Содержание
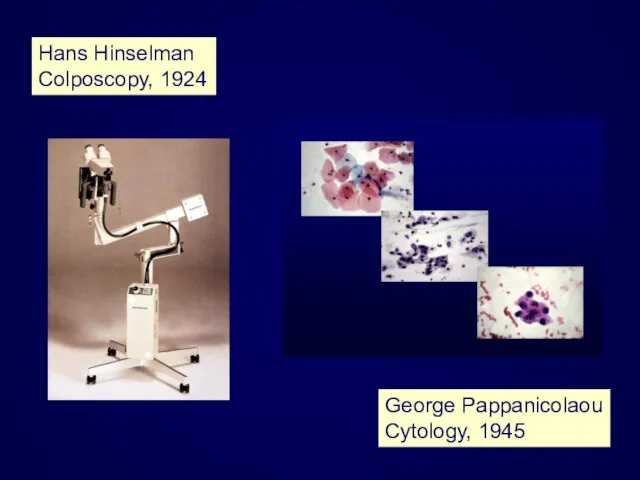
- 2. Hans Hinselman Colposcopy, 1924 George Pappanicolaou Cytology, 1945
- 3. Cervical cancer has become detectable and curable disease.
- 4. Recently, however, significant controversy has arisen over several aspects of the diagnosis and management of cervical
- 5. There is no dispute about the need to treat CIN 3 and few would argue that
- 6. These two grades of CIN (CIN 2 and CIN 3) are referred to as high-grade lesions
- 7. In the spectrum of cervical pathology the line between premalignant and benign lesions may be drawn
- 8. L-SIL High proportion of women affected Low risk of progression Significant regression may occur
- 9. Management of CIN 1 (L-SIL) Conservative Active
- 10. Management of L-SIL Close observation with cytologic and possibly colposcopic follow-up, without active treatment is the
- 14. Expectant management of CIN 1 is not totally without some risk...
- 15. ……. because of the: potential for a high-grade lesion to develop during follow-up already existing high-grade
- 18. If large lesions or persistent lesions are present or if the patient is at risk for
- 20. Active management of women with CIN 1 is recommended in the following cases: Unsatisfactory colposcopy Large,
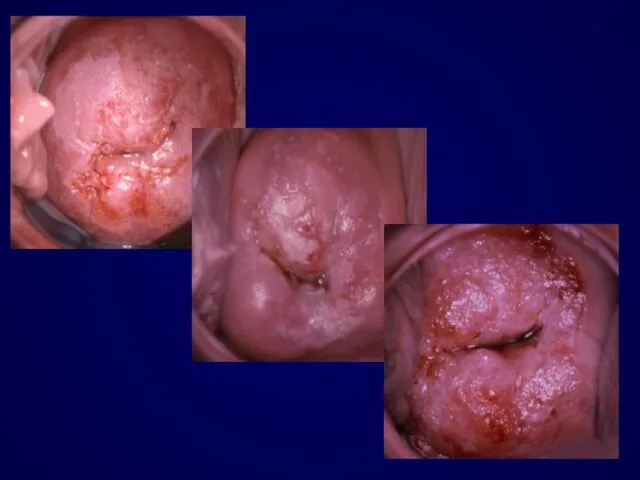
- 21. Women with biopsy confirmed H-SIL (CIN 2 and 3) have significant risk of disease progression to
- 24. The expectant management of CIN 2 and 3 with repeat cytology and colposcopy is not acceptable
- 27. Destruction or Excision ?
