Содержание
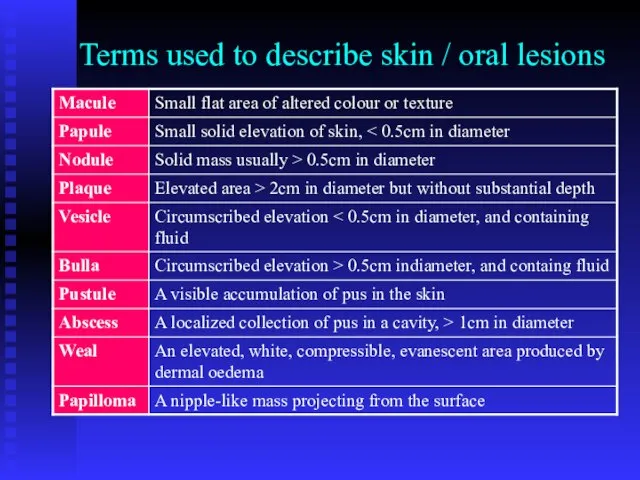
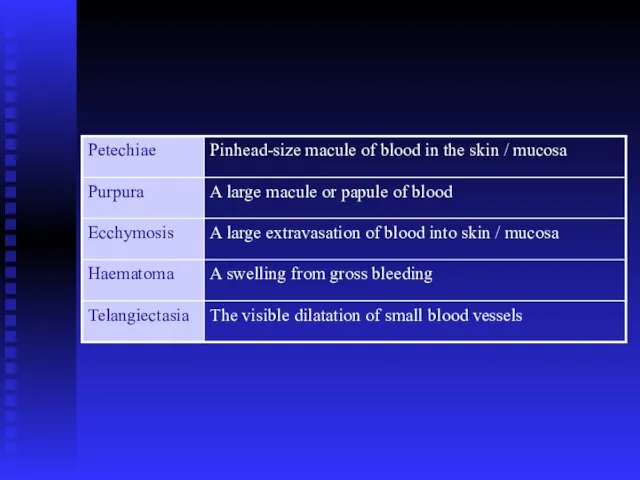
- 2. Terms used to describe skin / oral lesions
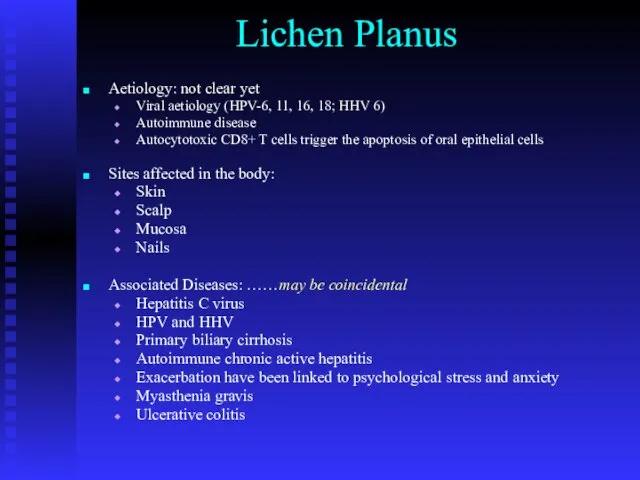
- 4. Lichen Planus Aetiology: not clear yet Viral aetiology (HPV-6, 11, 16, 18; HHV 6) Autoimmune disease
- 5. Skin lesions: Pink papules overlaid by fine white striations (Wickham’s striations). Itchy and bilateral Last for
- 6. Kobner phenomenon
- 7. Bilateral, itchy papules with scaly surface
- 8. Nail lesions: Vertical grooving and destruction of the nails (nails dystrophy).
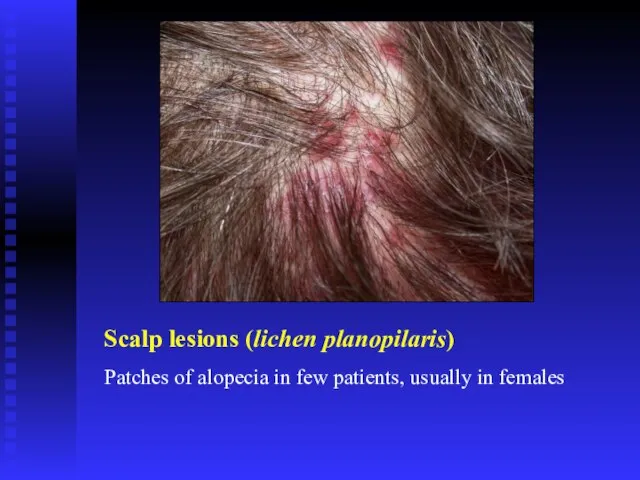
- 9. Scalp lesions (lichen planopilaris) Patches of alopecia in few patients, usually in females
- 10. Oral Lichen Planus Non-erosive Papular Linear Reticular Annular Plaque type Erosive Atrophic Bullous Ulcerative
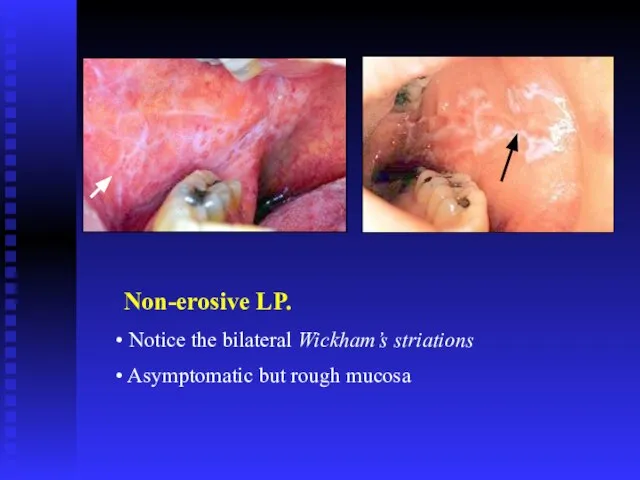
- 11. Non-erosive LP. Notice the bilateral Wickham’s striations Asymptomatic but rough mucosa
