Содержание
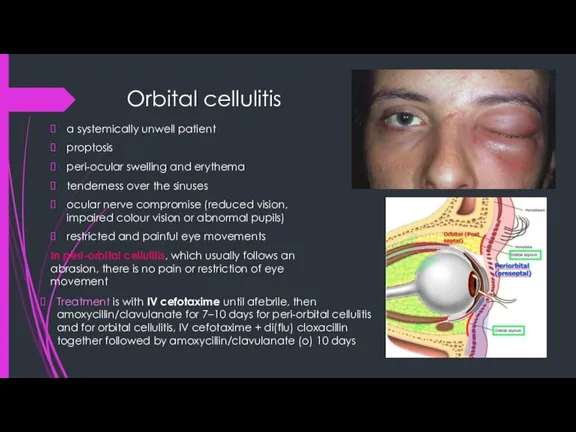
- 3. Orbital cellulitis a systemically unwell patient proptosis peri-ocular swelling and erythema tenderness over the sinuses ocular
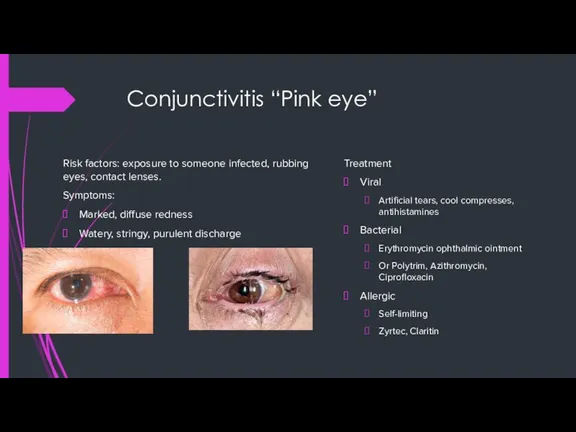
- 4. Conjunctivitis “Pink eye” Risk factors: exposure to someone infected, rubbing eyes, contact lenses. Symptoms: Marked, diffuse
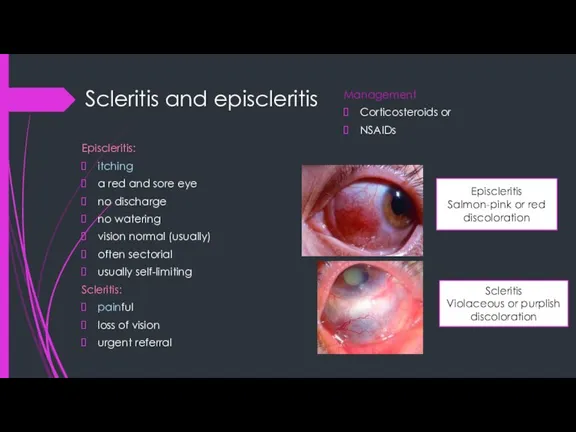
- 5. Scleritis and episcleritis Episcleritis: itching a red and sore eye no discharge no watering vision normal
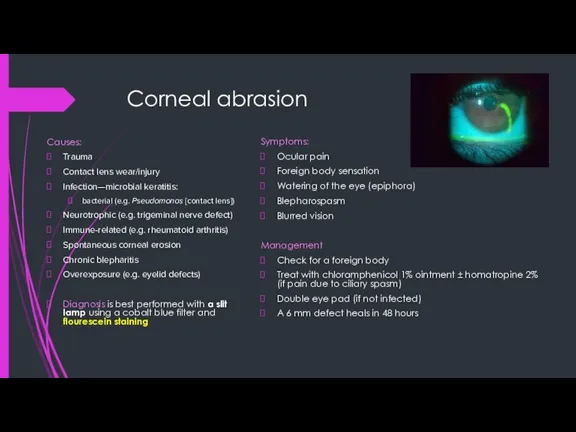
- 6. Corneal abrasion Causes: Trauma Contact lens wear/injury Infection—microbial keratitis: bacterial (e.g. Pseudomonas [contact lens]) Neurotrophic (e.g.
