Слайд 211/12/02
Lubna Piracha, D.O.
What is a Murmur?
It maybe a normal or abnormal sound
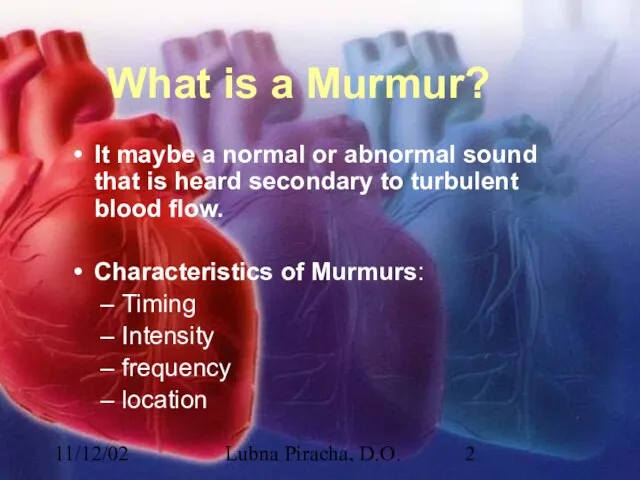
that is heard secondary to turbulent blood flow.
Characteristics of Murmurs:
Timing
Intensity
frequency
location
Слайд 311/12/02
Lubna Piracha, D.O.
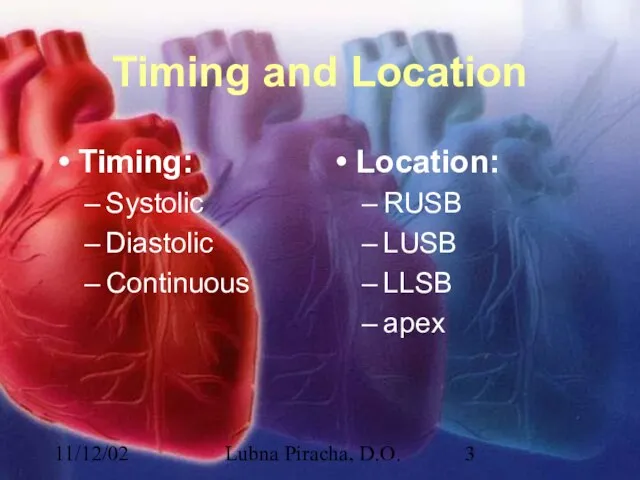
Timing and Location
Timing:
Systolic
Diastolic
Continuous
Location:
RUSB
LUSB
LLSB
apex
Слайд 411/12/02
Lubna Piracha, D.O.
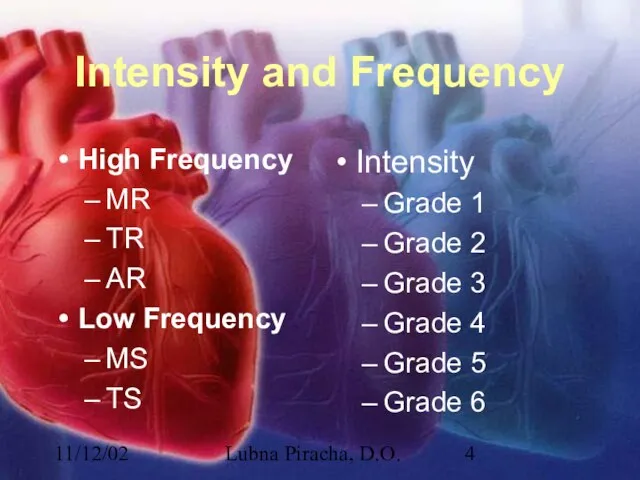
Intensity and Frequency
High Frequency
MR
TR
AR
Low Frequency
MS
TS
Intensity
Grade 1
Grade 2
Grade 3
Grade 4
Grade
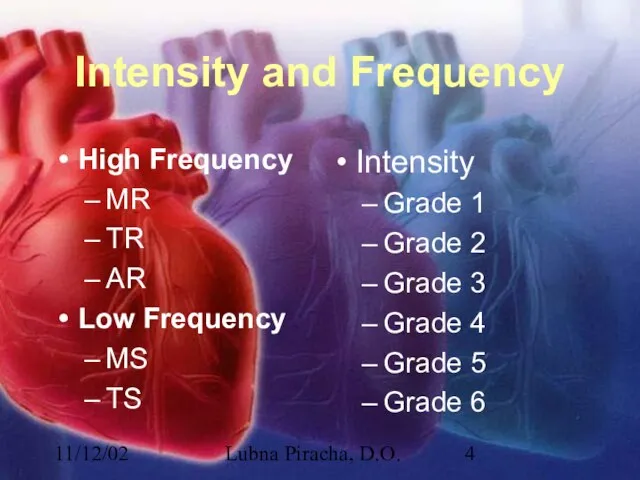
5
Grade 6
Слайд 511/12/02
Lubna Piracha, D.O.
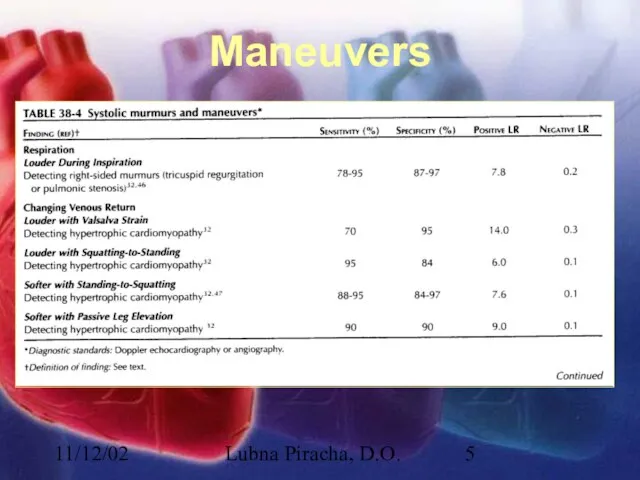
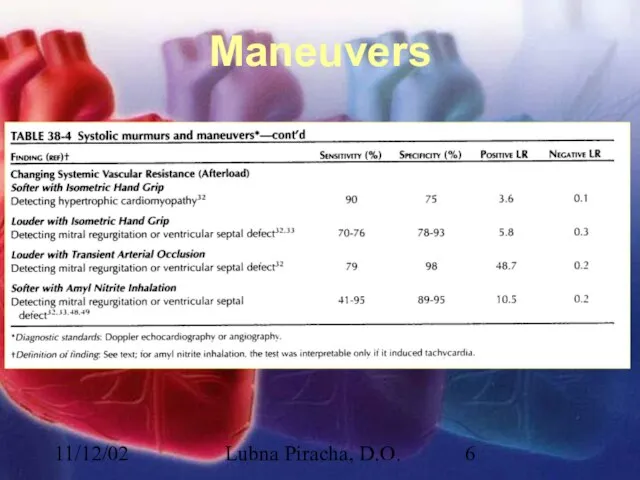
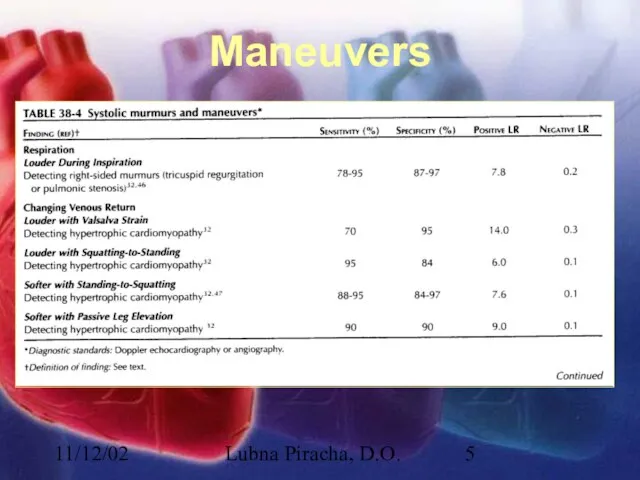
Maneuvers
Слайд 611/12/02
Lubna Piracha, D.O.
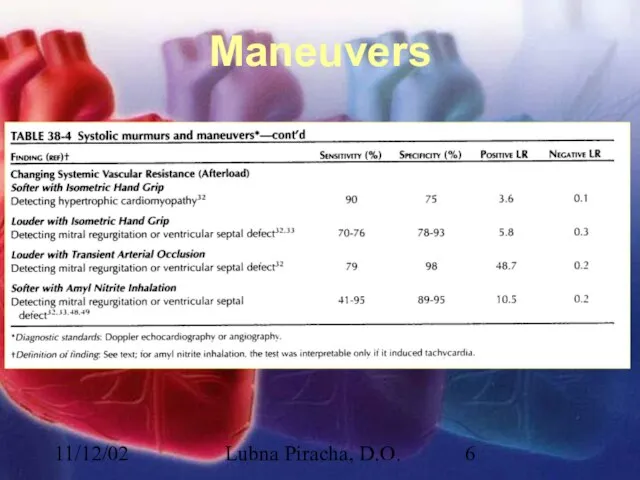
Maneuvers
Слайд 711/12/02
Lubna Piracha, D.O.