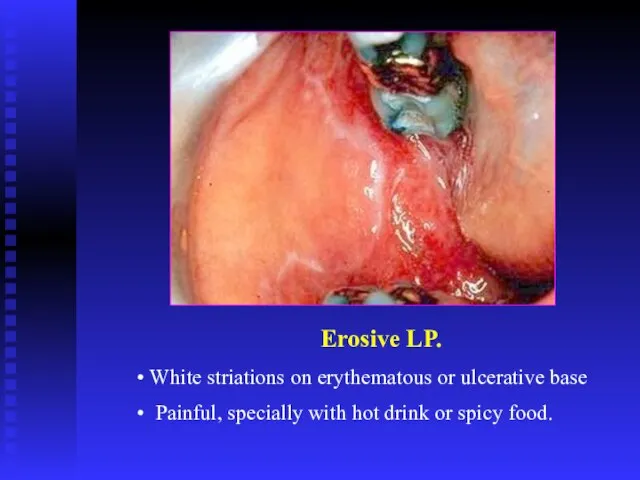
- 14. Erosive LP. White striations on erythematous or ulcerative base Painful, specially with hot drink or spicy
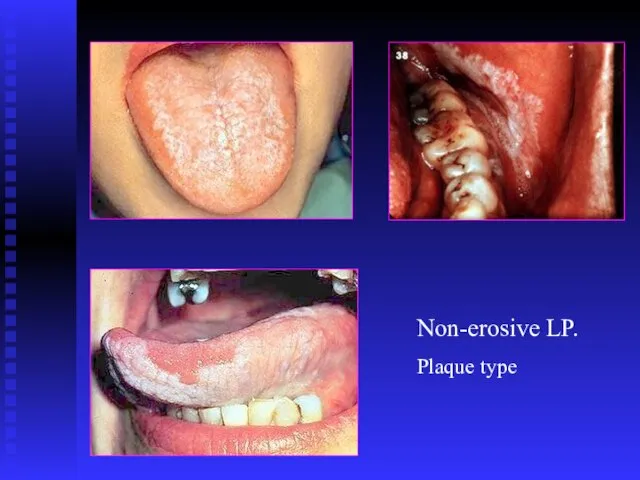
- 16. Non-erosive LP. Plaque type
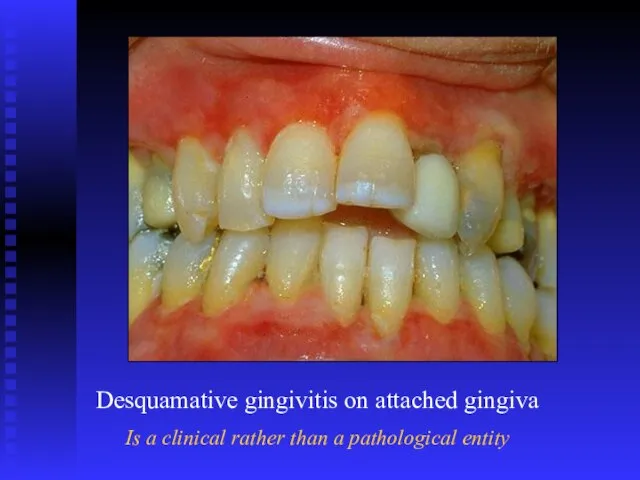
- 17. Desquamative gingivitis on attached gingiva Is a clinical rather than a pathological entity
- 18. Ulcers
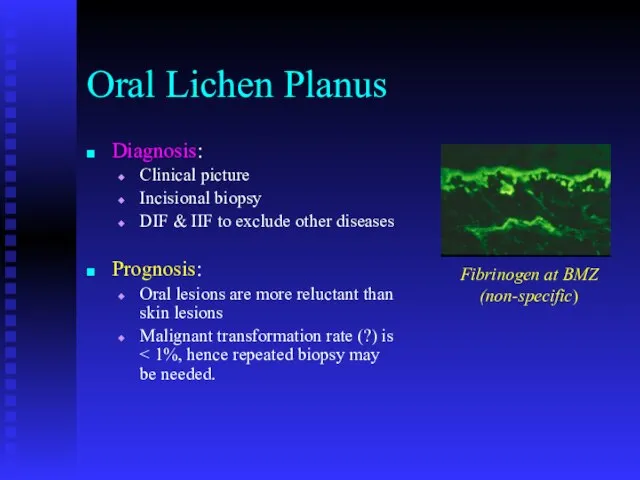
- 19. Oral Lichen Planus Diagnosis: Clinical picture Incisional biopsy DIF & IIF to exclude other diseases Prognosis:
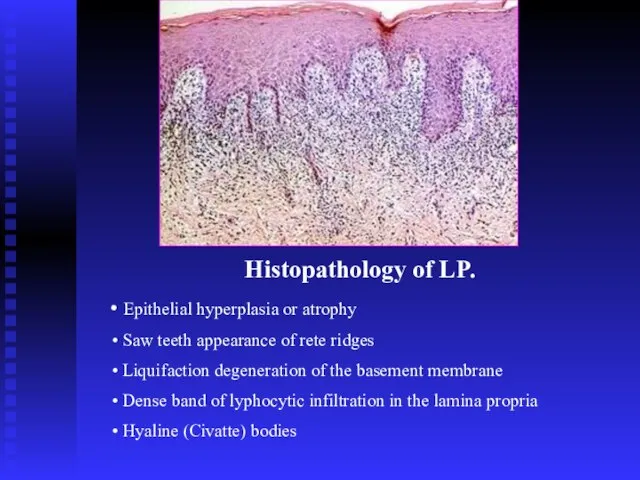
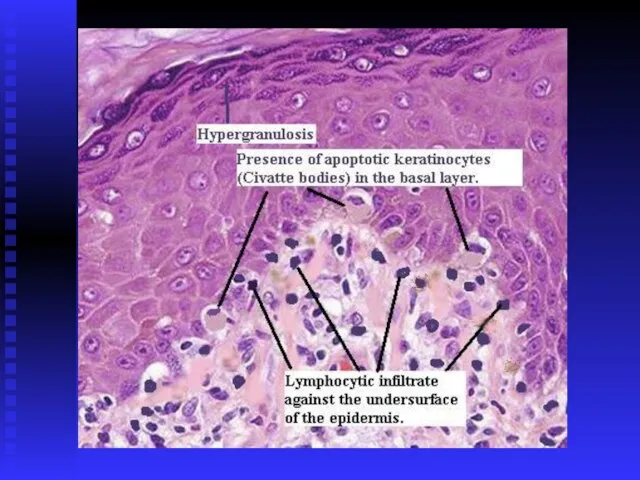
- 20. Histopathology of LP. Epithelial hyperplasia or atrophy Saw teeth appearance of rete ridges Liquifaction degeneration of
- 22. Treatment of OLP Aims of treatment Resolution of oral painful symptoms Resolution of oral mucosal lesions
- 23. Treatment of OLP. Skin lesions Steroid cream Systemic steroids Oral lesions: Minor erosive type Remove trauma