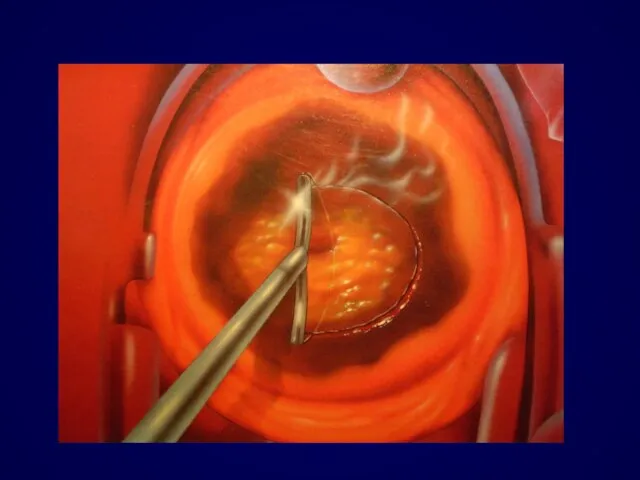
- 28. Management of HSIL excision recommended cold-knife laser conization LLETZ
- 29. Excision is necessary in: Unsatisfactory examination Large lesions Recurrent disease
- 33. Unless there are other compelling reasons for performing a hysterectomy, this procedure is considered unacceptable as
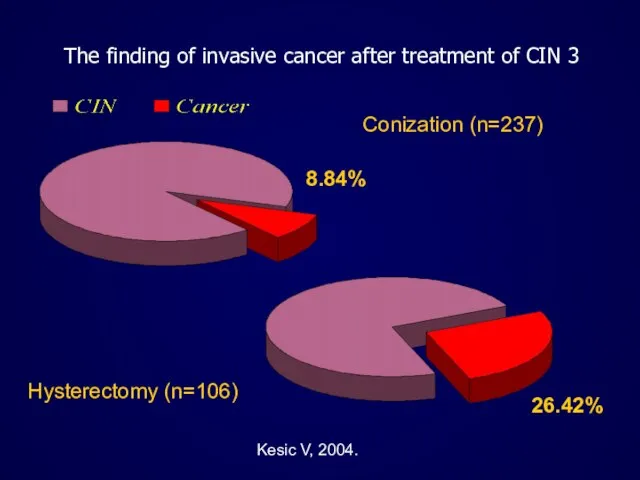
- 34. The finding of invasive cancer after treatment of CIN 3 Conization (n=237) 8.84% Hysterectomy (n=106) 26.42%
- 39. Vesna Kesic Institute of Obstetrics and Gynecology Clinical Center of Serbia International Scientific Conference Prevention of
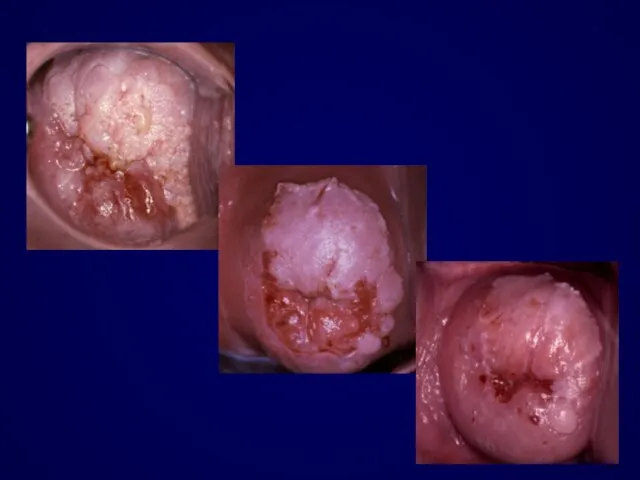