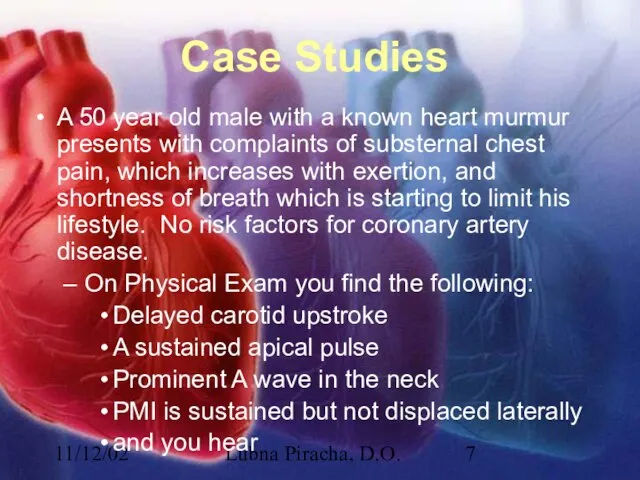
Case Studies
A 50 year old male with a known heart
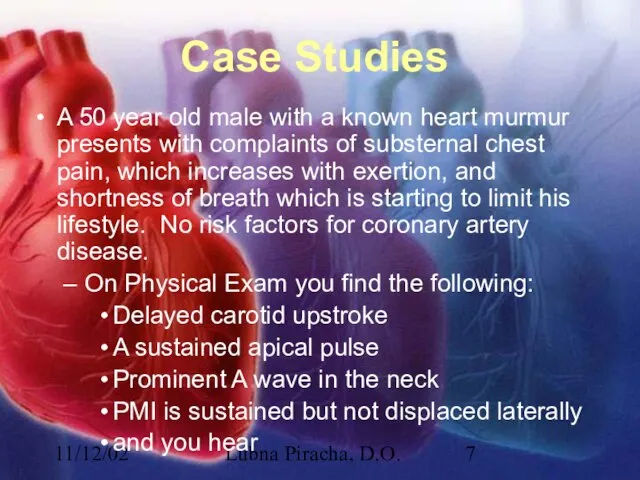
murmur presents with complaints of substernal chest pain, which increases with exertion, and shortness of breath which is starting to limit his lifestyle. No risk factors for coronary artery disease.
On Physical Exam you find the following:
Delayed carotid upstroke
A sustained apical pulse
Prominent A wave in the neck
PMI is sustained but not displaced laterally
and you hear
Слайд 811/12/02
Lubna Piracha, D.O.
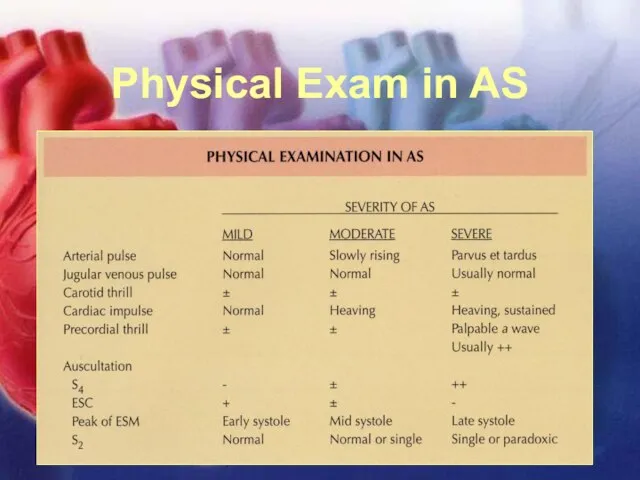
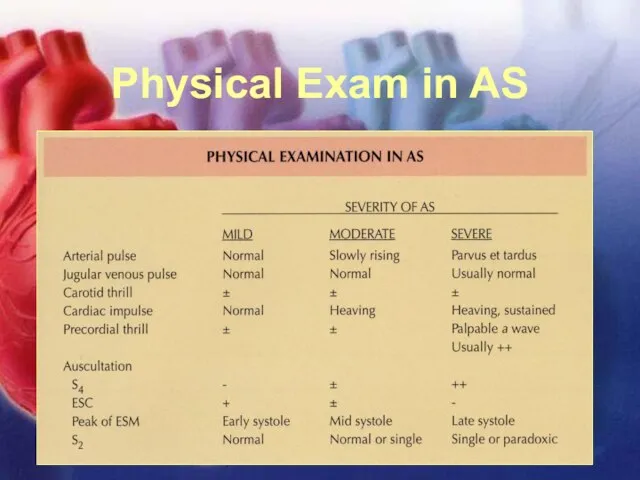
Physical Exam in AS
Слайд 911/12/02
Lubna Piracha, D.O.
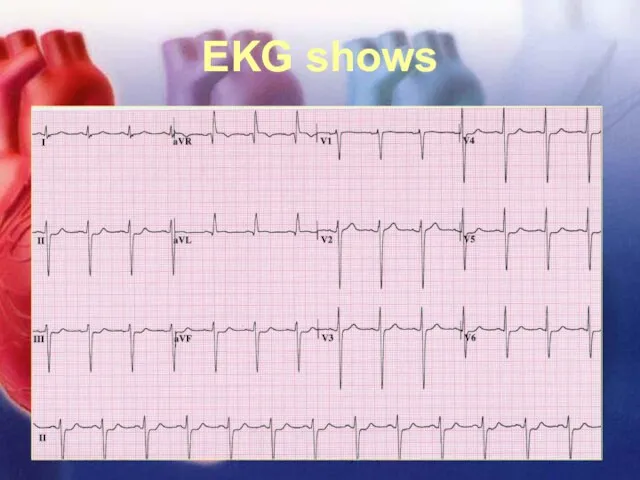
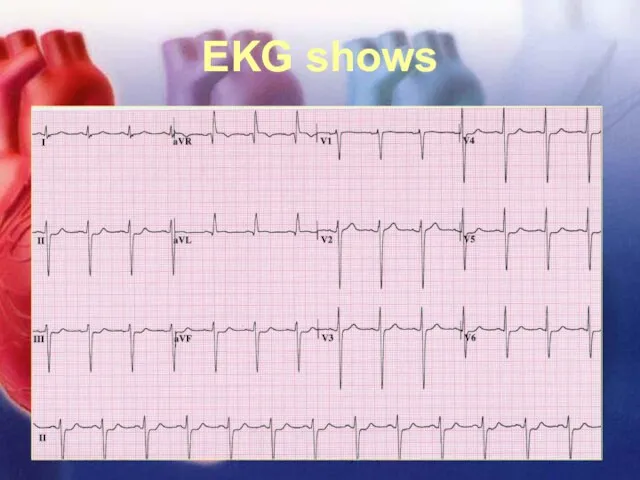
EKG shows
Слайд 1011/12/02
Lubna Piracha, D.O.
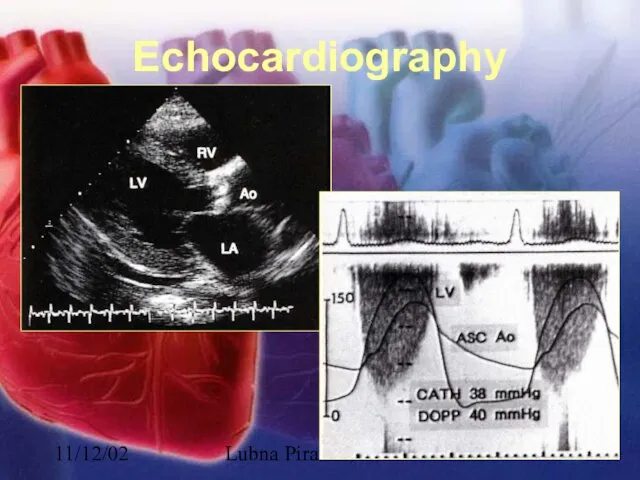
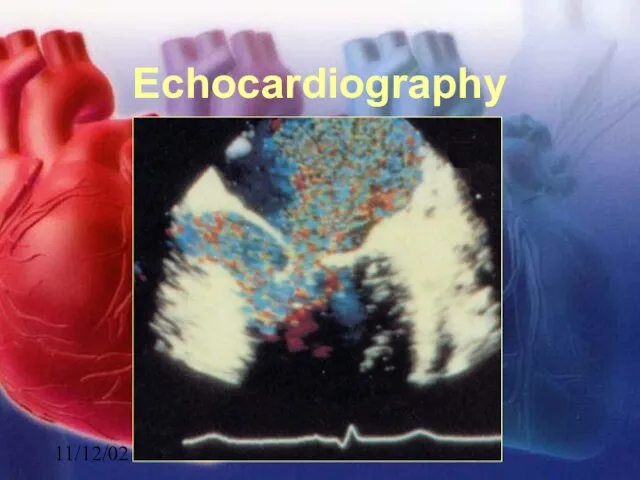
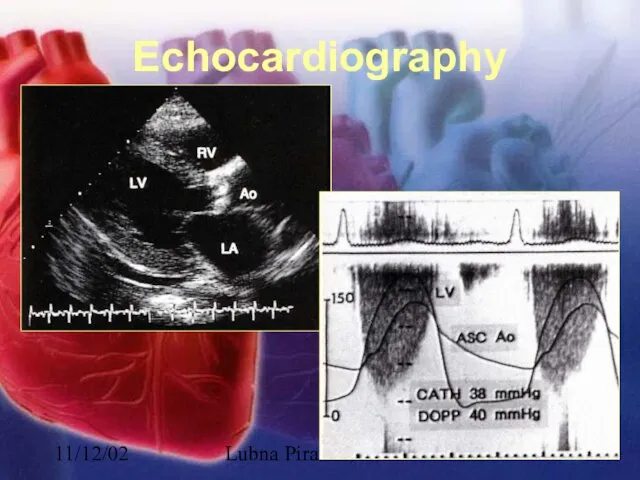
Echocardiography
Слайд 1111/12/02
Lubna Piracha, D.O.