- 24. Treatment of OLP. Oral lesions: Major erosive type High concentration steroid mouth wash Triamcinolone intra-lesional injections
- 25. ?Potentially malignant condition 0.4%-2% per five years observation
- 26. OLP – Patient’s follow up Follow up: Every month till resolution of symptoms Every 6-12 month
- 27. Lichenoid eruption The expression or unmasking of the lichen planus antigen may be induced by: Drugs
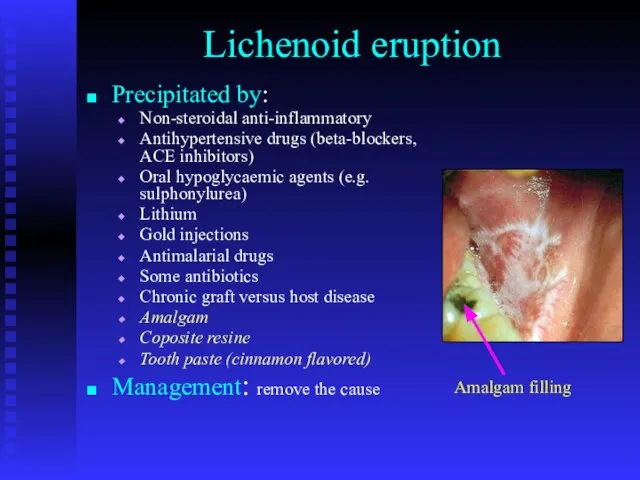
- 28. Lichenoid eruption Precipitated by: Non-steroidal anti-inflammatory Antihypertensive drugs (beta-blockers, ACE inhibitors) Oral hypoglycaemic agents (e.g. sulphonylurea)
- 29. Oral lichenoid lesions may be triggered by mechanical trauma (Koebner phenomenon) due to Calculus deposits Sharp
- 31. Pemphigus Auto-immune disease The patients usually between 40-60 years old Racial difference in incidence Most of
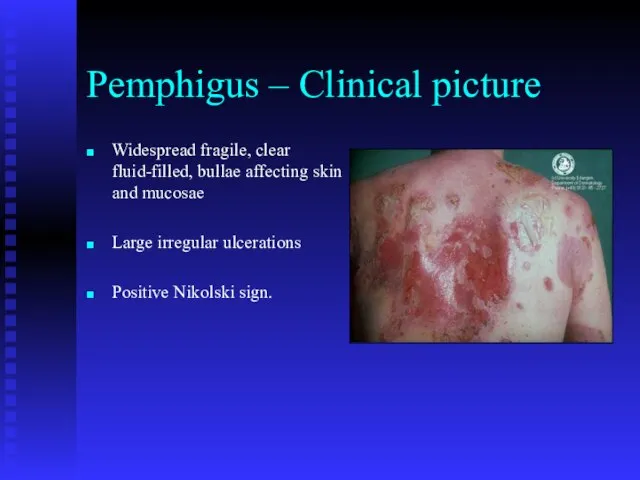