- 40. Treatment of cervical cancer is affected by the stage of the disease.
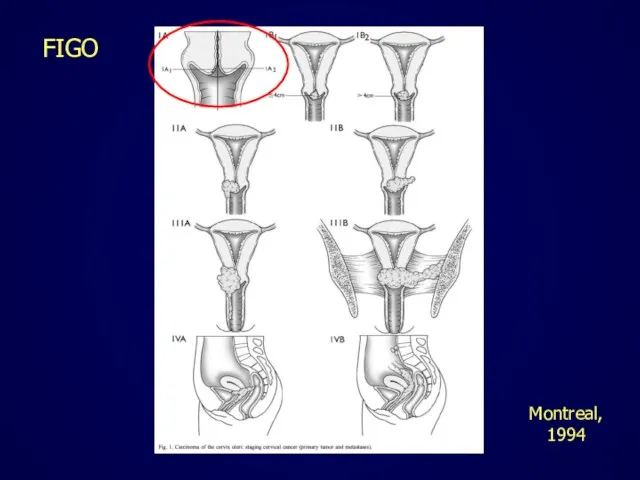
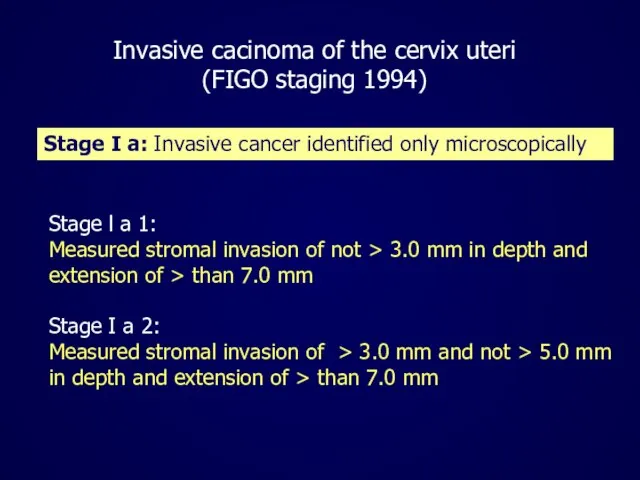
- 41. FIGO Montreal, 1994
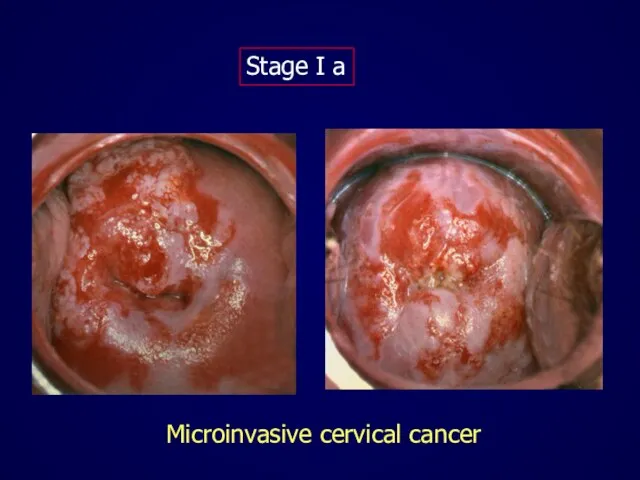
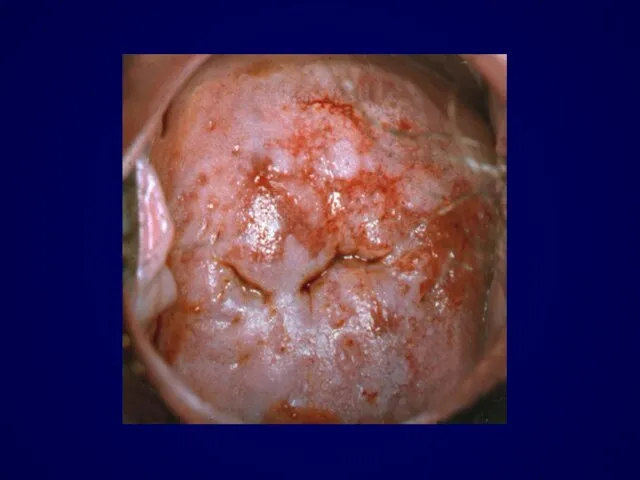
- 42. Microinvasive cervical cancer Stage I a
- 44. MESTWERDT reported 1947 about 30 small invasive carcinomas. No evidence for metastases! In 1953 he called
- 45. Stage l a 1: Measured stromal invasion of not > 3.0 mm in depth and extension
- 46. Were the microinvasive lesion and its preinvasive components removed in their entirety? What are the dimensions
- 47. The excision margins should be free of CIN and invasive disease !
