Содержание
- 2. Acute glomerulonephritis Acute GN is characterized by the abrupt onset of hematuria and proteinuria, often accompanied
- 3. Etiology Infectious Streptococcal Nonstreptococcal postinfectious glomerulonephritis Bacterial Viral Parasitic Noninfectious Multisystem systemic diseases Primary glomerular diseases
- 4. Pathogenesis Previously M-protein of the organism was felt to be responsible for PSGN. Recently, nephritis-associated streptococcal
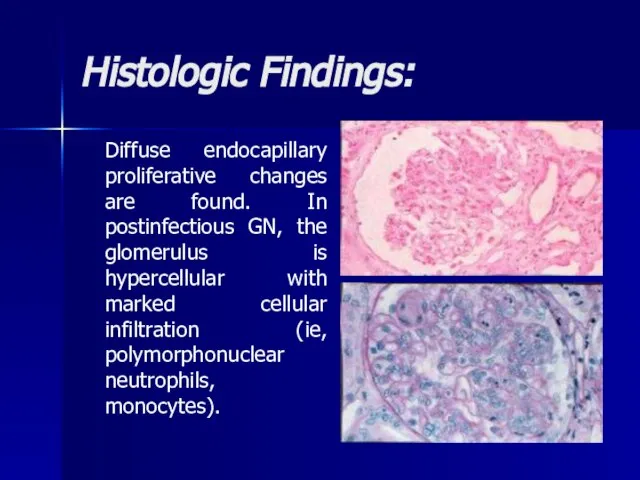
- 5. Pathology Diffuse endocapillary proliferative changes are found. In postinfectious GN, the glomerulus is hypercellular with marked
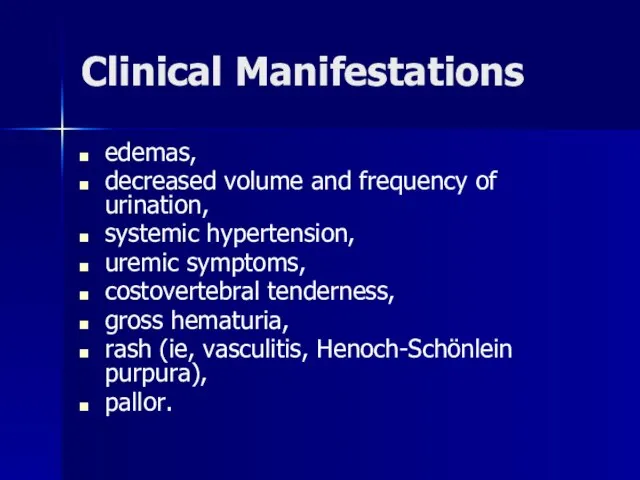
- 6. Clinical Manifestations edemas, decreased volume and frequency of urination, systemic hypertension, uremic symptoms, costovertebral tenderness, gross
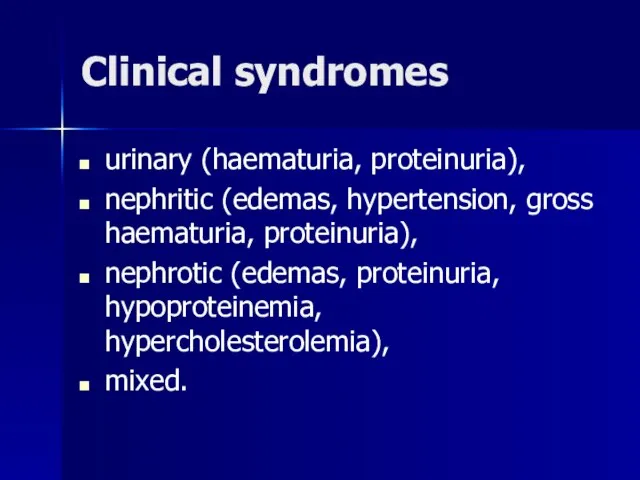
- 7. Clinical syndromes urinary (haematuria, proteinuria), nephritic (edemas, hypertension, gross haematuria, proteinuria), nephrotic (edemas, proteinuria, hypoproteinemia, hypercholesterolemia),