- 33. Pemphigus – Clinical picture Widespread fragile, clear fluid-filled, bullae affecting skin and mucosae Large irregular ulcerations
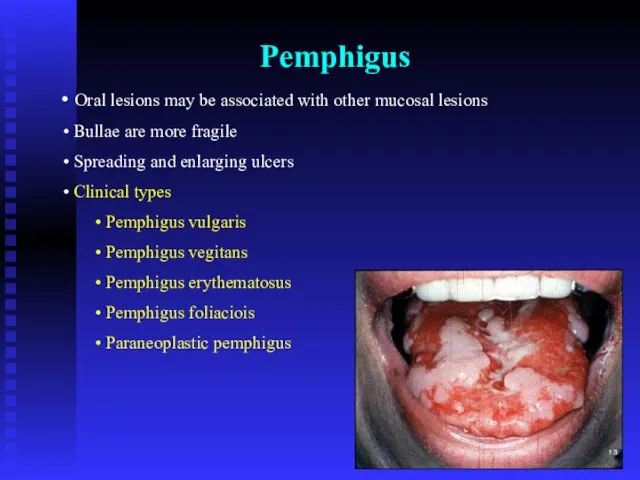
- 34. Pemphigus Oral lesions may be associated with other mucosal lesions Bullae are more fragile Spreading and
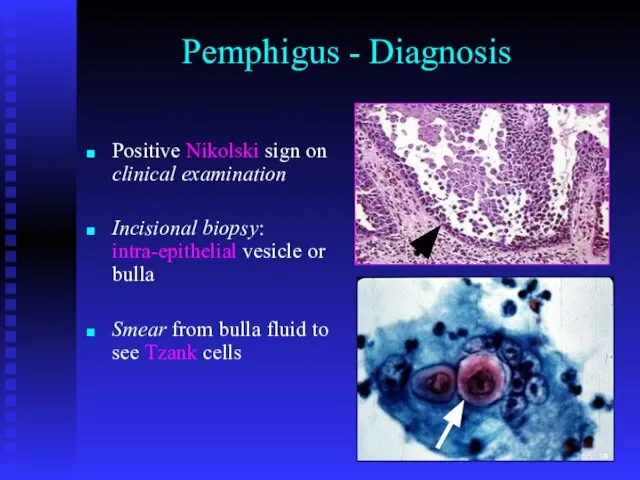
- 38. Pemphigus - Diagnosis Positive Nikolski sign on clinical examination Incisional biopsy: intra-epithelial vesicle or bulla Smear
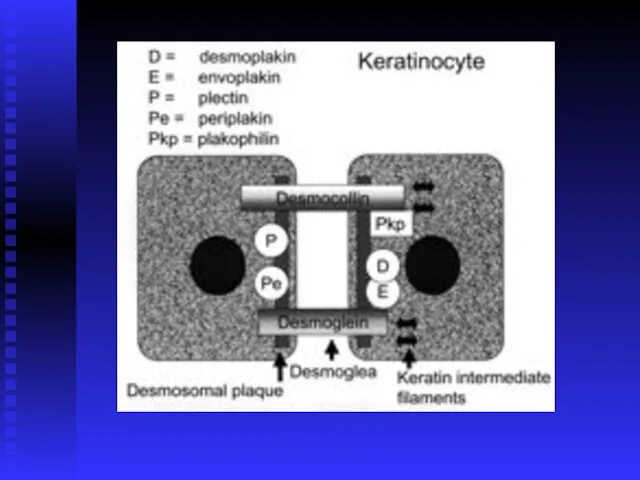
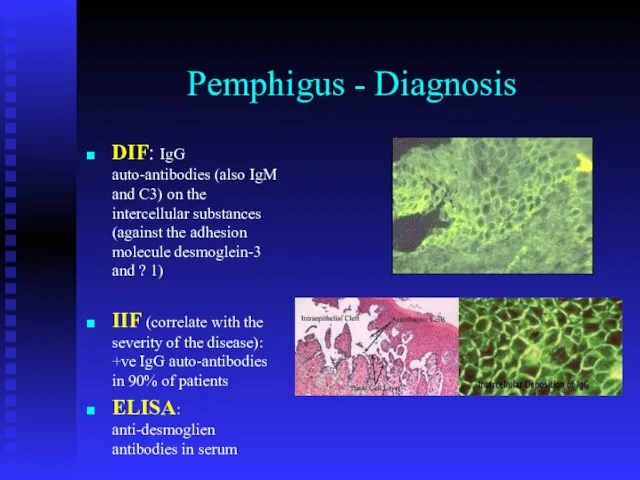
- 39. Pemphigus - Diagnosis DIF: IgG auto-antibodies (also IgM and C3) on the intercellular substances (against the
- 40. Direct & Indirect IF
- 41. Pemphigus - Treatment Multidisplinary Initial treatment with high doses of steroid (100mg prednisolone / day) Patients
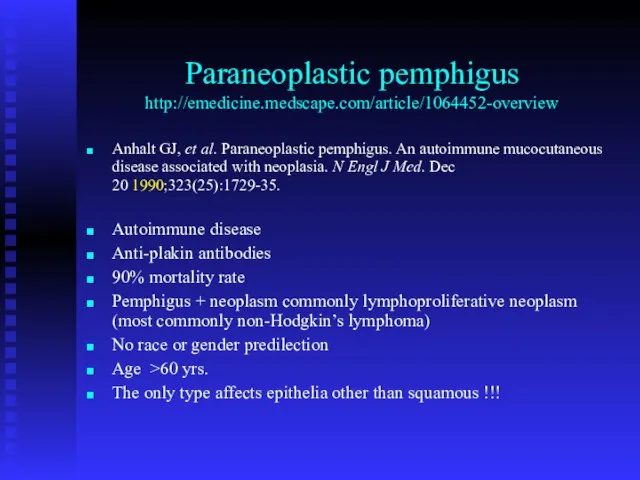
- 42. Paraneoplastic pemphigus http://emedicine.medscape.com/article/1064452-overview Anhalt GJ, et al. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia.