- 48. If the invasive lesion is excised but CIN extends to the excision margin then a repeat
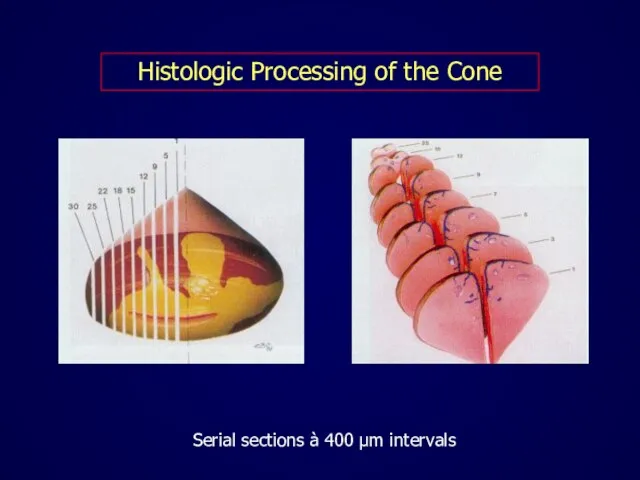
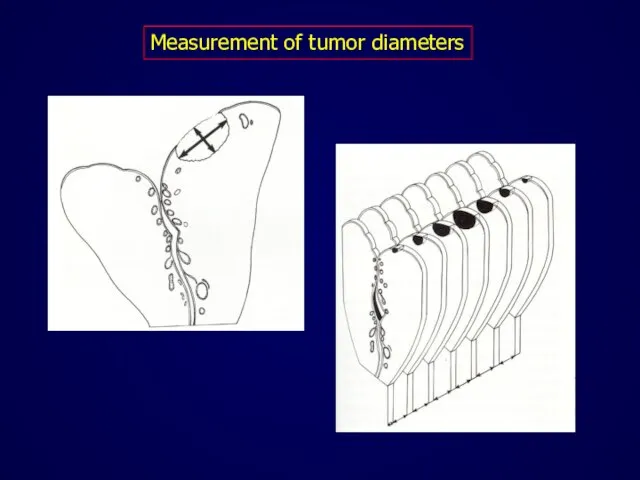
- 49. Histologic Processing of the Cone Serial sections à 400 μm intervals
- 50. Measurement of tumor diameters
- 51. Ideally, the management of microinvasive cancer Stage Ia should be planned in cooperation with an experienced
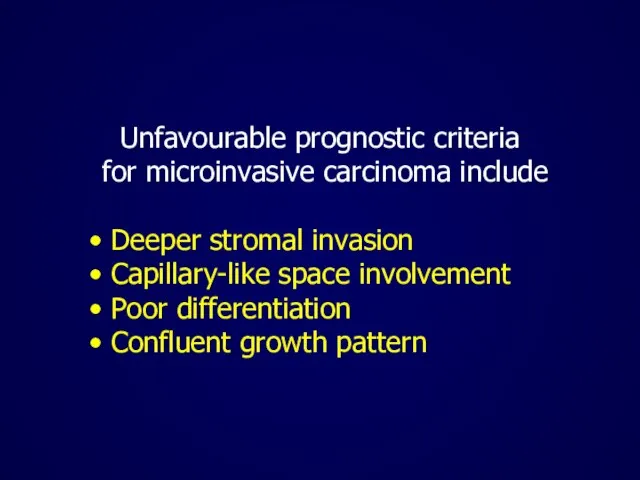
- 52. Unfavourable prognostic criteria for microinvasive carcinoma include Deeper stromal invasion Capillary-like space involvement Poor differentiation Confluent
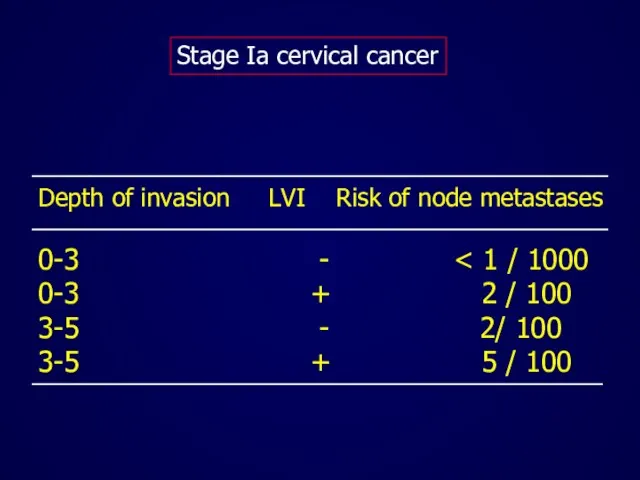
- 53. Depth of invasion LVI Risk of node metastases 0-3 - 0-3 + 2 / 100 3-5
- 54. Each patient with microinvasive cancer should be evaluated individually !