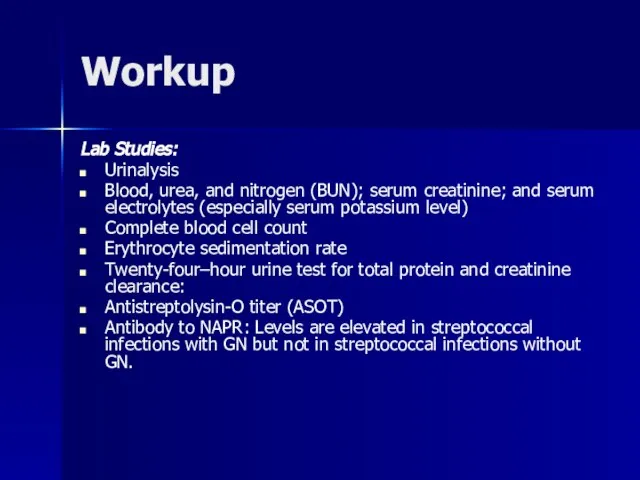
- 8. Workup Lab Studies: Urinalysis Blood, urea, and nitrogen (BUN); serum creatinine; and serum electrolytes (especially serum
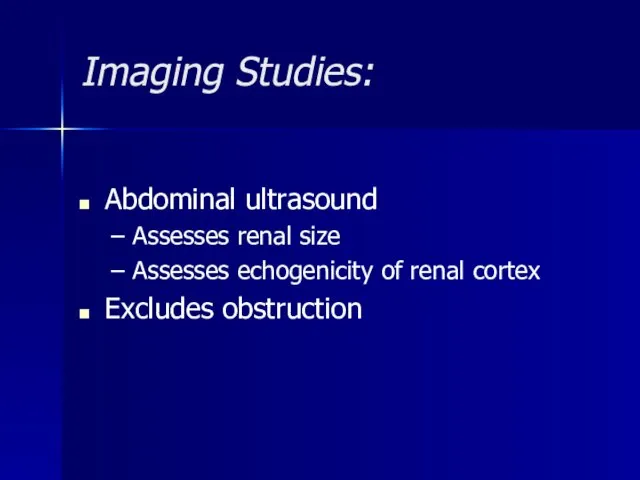
- 9. Imaging Studies: Abdominal ultrasound Assesses renal size Assesses echogenicity of renal cortex Excludes obstruction
- 10. Histologic Findings: Generally, a renal biopsy is not necessary for diagnosis of acute PSGN; however, in
- 11. Histologic Findings: Diffuse endocapillary proliferative changes are found. In postinfectious GN, the glomerulus is hypercellular with
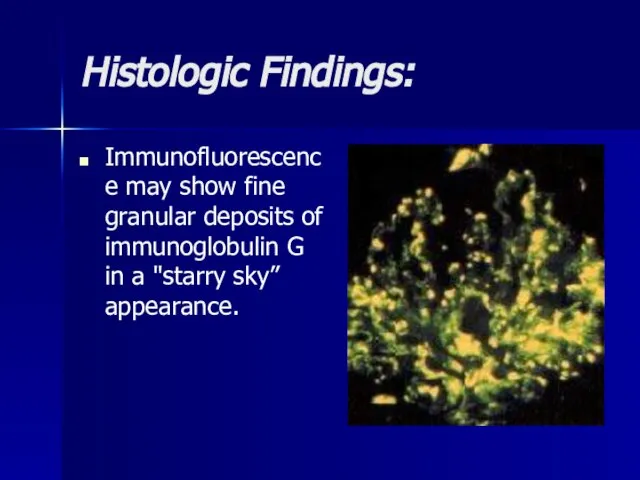
- 12. Histologic Findings: Immunofluorescence may show fine granular deposits of immunoglobulin G in a "starry sky” appearance.
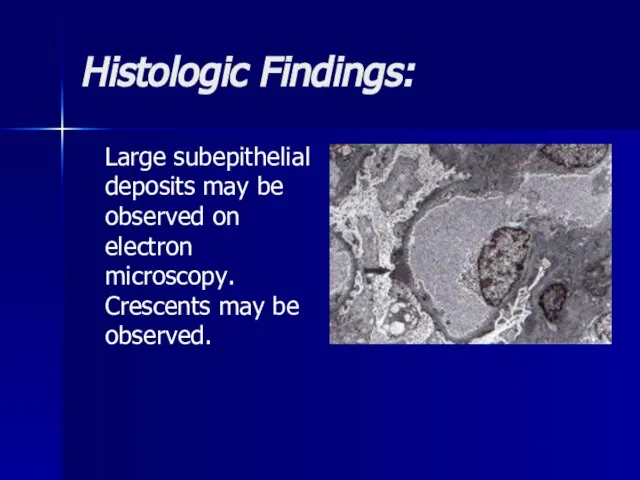
- 13. Histologic Findings: Large subepithelial deposits may be observed on electron microscopy. Crescents may be observed.