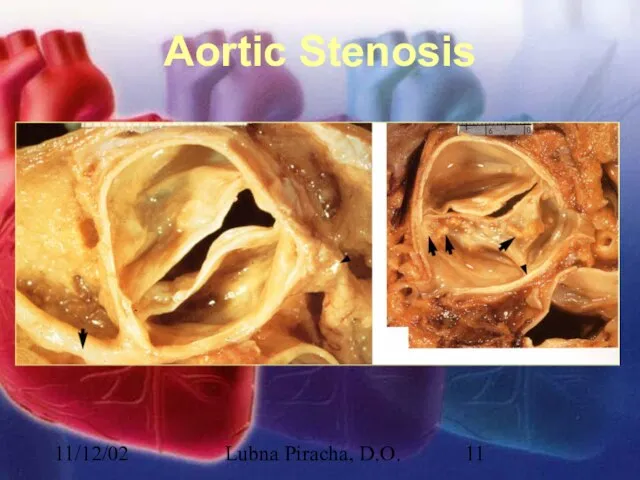
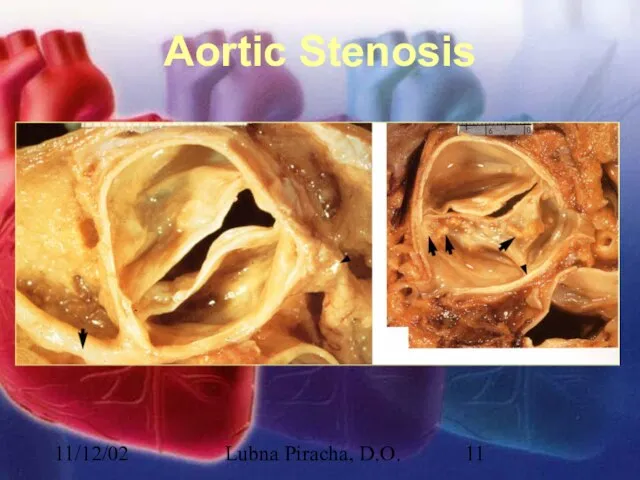
Aortic Stenosis
Слайд 1211/12/02
Lubna Piracha, D.O.
Aortic Stenosis
There is little hemodynamic disturbance that occurs as the
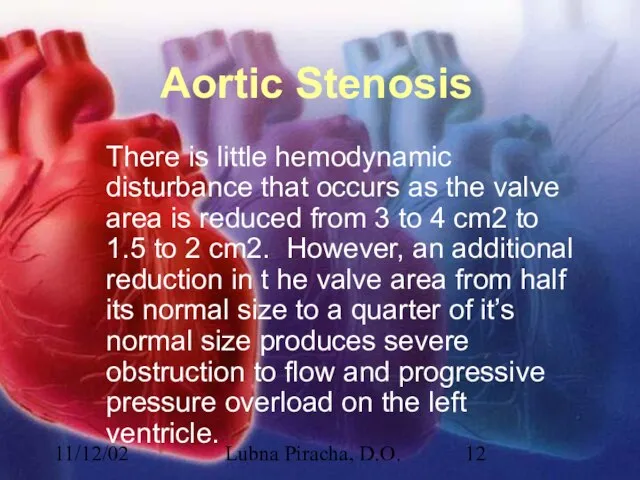
valve area is reduced from 3 to 4 cm2 to 1.5 to 2 cm2. However, an additional reduction in t he valve area from half its normal size to a quarter of it’s normal size produces severe obstruction to flow and progressive pressure overload on the left ventricle.
Слайд 1311/12/02
Lubna Piracha, D.O.
Aortic Stenosis continued:
Concentric hypertrophy develops in response to this overload.
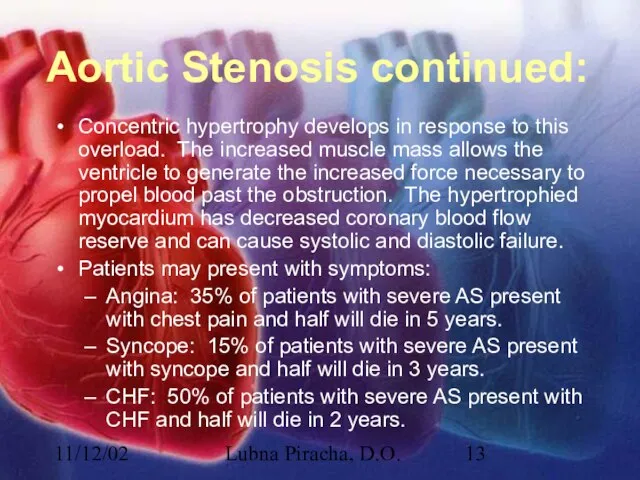
The increased muscle mass allows the ventricle to generate the increased force necessary to propel blood past the obstruction. The hypertrophied myocardium has decreased coronary blood flow reserve and can cause systolic and diastolic failure.
Patients may present with symptoms:
Angina: 35% of patients with severe AS present with chest pain and half will die in 5 years.
Syncope: 15% of patients with severe AS present with syncope and half will die in 3 years.
CHF: 50% of patients with severe AS present with CHF and half will die in 2 years.
Слайд 1411/12/02
Lubna Piracha, D.O.
Case Study:
A 45 year old male with a history of
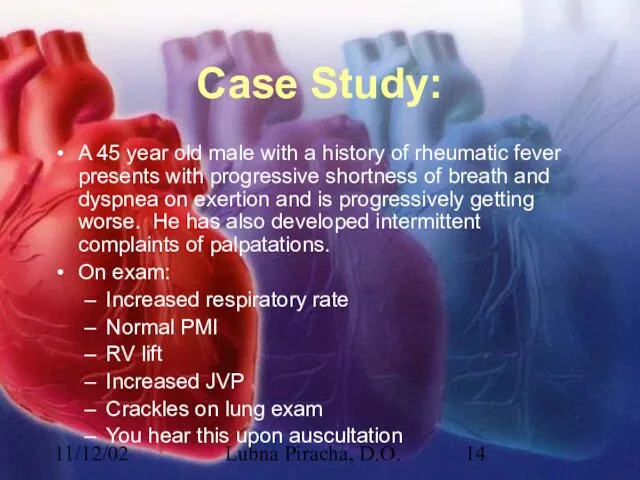
rheumatic fever presents with progressive shortness of breath and dyspnea on exertion and is progressively getting worse. He has also developed intermittent complaints of palpatations.
On exam:
Increased respiratory rate
Normal PMI
RV lift
Increased JVP
Crackles on lung exam
You hear this upon auscultation
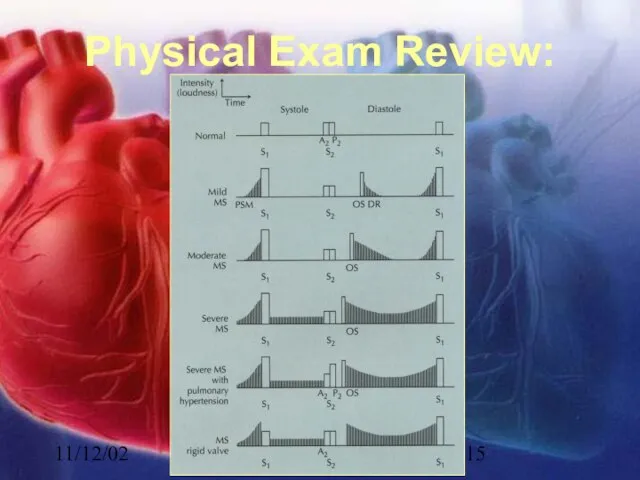
Слайд 1511/12/02
Lubna Piracha, D.O.
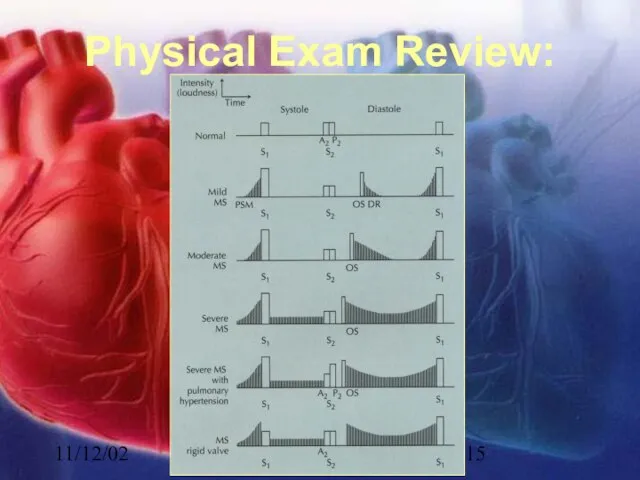
Physical Exam Review:
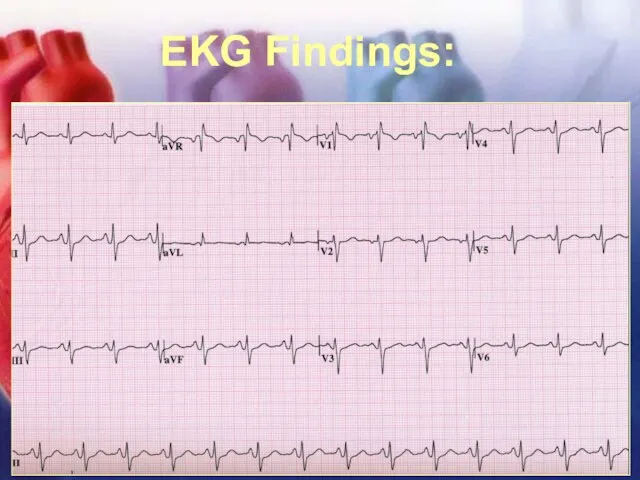
Слайд 1611/12/02
Lubna Piracha, D.O.
