Содержание
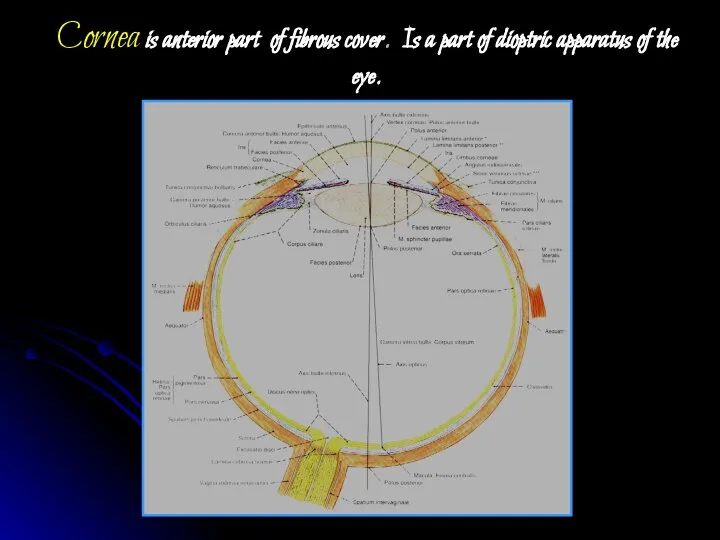
- 2. Cornea is anterior part of fibrous cover. Is a part of dioptric apparatus of the eye.
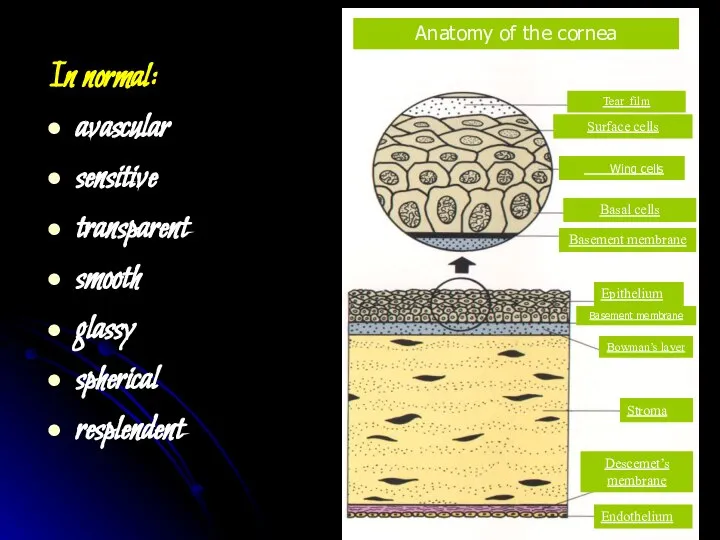
- 3. In normal: avascular sensitive transparent smooth glassy spherical resplendent
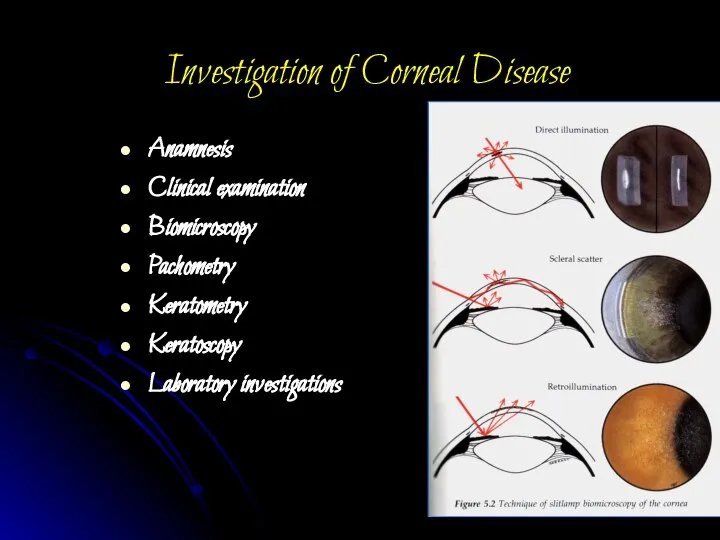
- 5. Investigation of Corneal Disease Anamnesis Clinical examination Biomicroscopy Pachometry Keratometry Keratoscopy Laboratory investigations
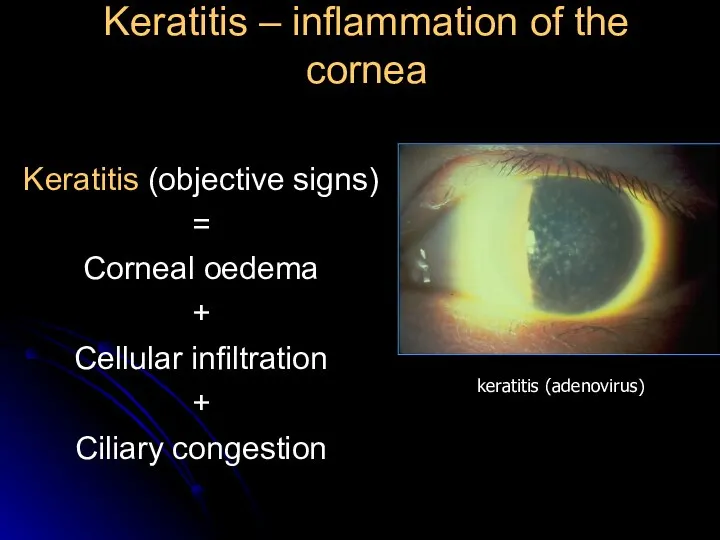
- 6. Keratitis – inflammation of the cornea Keratitis (objective signs) = Corneal oedema + Cellular infiltration +
- 7. Corneal syndrome photophobia lacrimation blepharospasm a sensation of a foreign body present behind the eyelids pain
- 8. Classification 1. Exogenous keratitis Corneal erosions Traumatic keratitis Bacterial keratitis Keratitis, caused by disease of conjunctiva,
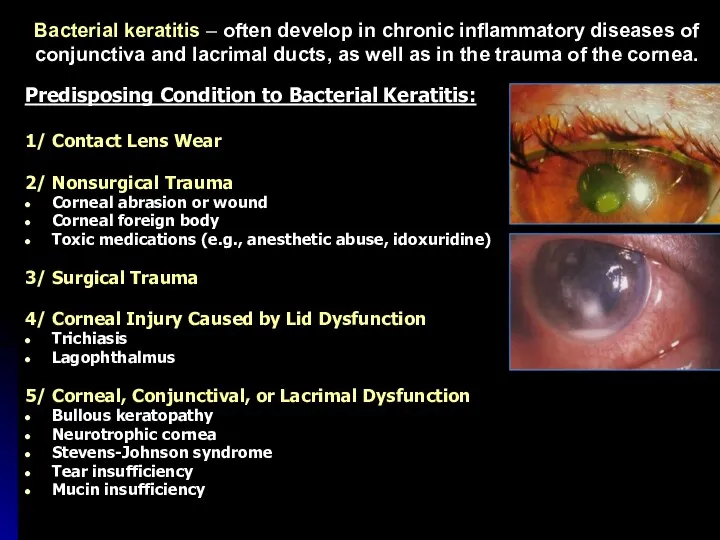
- 9. Bacterial keratitis – often develop in chronic inflammatory diseases of conjunctiva and lacrimal ducts, as well
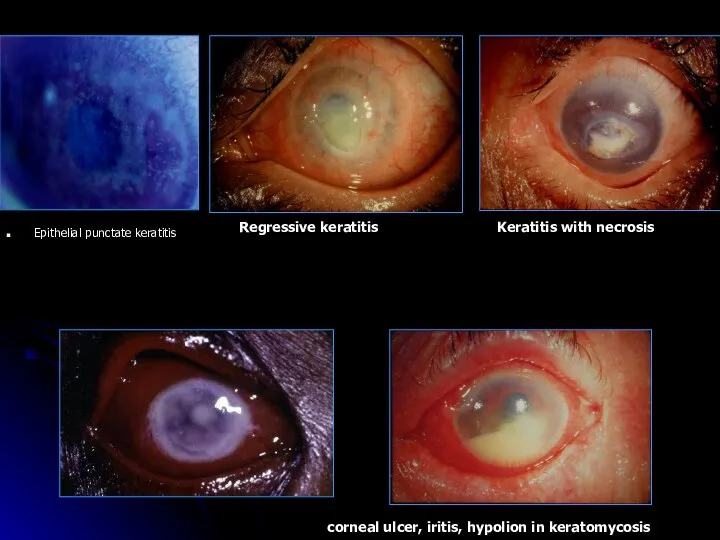
- 10. Epithelial punctate keratitis Keratitis with necrosis Regressive keratitis corneal ulcer, iritis, hypolion in keratomycosis