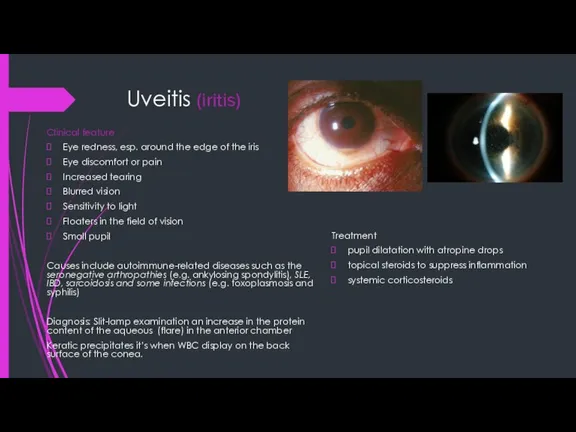
- 7. Uveitis (iritis) Clinical feature Eye redness, esp. around the edge of the iris Eye discomfort or
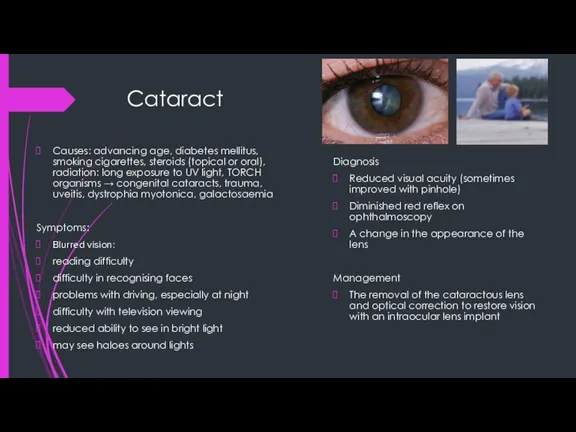
- 8. Cataract Causes: advancing age, diabetes mellitus, smoking cigarettes, steroids (topical or oral), radiation: long exposure to
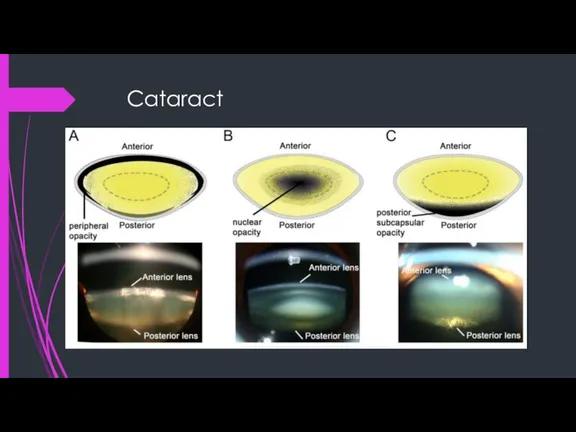
- 9. Cataract
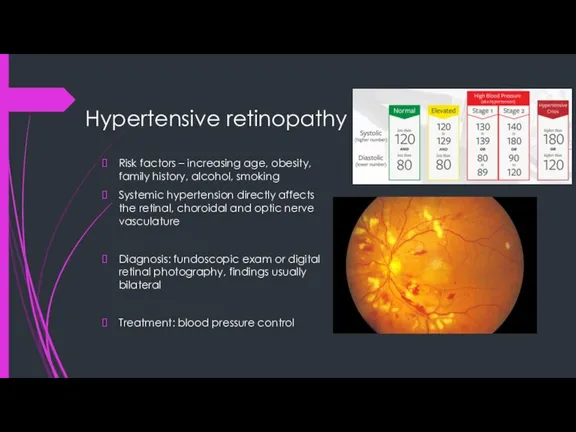
- 10. Hypertensive retinopathy Risk factors – increasing age, obesity, family history, alcohol, smoking Systemic hypertension directly affects
