Содержание
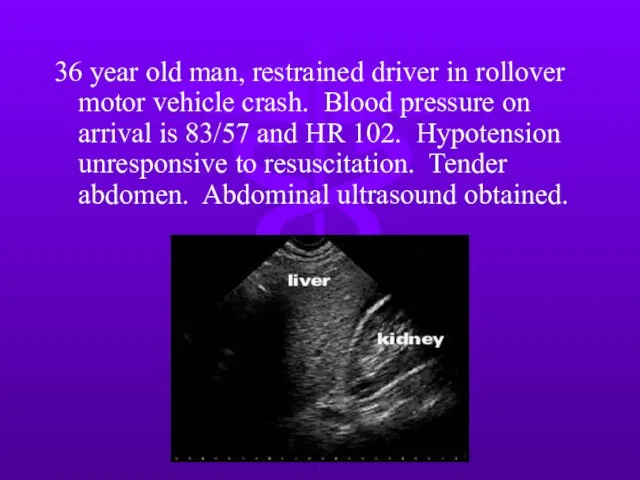
- 2. 36 year old man, restrained driver in rollover motor vehicle crash. Blood pressure on arrival is
- 3. Next step? Exploratory laparotomy Diagnostic peritoneal lavage Abdominal CT scan Serial observation
- 4. 28 y/o woman, unrestrained driver in a motor vehicle crash. Stable vital signs and LUQ tenderness,
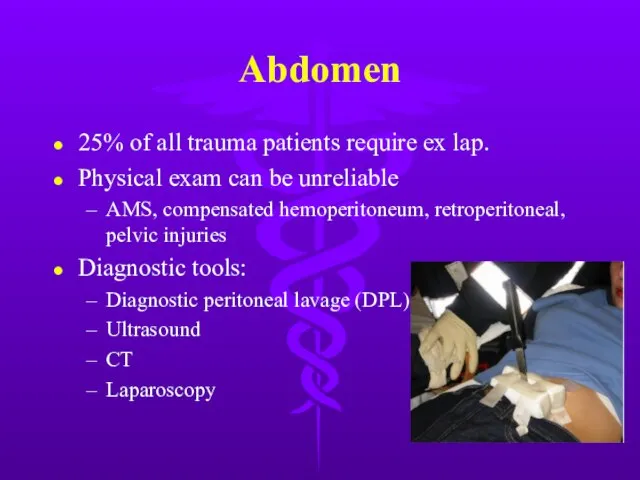
- 5. Abdomen 25% of all trauma patients require ex lap. Physical exam can be unreliable AMS, compensated
- 6. Diagnosis Test of choice dependent on hemodynamic stability and severity of associated injuries. Stable blunt trauma
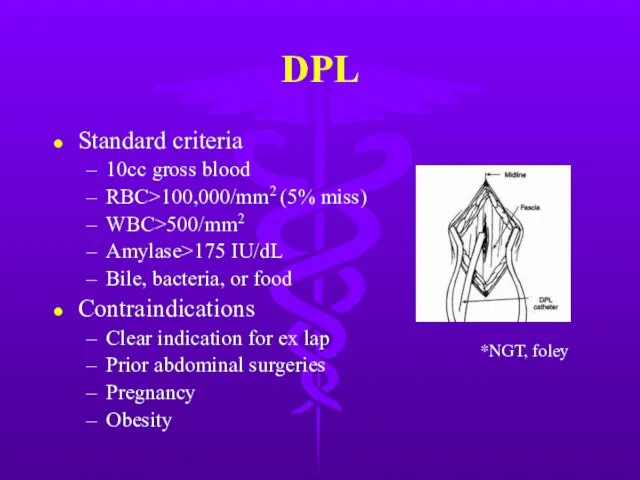
- 7. DPL Standard criteria 10cc gross blood RBC>100,000/mm2 (5% miss) WBC>500/mm2 Amylase>175 IU/dL Bile, bacteria, or food
- 8. DPL Highly sensitive to intraperitoneal blood, but low specificity → nontherapeutic explorations. Supraumbilical if pelvic fracture
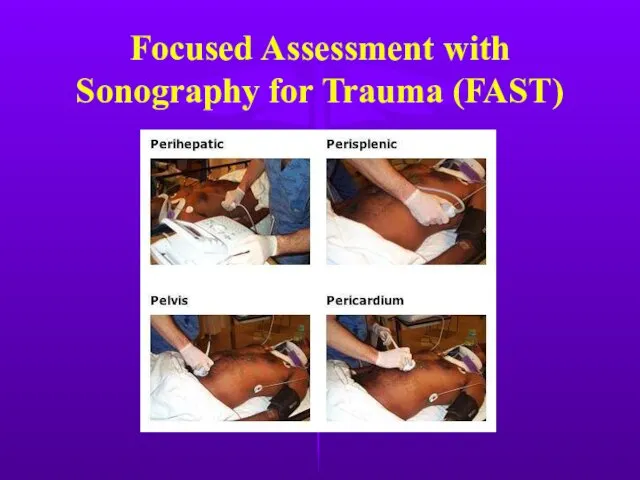
- 9. Focused Assessment with Sonography for Trauma (FAST)
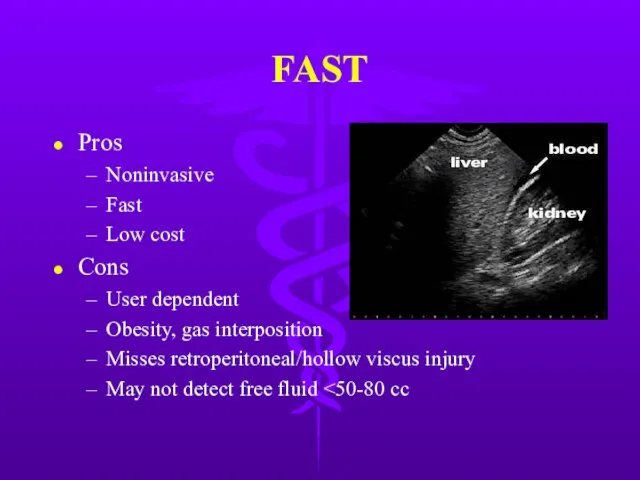
- 10. FAST Pros Noninvasive Fast Low cost Cons User dependent Obesity, gas interposition Misses retroperitoneal/hollow viscus injury
