Содержание
- 2. Dyspepsia syndrome is determined as pain or discomfort localized in the epigastric area closer to the
- 3. Patients' complaints on admission corresponding to the complex of symptoms in gastric dyspepsia: pains in the
- 4. A complex of symptoms in dyspepsia syndrome is to be distinguished from the one in gastroesophageal
- 5. Depending on the causes triggering dyspeptic disorders, there is organic and functional (non-ulcerative) dyspepsia.
- 6. Organic dyspepsia is recognized if the following markers are highlighted: esophageal disease: reflux- esophagitis gastric disease:
- 7. If to exclude the diseases mentioned after a through examination, the patients (in case the dyspeptic
- 8. Classification of functional dyspepsia. According to A. Smout et al. (1992) - according to intestinal motility:
- 9. According to N. Talley (1991), M. von Oytryve et al. (1993) - ulcerative-like variant; - refluxoid
- 10. In 20-69% of patients with ulcerative-like variant the duodeno-gastric reflux, delayed evacuation from the stomach, and
- 11. Clinical variation of non-ulcerative dyspepsia. Depending on the either symptoms predominated in the clinical presentation of
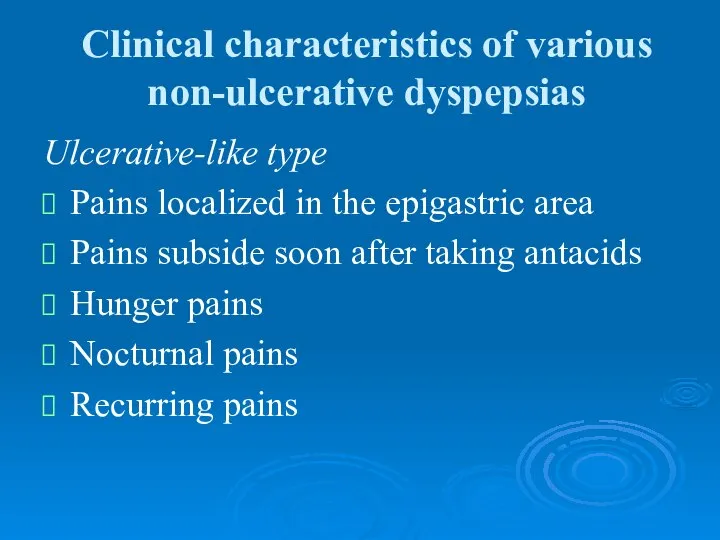
- 12. Clinical characteristics of various non-ulcerative dyspepsias Ulcerative-like type Pains localized in the epigastric area Pains subside
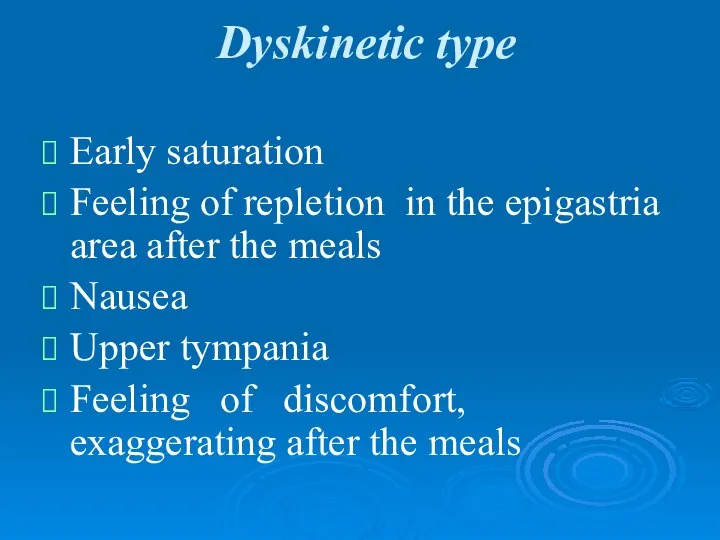
- 13. Dyskinetic type Early saturation Feeling of repletion in the epigastria area after the meals Nausea Upper
- 14. If the symptoms presented in patients do not correspond with the underlined variants, then the symptoms
- 15. Etiology and pathogenesis Chronic gastritis usually associated with pyloric helicobacterium (H. pylori), used to be recognized
- 16. Chronic gastritis associated with H. pylori is frequently revealed in patients with non-ulcerative dyspepsia syndrome. H.
- 17. The recent findings have also exposed the lack in distinction concerning the hydrochloric acid secretion in
- 18. Gastric and duodenal motility disorder proved to be the chief pathogenetic factors of non-ulcerative dyspepsia syndrome.
- 19. Correlation of various pathological and physiological mechanisms of functional dyspepsia with clinical symptoms.