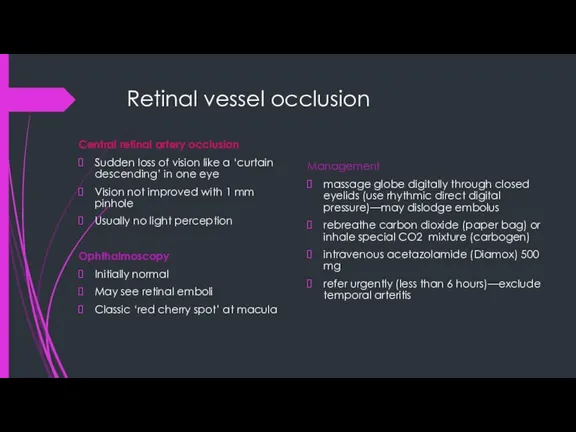
- 11. Retinal vessel occlusion Central retinal artery occlusion Sudden loss of vision like a ‘curtain descending’ in
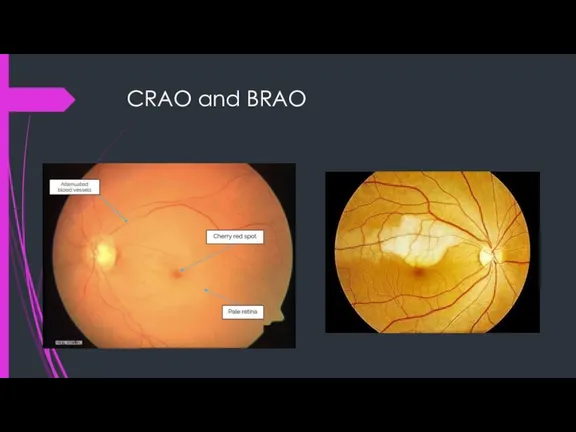
- 12. CRAO and BRAO
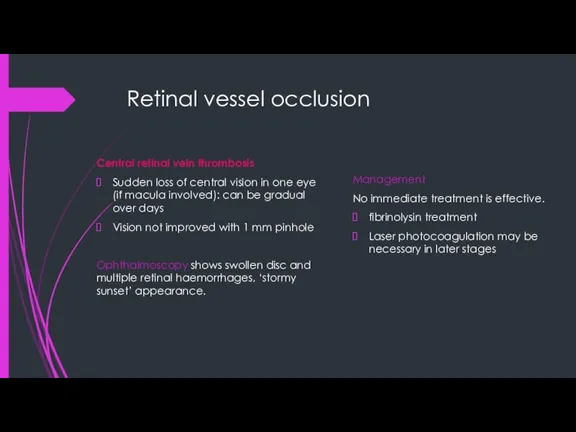
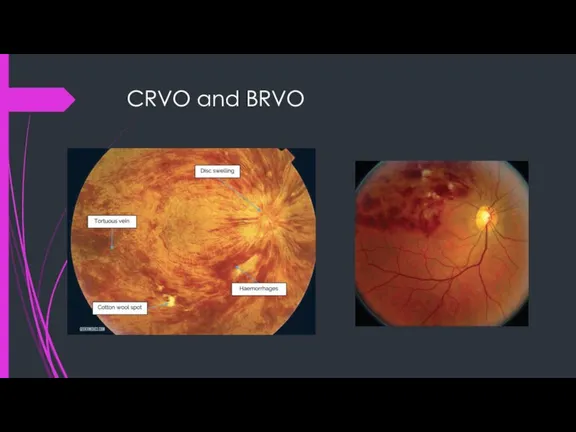
- 13. Retinal vessel occlusion Central retinal vein thrombosis Sudden loss of central vision in one eye (if
- 14. CRVO and BRVO
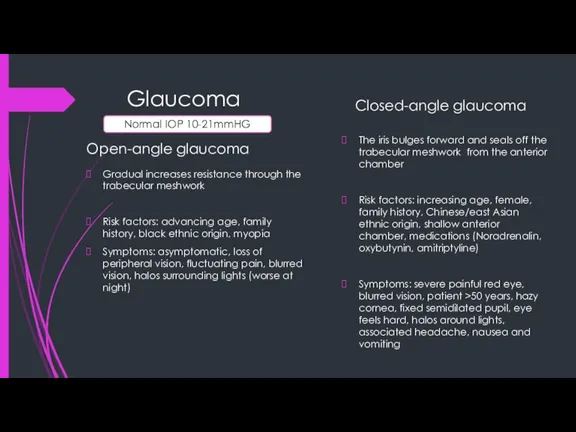
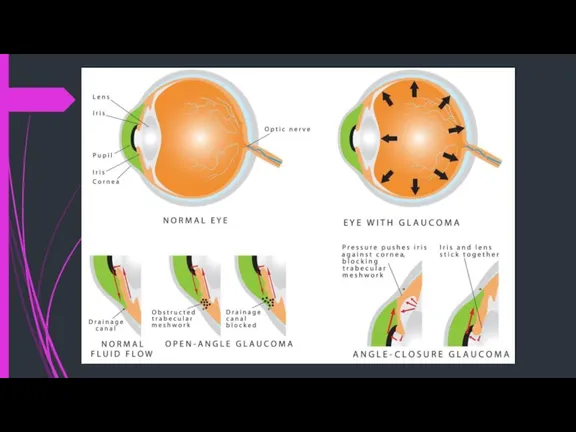