- 11. CT Scan Hemodynamically stable patient Pros Retroperitoneal assessment Nonoperative management of solid organ injury High specificity
- 12. Laparoscopy Role still being defined Good for diaphragm injury evaluation Cons Invasive Expensive Missed small bowel,
- 13. Gastric Injury Mostly penetrating trauma. Including iatrogenic injury from CPR NGT + aspirate for blood Intraop
- 14. Gastric Injury Post-op complications Bleeding, abscesses, gastric fistula, empyema Recent meal → neutralization of gastric acidity
- 15. Duodenal Injury Majority due to penetrating trauma. Blunt injury usually secondary to steering wheel blow to
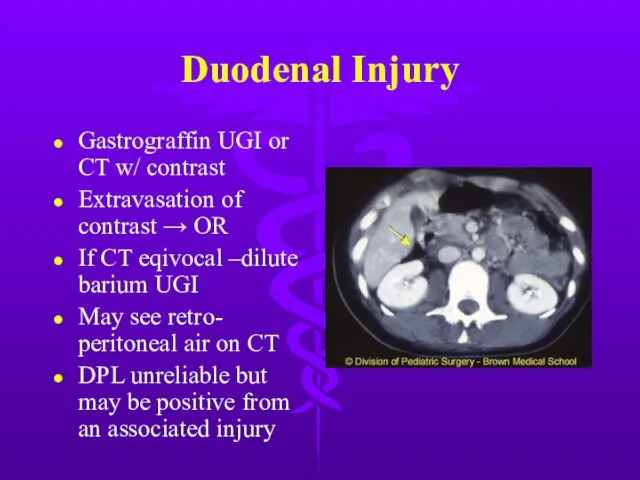
- 16. Duodenal Injury Gastrograffin UGI or CT w/ contrast Extravasation of contrast → OR If CT eqivocal
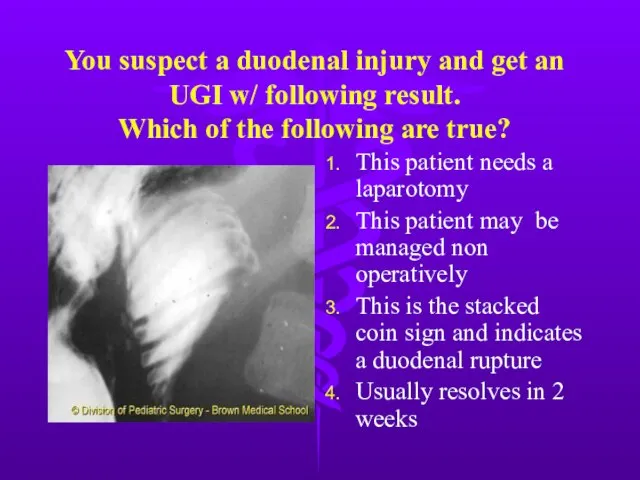
- 17. You suspect a duodenal injury and get an UGI w/ following result. Which of the following
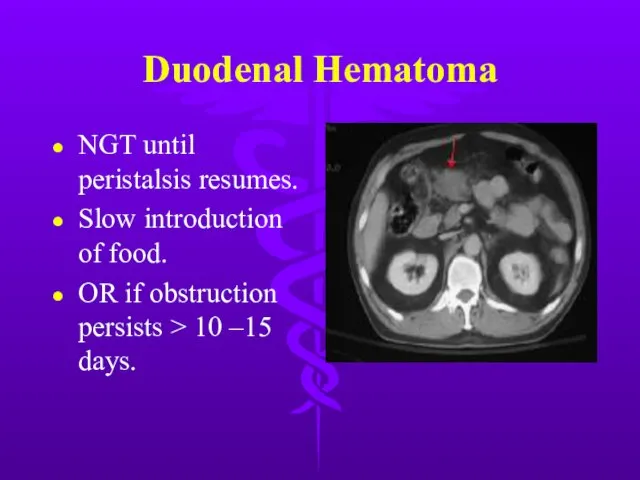
- 18. Duodenal Hematoma NGT until peristalsis resumes. Slow introduction of food. OR if obstruction persists > 10
- 19. Duodenal Injury Appropriate repair depends on injury severity and elapsed time 80-85% can be primarily repaired.