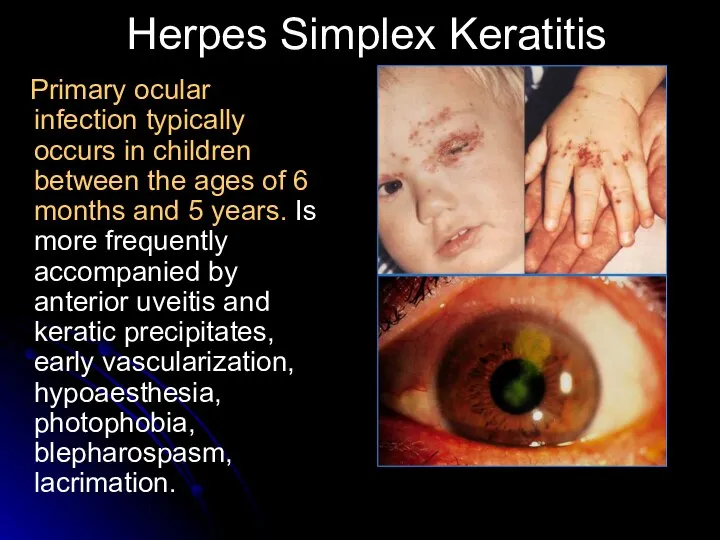
- 11. Herpes Simplex Keratitis Primary ocular infection typically occurs in children between the ages of 6 months
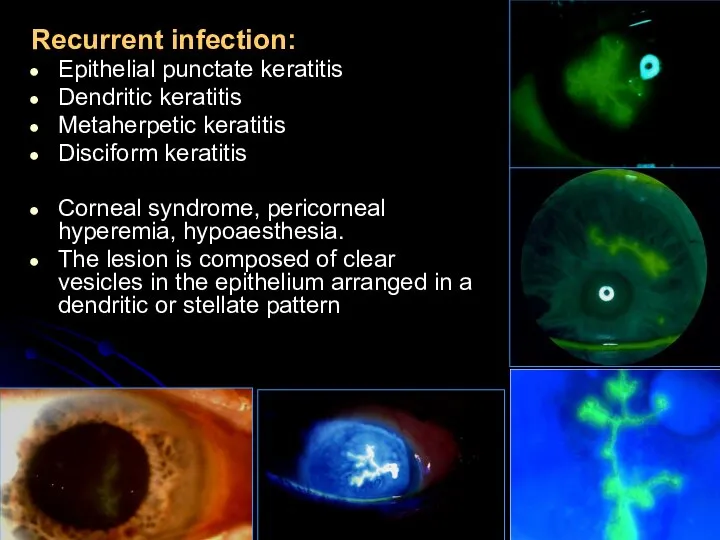
- 12. Recurrent infection: Epithelial punctate keratitis Dendritic keratitis Metaherpetic keratitis Disciform keratitis Corneal syndrome, pericorneal hyperemia, hypoaesthesia.
- 13. additional investigations of patients with keratitis review roentgenography of the additional nasal sinus and organs of
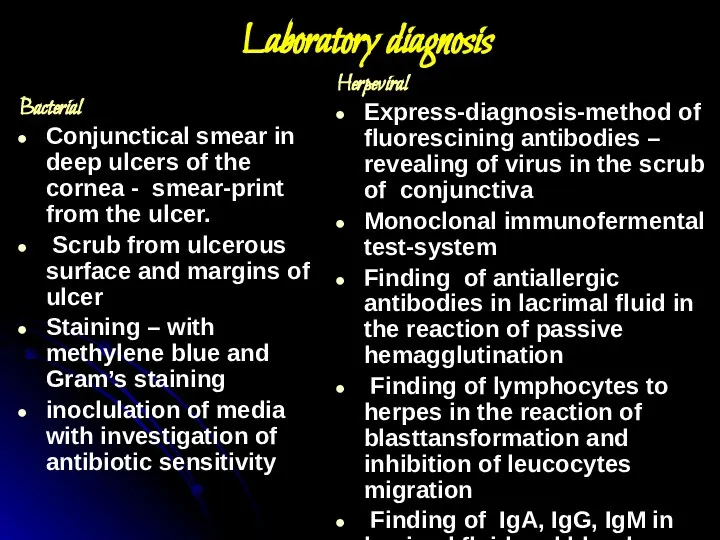
- 14. Laboratory diagnosis Herpeviral Express-diagnosis-method of fluorescining antibodies – revealing of virus in the scrub of conjunctiva
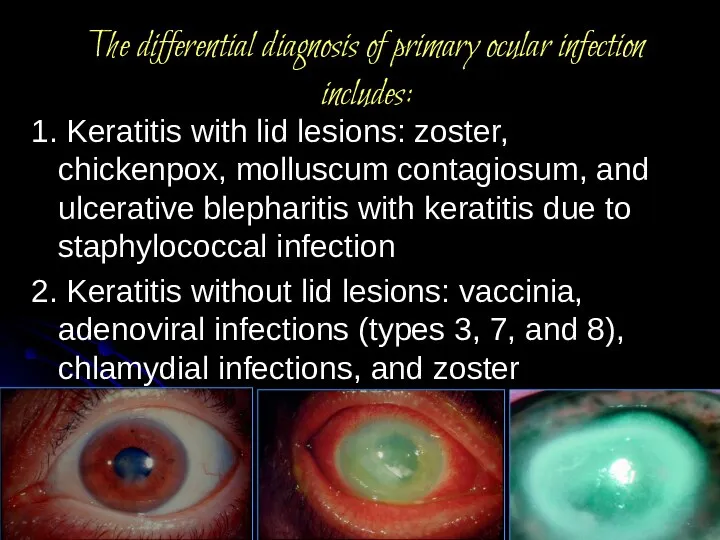
- 15. The differential diagnosis of primary ocular infection includes: 1. Keratitis with lid lesions: zoster, chickenpox, molluscum
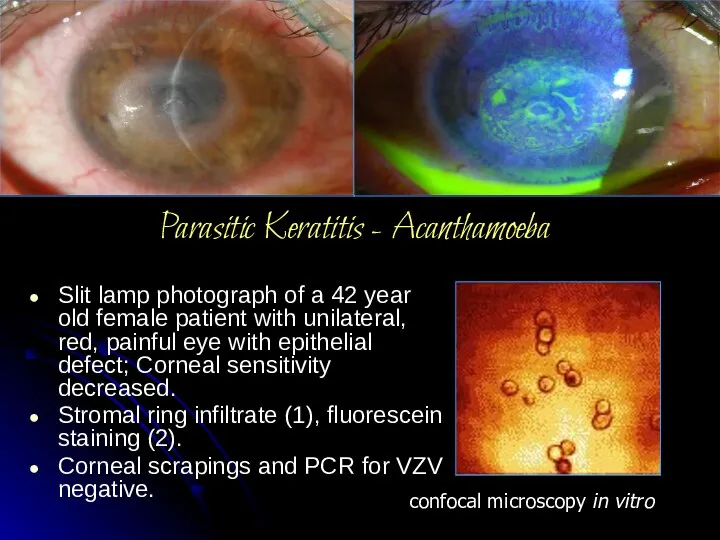
- 16. Parasitic Keratitis - Acanthamoeba Slit lamp photograph of a 42 year old female patient with unilateral,
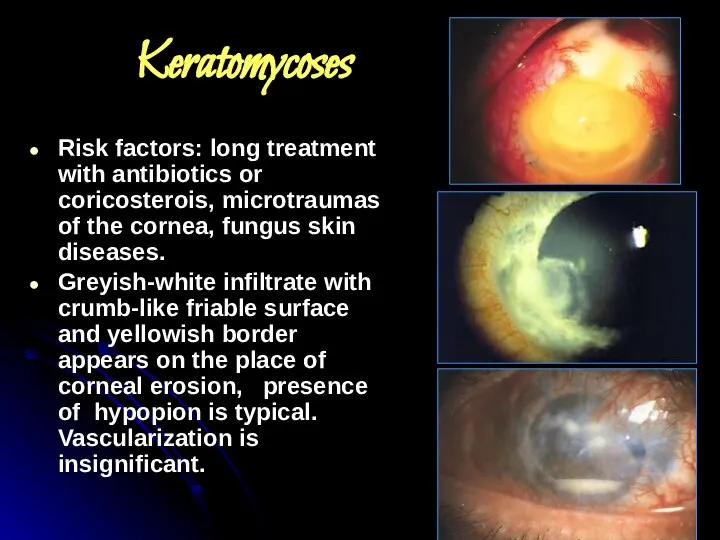
- 17. Keratomycoses Risk factors: long treatment with antibiotics or coricosterois, microtraumas of the cornea, fungus skin diseases.