- 15. Glaucoma Open-angle glaucoma Gradual increases resistance through the trabecular meshwork Risk factors: advancing age, family history,
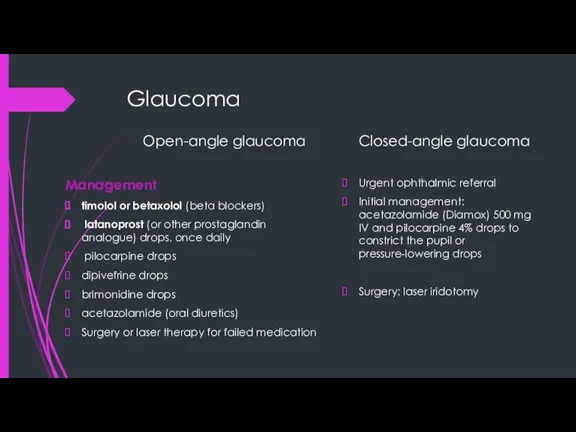
- 16. Glaucoma Open-angle glaucoma Management timolol or betaxolol (beta blockers) latanoprost (or other prostaglandin analogue) drops, once
- 17. Glaucoma
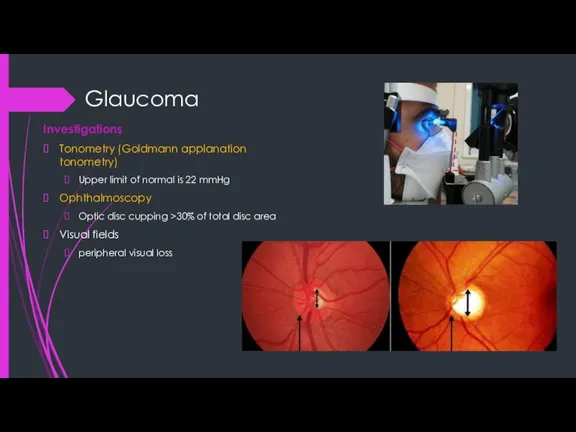
- 18. Glaucoma Investigations Tonometry (Goldmann applanation tonometry) Upper limit of normal is 22 mmHg Ophthalmoscopy Optic disc
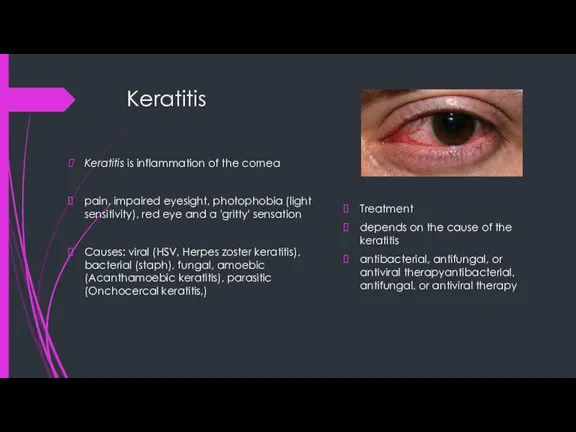