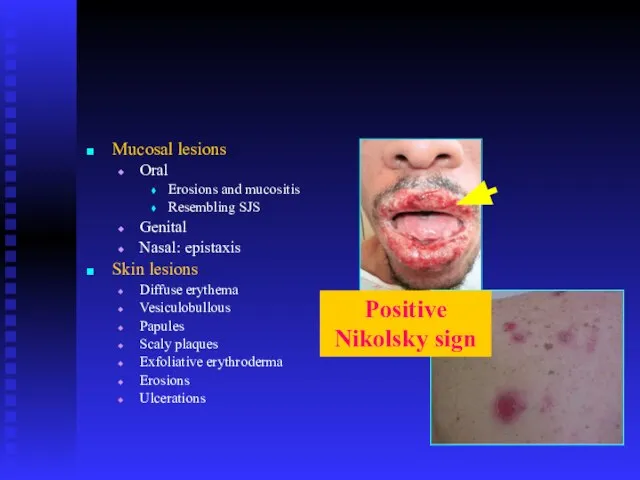
- 43. Mucosal lesions Oral Erosions and mucositis Resembling SJS Genital Nasal: epistaxis Skin lesions Diffuse erythema Vesiculobullous
- 44. Pemphigoid Auto-immune disease No racial predominance Two basic clinical types: Bullous (generalized) pemhigoid Mucousal (cicatricial) pemhigoid
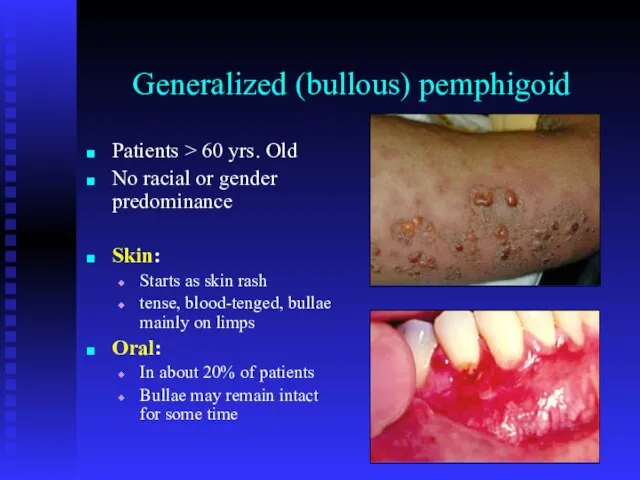
- 45. Generalized (bullous) pemphigoid Patients > 60 yrs. Old No racial or gender predominance Skin: Starts as
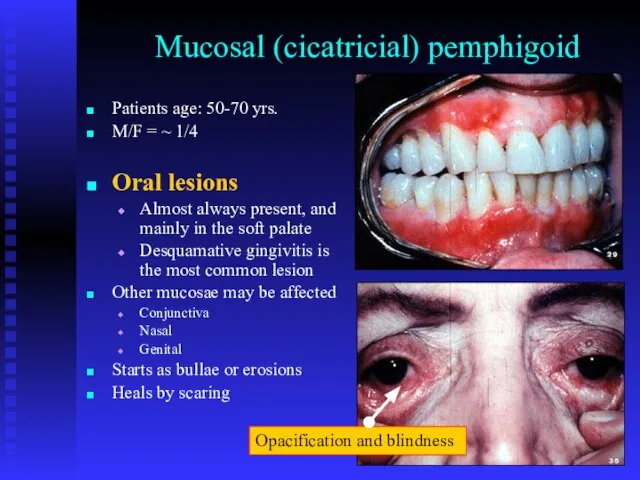
- 46. Mucosal (cicatricial) pemphigoid Patients age: 50-70 yrs. M/F = ~ 1/4 Oral lesions Almost always present,
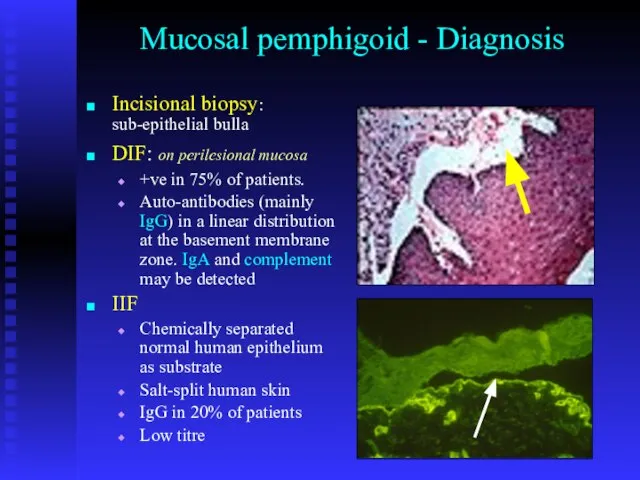
- 48. Mucosal pemphigoid - Diagnosis Incisional biopsy: sub-epithelial bulla DIF: on perilesional mucosa +ve in 75% of
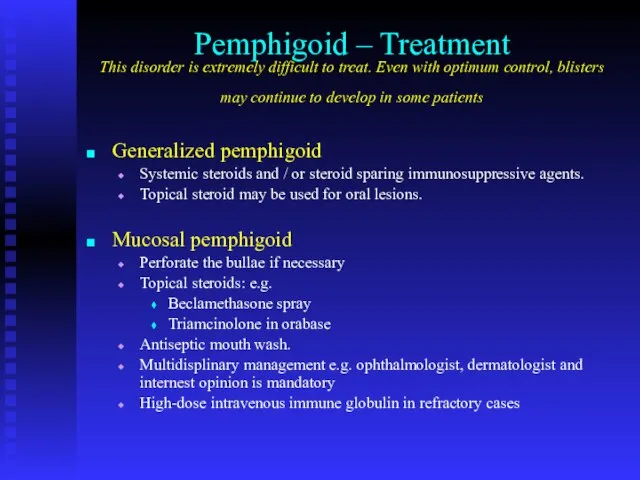
- 49. Pemphigoid – Treatment This disorder is extremely difficult to treat. Even with optimum control, blisters may
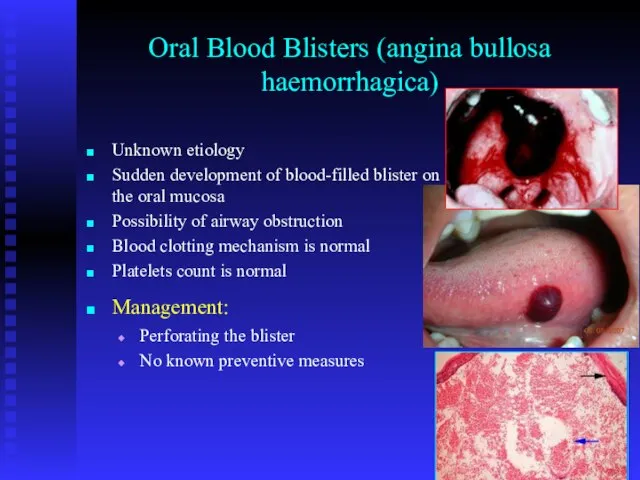
- 50. Oral Blood Blisters (angina bullosa haemorrhagica) Unknown etiology Sudden development of blood-filled blister on the oral
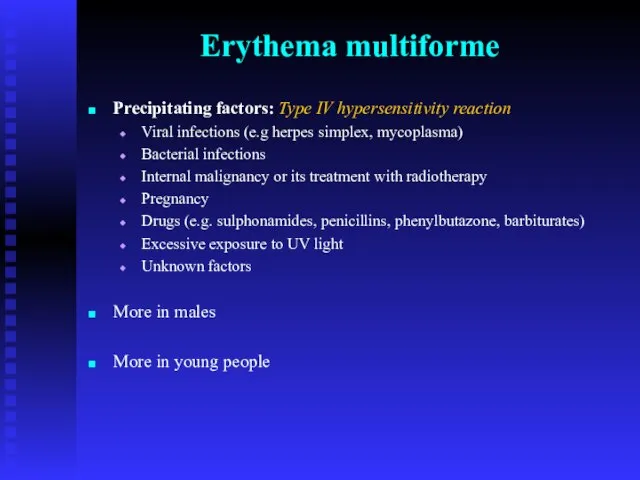
- 51. Erythema multiforme Precipitating factors: Type IV hypersensitivity reaction Viral infections (e.g herpes simplex, mycoplasma) Bacterial infections