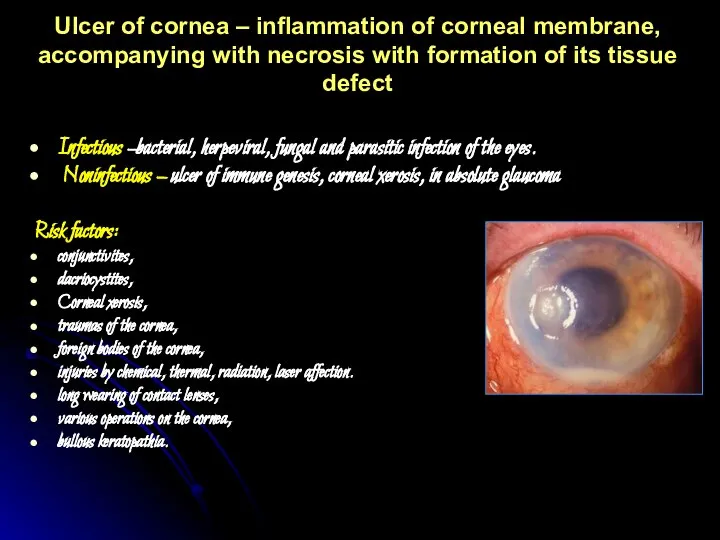
- 18. Ulcer of cornea – inflammation of corneal membrane, accompanying with necrosis with formation of its tissue
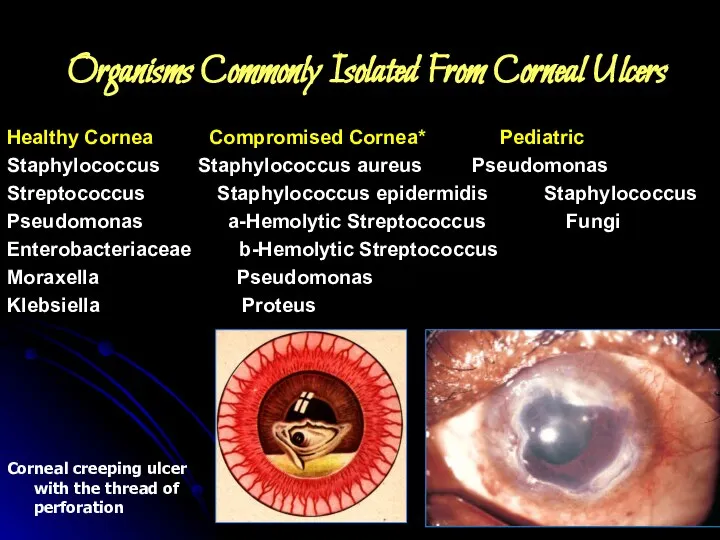
- 19. Organisms Commonly Isolated From Corneal Ulcers Healthy Cornea Compromised Cornea* Pediatric Staphylococcus Staphylococcus aureus Pseudomonas Streptococcus
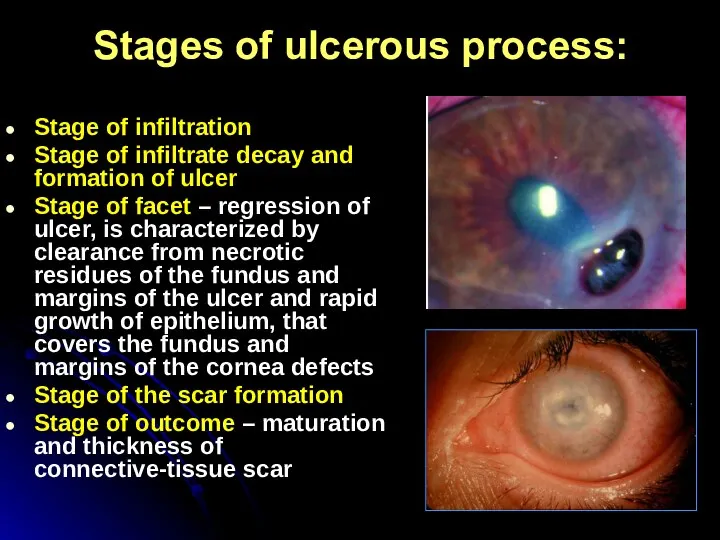
- 20. Stages of ulcerous process: Stage of infiltration Stage of infiltrate decay and formation of ulcer Stage
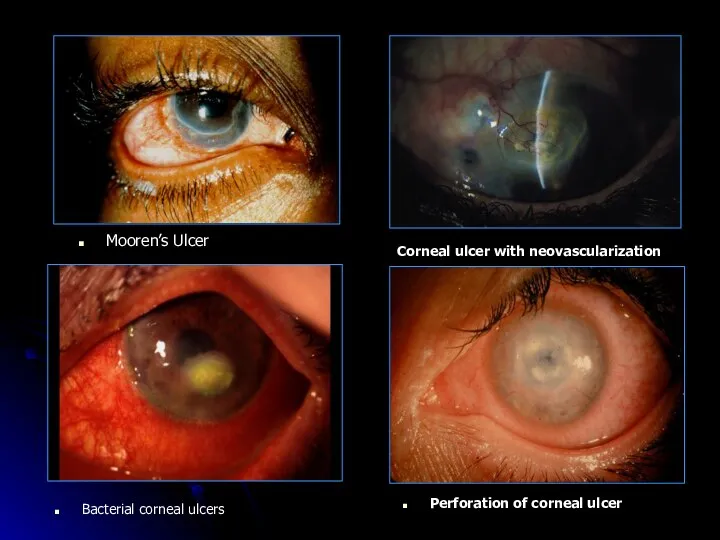
- 21. Mooren’s Ulcer Corneal ulcer with neovascularization Bacterial corneal ulcers Perforation of corneal ulcer
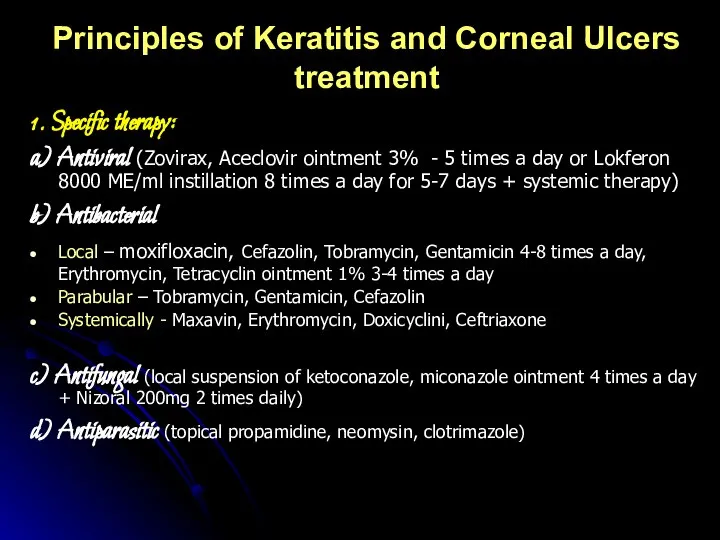
- 22. Principles of Keratitis and Corneal Ulcers treatment 1. Specific therapy: a) Antiviral (Zovirax, Aceclovir ointment 3%
- 23. 2. Pathogenetic therapy Antiinflammatory (Eye drops – only non-steroidal antiinflammatory: Naclof. Parabular or intravenous injection of
- 24. Following arresting of inflammatory process a course of resolving therapy (fibrinolysin, lidase) Penetrating keratoplasty indicated for
- 25. Complications of keratitis: limbal and scleral extension corneal perforation iridocyclitis endophthalmitis Panophthalmitis Secondary glaucoma Corneal scarring:
