization requires training to decrease the risk of infection and urethral trauma, which is important in men with significant prostate enlargement. If PVR urine cannot be measured in the office setting and if overflow incontinence is strongly suspected, further urodynamic evaluation is warranted.10,12
A PVR urine measurement less than 50 mL is negative for overflow; 100 to 200 mL is considered indeterminate (and the measurement should be repeated on another occasion); and greater than 200 mL is suggestive of over-flow as a main contributing factor of incontinence.
Слайд 22If the cause of urinary incontinence is unclear after the assessment, referral
If the cause of urinary incontinence is unclear after the assessment, referral
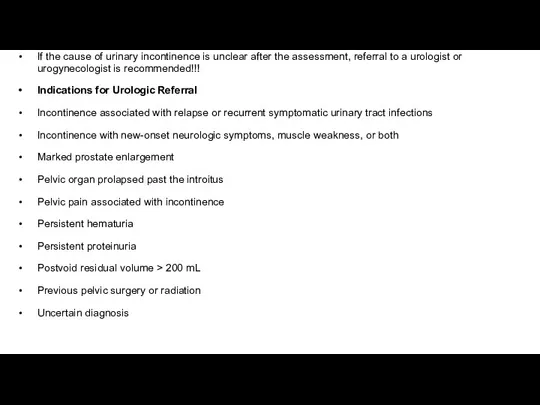
Indications for Urologic Referral
Incontinence associated with relapse or recurrent symptomatic urinary tract infections
Incontinence with new-onset neurologic symptoms, muscle weakness, or both
Marked prostate enlargement
Pelvic organ prolapsed past the introitus
Pelvic pain associated with incontinence
Persistent hematuria
Persistent proteinuria
Postvoid residual volume > 200 mL
Previous pelvic surgery or radiation
Uncertain diagnosis
Слайд 23Routine referral for urodynamic testing is not recommended, even if a patient
Routine referral for urodynamic testing is not recommended, even if a patient
Nager CW, Brubaker L, Litman HJ, et al.; Urinary Incontinence Treatment Network. A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med. 2012;366(21):1987–1997.
Слайд 26Pelvic floor muscle (Kegel) exercises — Consistent with guidelines from the American College of
Pelvic floor muscle (Kegel) exercises — Consistent with guidelines from the American College of
Initial instructions — These exercises can be effective for both stress and urgency incontinence [25] (see "Patient education: Pelvic floor muscle exercises (Beyond the Basics)"). The basic regimen consists of three sets of 8 to 12 contractions sustained for 8 to 10 seconds each, performed three times a day. Patients should try to do this every day and continue for at least 15 to 20 weeks
Слайд 27PHARMACOLOGIC THERAPY
Medications can be used to treat urge and mixed incontinence if
PHARMACOLOGIC THERAPY
Medications can be used to treat urge and mixed incontinence if
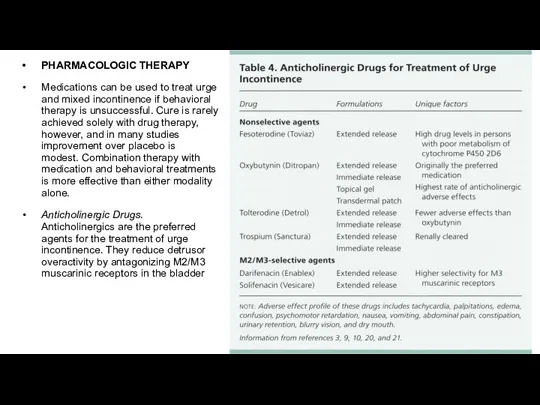
Anticholinergic Drugs. Anticholinergics are the preferred agents for the treatment of urge incontinence. They reduce detrusor overactivity by antagonizing M2/M3 muscarinic receptors in the bladder
Слайд 30Beta-Adrenergic Agonists. Approved by the FDA in 2012, mirabegron (Myrbetriq) is from
Beta-Adrenergic Agonists. Approved by the FDA in 2012, mirabegron (Myrbetriq) is from
OnabotulinumtoxinA. Also recently approved by the FDA, injection of onabotulinumtoxinA (Botox) into the detrusor muscle can be considered for treating urge incontinence that has not responded to conservative treatments.7,9,25,29 OnabotulinumtoxinA is superior to placebo in reducing incontinence as well as in improving quality of life.29 Symptom reduction lasts three to six months.9,29 Optimal doses for effectiveness and long-term safety have not yet been determined.14,29
Estrogen. Although intravaginal estrogen is sometimes used to treat urge incontinence, neither intravaginal nor systemic estrogens are FDA-approved for this. Systemic estrogen has been shown to worsen incontinence.10,30
Слайд 31SURGERY
Urge incontinence can be treated with surgically implanted devices that stimulate the
SURGERY
Urge incontinence can be treated with surgically implanted devices that stimulate the





 Витамины Сила Алтая
Витамины Сила Алтая SA Tallinna Hambapolikliinik
SA Tallinna Hambapolikliinik Методы культивирования и выделения чистых культур аэробов
Методы культивирования и выделения чистых культур аэробов Хімія та медицина
Хімія та медицина Транзиторные состояния неонатального периода
Транзиторные состояния неонатального периода Остеомиелит челюсти
Остеомиелит челюсти Кровь
Кровь Первичный туберкулез тренинг по основным формам первичного туберкулеза легких
Первичный туберкулез тренинг по основным формам первичного туберкулеза легких Имижд медицинской сестры, как часть имиджа лечебного учреждения
Имижд медицинской сестры, как часть имиджа лечебного учреждения Хронический гастрит у детей
Хронический гастрит у детей Гериатриядағы лабораториялық диагносика
Гериатриядағы лабораториялық диагносика Операция
Операция Местноанестезирующие средства. Определение понятия. Классификация местных анестетиков по химической структуре
Местноанестезирующие средства. Определение понятия. Классификация местных анестетиков по химической структуре Клинико-лабораторная оценка эффективности албендазола при описторхозной инвазии
Клинико-лабораторная оценка эффективности албендазола при описторхозной инвазии Частная психопатология
Частная психопатология Репродуктивное здоровье студентов
Репродуктивное здоровье студентов Ішкі секреция бездерінің аурулары бар науқастарды күту және бақылау
Ішкі секреция бездерінің аурулары бар науқастарды күту және бақылау Этические аспекты эвтаназии
Этические аспекты эвтаназии Презентация!!!!!!!!!!!!!!
Презентация!!!!!!!!!!!!!! Математические модели анализа медицинских данных, методы и алгоритмы их реализации
Математические модели анализа медицинских данных, методы и алгоритмы их реализации Три поколения клиентов мастера депиляции
Три поколения клиентов мастера депиляции Острый обструктивный ларингит. Эпиглоттит
Острый обструктивный ларингит. Эпиглоттит Сознание
Сознание Зарядка для глаз
Зарядка для глаз Шовный материал и узлы в хирургии
Шовный материал и узлы в хирургии Кардиомиопатии. Миокардиты
Кардиомиопатии. Миокардиты Онтофилогенетические пороки пищеварительной системы
Онтофилогенетические пороки пищеварительной системы Наследование групп крови
Наследование групп крови