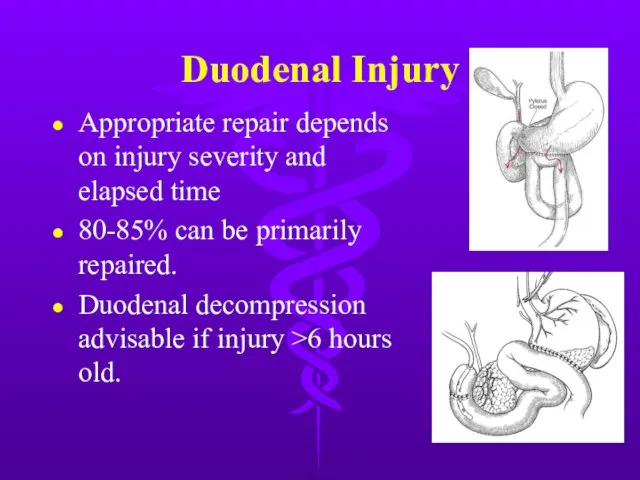
- 20. The upper abdomen of a 42 y/o male strikes the steering wheel during a MVA. After
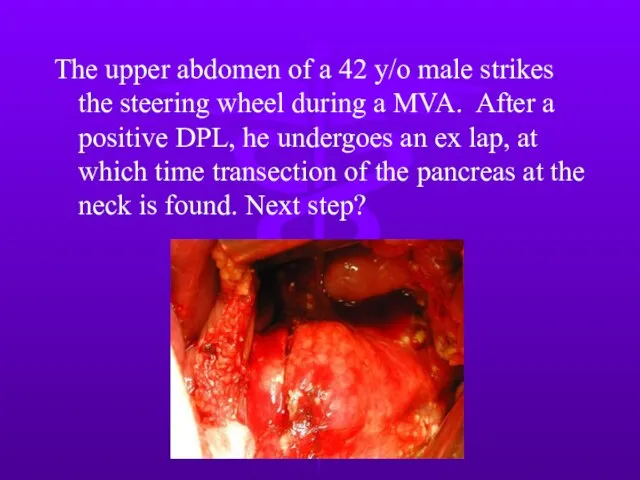
- 21. Next step? Distal pancreatectomy with oversewing and drainage of proximal stump. Primary repair and drainage of
- 23. Pancreatic Injury Rare 10-12% of abdominal injuries, but mortality 10-25%, mostly from associated intra-abd injury Most
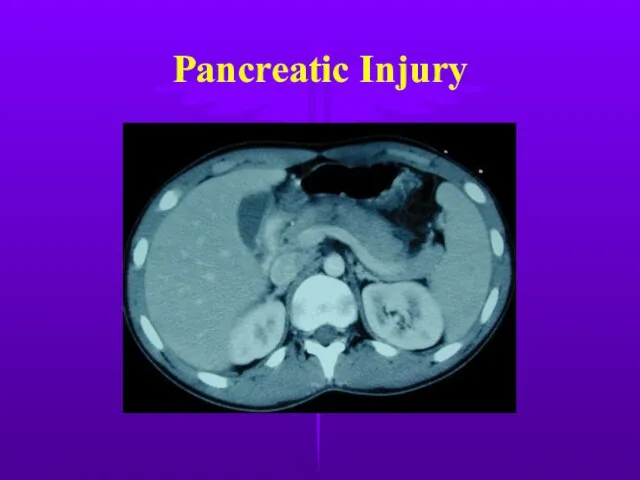
- 24. Pancreatic Injury
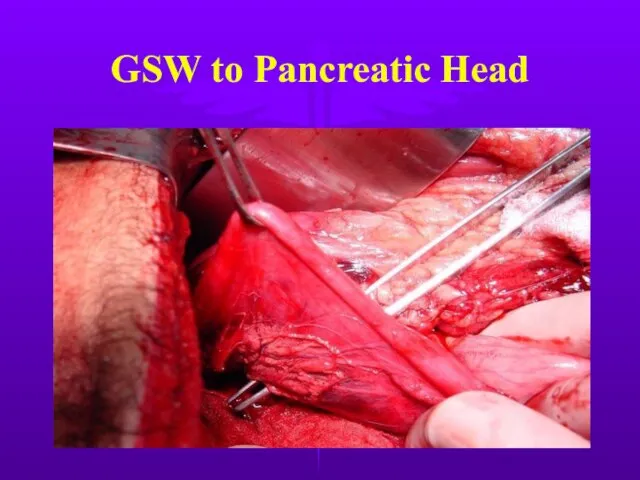
- 25. GSW to Pancreatic Head
- 26. Pancreatic Injury Divided into proximal or distal according to location on the R or L of
- 27. Complications after Pancreatic Trauma High complication rate 35-40% Most common are pancreatic fistulas & abscesses Most
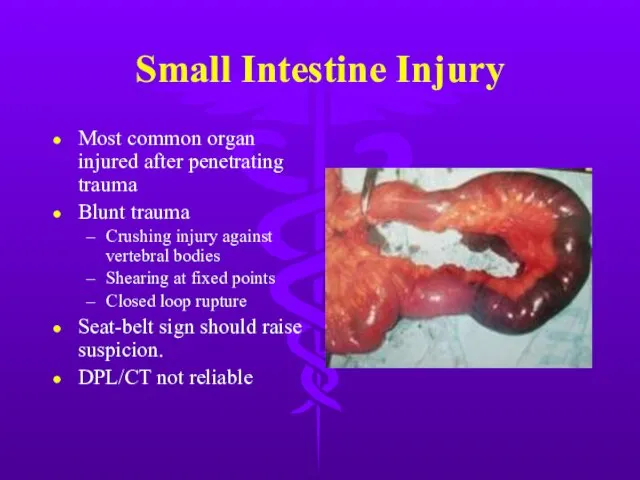
- 28. Small Intestine Injury Most common organ injured after penetrating trauma Blunt trauma Crushing injury against vertebral