- 55. If distant spread is very unlikely, simple but complete excision of the lesion suffices. If it
- 56. The reasons of conservative surgery in microinvasive cervical cancer To preserve fertility To prevent the potential
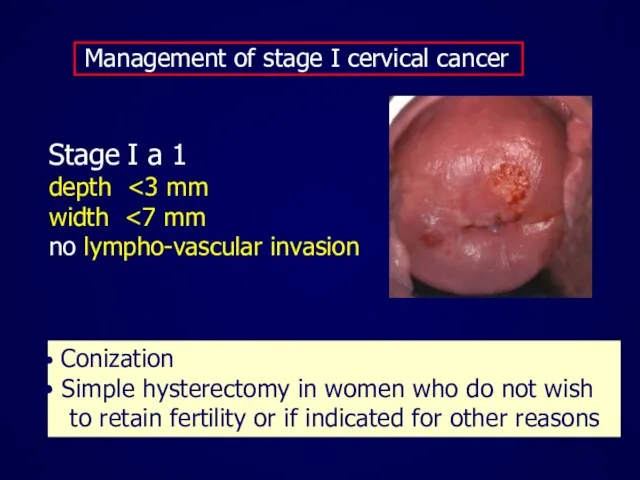
- 57. Management of stage I cervical cancer Stage I a 1 depth width no lympho-vascular invasion Conization
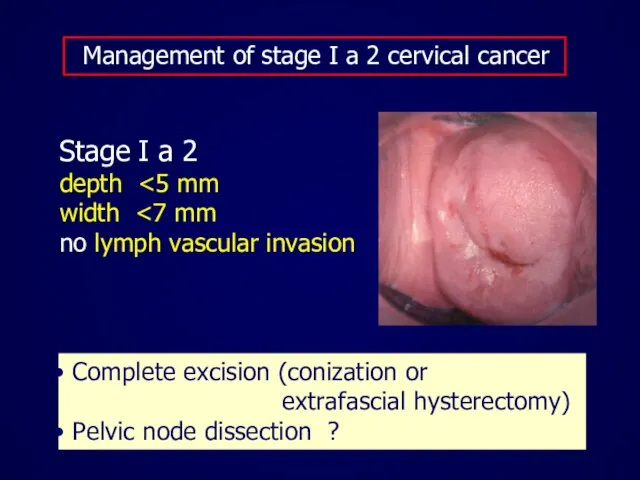
- 58. Management of stage I a 2 cervical cancer Stage I a 2 depth width no lymph
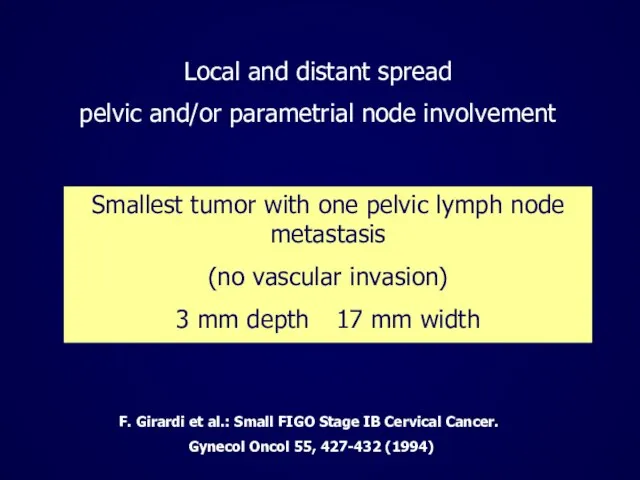
- 59. Smallest tumor with one pelvic lymph node metastasis (no vascular invasion) 3 mm depth 17 mm
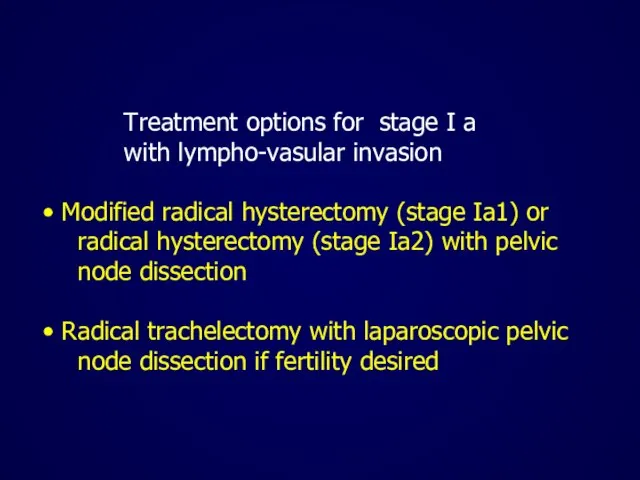
- 61. Treatment options for stage I a with lympho-vasular invasion Modified radical hysterectomy (stage Ia1) or radical
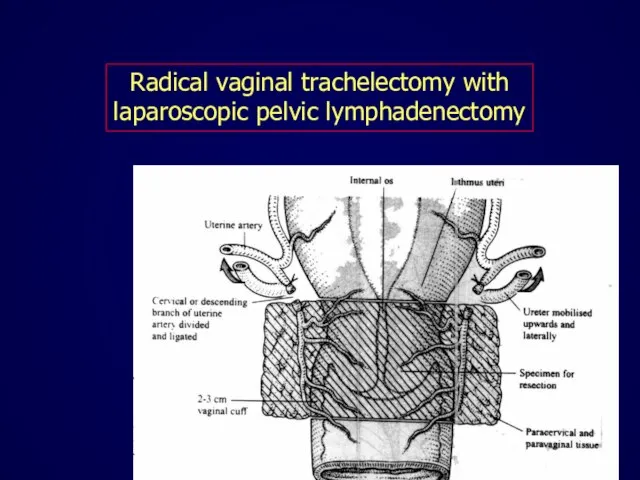
- 62. Radical vaginal trachelectomy with laparoscopic pelvic lymphadenectomy
- 63. Recurrence rates after trachelectomy are comparable to radical hysterectomy (aproximately 4%) Plante et al. Gynecol Oncol.