- 19. Keratitis Keratitis is inflammation of the cornea pain, impaired eyesight, photophobia (light sensitivity), red eye and
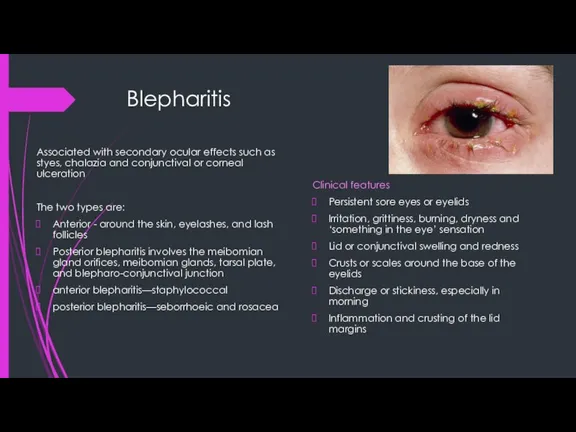
- 20. Blepharitis Clinical features Persistent sore eyes or eyelids Irritation, grittiness, burning, dryness and ‘something in the
- 21. Blepharitis Management Anterior blepharitis A systematic and long-term commitment to a program of eyelid margin hygiene
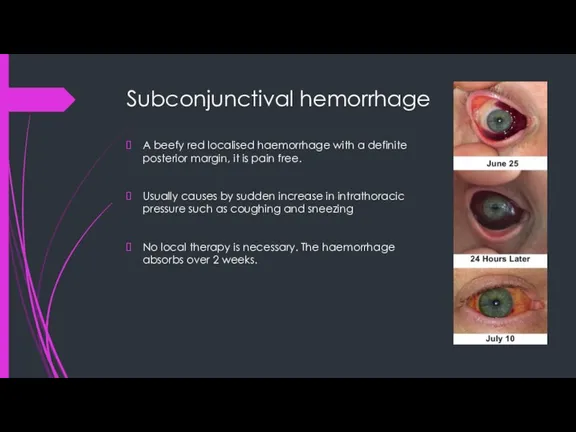
- 22. Subconjunctival hemorrhage A beefy red localised haemorrhage with a definite posterior margin, it is pain free.