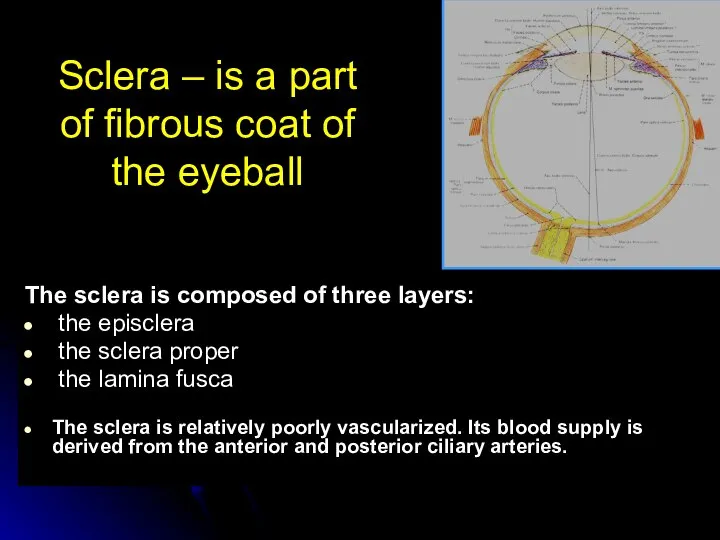
- 26. Sclera – is a part of fibrous coat of the eyeball The sclera is composed of
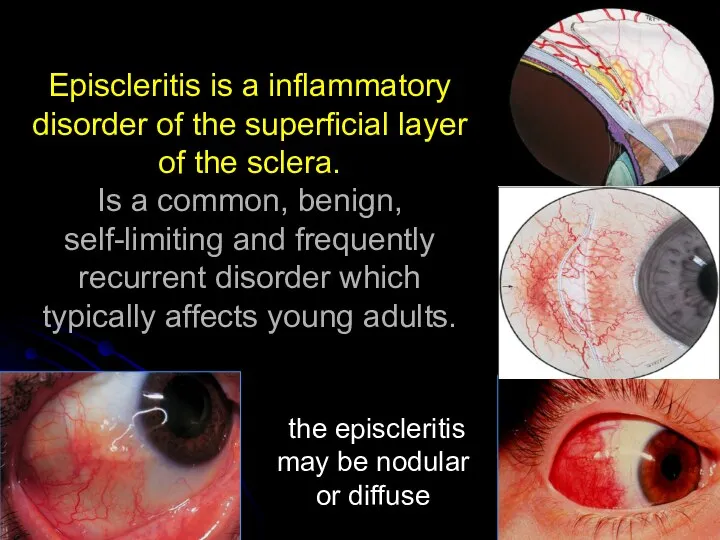
- 28. Episcleritis is a inflammatory disorder of the superficial layer of the sclera. Is a common, benign,
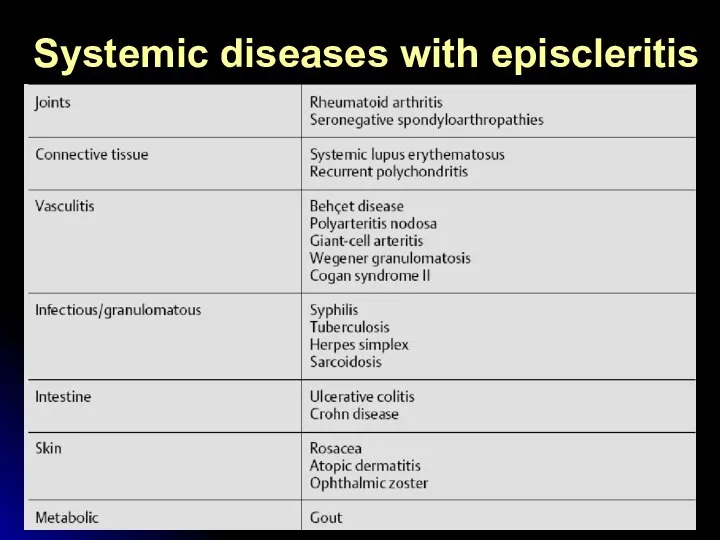
- 29. Systemic diseases with episcleritis
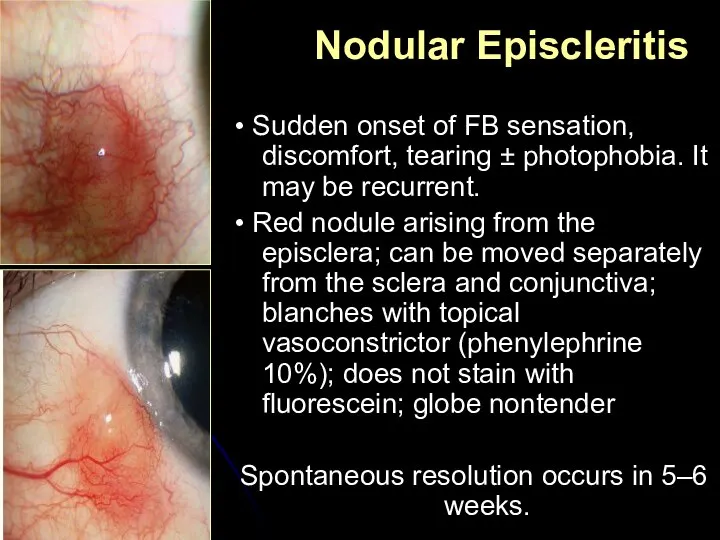
- 30. • Sudden onset of FB sensation, discomfort, tearing ± photophobia. It may be recurrent. • Red
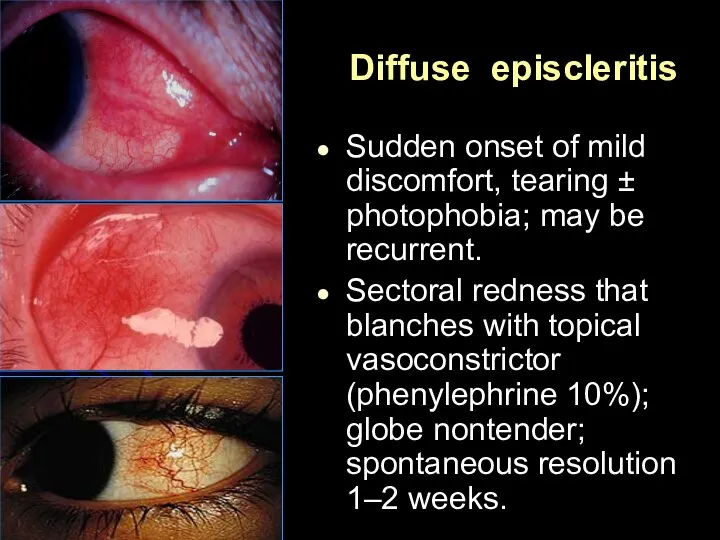
- 31. Diffuse episcleritis Sudden onset of mild discomfort, tearing ± photophobia; may be recurrent. Sectoral redness that
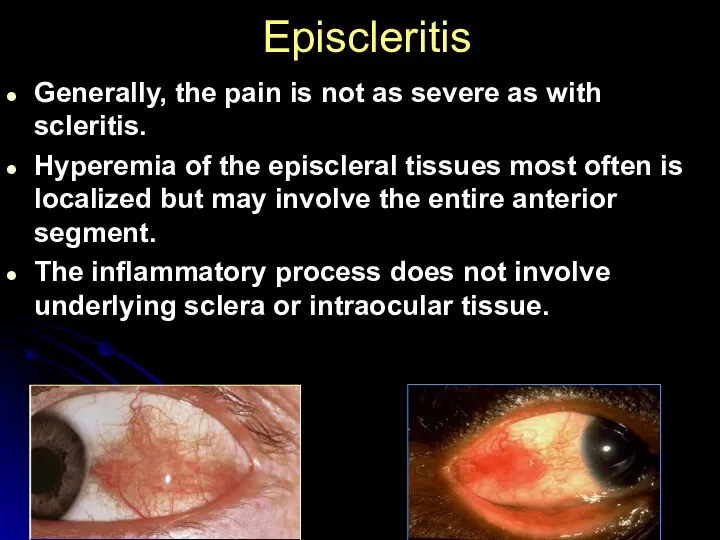
- 32. Episcleritis Generally, the pain is not as severe as with scleritis. Hyperemia of the episcleral tissues
- 33. Treatment If mild, no treatment is required. Supportive: reassurance ± cold compresses. Topical: consider lubricants ±
- 34. COMPLICATIONS Involvement of other ocular structures is rare in patients with episcleritis. The peripheral cornea can
- 35. COURSE AND PROGNOSIS Episcleritis is a mild, non-vision-threatening inflammation of the episclera that may recur over
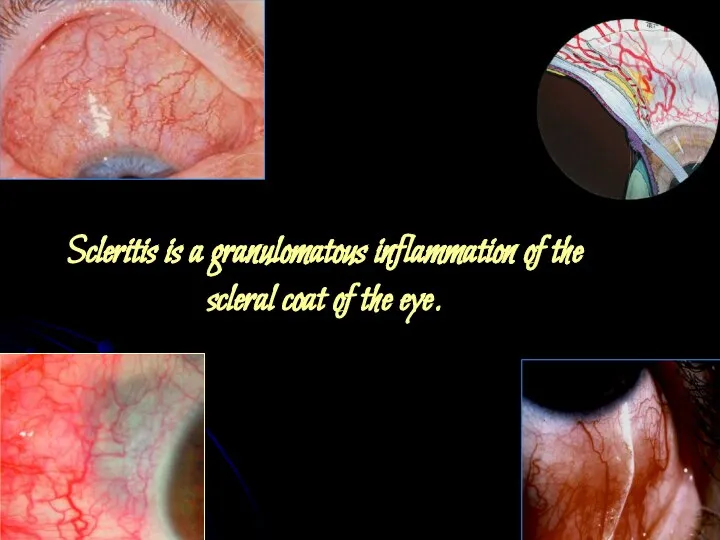
- 36. Scleritis is a granulomatous inflammation of the scleral coat of the eye.