- 14. Differentials Crescentic Glomerulonephritis, Crescentic Glomerulonephritis, Diffuse Proliferative Glomerulonephritis, Crescentic Glomerulonephritis, Diffuse Proliferative Glomerulonephritis, Membranoproliferative Glomerulonephritis, Crescentic
- 15. Treatment Treat the underlying infections when acute GN is associated with chronic infections. Antimicrobial therapy Antibiotics
- 16. Prognosis Prognosis of acute PSGN is generally excellent in children. Within a week or so of
- 17. Chronic glomerulonephritis The condition is characterized by irreversible and progressive glomerular and tubulointerstitial fibrosis, ultimately leading
- 18. Etiology Nearly all forms of acute glomerulonephritis have a tendency to progress to chronic glomerulonephritis. The
- 19. Pathogenesis Reduction in nephron mass from the initial injury reduces the GFR. This reduction leads to
- 20. Histologic Findings In early stages, the glomeruli may still show some evidence of the primary disease.
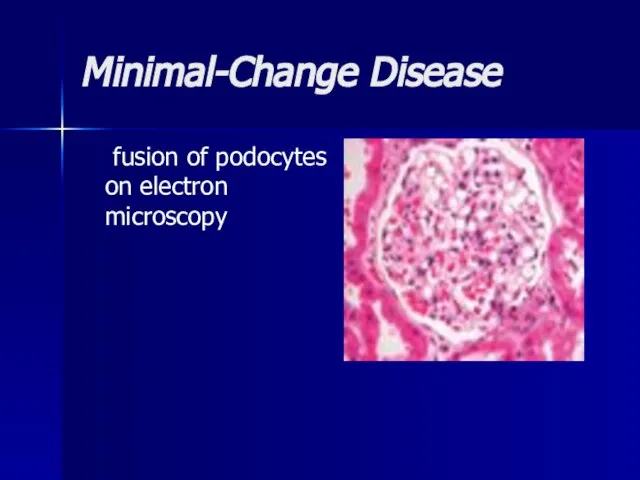
- 21. Minimal-Change Disease fusion of podocytes on electron microscopy
- 22. Focal segmental glomerulosclerosis Segmental areas of glomerular sclerosis, hyalinization of glomerular capillaries and positive IF for
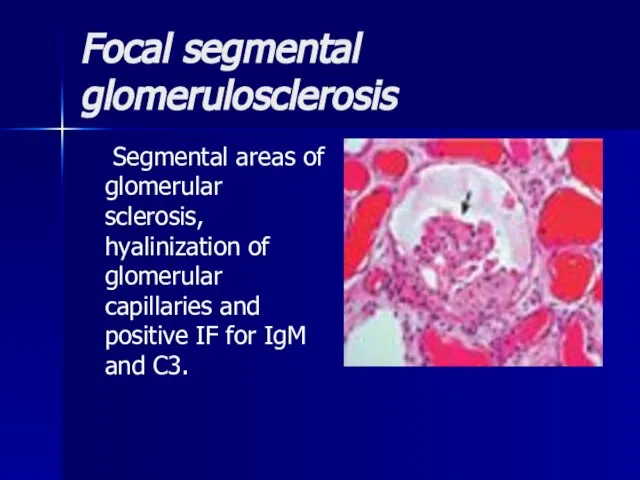
- 23. Mesangiocapillary GN large glomeruli with mesangial proliferation and ‘double’ BM. 2 histological types: type I (subendothelial
- 24. Membranous nephropathy thickened BM, IF +ve for IgG & C3 and subepithelial deposits on EM
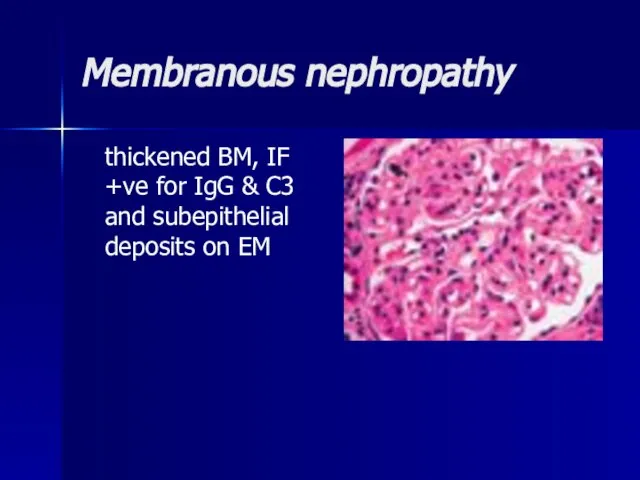
- 25. Mesangial proliferative GN Hypercellularity, mesangial proliferation, inflammatory cell infiltrate, positive IF for IgG and C3 and
- 26. Clinical Manifestations Uremia-specific findings Edemas Hypertension Jugular venous distension (if severe volume overload is present) Pulmonary
- 27. Clinical variants Latent (changes in urine) Hypertensive (increased blood pressure) Hematuric Nephrotic (edemas, proteinuria, hypoproteinemia, hypercholesterolemia),
- 28. Lab Studies Urinalysis Urinary protein excretion CBC count Serum chemistry Serum creatinine and urea nitrogen levels
- 29. Imaging Studies Renal ultrasonogram Obtain a renal ultrasonogram to determine renal size, to assess for the