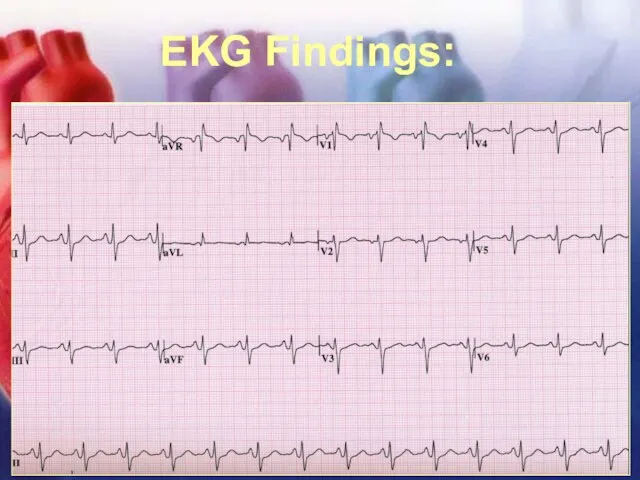
EKG Findings:
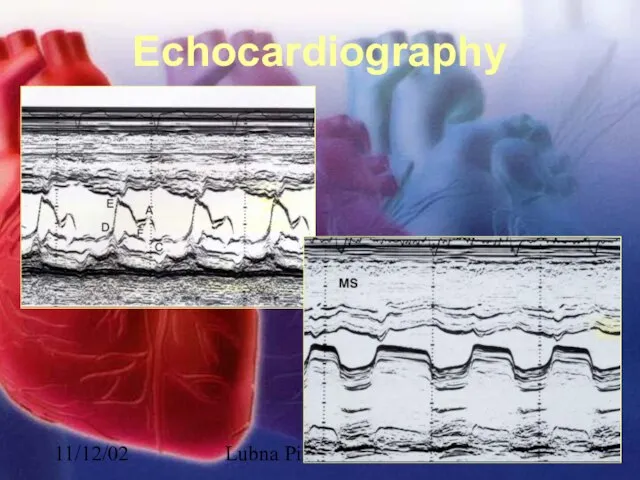
Слайд 1711/12/02
Lubna Piracha, D.O.
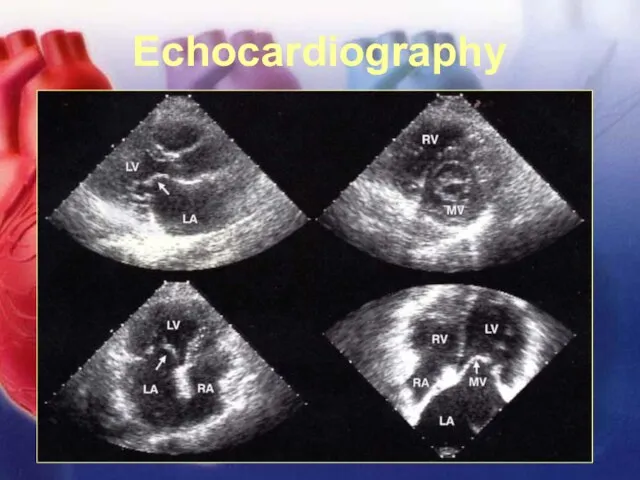
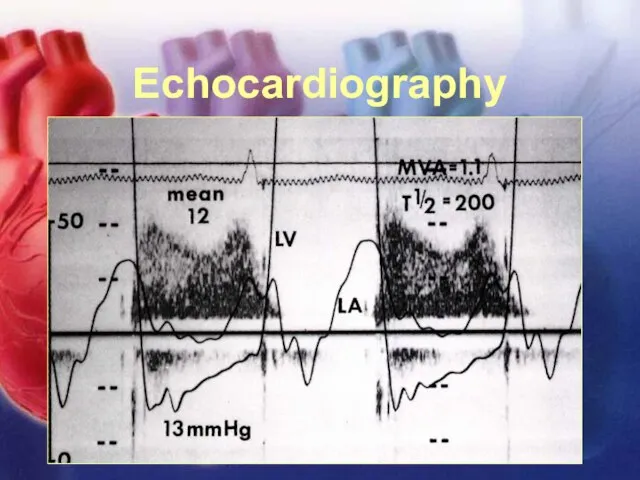
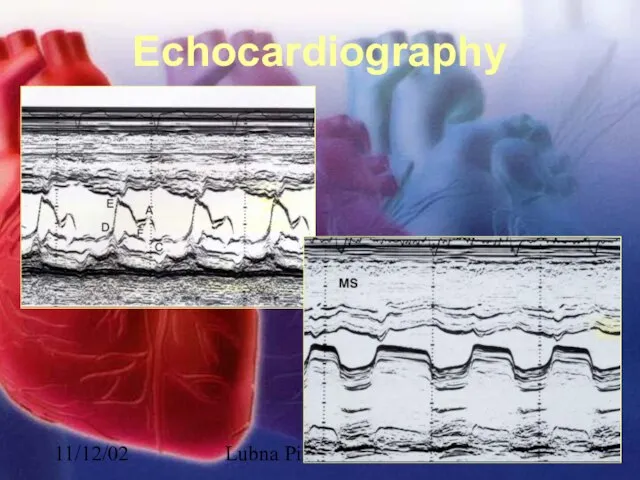
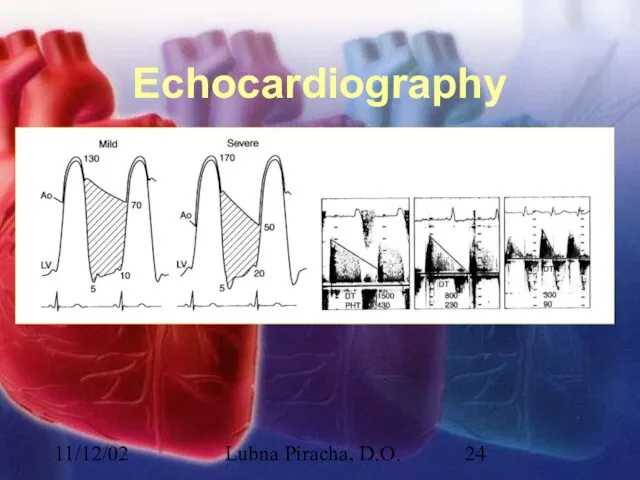
Echocardiography
Слайд 1811/12/02
Lubna Piracha, D.O.
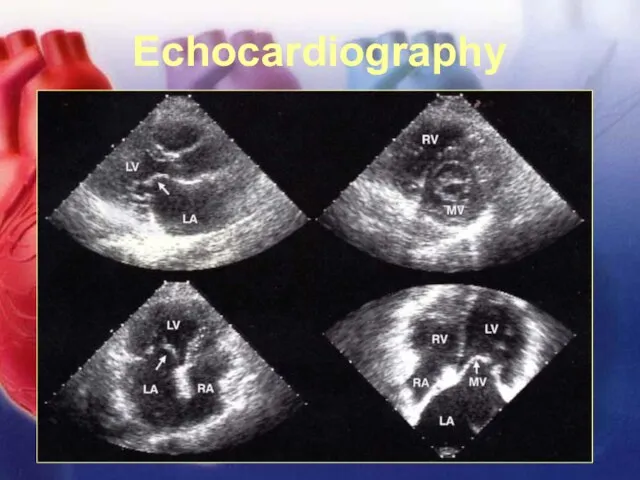
Echocardiography
Слайд 1911/12/02
Lubna Piracha, D.O.
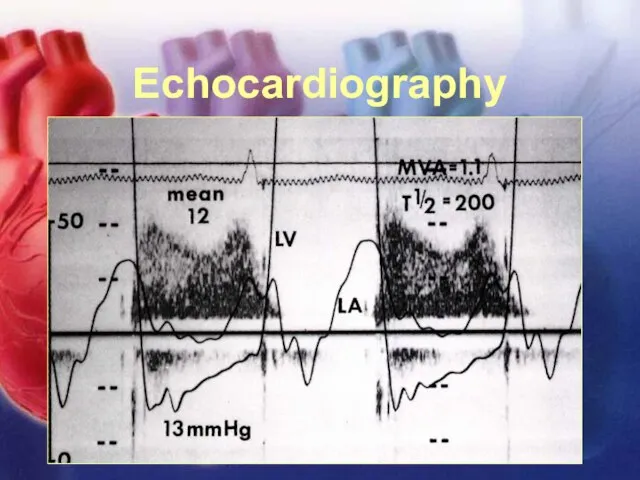
Echocardiography
Слайд 2011/12/02
Lubna Piracha, D.O.
Mitral Stenosis
In severe mitral stenosis the left ventricle is
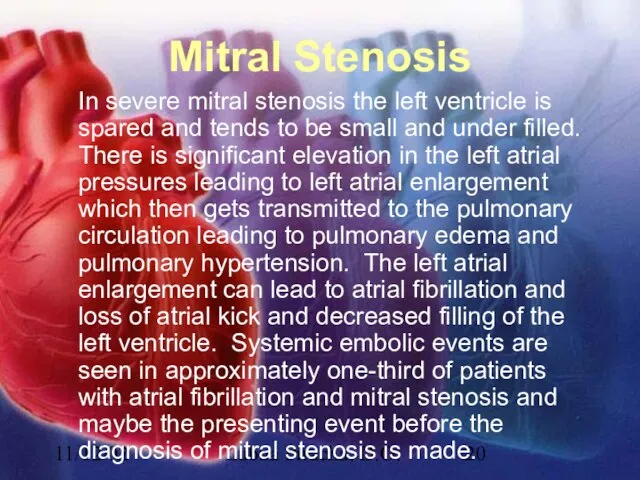
spared and tends to be small and under filled. There is significant elevation in the left atrial pressures leading to left atrial enlargement which then gets transmitted to the pulmonary circulation leading to pulmonary edema and pulmonary hypertension. The left atrial enlargement can lead to atrial fibrillation and loss of atrial kick and decreased filling of the left ventricle. Systemic embolic events are seen in approximately one-third of patients with atrial fibrillation and mitral stenosis and maybe the presenting event before the diagnosis of mitral stenosis is made.
