Содержание
- 2. Learning objectives 1. Understand why good diabetic control reduces the incidence of long-term complications. 2. Differentiate
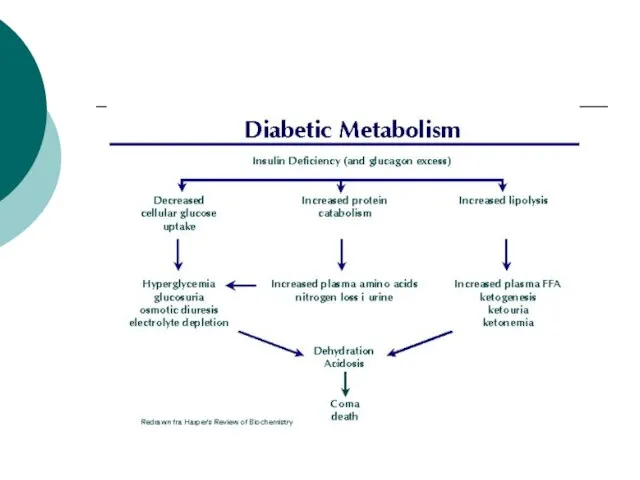
- 3. Diabetes Mellitus Metabolic disease affecting CHO, protein and fat metabolism due to insulin deficiency or inefficiency.
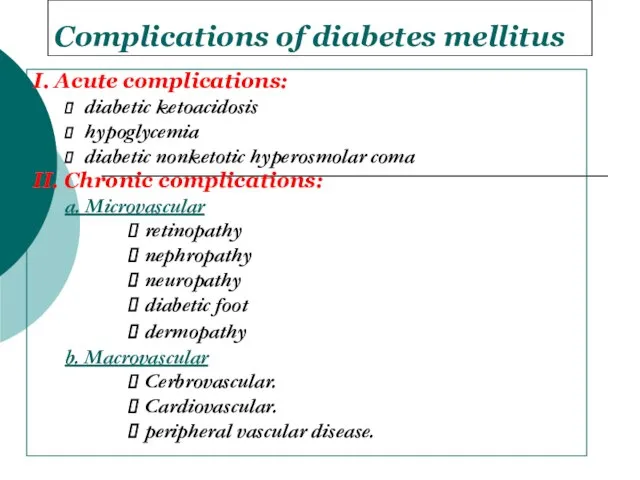
- 5. Complications of diabetes mellitus I. Acute complications: diabetic ketoacidosis hypoglycemia diabetic nonketotic hyperosmolar coma II. Chronic
- 6. Diabetic ketoacidosis (DKA) May be the 1st presentation of type 1 DM. Result from absolute insulin
- 7. Pathophysiology of DKA Ketosis Dehydration Electrolyte imbalance
- 8. Diagnosis of DKA Hyperglycemia Ketonuria and ketonemia Acidosis (PH
- 9. Predisposing factors for DKA Infection Trauma Myocardial Infarction Stroke Surgery Emotional stress
- 10. Clinical presentation of DKA Polyurea and polydepsia. Nausea and vomiting. Anorexia and abdominal pain. Tachycardia. Fruity
- 11. Treatment of DKA Fluid replacement. Insulin therapy for hyperglycemia. Electrolyte correction. Acidosis correction. Treatment of precipitating
- 12. Complication of DKA Cerebral edema Vascular thrombosis Infection M I Acute gastric dilatation Respiratory distress syndrome
- 13. Hypoglycemic coma Hypoglycemia is the most frequent acute complication in type 1 diabetes. Hypoglycemia is the
- 14. Clinical manifestations of hypoglycemia: Autonomic dysfunctions: 1. Hunger 2. Tremor 3. Palpitation 4. Anxiety 5. Pallor
- 15. Neurologic dysfunctions: 1. Impaired thinking 2. Change of mood 3. Irritability 4. Headache 5. Convulsion 6.