- 30. Differentials Azotemia Azotemia, Chronic Renal Failure Azotemia, Chronic Renal Failure, Acute Glomerulonephritis, Azotemia, Chronic Renal Failure,
- 31. Treatment The target pressure for patients with proteinuria greater than 1 g/d is less than 125/75
- 32. Treatment Renal osteodystrophy can be managed early by replacing vitamin D and by administering phosphate binders.
- 33. Treatment Minimal change glomerulonephritis (MCGN) Corticosteroids induce remission in >90% of children and 80% of adults
- 34. Treatment Focal segmental glomerulosclerosis Poor response to corticosteroids (10–30%). Cyclophosphamide or ciclosporin (=cylosporin) may be used
- 35. Treatment Mesangiocapillary GN Treatment: None is of proven benefit. Prognosis: 50% develop ESRF.
- 36. Treatment Membranous nephropathy If renal function deteriorates, consider corticosteroids and chlorambucil (Ponticelli regimen). Prognosis: Untreated, 15%
- 37. Treatment Mesangial proliferative GN Antibiotics, diuretics, and antihypertensives as necessary. Dialysis is rarely required. Prognosis: Good.
- 38. Rapidly Progressive Glomerulonephritis Rapidly progressive glomerulonephritis (RPGN) is a disease of the kidney that results in
- 39. Etiology The cause of RPGN is unknown. A genetic predisposition may exist for the development of
- 40. Pathogenesis In the mid 1970s, a group of patients was described who fit the clinical criteria
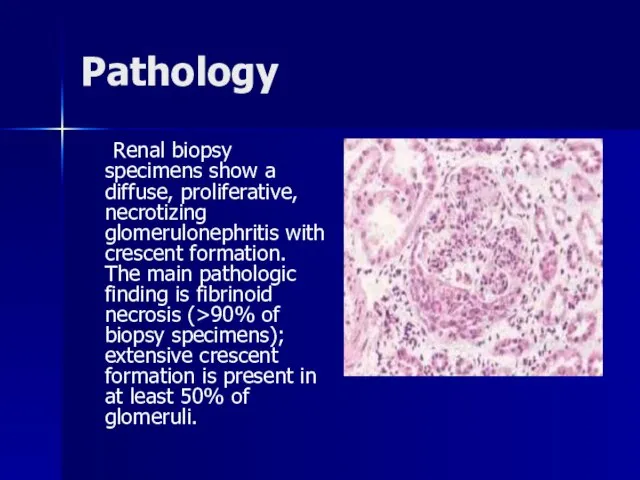
- 41. Pathology Renal biopsy specimens show a diffuse, proliferative, necrotizing glomerulonephritis with crescent formation. The main pathologic
- 42. Classification RPGN is classified pathologically into 3 categories: (1) anti-GBM antibody disease (approximately 3% of cases),
- 43. Clinical Manifestations Symptoms and signs of renal failure, loin pain, haematuria, systemic symptoms (fever, malaise, myalgia,
- 44. Workup: Lab Studies The most important requirement in the diagnosis ofantineutrophil cytoplasmic antibodies (ANCA) ANCA-associated disease
- 45. Differentials Amyloidosis, Amyloidosis, Antiphospholipid Syndrome, Amyloidosis, Antiphospholipid Syndrome, Churg-Strauss Syndrome, Amyloidosis, Antiphospholipid Syndrome, Churg-Strauss Syndrome, Cryoglobulinemia,
- 46. Treatment High-dose corticosteroids; cyclophosphamide ± plasma exchange/ renal transplantation. Prognosis: Poor if initial serum creatinine >600µmol/L.