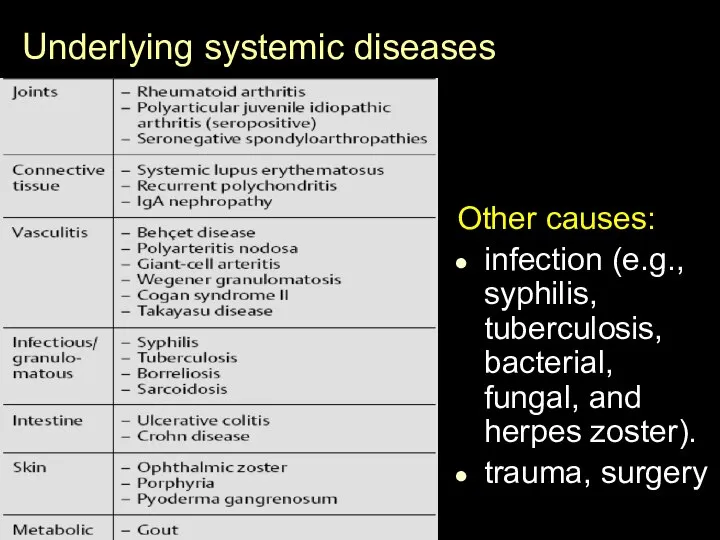
- 37. Underlying systemic diseases Other causes: infection (e.g., syphilis, tuberculosis, bacterial, fungal, and herpes zoster). trauma, surgery
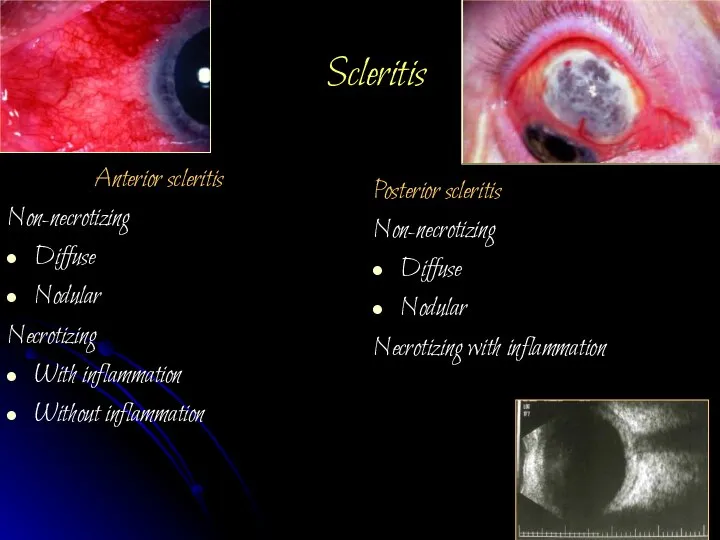
- 38. Scleritis Anterior scleritis Non-necrotizing Diffuse Nodular Necrotizing With inflammation Without inflammation Posterior scleritis Non-necrotizing Diffuse Nodular
- 39. Scleritis presents in the fourth to sixth decade with the gradual onset of classic symptoms of
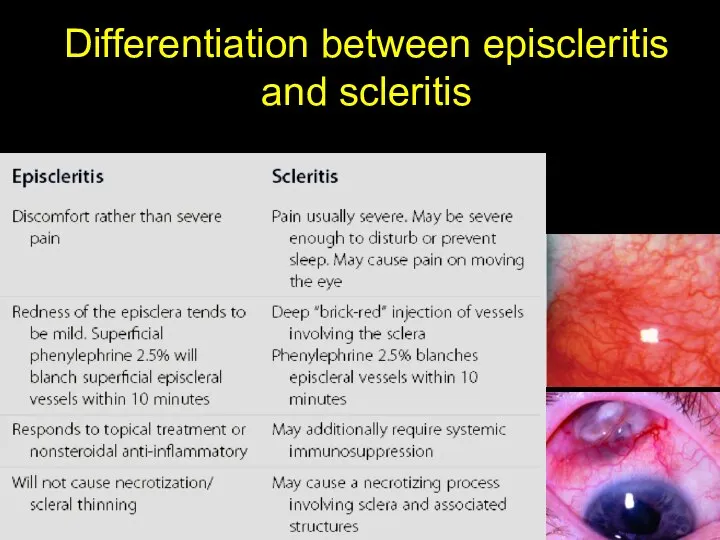
- 40. Differentiation between episcleritis and scleritis
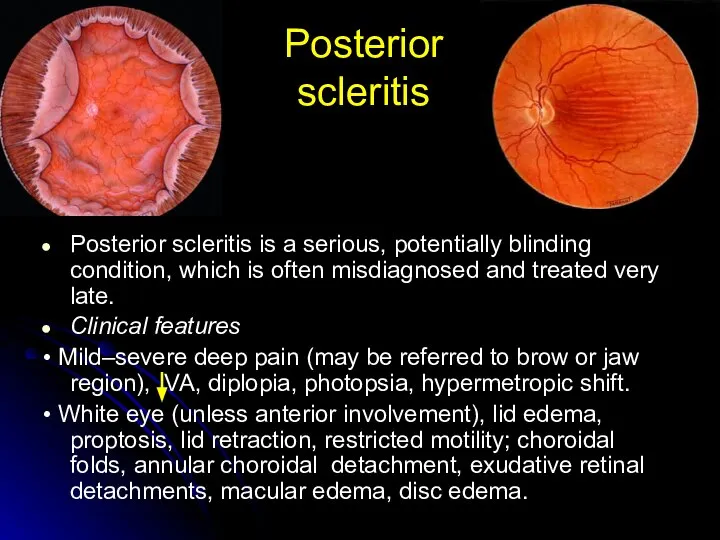
- 41. Posterior scleritis Posterior scleritis is a serious, potentially blinding condition, which is often misdiagnosed and treated
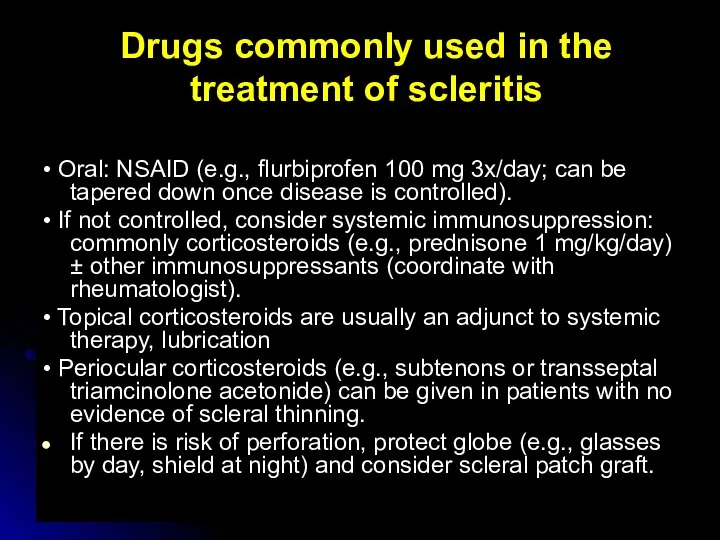
- 42. Drugs commonly used in the treatment of scleritis • Oral: NSAID (e.g., flurbiprofen 100 mg 3x/day;
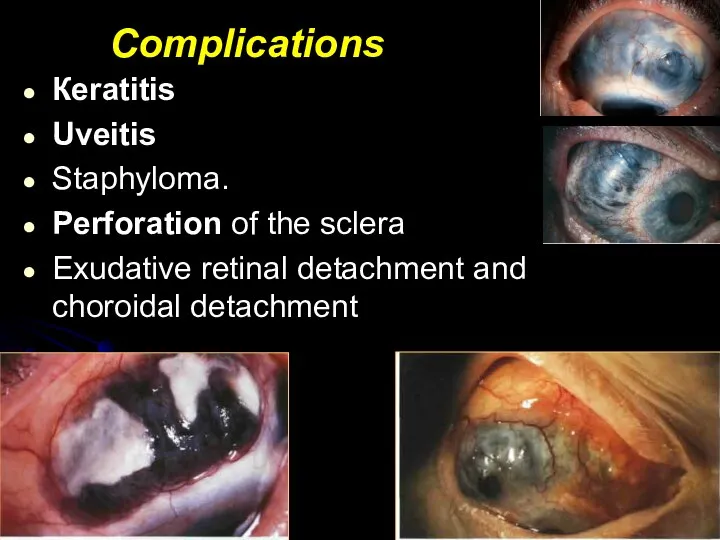
- 43. Complications Кeratitis Uveitis Staphyloma. Perforation of the sclera Exudative retinal detachment and choroidal detachment
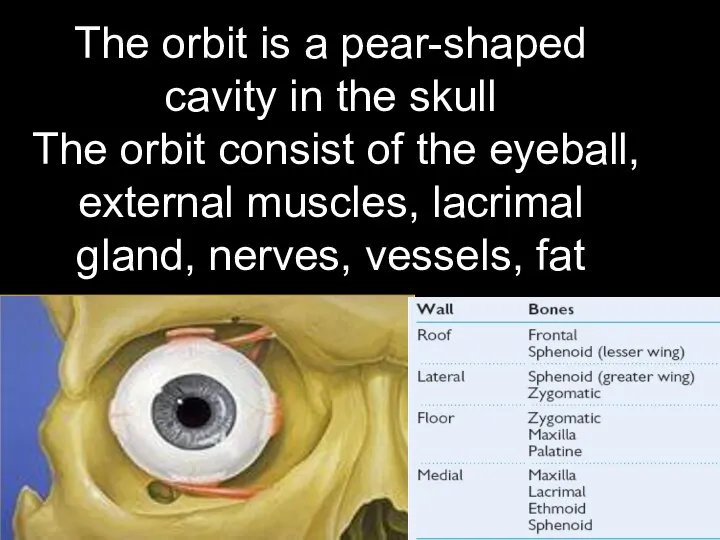
- 44. The orbit is a pear-shaped cavity in the skull The orbit consist of the eyeball, external
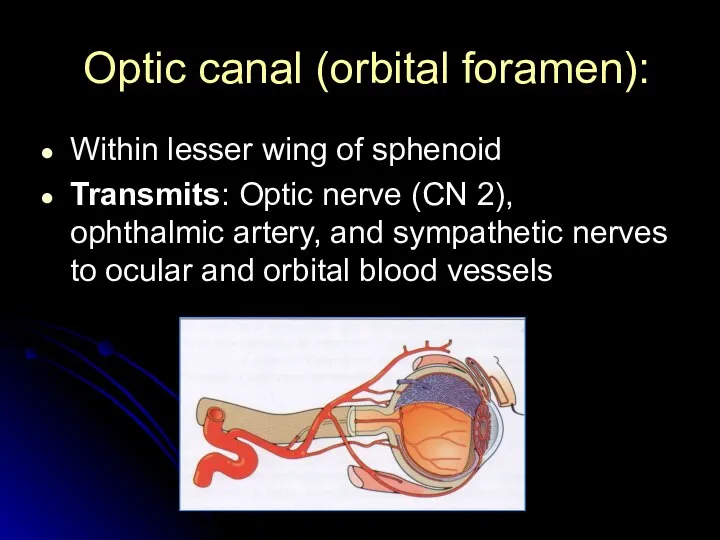
- 45. Optic canal (orbital foramen): Within lesser wing of sphenoid Transmits: Optic nerve (CN 2), ophthalmic artery,
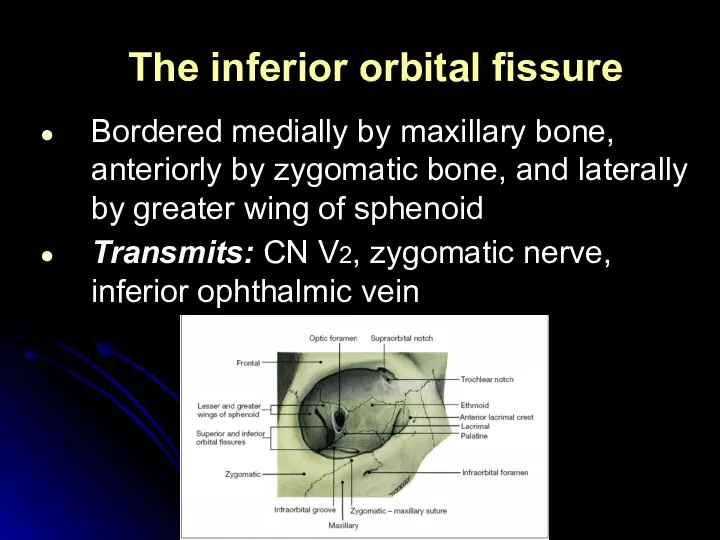
- 46. The inferior orbital fissure Bordered medially by maxillary bone, anteriorly by zygomatic bone, and laterally by