Слайд 2111/12/02
Lubna Piracha, D.O.
Case Studies:
A 52 year old female presents with complaints of
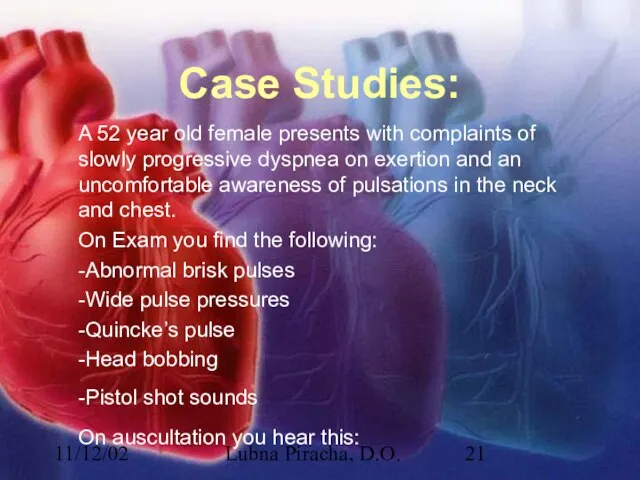
slowly progressive dyspnea on exertion and an uncomfortable awareness of pulsations in the neck and chest.
On Exam you find the following:
-Abnormal brisk pulses
-Wide pulse pressures
-Quincke’s pulse
-Head bobbing
-Pistol shot sounds
On auscultation you hear this:
Слайд 2211/12/02
Lubna Piracha, D.O.
Physical Exam Review
Early diastolic murmur of regurgitation
blowing, and high frequency,
and decrescendo in shape.
Systolic aortic flow murmur
Austin flint murmur
Слайд 2311/12/02
Lubna Piracha, D.O.
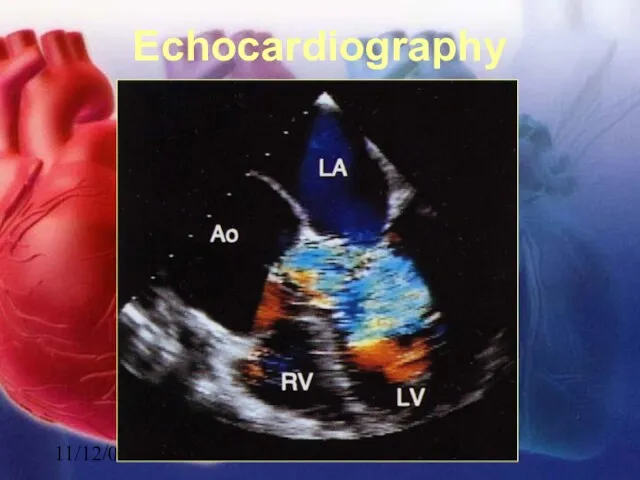
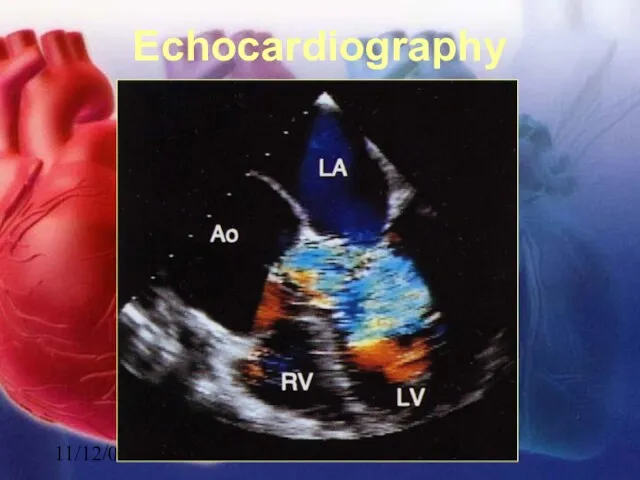
Echocardiography
Слайд 2411/12/02
Lubna Piracha, D.O.
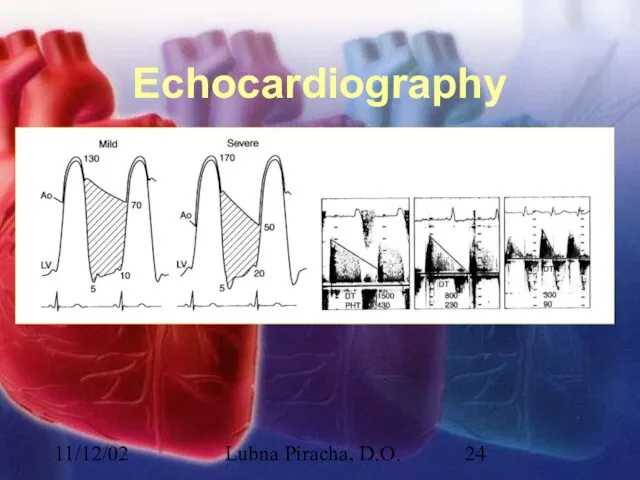
Echocardiography
Слайд 2511/12/02
Lubna Piracha, D.O.
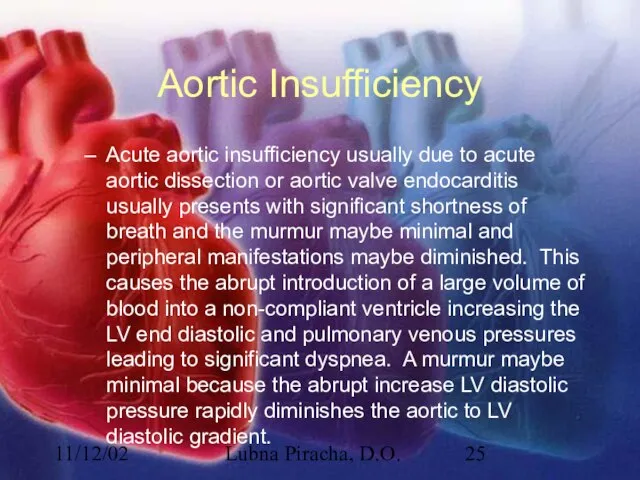
Aortic Insufficiency
Acute aortic insufficiency usually due to acute aortic dissection
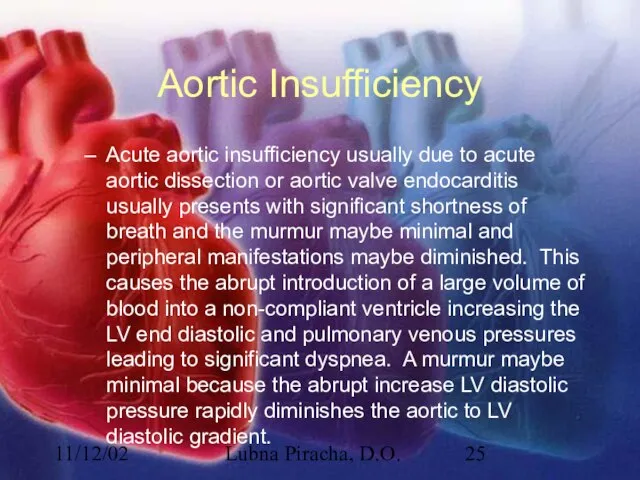
or aortic valve endocarditis usually presents with significant shortness of breath and the murmur maybe minimal and peripheral manifestations maybe diminished. This causes the abrupt introduction of a large volume of blood into a non-compliant ventricle increasing the LV end diastolic and pulmonary venous pressures leading to significant dyspnea. A murmur maybe minimal because the abrupt increase LV diastolic pressure rapidly diminishes the aortic to LV diastolic gradient.
Слайд 2611/12/02
Lubna Piracha, D.O.
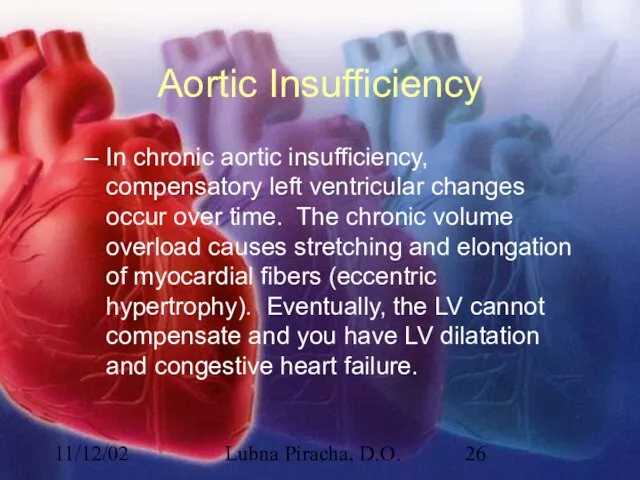
Aortic Insufficiency
In chronic aortic insufficiency, compensatory left ventricular changes occur
over time. The chronic volume overload causes stretching and elongation of myocardial fibers (eccentric hypertrophy). Eventually, the LV cannot compensate and you have LV dilatation and congestive heart failure.
Слайд 2711/12/02
Lubna Piracha, D.O.