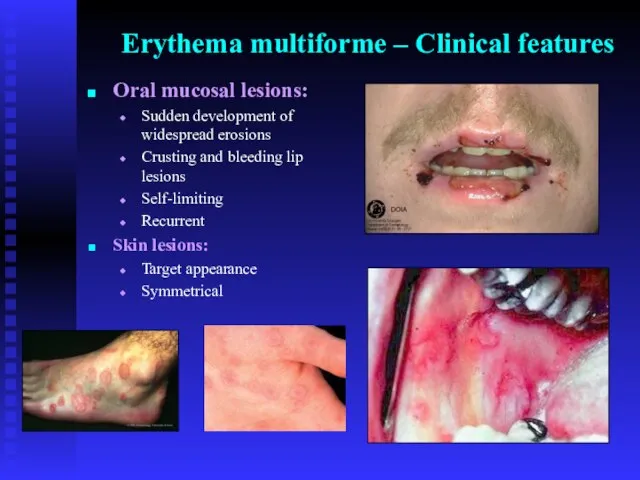
- 52. Erythema multiforme – Clinical features Oral mucosal lesions: Sudden development of widespread erosions Crusting and bleeding
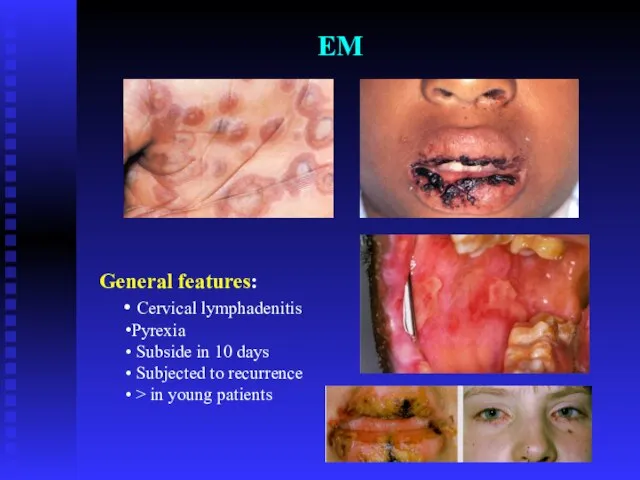
- 53. EM General features: Cervical lymphadenitis Pyrexia Subside in 10 days Subjected to recurrence > in young
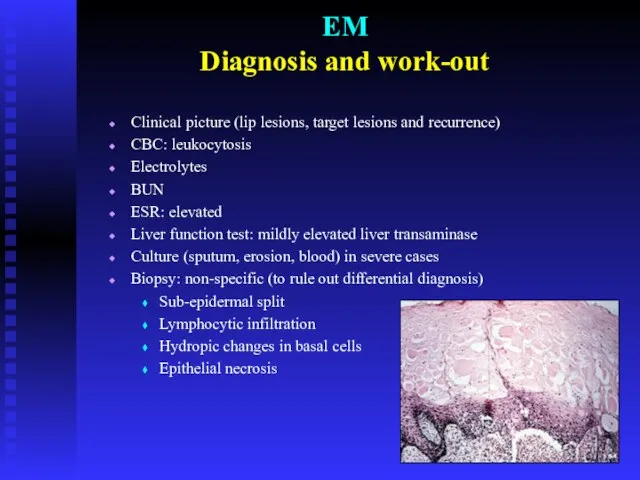
- 55. EM Diagnosis and work-out Clinical picture (lip lesions, target lesions and recurrence) CBC: leukocytosis Electrolytes BUN
- 56. EM Treatment - Management Remove the cause if possible Treat infections Fluid intake and soft diet;
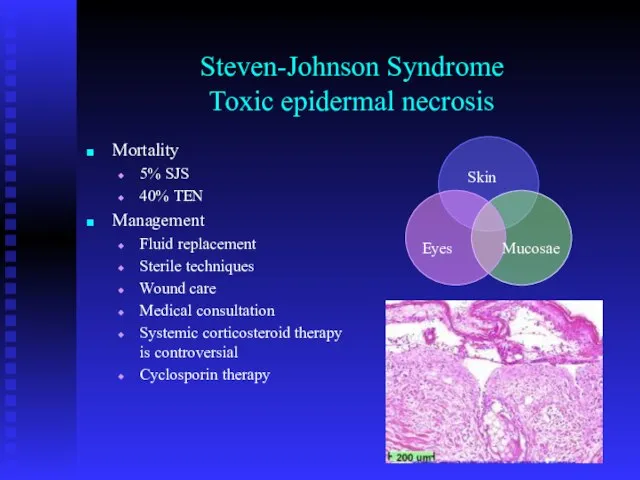
- 57. Steven-Johnson Syndrome Toxic epidermal necrosis Mortality 5% SJS 40% TEN Management Fluid replacement Sterile techniques Wound
- 59. Lupus Erythematosus Autoimmune disease Two main clinical divisions: Discoid lupus erythematosus (DLE) Systemic lupus erythematosus (SLE)
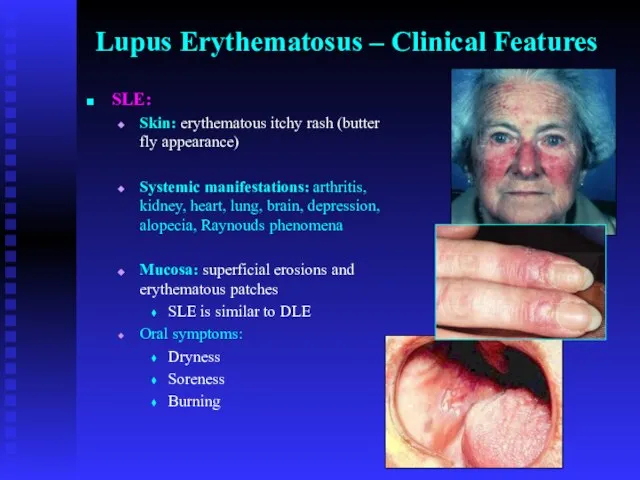
- 60. Lupus Erythematosus – Clinical Features SLE: Skin: erythematous itchy rash (butter fly appearance) Systemic manifestations: arthritis,
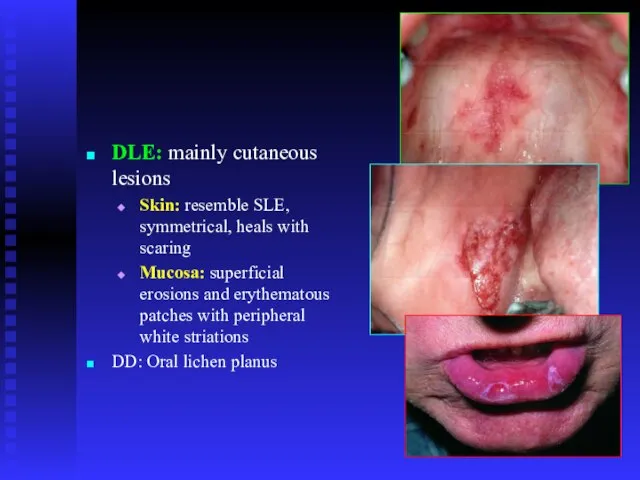