- 29. Small Intestine Injury
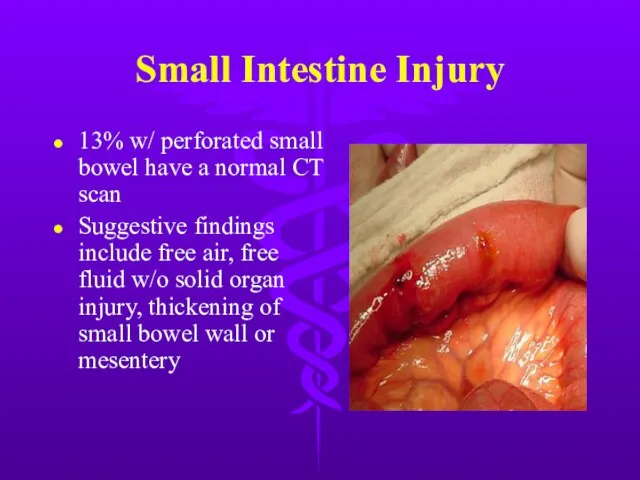
- 30. Small Intestine Injury 13% w/ perforated small bowel have a normal CT scan Suggestive findings include
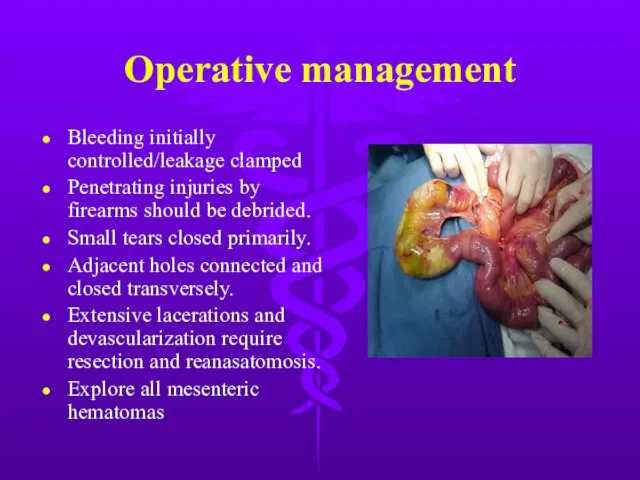
- 31. Operative management Bleeding initially controlled/leakage clamped Penetrating injuries by firearms should be debrided. Small tears closed
- 32. Colon Injury Second most frequent injured organ, usually from penetrating trauma Repair within 2 hours dramatically
- 33. Colon Injury Primary repair criteria Early diagnosis (within 4-6 hours) Absence of prolonged shock/hypotension Absence of
- 34. Rectal Injury Most from GSW Other causes - foreign body, impalement, pelvic fractures, and iatrogenic Lower
- 35. Rectal Injury Extraperitoneal injury Primary closure Diverting colostomy Washout of rectal stump Wide presacral drainage Intraperitoneal