- 47. The superior orbital fissure is a slit linking the cranium and the orbit, between the greater
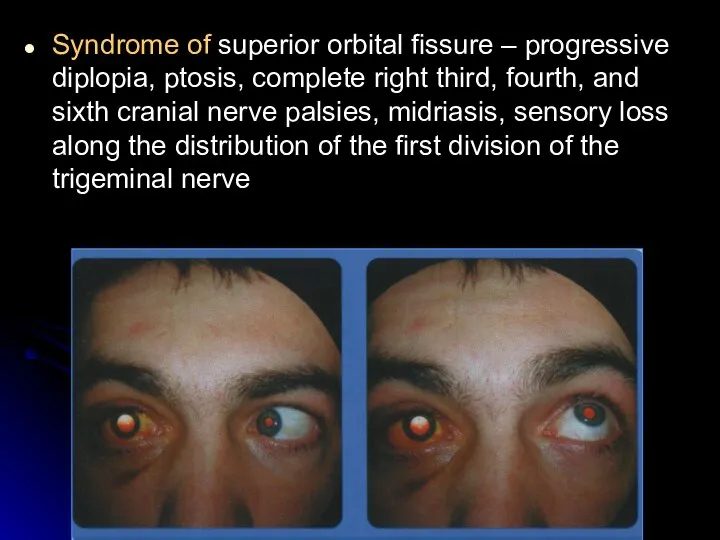
- 48. Syndrome of superior orbital fissure – progressive diplopia, ptosis, complete right third, fourth, and sixth cranial
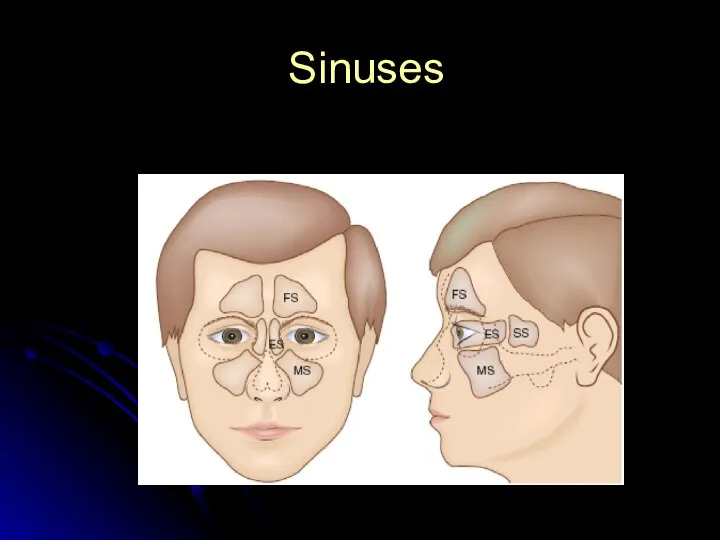
- 49. Sinuses
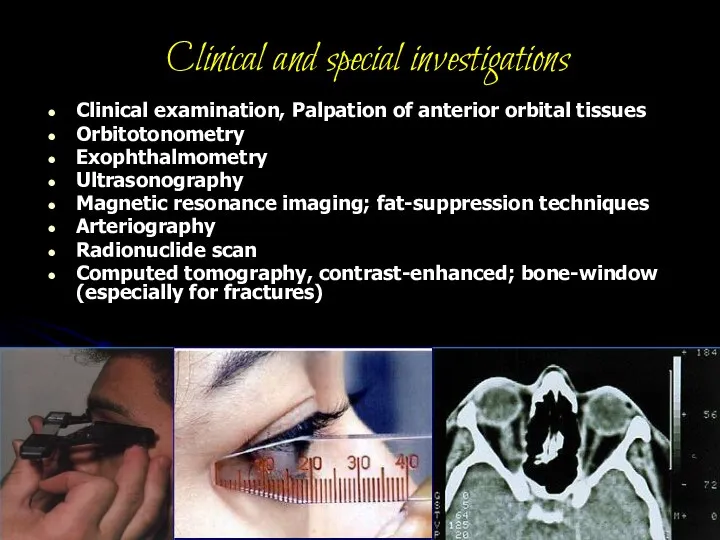
- 50. Clinical and special investigations Clinical examination, Palpation of anterior orbital tissues Orbitotonometry Exophthalmometry Ultrasonography Magnetic resonance
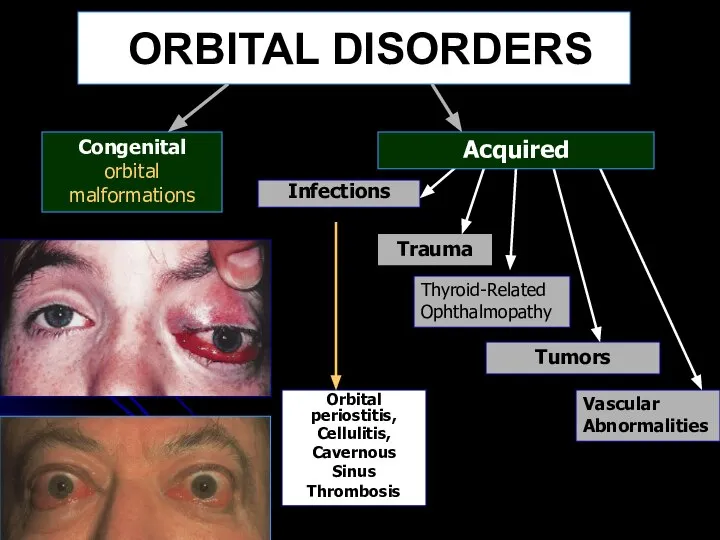
- 51. ORBITAL DISORDERS Congenital orbital malformations Infections Orbital periostitis, Cellulitis, Cavernous Sinus Thrombosis Trauma Thyroid-Related Ophthalmopathy Vascular
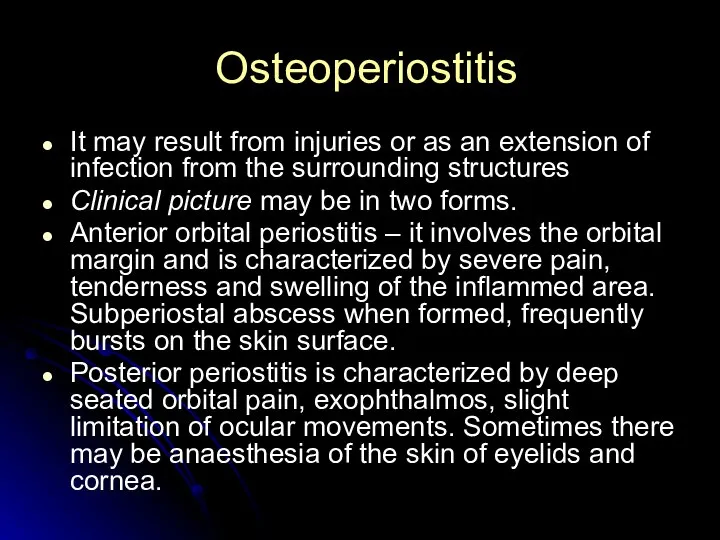
- 52. Osteoperiostitis It may result from injuries or as an extension of infection from the surrounding structures
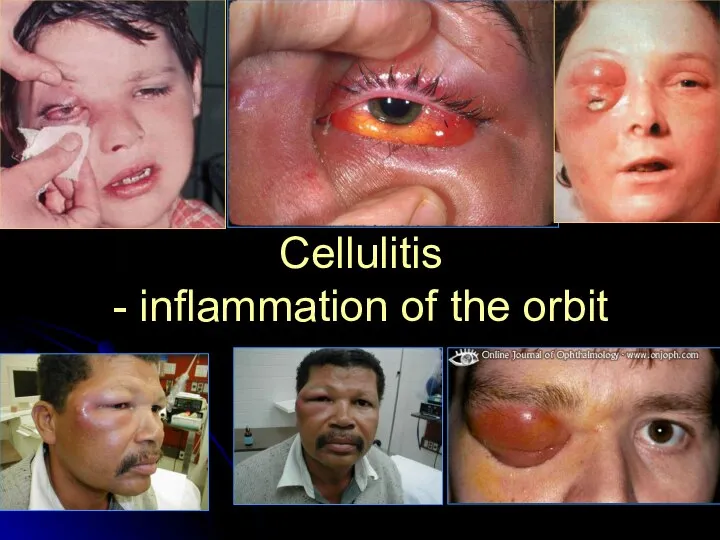
- 53. Cellulitis - inflammation of the orbit
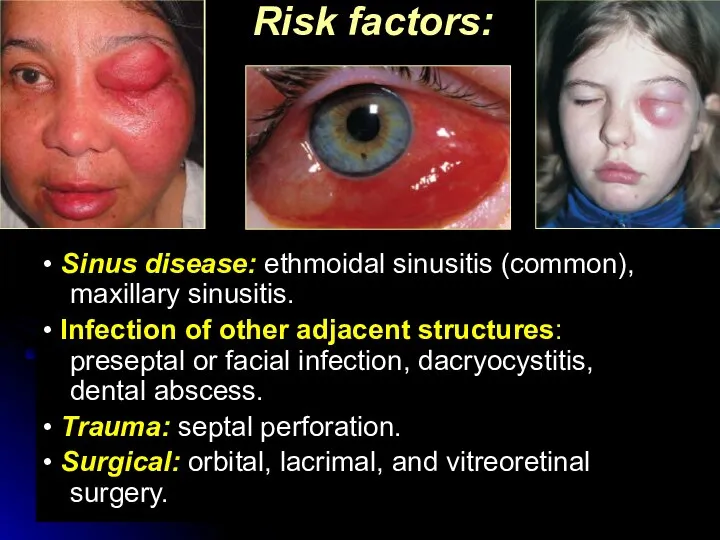
- 54. Risk factors: • Sinus disease: ethmoidal sinusitis (common), maxillary sinusitis. • Infection of other adjacent structures:
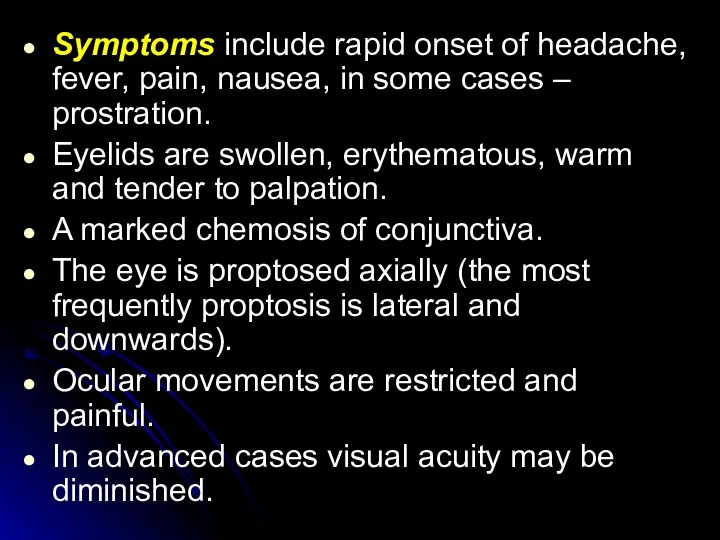
- 55. Symptoms include rapid onset of headache, fever, pain, nausea, in some cases – prostration. Eyelids are
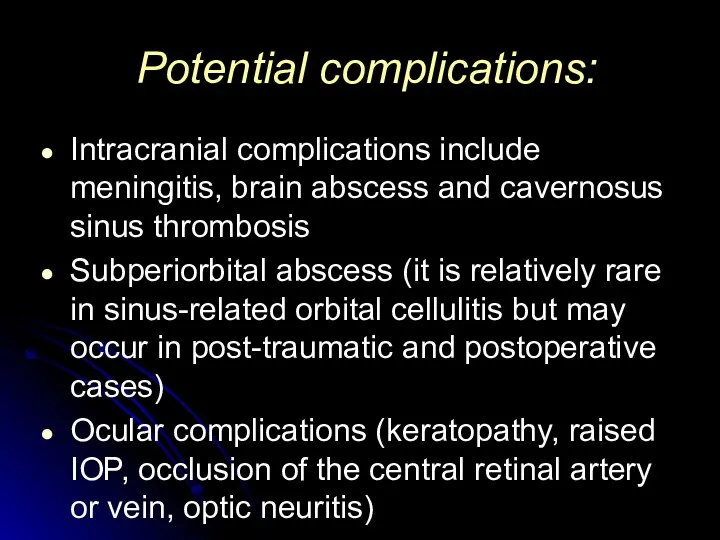
- 56. Potential complications: Intracranial complications include meningitis, brain abscess and cavernosus sinus thrombosis Subperiorbital abscess (it is