- 47. Chronic Pyelonephritis Chronic pyelonephritis is renal injury induced by recurrent or persistent renal infection.
- 48. Etiology E. coli is the commonest (>70% in the community and 41% in hospital). Others include
- 49. Pathogenesis It occurs almost exclusively in patients with major anatomic anomalies, including urinary tract obstruction, struvite
- 50. Clinical Manifestations Fever Lethargy Nausea and vomiting Flank pain or dysuria Hypertension
- 51. Workup Lab Studies: Urinalysis Urinalysis results may reveal pyuria. Obtain a urine culture, which often isolates
- 52. Imaging Studies Intravenous urogram Voiding cystourethrogram. Radioisotopic scanning with technetium dimercaptosuccinic acid.
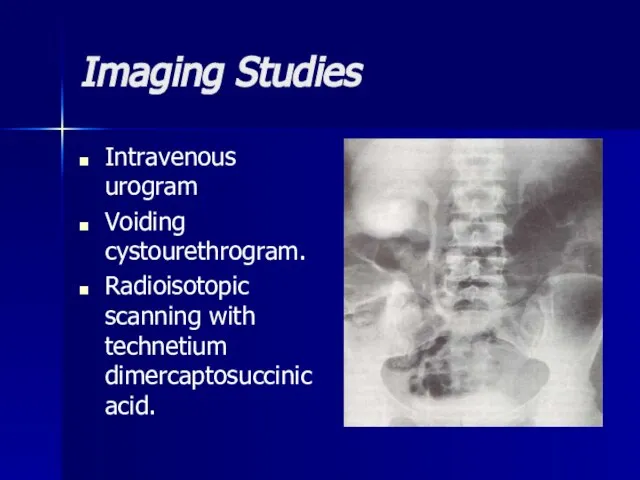
- 53. Imaging Studies Cystoscopy. Renal sonography. CT scan.
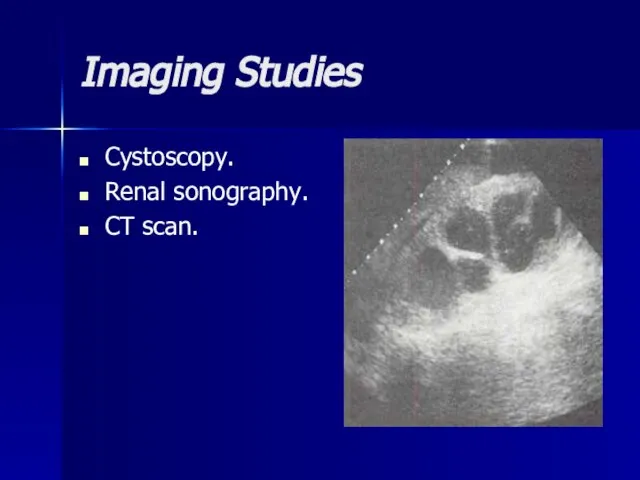
- 54. Differentials Azotemia, Azotemia, Chronic Renal Failure, Azotemia, Chronic Renal Failure, Hypertension, Azotemia, Chronic Renal Failure, Hypertension,
- 55. Treatment Medical therapy with antibiotics such as amoxicillin, trimethoprim/sulfamethoxazole (Bactrim), trimethoprim alone, or nitrofurantoin is usually
- 56. Surgical Care The following are indications for surgical therapy: Failure to comply with medical regimen Breakthrough
- 58. Скачать презентацию
 RRYa
RRYa Устройство стрелкового оружия
Устройство стрелкового оружия Система упражнений для формирования устойчивого навыка чтения у младших школьников
Система упражнений для формирования устойчивого навыка чтения у младших школьников Оборудование для шлифования дерева
Оборудование для шлифования дерева Обобщающий урок по теме «Производная и первообразная»
Обобщающий урок по теме «Производная и первообразная» День народного единства 17 сентября
День народного единства 17 сентября Взаимодействие ДОУ и семьи по экологическому воспитанию дошкольников
Взаимодействие ДОУ и семьи по экологическому воспитанию дошкольников  Узнай значения этих слов: красный угол трапеза благосостояние лад образ жизни родной очаг лампада поколение крестьянский мир домо
Узнай значения этих слов: красный угол трапеза благосостояние лад образ жизни родной очаг лампада поколение крестьянский мир домо Внутренняя энергия. Способы изменения внутренней энергии
Внутренняя энергия. Способы изменения внутренней энергии Особенности применения специальных налоговых режимов в РФ
Особенности применения специальных налоговых режимов в РФ Eye tracking
Eye tracking «Киевская Русь. Основные направления внутренней и внешней политики киевских князей».