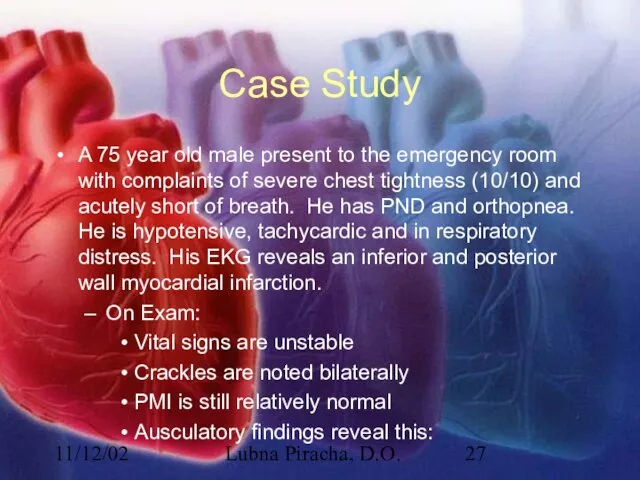
Case Study
A 75 year old male present to the emergency
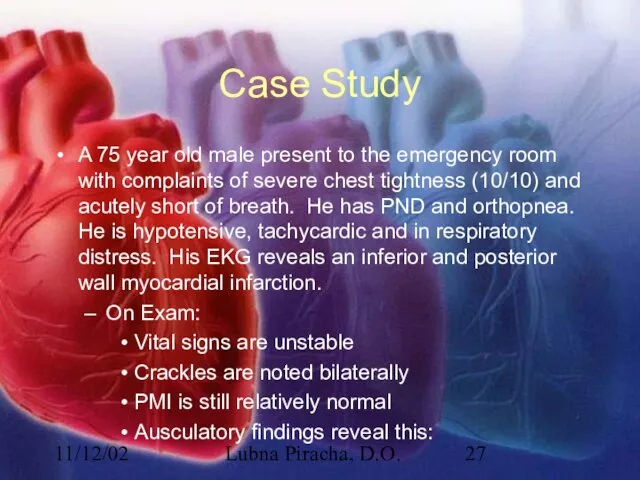
room with complaints of severe chest tightness (10/10) and acutely short of breath. He has PND and orthopnea. He is hypotensive, tachycardic and in respiratory distress. His EKG reveals an inferior and posterior wall myocardial infarction.
On Exam:
Vital signs are unstable
Crackles are noted bilaterally
PMI is still relatively normal
Ausculatory findings reveal this:
Слайд 2811/12/02
Lubna Piracha, D.O.
Physical Exam Review
In acute MR, there is tachycardia, the murmur

maybe short and confined to early systole, because the LA pressures are elevated.
In chronic MR, the murmur is typically holosystolic starting after S1.
Слайд 2911/12/02
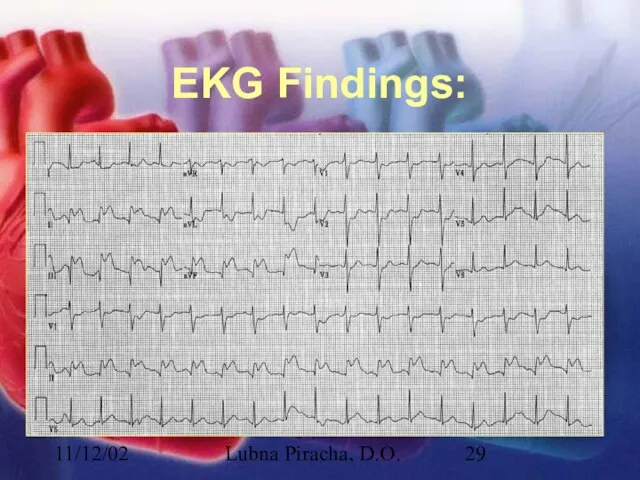
Lubna Piracha, D.O.
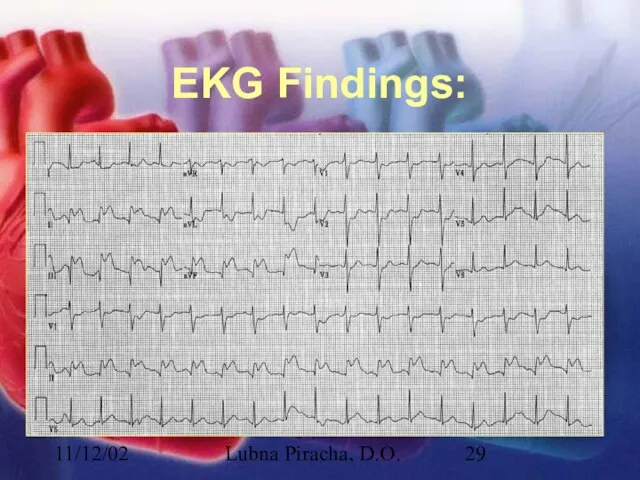
EKG Findings:
Слайд 3011/12/02
Lubna Piracha, D.O.
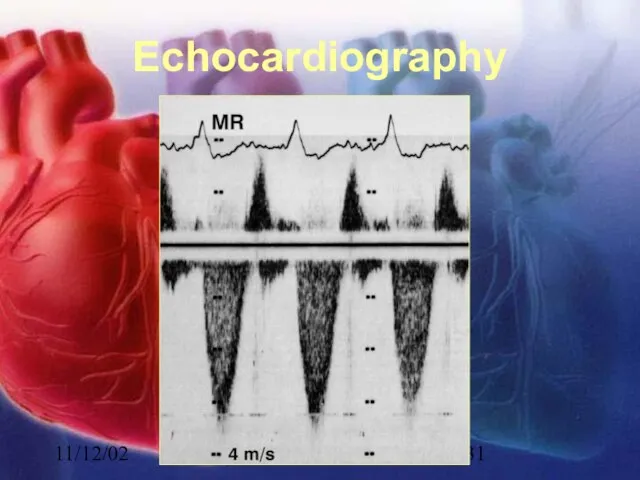
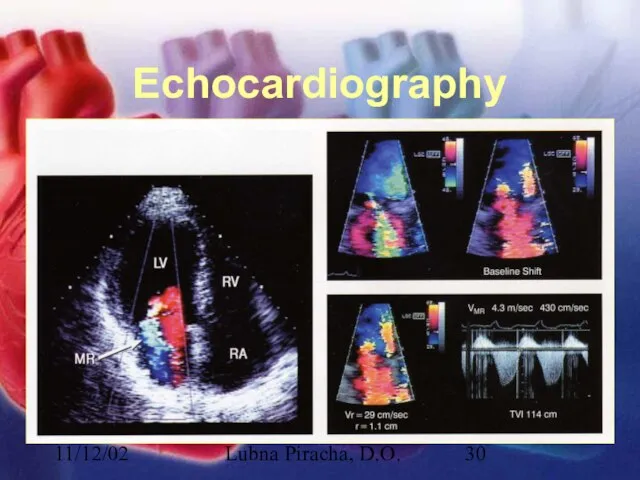
Echocardiography
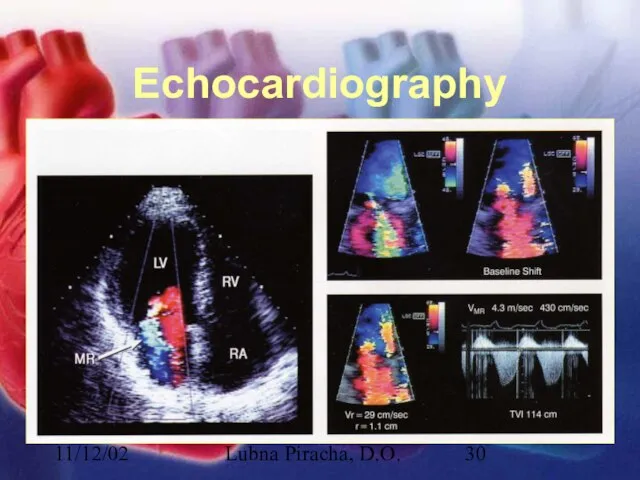
Слайд 3111/12/02
Lubna Piracha, D.O.
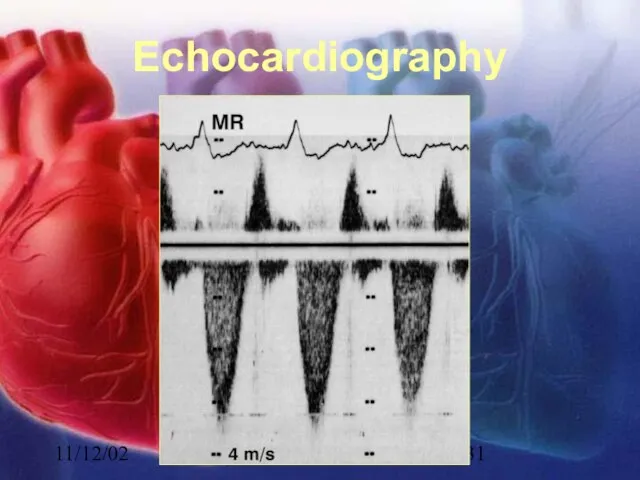
Echocardiography
Слайд 3211/12/02
Lubna Piracha, D.O.
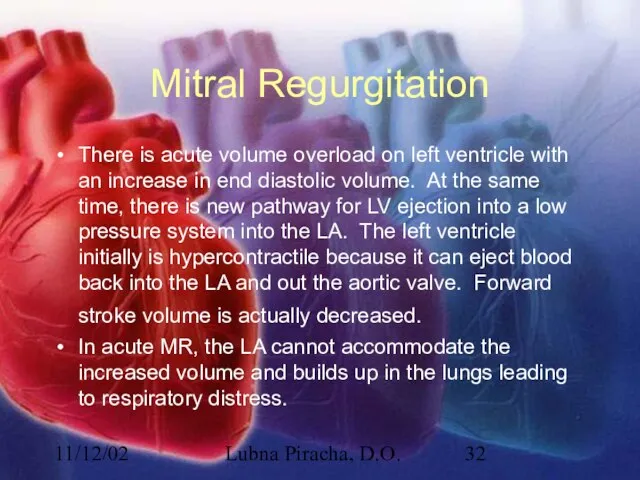
Mitral Regurgitation
There is acute volume overload on left ventricle with
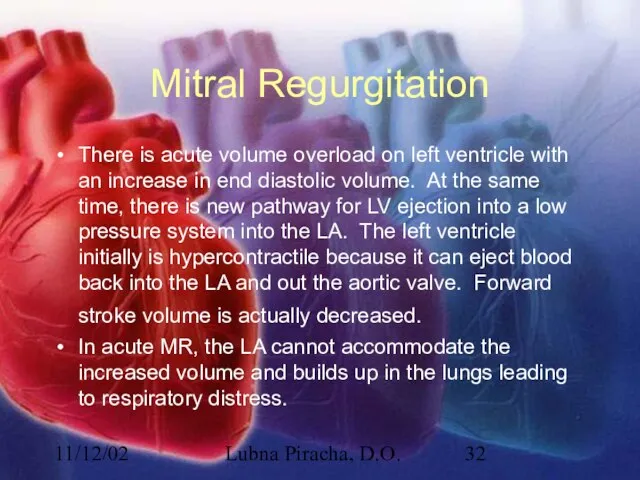
an increase in end diastolic volume. At the same time, there is new pathway for LV ejection into a low pressure system into the LA. The left ventricle initially is hypercontractile because it can eject blood back into the LA and out the aortic valve. Forward stroke volume is actually decreased.