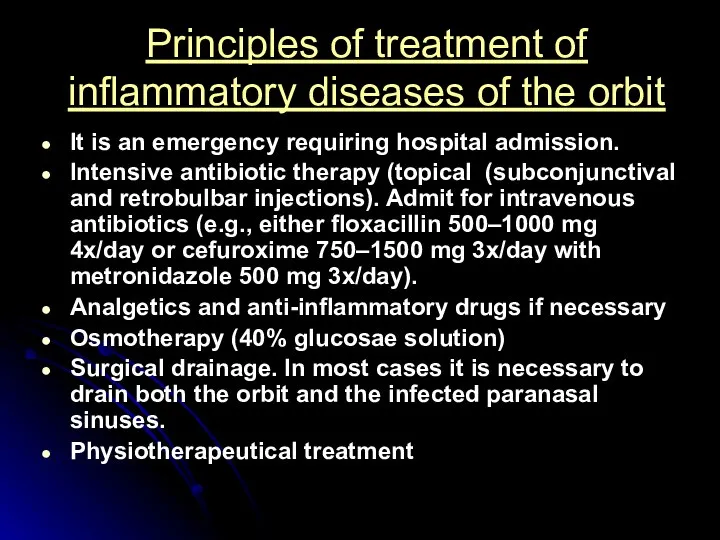
- 57. Principles of treatment of inflammatory diseases of the orbit It is an emergency requiring hospital admission.
- 59. Скачать презентацию




 Нарушение порядка представления информации о реакциях и об осложнениях
Нарушение порядка представления информации о реакциях и об осложнениях Атеросклероз и его клинические проявления. Лекция 2
Атеросклероз и его клинические проявления. Лекция 2 Аутофагия
Аутофагия Определение пульса и его характеристика
Определение пульса и его характеристика Стомотология. Заболевания, связанные с заболеваниями полости рта. Востребованные процедуры
Стомотология. Заболевания, связанные с заболеваниями полости рта. Востребованные процедуры Атеросклероз и его основные клинические проявления
Атеросклероз и его основные клинические проявления Заболевания при которых показан массаж
Заболевания при которых показан массаж Герпесвирусные инфекции V, VI, VII, VIII типов
Герпесвирусные инфекции V, VI, VII, VIII типов Первая помощь при неотложных состояниях
Первая помощь при неотложных состояниях Синдром нижней полой вены
Синдром нижней полой вены Основы ЭЭГ
Основы ЭЭГ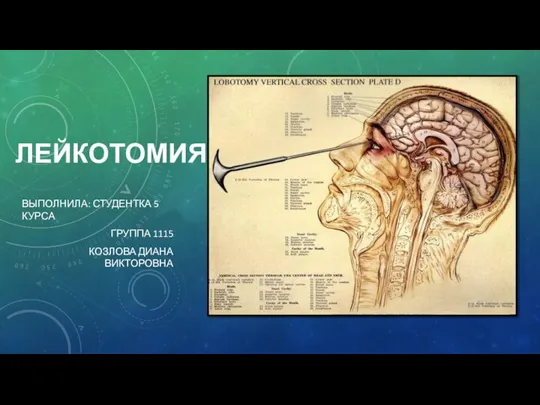 Лейкотомия (лоботомия)
Лейкотомия (лоботомия) Водно-липидная мантия
Водно-липидная мантия Шкала Сильвермана
Шкала Сильвермана Введение в оперативную урологию
Введение в оперативную урологию ВИЧ,СПИД. Профилактика
ВИЧ,СПИД. Профилактика Пищевые отравления