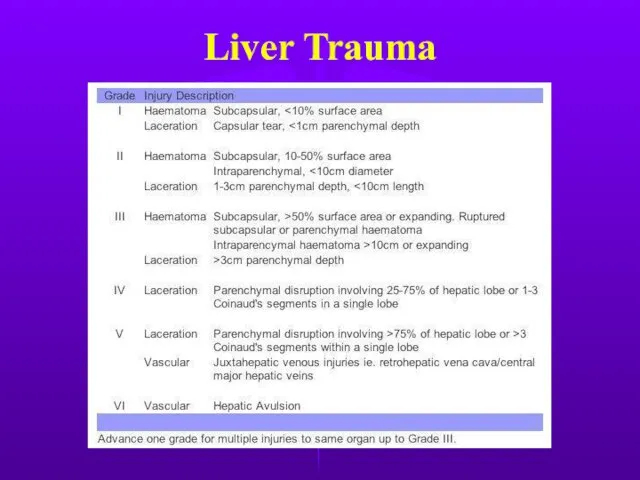
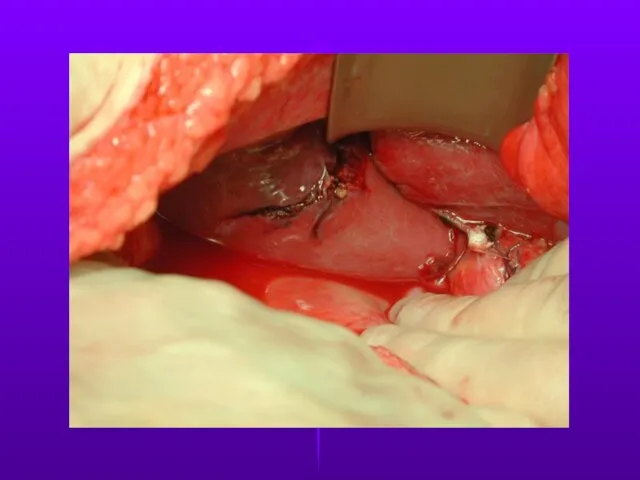
- 36. Liver Trauma Frequently injured in both blunt & penetrating trauma. Control of profuse bleeding from deep
- 37. Liver Trauma
- 38. Liver Trauma
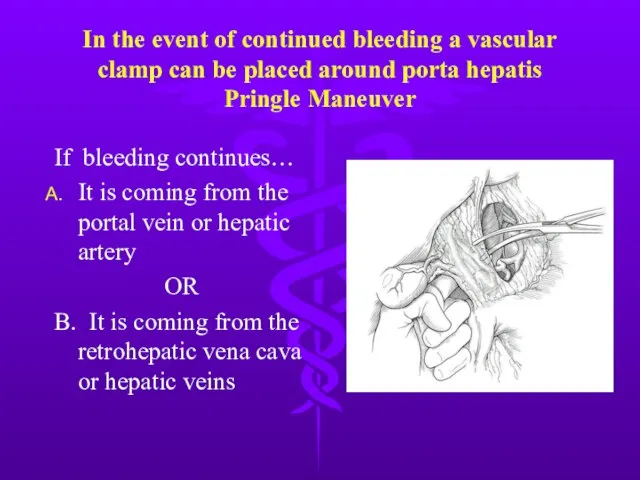
- 39. In the event of continued bleeding a vascular clamp can be placed around porta hepatis Pringle
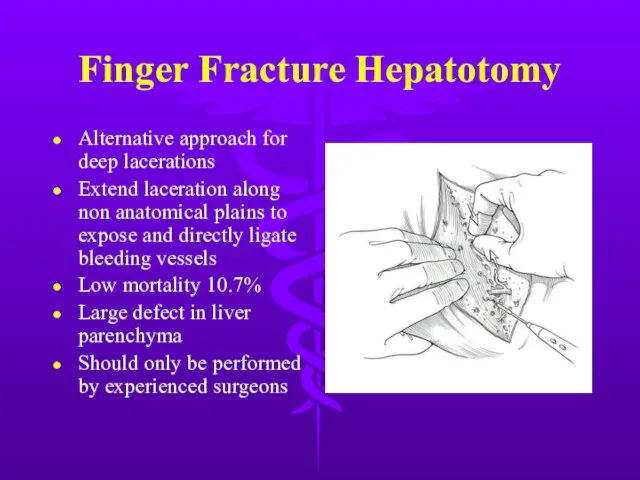
- 40. Finger Fracture Hepatotomy Alternative approach for deep lacerations Extend laceration along non anatomical plains to expose
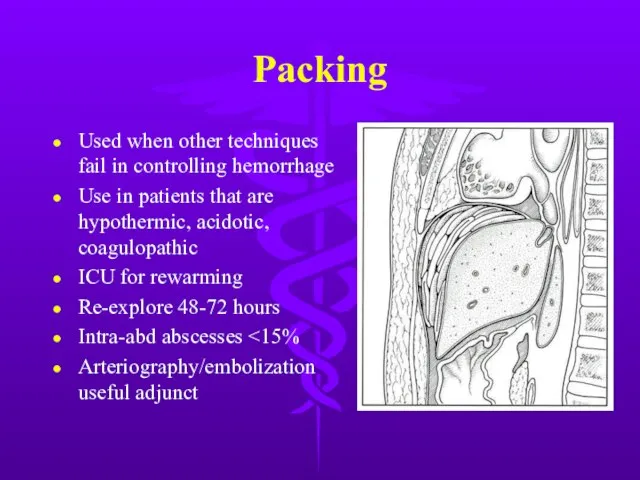
- 41. Packing Used when other techniques fail in controlling hemorrhage Use in patients that are hypothermic, acidotic,
- 42. Of the following hemodynamically stable patients, who is most likely to fail non-operative management. 8 y/o
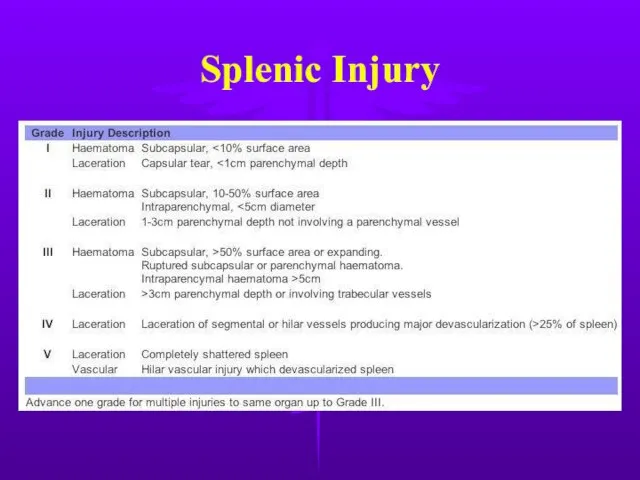
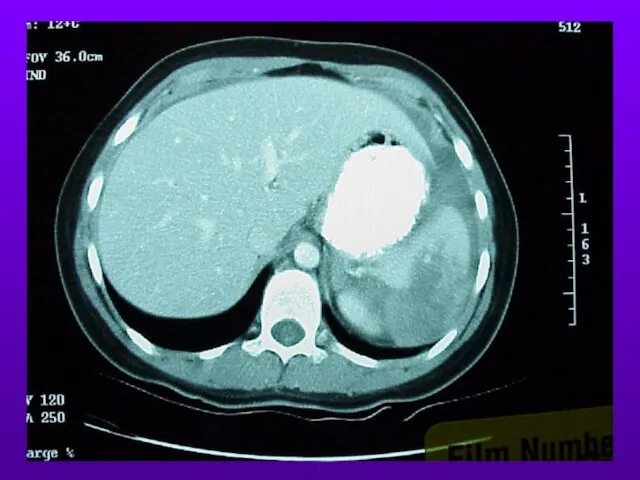