- 16. Predisposing factors Missed meal Change in physical activity Alterations or errors in insulin dosage Alcohol ingestion
- 17. Treatment of hypoglycemia In mild cases oral rapidly absorbed carbohydrate In sever cases (comatose patient) iv
- 18. Chronic Complications of DM A. Macrovascular Complications: B. Microvascular Complications:
- 19. Macro-vascular Complications: Ischemic heart diseases. Cerebrovascular diseases. Peripheral vascular diseases. Diabetic patients have a 2 to
- 20. Macro-vascular Complications: Accelerated atherosclerosis involving the aorta and large- and medium-sized arteries. Myocardial infarction, caused by
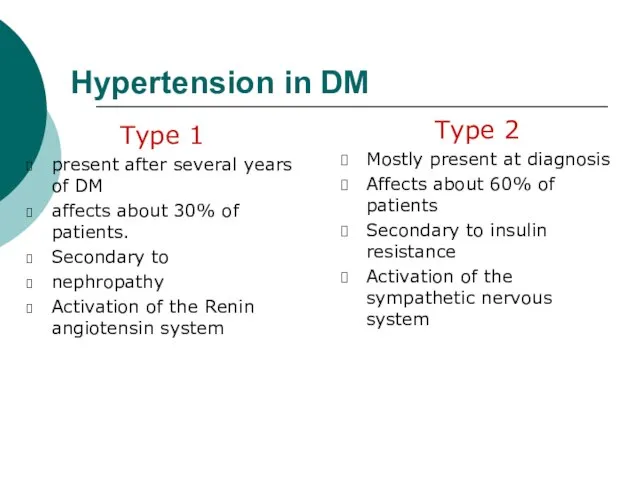
- 21. Hypertension in DM Type 1 present after several years of DM affects about 30% of patients.
- 22. Dyslipidaemia in DM Most common abnormality is ↓ HDL and ↑ Triglycerides A low HDL is
- 23. Screening for Macrovascular Complications 1. Examine pulses for cardiovascular diseases. 2. Lipogram (lipid profile). 3. ECG.
- 24. Microvascular complications are specific to diabetes and related to longstanding hyperglycaemia. Both Type1 DM and Type2
- 25. Pathophysiology of microvascular disease In diabetes, the microvasculature shows both functional and structural abnormalities. The structural
- 26. The main functional abnormalities include increased capillary permeability, viscosity, and disturbed platelet function. These changes occur
- 27. Platelets from diabetic patients show an exaggerated tendency to aggregate, perhaps mediated by altered prostaglandin metabolism.
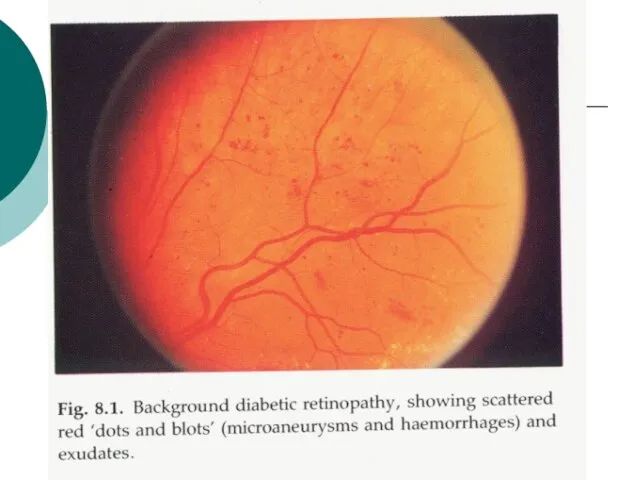
- 28. 1- Diabetic retinopathy * Pathogenesis: Histologically the earliest lesion is thickening of the capillary basement membrane.