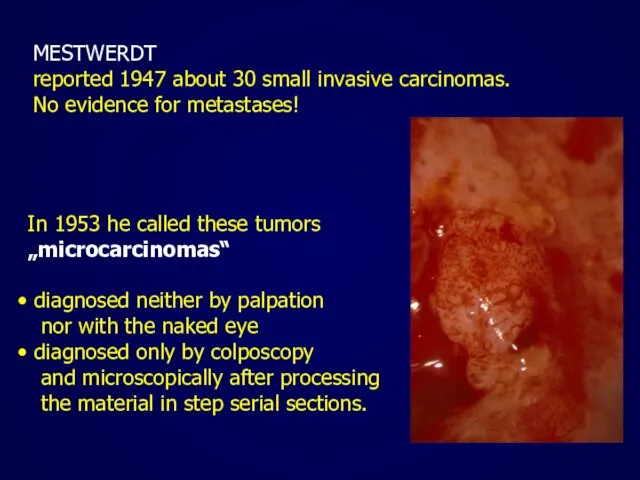
- 64. Radical trachelectomy Successful pregnancy in 26.5% cases Plante et al. Gynecol Oncol. 2004 ;94:614-23
- 65. Prerequisites for trachelectomy Strong fertility desire Patient Tumor No lymphovascular invasion Negative lymphnodes Favorable histology Length
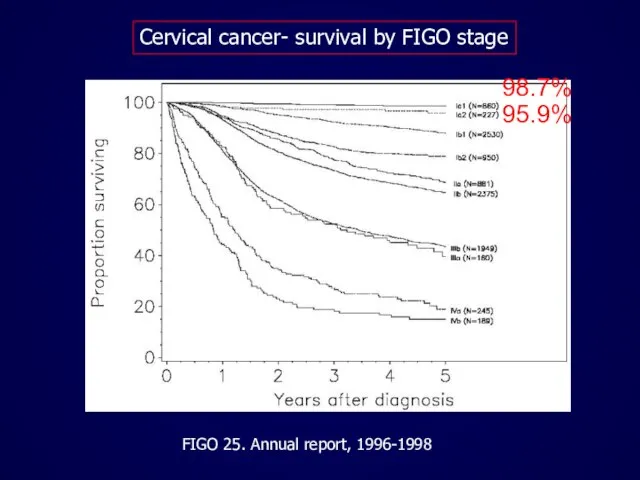
- 66. Cervical cancer- survival by FIGO stage FIGO 25. Annual report, 1996-1998 98.7% 95.9%
- 68. Скачать презентацию

















 Академический университет им. Ж.И. Алферова
Академический университет им. Ж.И. Алферова Колонны, балки, раскосы в строительстве
Колонны, балки, раскосы в строительстве Влияние на организм химически опасных веществ.