- 43. Splenic Injury Most frequently injured intra-abdominal organ in blunt trauma. Splenic preservation when possible OPSI (0.6%
- 44. Splenic Injury Nonoperative criteria Hemodynamic stability Negative abdominal examination Absence of contrast extravasation Angiography/embolization an option
- 45. Splenic Injury
- 46. Splenic Injury
- 47. Splenic Injury
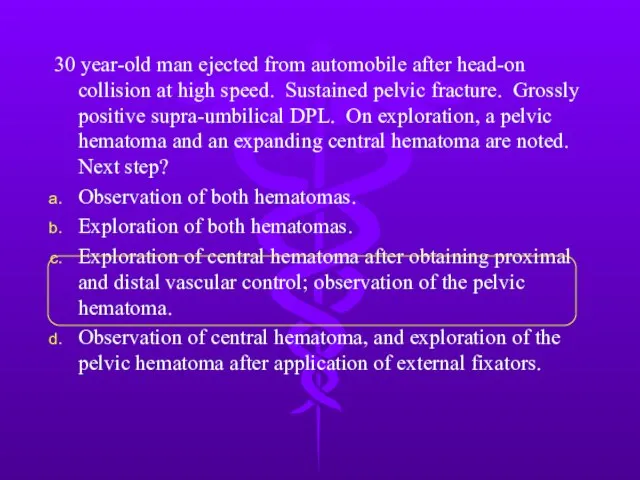
- 48. 30 year-old man ejected from automobile after head-on collision at high speed. Sustained pelvic fracture. Grossly
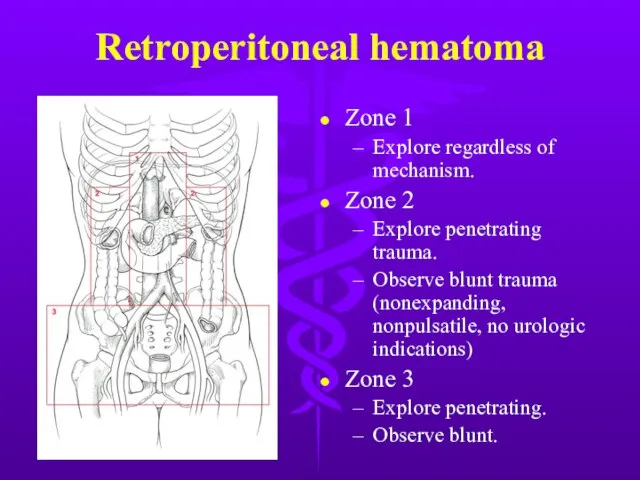
- 49. Retroperitoneal hematoma Zone 1 Explore regardless of mechanism. Zone 2 Explore penetrating trauma. Observe blunt trauma
- 50. Damage Control Abbreviated laparotomy and temporary packing Effort to blunt physiologic response to shock and hemorrhage
- 51. Damage Control
- 52. 30 y/o woman sustained crushing injury to right lower leg. Arrived at hospital 12 hours later.