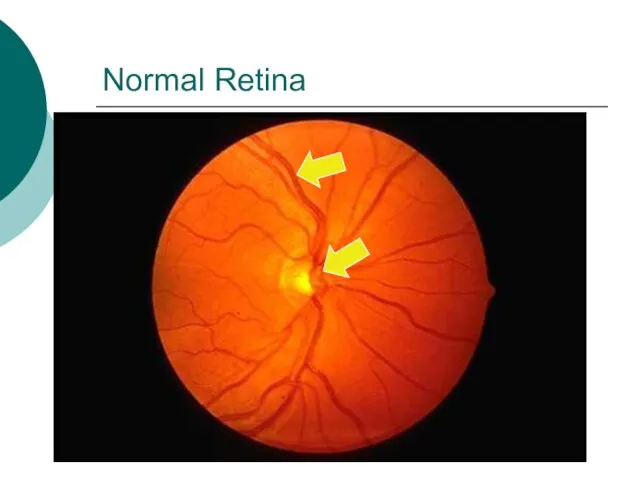
- 29. Normal Retina
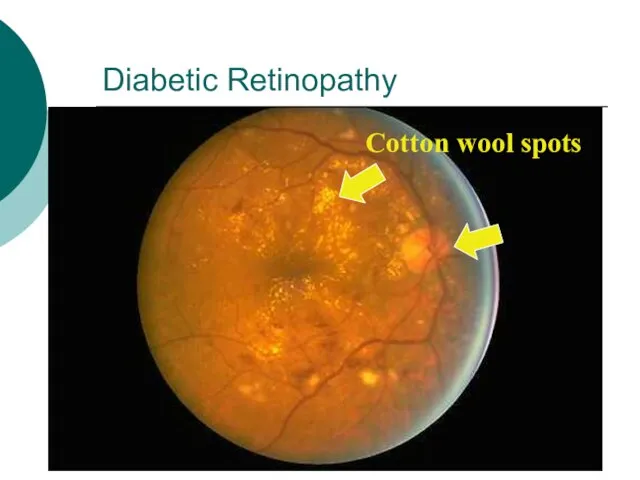
- 31. Diabetic Retinopathy Cotton wool spots
- 32. Other Eye Complications - Cataracts. - Glaucoma - Macular edema. Ischaemic maculopathy. Proliferative retinopathy. Vitreous Bleeding.
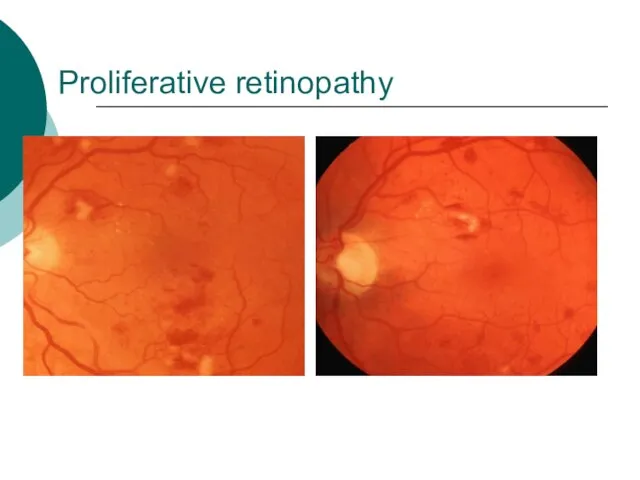
- 33. Proliferative retinopathy
- 34. Vitreous Bleeding
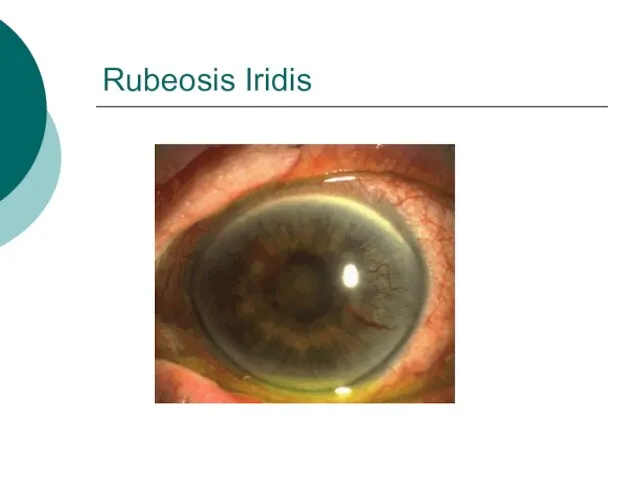
- 35. Rubeosis Iridis
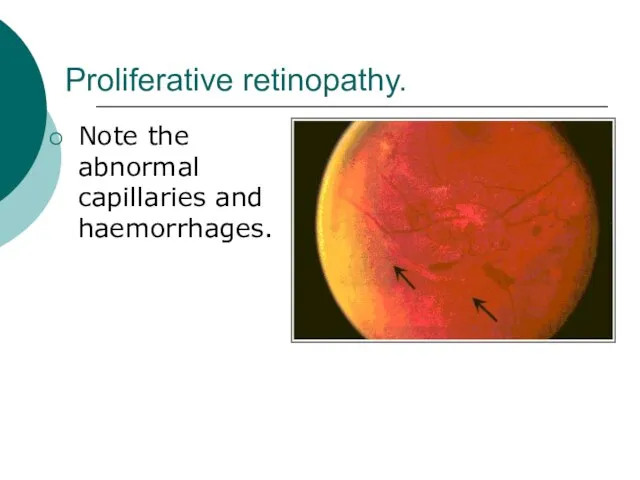
- 36. Proliferative retinopathy. Note the abnormal capillaries and haemorrhages.