«Киевская Русь. Основные направления внутренней и внешней политики киевских князей». Thinking Like economist
Thinking Like economist Развертки домов и силуэты котов для создания бумажного города
Развертки домов и силуэты котов для создания бумажного города ПРАВОВАЯ ОХРАНА ПРОГРАММ И ДАННЫХ. ЗАЩИТА ИНФОРМАЦИИ.
ПРАВОВАЯ ОХРАНА ПРОГРАММ И ДАННЫХ. ЗАЩИТА ИНФОРМАЦИИ. Единый день пенсионной грамотности
Единый день пенсионной грамотности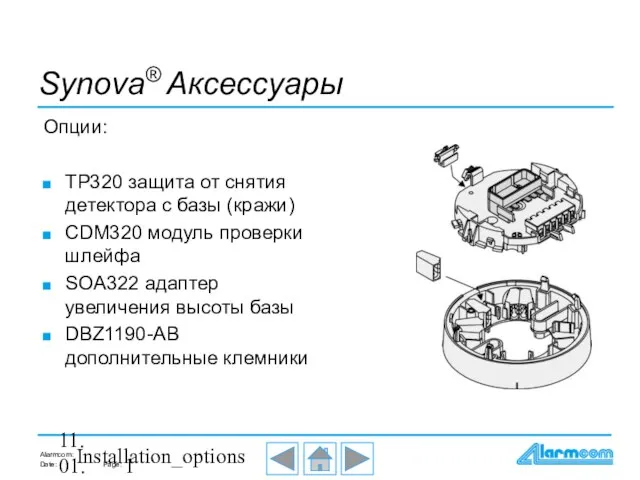 Synova® Аксессуары
Synova® Аксессуары Н. А. Некрасов Есть женщины в русских селеньях…
Н. А. Некрасов Есть женщины в русских селеньях…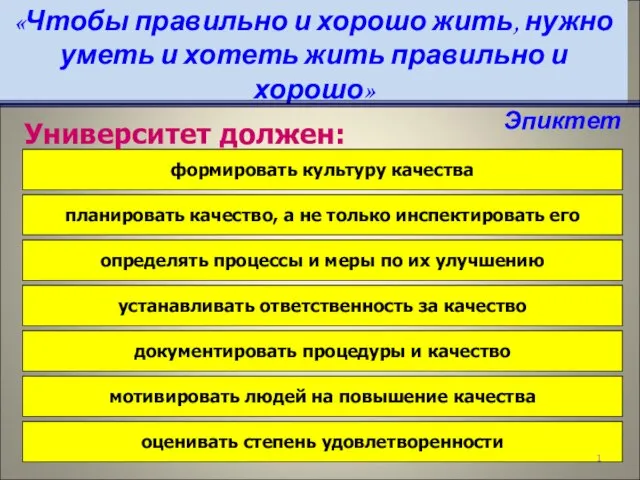 Университет должен:
Университет должен: Спасская башня
Спасская башня Презентация на тему Буддизм
Презентация на тему Буддизм  ГРИПП И ЕГО ПРОФИЛАКТИКА
ГРИПП И ЕГО ПРОФИЛАКТИКА www.dnevnik.ru
www.dnevnik.ru Деструктивное поведение подростка: как увидеть проблемы и предотвратить суицид
Деструктивное поведение подростка: как увидеть проблемы и предотвратить суицид Презентация на тему Одночлены. Арифметические операции над одночленами
Презентация на тему Одночлены. Арифметические операции над одночленами Профессия. Почтальон
Профессия. Почтальон פעילות מנייה פריטים בבית
פעילות מנייה פריטים בבית Внешнее строение, скелет и мускулатура земноводных
Внешнее строение, скелет и мускулатура земноводных