In acute MR, the LA cannot accommodate the increased volume and builds up in the lungs leading to respiratory distress.
Слайд 3311/12/02
Lubna Piracha, D.O.
Mitral Regurgitation
In chronic MR, the LA will slowly dilate, the
LV will constantly be volume overloaded and eventually weaken. Both of these will eventually lead to congestive heart failure.
Слайд 3411/12/02
Lubna Piracha, D.O.
Case Study
A 22 year old male presents for a routine
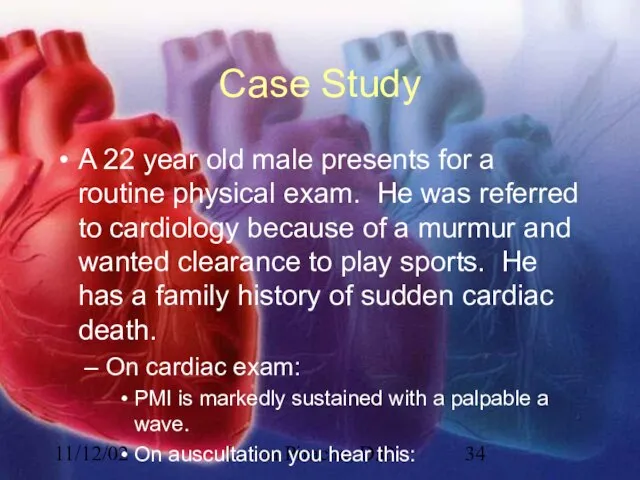
physical exam. He was referred to cardiology because of a murmur and wanted clearance to play sports. He has a family history of sudden cardiac death.
On cardiac exam:
PMI is markedly sustained with a palpable a wave.
On auscultation you hear this:
Слайд 3511/12/02
Lubna Piracha, D.O.
Physical Exam Review
A spike and dome arterial pulse
PMI will be
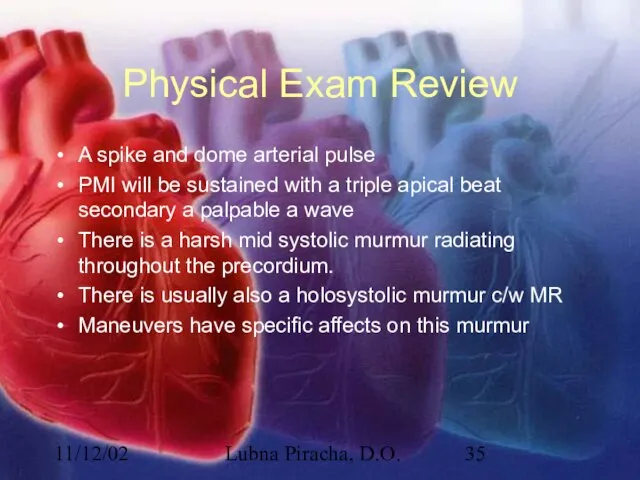
sustained with a triple apical beat secondary a palpable a wave
There is a harsh mid systolic murmur radiating throughout the precordium.
There is usually also a holosystolic murmur c/w MR
Maneuvers have specific affects on this murmur
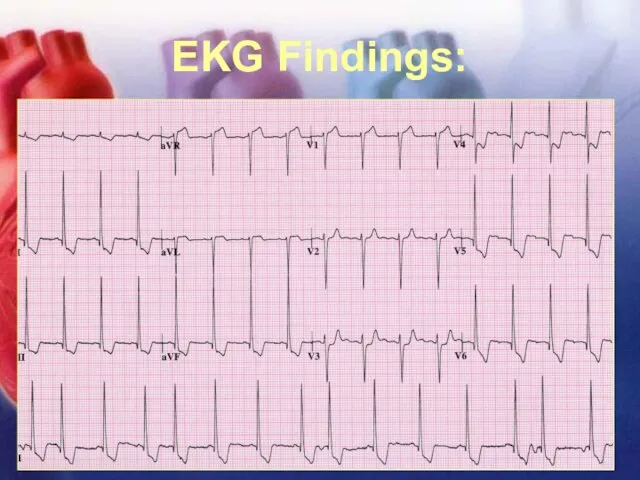
Слайд 3611/12/02
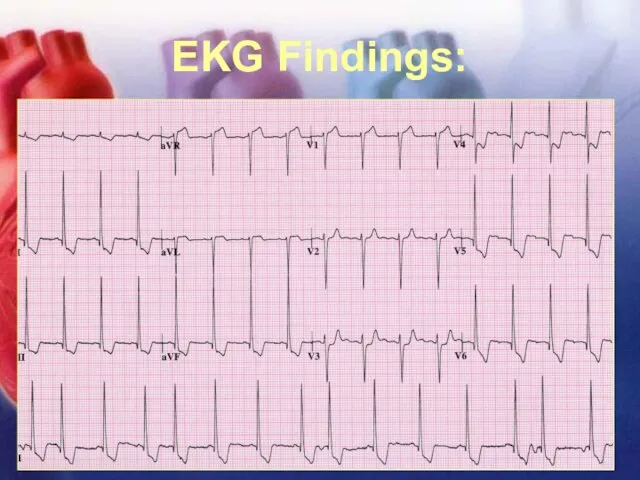
Lubna Piracha, D.O.
EKG Findings:
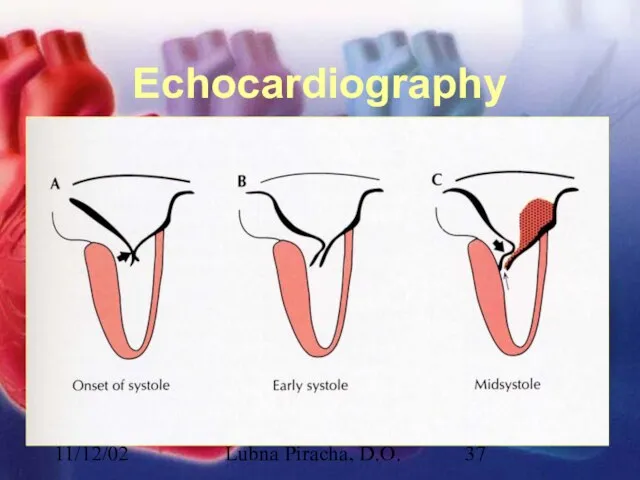
Слайд 3711/12/02
Lubna Piracha, D.O.
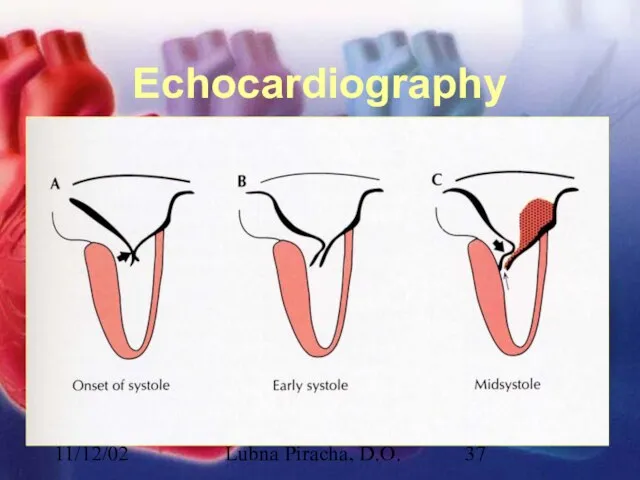
Echocardiography
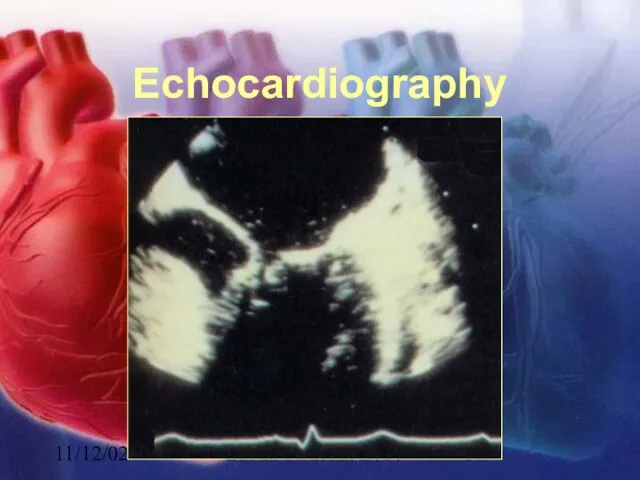
Слайд 3811/12/02
Lubna Piracha, D.O.