- 61. DLE: mainly cutaneous lesions Skin: resemble SLE, symmetrical, heals with scaring Mucosa: superficial erosions and erythematous
- 62. Lupus Erythematosus Diagnosis: IMF: antinuclear antibodies (ANA) +ve in 90% of patients. DMF Biopsy and histopathological
- 63. Prognosis No cure Renal disease is the main morbidity and mortality Thrombocytopenia and hemolytic anemia in
- 65. Скачать презентацию















 Панорамна фотозйомка
Панорамна фотозйомка СИСТЕМА ОПЛАТЫ ТРУДА ТК РФ СТАТЬЯ 135 «Установление заработной платы» Заработная плата работнику устанавливается трудовым договор
СИСТЕМА ОПЛАТЫ ТРУДА ТК РФ СТАТЬЯ 135 «Установление заработной платы» Заработная плата работнику устанавливается трудовым договор Воротники
Воротники Эссе на английском
Эссе на английском Раны, способы остановки кровотечений
Раны, способы остановки кровотечений Я умею ставить цели и достигать их
Я умею ставить цели и достигать их «Автоматизированная среда аттестации (АСА)»
«Автоматизированная среда аттестации (АСА)» Агентство по ипотечному жилищному кредитованию
Агентство по ипотечному жилищному кредитованию ФГУП машиностроительный завод им. Дзержинского
ФГУП машиностроительный завод им. Дзержинского Типы персональных компьютеров
Типы персональных компьютеров БАНК УРАЛСИБ НА РЫНКЕ Жилищно-коммунальных услуг