- 37. 2- Diabetic Nephropathy (DN) - Diabetic nephropathy is defined by persistent albuminuria (>300 mg/day), decrease glomerular
- 38. Risk factors of DN Duration of DM. Family History of hypertension. Cardiovascular disease, nephropathy. Hyperglycemia. Hypertension.
- 39. Pathogenesis: The glomerular and vascular lesions are linked to hyperglycemia. Nonenzymatic glycosylation to glomerular proteins results
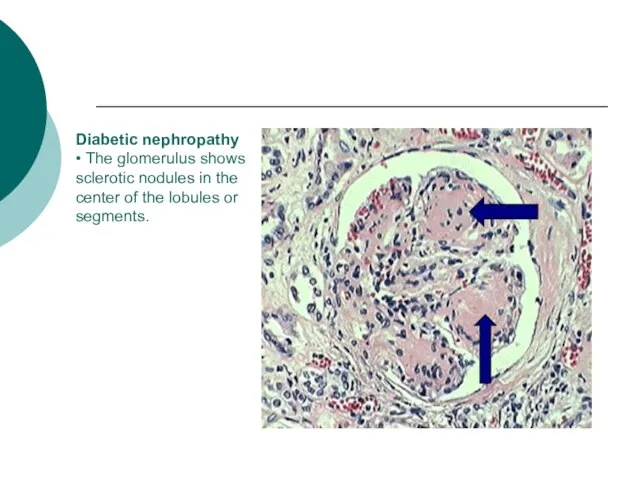
- 40. Pathological pattern of DN Diffuse form (more common): consist of thickining of glomerular basement membrane with
- 41. Diabetic nephropathy • The glomerulus shows sclerotic nodules in the center of the lobules or segments.
- 42. Treatment to prevent progression to DN Glycaemic control. ACE inhibitor . Blood pressure control. Smoking cessation.
- 43. 4. Diabetic Neuropathy 1. Sensorimotor neuropathy. 2. Autonomic neuropathy.
- 44. Sensorimotor Neuropathy Numbness, paresthesias. Feet are mostly affected, hands are seldom affected. Complicated by ulceration (painless),
- 45. Complications of Sensorimotor neuropathy
- 46. Autonomic Neuropathy Postural hypotension. Diabetic diarrhea. Neuropathic bladder. Erectile dysfunction.
- 47. 5. Infections Community acquired pneumonia Acute bacterial cystitis Acute pyelonephritis Pyelonephritis Perinephric abscess Fungal cystitis.
- 48. foot care Patient should check feet daily Wash feet daily Keep toe nails short Protect feet
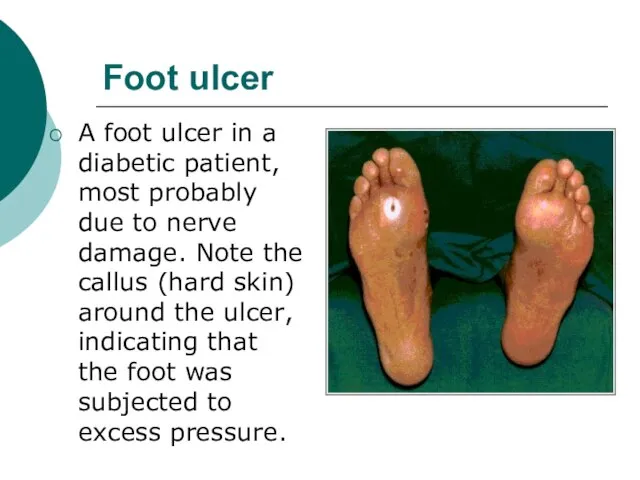
- 49. Foot ulcer A foot ulcer in a diabetic patient, most probably due to nerve damage. Note
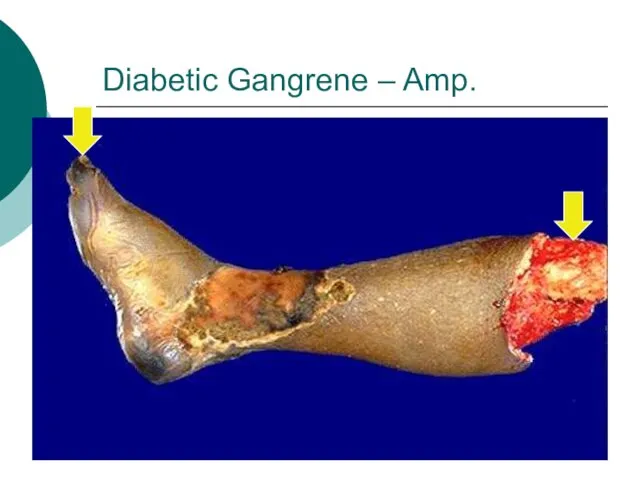
- 50. Diabetic Gangrene – Amp.