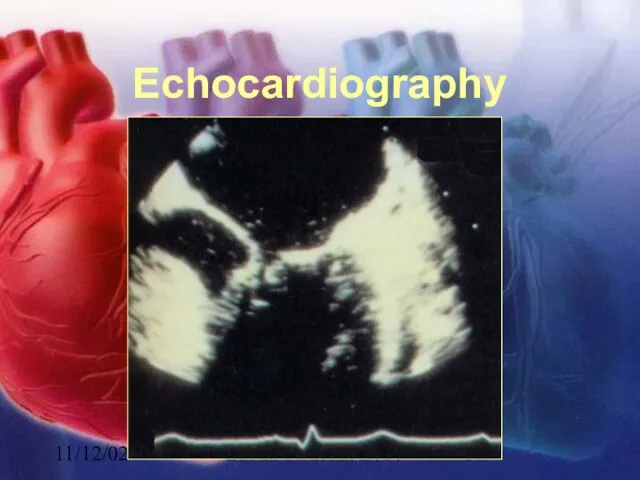
Echocardiography
Слайд 3911/12/02
Lubna Piracha, D.O.
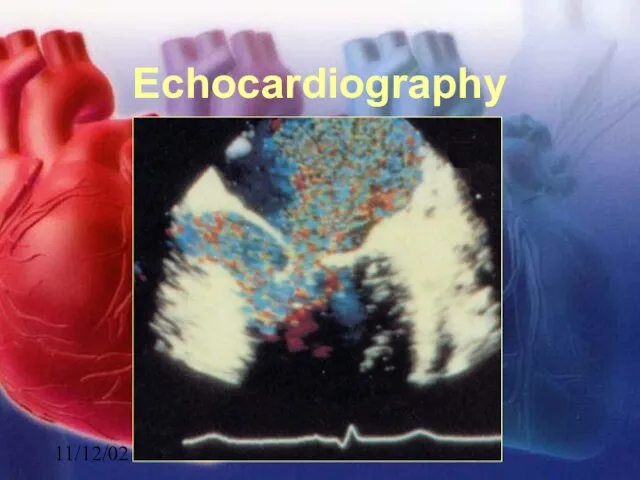
Echocardiography
Слайд 4011/12/02
Lubna Piracha, D.O.
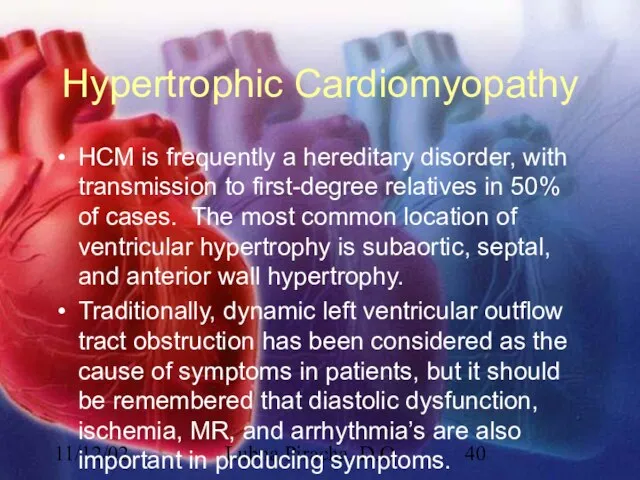
Hypertrophic Cardiomyopathy
HCM is frequently a hereditary disorder, with transmission to
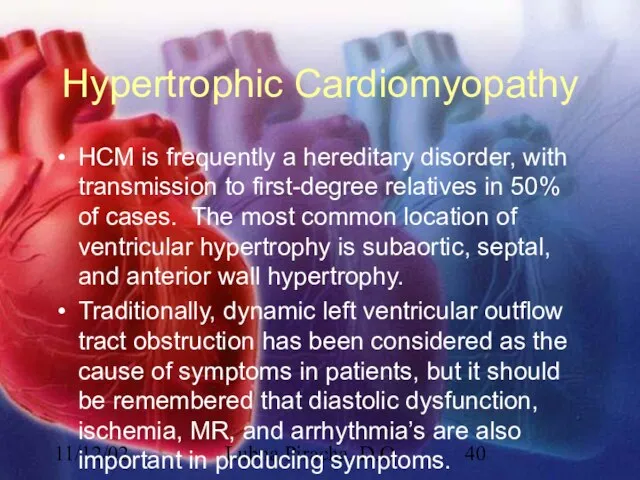
first-degree relatives in 50% of cases. The most common location of ventricular hypertrophy is subaortic, septal, and anterior wall hypertrophy.
Traditionally, dynamic left ventricular outflow tract obstruction has been considered as the cause of symptoms in patients, but it should be remembered that diastolic dysfunction, ischemia, MR, and arrhythmia’s are also important in producing symptoms.

 Вводный инструктаж по технике безопасности на уроках физической культуры
Вводный инструктаж по технике безопасности на уроках физической культуры ВПР по математике 5 класс
ВПР по математике 5 класс Философия мечты
Философия мечты Неформальные движения молодёжи
Неформальные движения молодёжи Чувство прекрасного
Чувство прекрасного Концептуальные основы корпоративной социальной ответственности
Концептуальные основы корпоративной социальной ответственности  Потолочная система охлаждения панельного типа Uponor Comfort
Потолочная система охлаждения панельного типа Uponor Comfort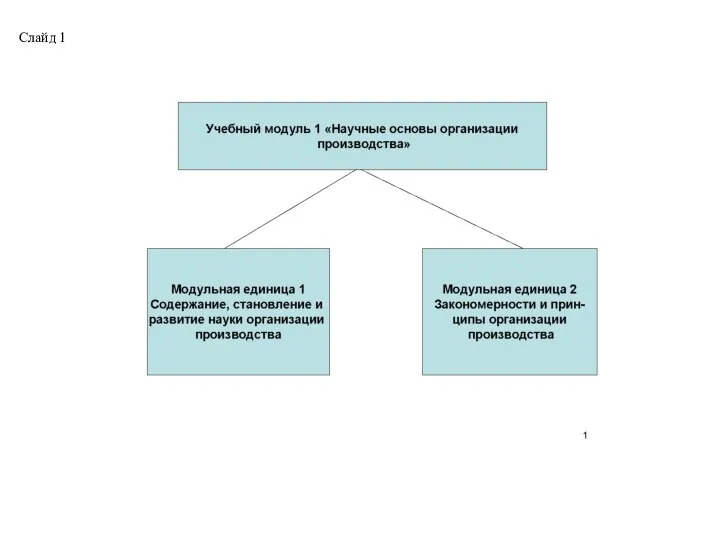 Тема 1.1.Организация производства как система научных знаний
Тема 1.1.Организация производства как система научных знаний Кафтан Урок №4
Кафтан Урок №4 Көксерек в театре
Көксерек в театре Моря Атлантического океана
Моря Атлантического океана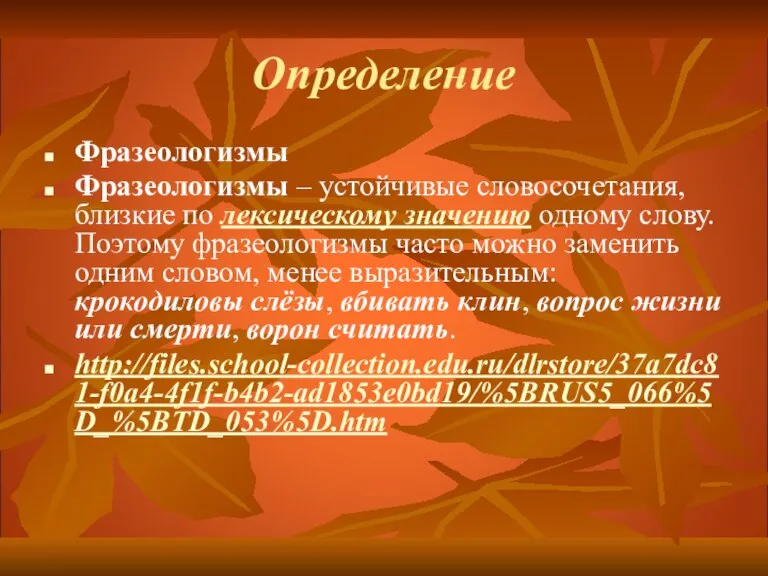 Сходство и различие фразеологизмов и пословиц
Сходство и различие фразеологизмов и пословиц Кинесика как составной элемент невербальной коммуникации
Кинесика как составной элемент невербальной коммуникации Правовое регулирование оборота земель сельскохозяйственного назначения
Правовое регулирование оборота земель сельскохозяйственного назначения Гражданственность
Гражданственность Естественный ядерный реактор Окло
Естественный ядерный реактор Окло Презентация на тему Реки России
Презентация на тему Реки России План местности. Условные знаки
План местности. Условные знаки 10 години в 10 минути Христина Машкова “Четиринадесети рекламен форум”
10 години в 10 минути Христина Машкова “Четиринадесети рекламен форум” Моё блюдо: Яичница с овощами
Моё блюдо: Яичница с овощами Энде Михаэль Андреас Гельмут 1929-1995
Энде Михаэль Андреас Гельмут 1929-1995 Изменение состояния региональной гемодинамики у больных с ОАСНК с различной тяжестью ишемии нижних конечностей при лечении мето
Изменение состояния региональной гемодинамики у больных с ОАСНК с различной тяжестью ишемии нижних конечностей при лечении мето Русская кухня
Русская кухня Решение задач
Решение задач Исследование статической устойчивости асинхронной нагрузки при питании их от шин бесконечной мощности
Исследование статической устойчивости асинхронной нагрузки при питании их от шин бесконечной мощности Презентация на тему Инфаркт миокарда
Презентация на тему Инфаркт миокарда  Lecture 1
Lecture 1 Правда или ложь
Правда или ложь