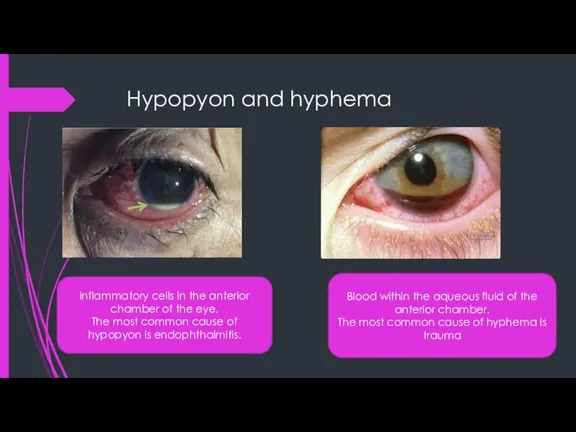
- 23. Hypopyon and hyphema inflammatory cells in the anterior chamber of the eye. The most common cause
- 25. Скачать презентацию
 Биоэтика спорта высших достижений
Биоэтика спорта высших достижений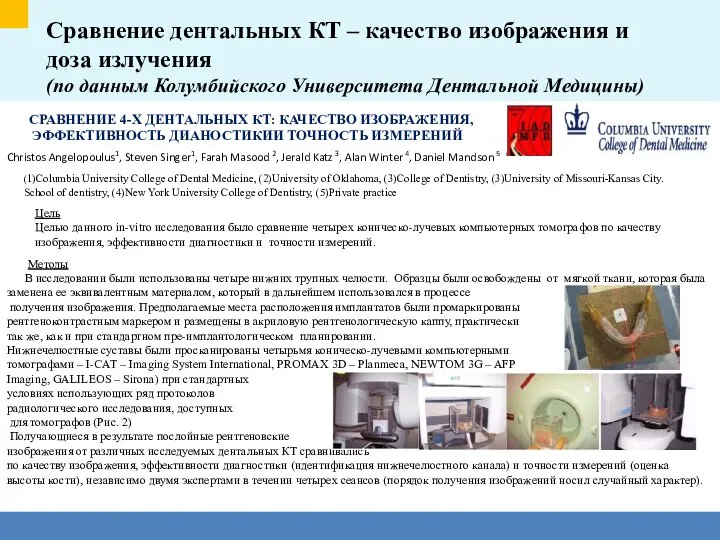 Сравнение дентальных КТ – качество изображения и доза излучения (по данным Колумбийского университета дентальной медицины)
Сравнение дентальных КТ – качество изображения и доза излучения (по данным Колумбийского университета дентальной медицины) Введение в профилактику. Гигиена полости рта
Введение в профилактику. Гигиена полости рта Перетренированность: мышечная, нервная, психологическая
Перетренированность: мышечная, нервная, психологическая Методы обследования при заболеваниях органов дыхания
Методы обследования при заболеваниях органов дыхания Запоминалка для черепных нервов. Вегетативная НС. Методы исследования НС
Запоминалка для черепных нервов. Вегетативная НС. Методы исследования НС Борьба с инфекционными заболеваниями. Родительское собрание
Борьба с инфекционными заболеваниями. Родительское собрание Пневмонии. Плевриты (лекция 1)
Пневмонии. Плевриты (лекция 1) Коллапс. Причины коллапса
Коллапс. Причины коллапса Дезинфекция
Дезинфекция Role of exosomes in pregnancy loss (miscarriage) CD 9, 81, 63
Role of exosomes in pregnancy loss (miscarriage) CD 9, 81, 63 Рациональное питание
Рациональное питание Сахарный диабет
Сахарный диабет Буклет. Польза ходьбы
Буклет. Польза ходьбы Кариес. Кариесогенные факторы в полости рта. Способы их выявления и устранения. Зубные отложения и методы их выявления
Кариес. Кариесогенные факторы в полости рта. Способы их выявления и устранения. Зубные отложения и методы их выявления Проблемы пациента с гастродуоденитом и реализация программы сестринских вмешательств
Проблемы пациента с гастродуоденитом и реализация программы сестринских вмешательств Хроническая обструктивная болезнь легких (ХОБЛ)
Хроническая обструктивная болезнь легких (ХОБЛ) Центр реабилитации
Центр реабилитации Клеточные дистрофии. Накопление метаболитов в тканях
Клеточные дистрофии. Накопление метаболитов в тканях Анатомия и физиология сердца (лекция 4)
Анатомия и физиология сердца (лекция 4) Исторические аспекты формирования биомедицинской этики
Исторические аспекты формирования биомедицинской этики Гипотрофия
Гипотрофия Дэниел Киш. Ретинобластома
Дэниел Киш. Ретинобластома Проведение сестринского ухода во фтизиатрии
Проведение сестринского ухода во фтизиатрии Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review
Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review Гемобластозы и анемии
Гемобластозы и анемии Плоскоклеточный рак
Плоскоклеточный рак Оценка функционального состояния сердечно-сосудистой системы
Оценка функционального состояния сердечно-сосудистой системы