- 53. Compartment Syndrome Common in forearm and lower leg secondary to defined fascial boundaries. Four Ps: pressure,
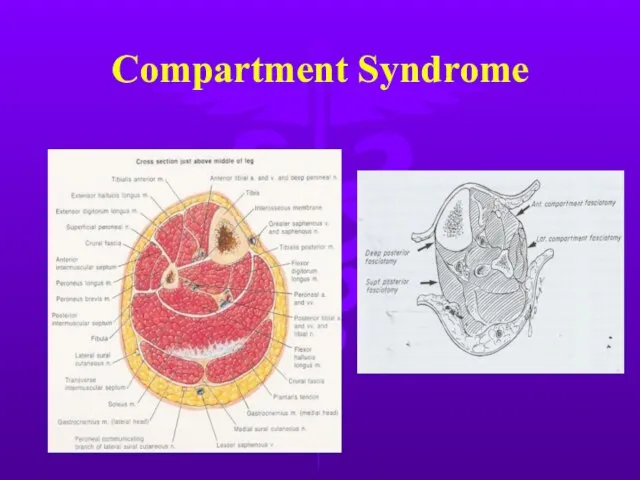
- 54. Compartment Syndrome
- 55. Fasciotomy
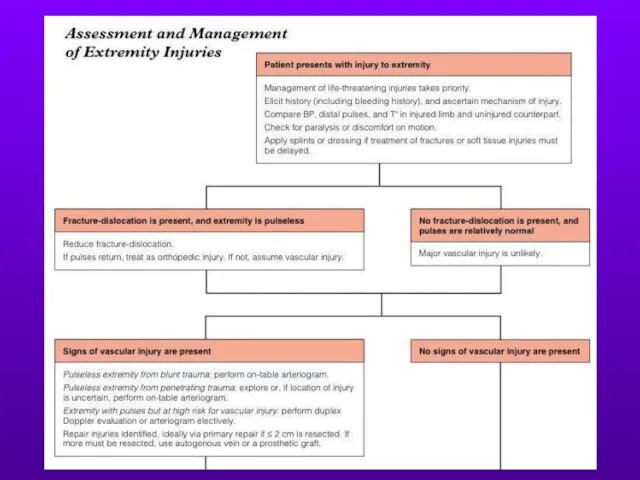
- 56. Extremity Injuries
- 57. With regard to cervical spine injury, which of the following is/are true? Jefferson fractures (C1) are
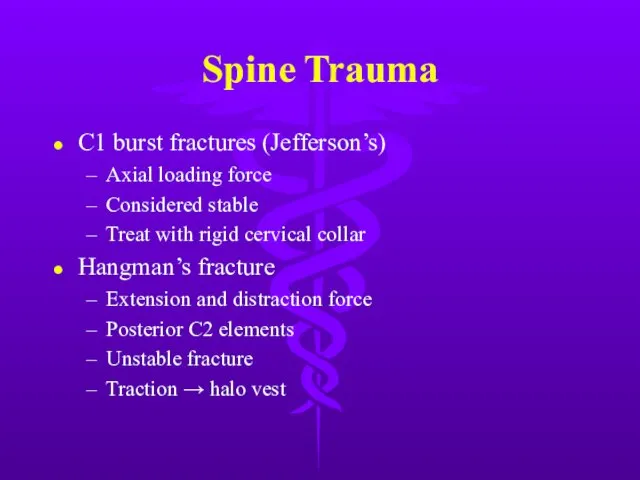
- 58. Spine Trauma C1 burst fractures (Jefferson’s) Axial loading force Considered stable Treat with rigid cervical collar
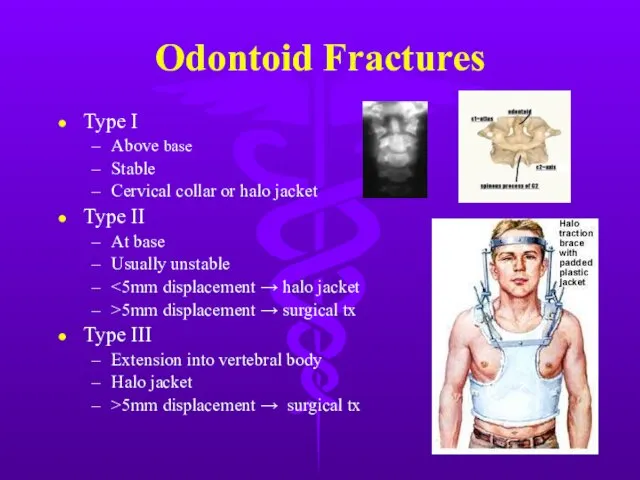
- 59. Odontoid Fractures Type I Above base Stable Cervical collar or halo jacket Type II At base
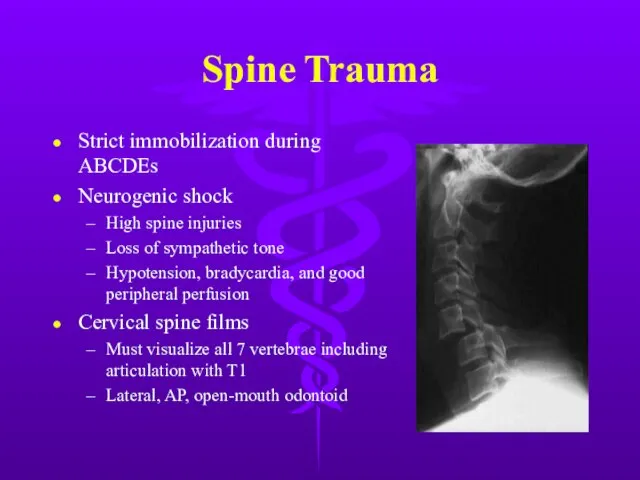
- 60. Spine Trauma Strict immobilization during ABCDEs Neurogenic shock High spine injuries Loss of sympathetic tone Hypotension,
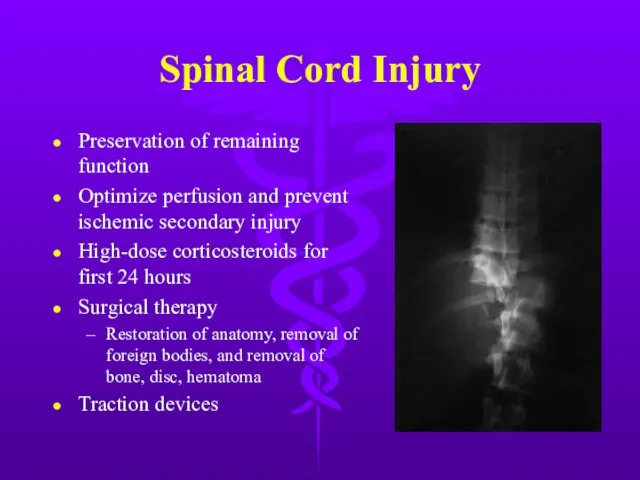
- 61. Spinal Cord Injury Preservation of remaining function Optimize perfusion and prevent ischemic secondary injury High-dose corticosteroids
- 63. Скачать презентацию






 День рождения Влада
День рождения Влада Модернизация уличного освещения с. Вешкелица, Суоярвского района, Республики Карелия
Модернизация уличного освещения с. Вешкелица, Суоярвского района, Республики Карелия STAYING LEAN: A CHALLENGE FOR BIGGER COMPANIES
STAYING LEAN: A CHALLENGE FOR BIGGER COMPANIES Строение и значение нервной системы
Строение и значение нервной системы Нормативно-правовые основы и порядок оформления документов на выдачу музейных предметов для передвижных выставок
Нормативно-правовые основы и порядок оформления документов на выдачу музейных предметов для передвижных выставок Как мы провели лето
Как мы провели лето Вождение коротких модулей
Вождение коротких модулей  Народный инструмент Башкортостана Курай
Народный инструмент Башкортостана Курай Формирование основ сохранения здоровья средствами художественного слова