Влияние на организм химически опасных веществ. Презентация на тему Диковинные деревья
Презентация на тему Диковинные деревья  Предприниматели Бердниковы – основатели лесопромышленной отрасли в Ветлужском уезде
Предприниматели Бердниковы – основатели лесопромышленной отрасли в Ветлужском уезде Природные сообщества: луг, озеро, поле
Природные сообщества: луг, озеро, поле Пироги
Пироги Корней Иванович Чуковский
Корней Иванович Чуковский Отпуск
Отпуск Олимпиада в Сочи
Олимпиада в Сочи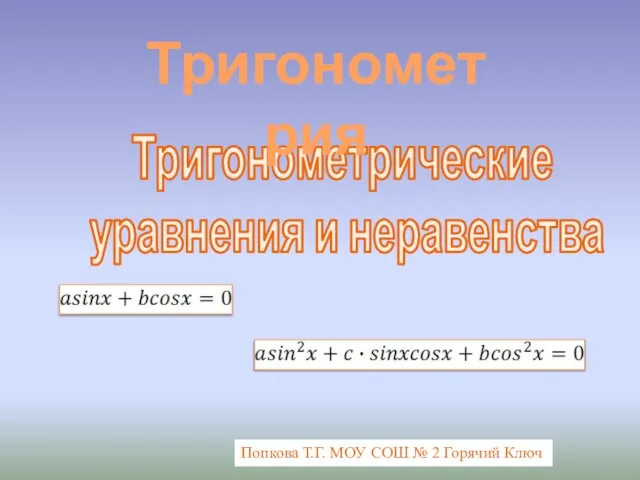 Тригонометрические уравнения и неравенства
Тригонометрические уравнения и неравенства Deutschland. Ein Wintermarchen. Германия. Зимняя сказка.
Deutschland. Ein Wintermarchen. Германия. Зимняя сказка. ООО Кинда
ООО Кинда Презентация на тему Семья и семейные ценности
Презентация на тему Семья и семейные ценности  Методическое объединение математики и информатики
Методическое объединение математики и информатики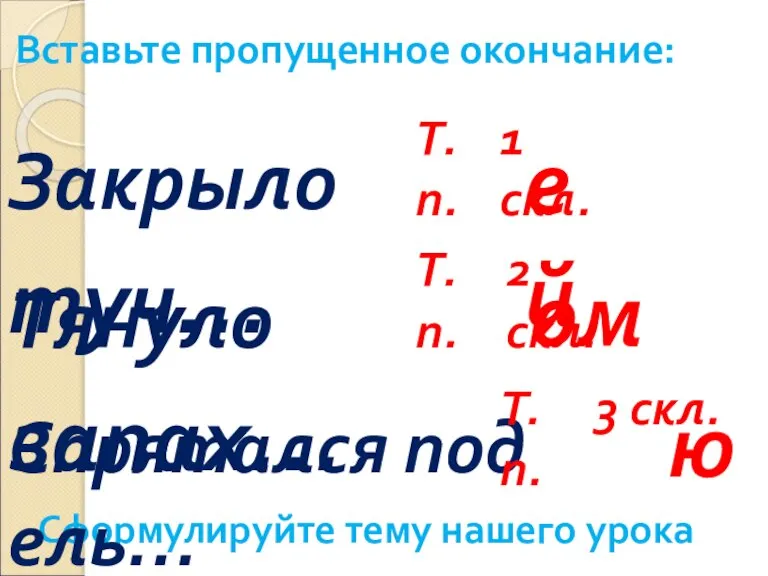 Правописание безударных окончаний существительных в творительном падеже
Правописание безударных окончаний существительных в творительном падеже Система нормативно-технических документов, устанавливающих требвоания к техническому
Система нормативно-технических документов, устанавливающих требвоания к техническому Интеллектуальная игра Новогодние традиции
Интеллектуальная игра Новогодние традиции Озоновая камера
Озоновая камера W.Shakespear’s heroines. Героини Вильяма Шекспира
W.Shakespear’s heroines. Героини Вильяма Шекспира Технология обработки материалов
Технология обработки материалов Современная медицинская кадровая система как основа формирования регионального и федерального регистра медицинских работников
Современная медицинская кадровая система как основа формирования регионального и федерального регистра медицинских работников 2 Парк ПС
2 Парк ПС Резина
Резина Ракообразные, их многообразие, общие черты и значение
Ракообразные, их многообразие, общие черты и значение Exbury Gardens
Exbury Gardens Гидроэлектростанции России
Гидроэлектростанции России Автоматы и пулеметы
Автоматы и пулеметы