- 52. Скачать презентацию


 Тема: Роль права в жизни человека, общества, государства § 29
Тема: Роль права в жизни человека, общества, государства § 29 Краеведческий музеймуниципального бюджетного образовательного учреждения Запрудновской средней общеобразовательной школы
Краеведческий музеймуниципального бюджетного образовательного учреждения Запрудновской средней общеобразовательной школы Аксонометрические проекции плоскогранных предметов
Аксонометрические проекции плоскогранных предметов Готовые выкройки и чертежи одежды в журналах мод
Готовые выкройки и чертежи одежды в журналах мод Контроль на обогатительных фабриках
Контроль на обогатительных фабриках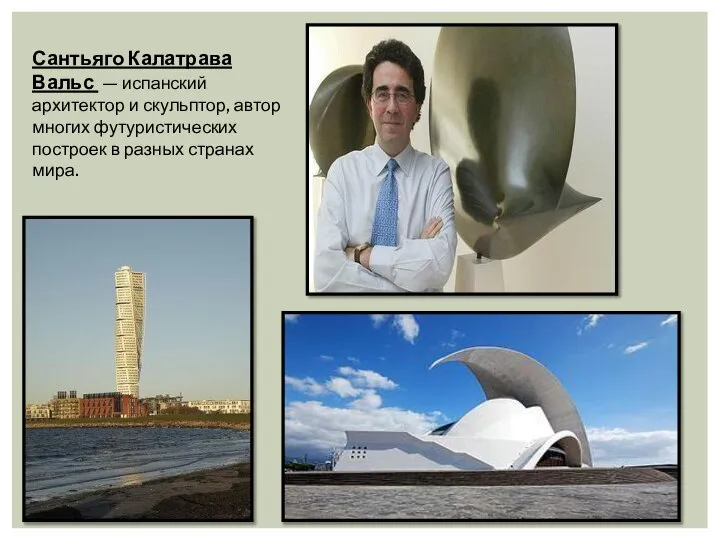 Сантьяго Калатрава Вальс
Сантьяго Калатрава Вальс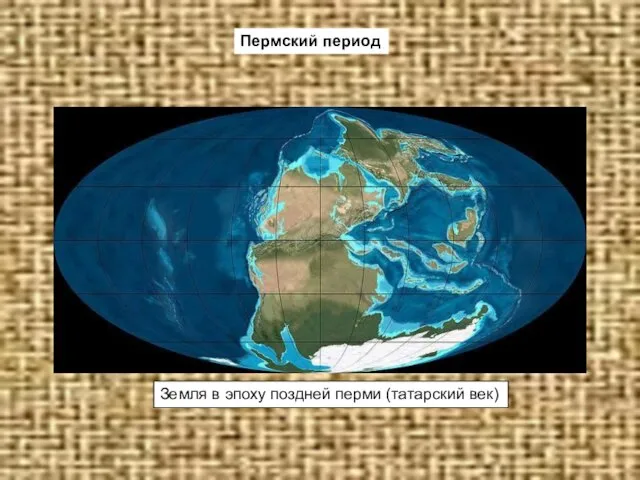 Презентация на тему Пермский период
Презентация на тему Пермский период Презентация по проектной деятельности 2 группа
Презентация по проектной деятельности 2 группа Школа стилиста Eleganzza
Школа стилиста Eleganzza Питание невидимок
Питание невидимок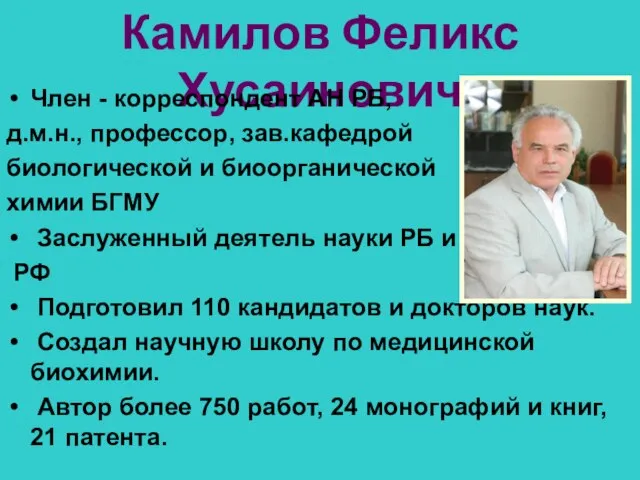 Камилов Феликс Хусаинович
Камилов Феликс Хусаинович Храмы – творение мастеров.