БАНК УРАЛСИБ НА РЫНКЕ Жилищно-коммунальных услуг РБС-Сеть — ваша партнёрская программа
РБС-Сеть — ваша партнёрская программа Правильные многогранники:
Правильные многогранники: Учимся делать салфетки
Учимся делать салфетки Зрительный диктант3
Зрительный диктант3 Петербург Достоевского
Петербург Достоевского Центр практических навыков СтГМА
Центр практических навыков СтГМА фрезерование
фрезерование Основы религиозных культур и светской этики
Основы религиозных культур и светской этики Человек и человечность. Что такое гуманизм
Человек и человечность. Что такое гуманизм Концепт для косметологической клиники
Концепт для косметологической клиники Вибродиагностика насосно-компрессорного оборудования
Вибродиагностика насосно-компрессорного оборудования Пищеварительная система у позвоночных животных
Пищеварительная система у позвоночных животных Индийско-российская программа развития телекоммуникаций и информационных технологий
Индийско-российская программа развития телекоммуникаций и информационных технологий Антонис ван Дейк и Снейдерс
Антонис ван Дейк и Снейдерс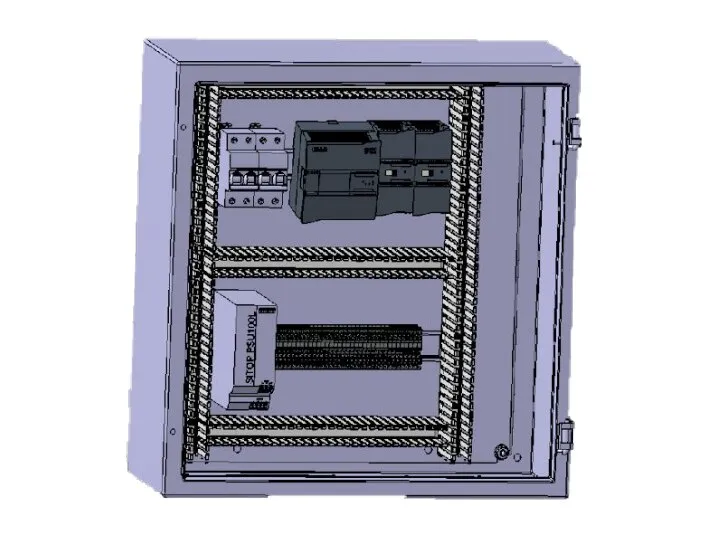 Электрошкаф
Электрошкаф Система «ОРГСТРУКТУРА»
Система «ОРГСТРУКТУРА» Терроризм угроза обществу
Терроризм угроза обществу