Формирование основ сохранения здоровья средствами художественного слова Презентация на тему Виды информационных технологий
Презентация на тему Виды информационных технологий Формула дивана
Формула дивана Галерея душевых Dushllery
Галерея душевых Dushllery Образовательная площадка Мониторинг и отчет по ПРДСО
Образовательная площадка Мониторинг и отчет по ПРДСО Обучение техники бега с низкого старт
Обучение техники бега с низкого старт 65-ой годовщине прорыва ленинградской блокады посвящается
65-ой годовщине прорыва ленинградской блокады посвящается Государственная услуга по организации профессиональной ориентации
Государственная услуга по организации профессиональной ориентации Проект ZOOйога (старший дошкольный возраст)
Проект ZOOйога (старший дошкольный возраст) Понятие товара в налоговом праве
Понятие товара в налоговом праве Экология Сузюмов А.В
Экология Сузюмов А.В ВЫБЕРИТЕ ПРАВИЛЬНЫЙ ОТВЕТ.
ВЫБЕРИТЕ ПРАВИЛЬНЫЙ ОТВЕТ.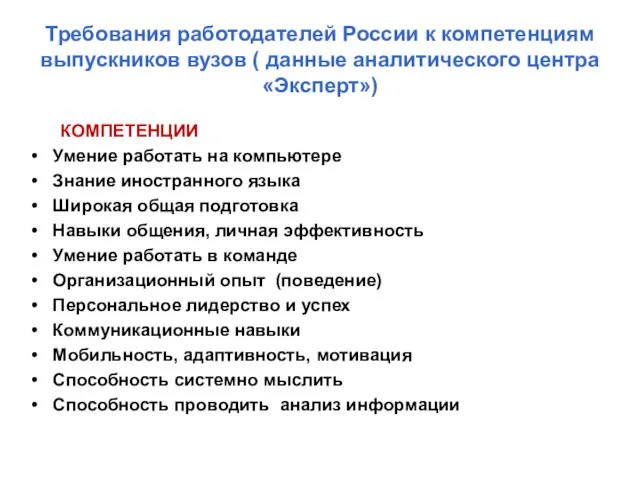 Требования работодателей России к компетенциям выпускников вузов ( данные аналитического центра «Эксперт»)
Требования работодателей России к компетенциям выпускников вузов ( данные аналитического центра «Эксперт») Макролон 1239 в производстве возвратных бутылей для воды (18.9 л)
Макролон 1239 в производстве возвратных бутылей для воды (18.9 л) Понятие о географии населения. Численность и воспроизводство населения
Понятие о географии населения. Численность и воспроизводство населения Датчики-реле давления ДЕМ-РАСКО
Датчики-реле давления ДЕМ-РАСКО Менеджмент качества и конкурентоспособность организации
Менеджмент качества и конкурентоспособность организации Тест по теме «Информация. Информационные процессы»
Тест по теме «Информация. Информационные процессы» Շառլ Ազնավուր
Շառլ Ազնավուր Игра в черное и белое
Игра в черное и белое