Храмы – творение мастеров. Экономика предприятия и предпринимательства
Экономика предприятия и предпринимательства Текущие тенденции в динамике валютного курса рубля, инфляции и процентных ставок
Текущие тенденции в динамике валютного курса рубля, инфляции и процентных ставок Тема 1. Функциональные возможности ГИСЗанятие № 3. Базы данных и системы управления ими в ГИС
Тема 1. Функциональные возможности ГИСЗанятие № 3. Базы данных и системы управления ими в ГИС ДИПЛОМНАЯ РАБОТА на тему: «Учёт и анализ оплаты труда и расчётов с рабочими и служащими (на материалах УП «Завод Радиан», г. Минск)»
ДИПЛОМНАЯ РАБОТА на тему: «Учёт и анализ оплаты труда и расчётов с рабочими и служащими (на материалах УП «Завод Радиан», г. Минск)»  Некоторые аспекты деятельности Регионального управления №25 и ФГУЗ ЦГиЭ №25 ФМБА России, по формированию положительного имиджа о
Некоторые аспекты деятельности Регионального управления №25 и ФГУЗ ЦГиЭ №25 ФМБА России, по формированию положительного имиджа о Миф как форма мировоззрения
Миф как форма мировоззрения Виды интертекстуальных связей
Виды интертекстуальных связей Классификатор характера сделки Подготовила: Клеутина С.А., ДС_01
Классификатор характера сделки Подготовила: Клеутина С.А., ДС_01 Психолого-педагогическое сопровождение профессионального самоопределения старшеклассников в рамках сетевого взаимодействия о
Психолого-педагогическое сопровождение профессионального самоопределения старшеклассников в рамках сетевого взаимодействия о Жизненные формы растений. Растительные ткани
Жизненные формы растений. Растительные ткани Политико-территориальное устройство США
Политико-территориальное устройство США Психопатологическая семиотика
Психопатологическая семиотика УСЛОВНЫЙ ОПЕРАТОР
УСЛОВНЫЙ ОПЕРАТОР Защищённый грунт. Урок сельскохозяйственного труда
Защищённый грунт. Урок сельскохозяйственного труда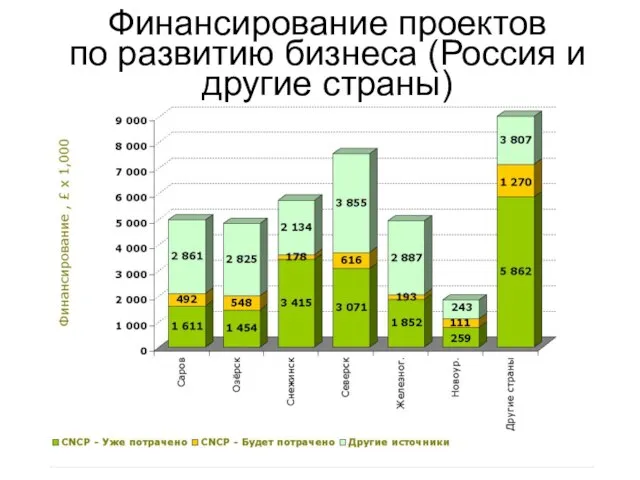 Финансирование проектов по развитию бизнеса (Россия и другие страны)
Финансирование проектов по развитию бизнеса (Россия и другие страны) Пожары на объектах добычи и хранения жидкого и газообразного топлива
Пожары на объектах добычи и хранения жидкого и газообразного топлива