Пищевые отравления 5.7. Кількісний та якісний склад учасників освітнього процесу закладу освіти
5.7. Кількісний та якісний склад учасників освітнього процесу закладу освіти Пациент: Айбекқызы Фарида , 8 лет
Пациент: Айбекқызы Фарида , 8 лет Схема физической реабилитация при переломах длинных трубчатых костей и костей плечевого пояса
Схема физической реабилитация при переломах длинных трубчатых костей и костей плечевого пояса Лекарственное значение корня
Лекарственное значение корня Лекарственные средства, применяемые при аллергических реакциях немедленного типа
Лекарственные средства, применяемые при аллергических реакциях немедленного типа Классификации инфекций в микробиологии
Классификации инфекций в микробиологии Препятствия на пути вакцинации детей в рамках национального календаря профилактических прививок и пути их преодоления
Препятствия на пути вакцинации детей в рамках национального календаря профилактических прививок и пути их преодоления О состоянии смертности по ЛПУ по итогам 6 месяцев 2021 г
О состоянии смертности по ЛПУ по итогам 6 месяцев 2021 г Паразитизм. Пути эволюции паразитов. Заболевания
Паразитизм. Пути эволюции паразитов. Заболевания Ағзаға инсулин еңгізгенде қандай процесс байқалады: гипергликемия, гликогенолиз, гликогеннің глюкозаға ауысуы
Ағзаға инсулин еңгізгенде қандай процесс байқалады: гипергликемия, гликогенолиз, гликогеннің глюкозаға ауысуы Панацея для фронта. Антибиотик крустозин. История создания
Панацея для фронта. Антибиотик крустозин. История создания