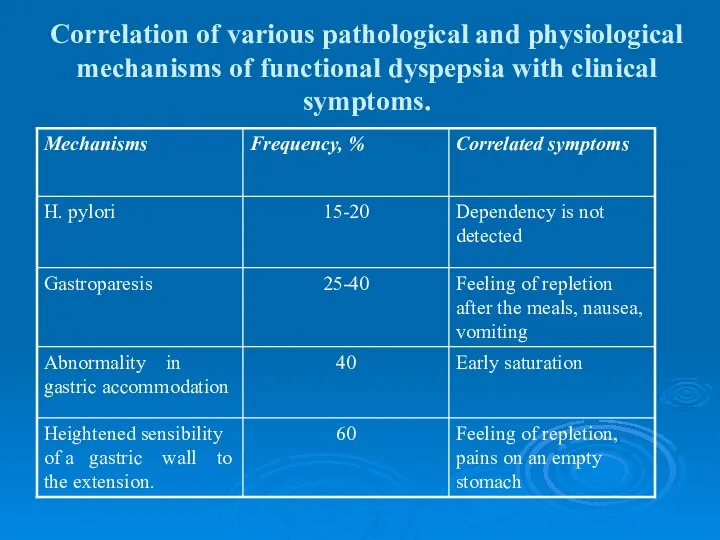
- 20. Gastric accommodation disorder (accommodation is determined here as capability of the fundic part of the stomach
- 21. Gastric accommodation disorder (accommodation is determined here as capability of the fundic part of the stomach
- 22. If stomach evacuates the food well, the cause for the dyspeptic complaints is a heightened sensibility
- 23. Diagnosis and differential diagnosis. A complex of symptoms in non-ulcerative dyspepsia is of no specific ground,
- 24. It is essential to take into account secondary motility derangement of the upper parts of the
- 25. The syndrome of gastric dyspepsia in ulcerative disease characterizes with response on food, seasonal character of
- 26. stomach ulcer The diagnostical method of stomach ulcer is an X-ray examination. But in some cases,
- 27. Stomach cancer Stomach cancer is manifested by gastric dyspepsia, which characterizes with persistence and progression. The
- 28. chronic cholecystitis Dyspeptic complaints have a more frequent occurrence during the chronic cholecystitis development. Vomiting is
- 29. During the period of exacerbation, patients complain of nausea, bitter taste, eructation with bitter. Due to
- 30. pancreatic dyspepsia is expressed in exacerbation or severe course of the disease. It is manifested by:
- 31. Gastric dyspepsia in chronic gastritis is characterized with the dependency on diet violence. It is presented
- 32. As the disease progresses, patients with chronic gastritis have tendency to hyposecretion and reduction in acidity
- 33. Antral gastritis, gastroduodenitis may resemble ulcerative disease of the duodenum in their clinical manifestations. The disease
- 34. Gastroesophageal reflux disease is a chronic recurrence conditioned by retrograde entrance of food mass into esophagus.
- 35. Pains in the epigastrium associated or not with the food taken may occur quite often. Vomiting
- 36. Methods of differential diagnosis applied in functional dyspepsia. Esophagogastroduodenoscopy X-ray examination Ultrasonography Intragastric and intraesophageal monitoring
- 37. Clinical and biomedical blood tests, as well as ultrasound investigations of the abdomen, gastroduodenoscopy and X-ray
- 38. It is supposed to be important to take alarm symptoms or «red flags» into account while
- 39. Alarm symptoms are characterized as follows: fever anemia dysphagy leukocytosis visible admixture accelerated ESR blood in
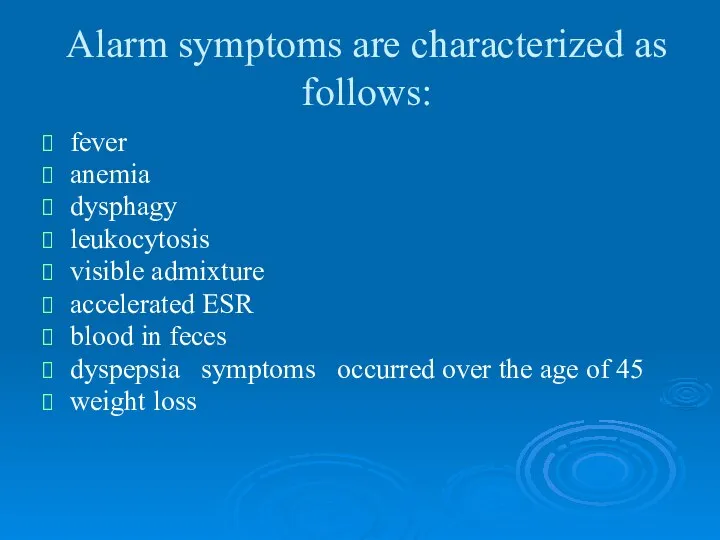
- 40. Treatment. The treatment procedures are to be complex and include not only drug administration, but also
- 41. Antacidic and antisecretory drugs (H2-blockers and blockers of proton pump) are indicated in ulcerative-like variant of
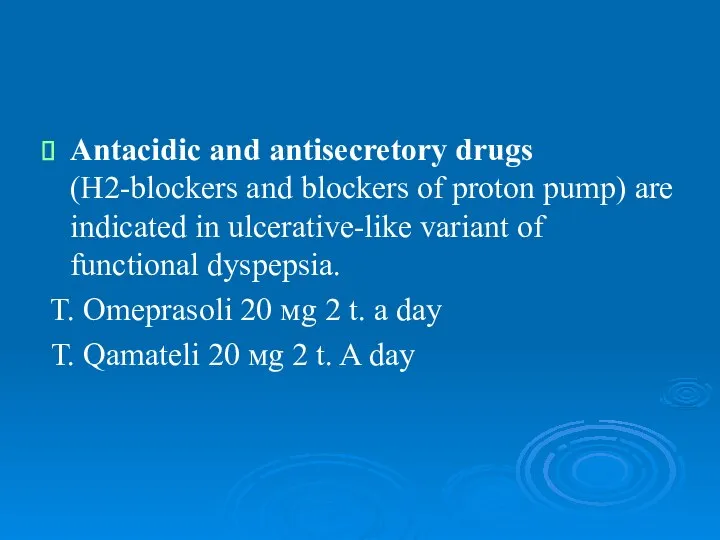
- 42. Some patients (about 20-25%) may express positive response to anti-helicobacterial eradication therapy. The treatment may have
- 43. Eradication therapy T. Omeprasoli 20 mg 2 t. a day T. Clarithromycini 500 mg 2 t.
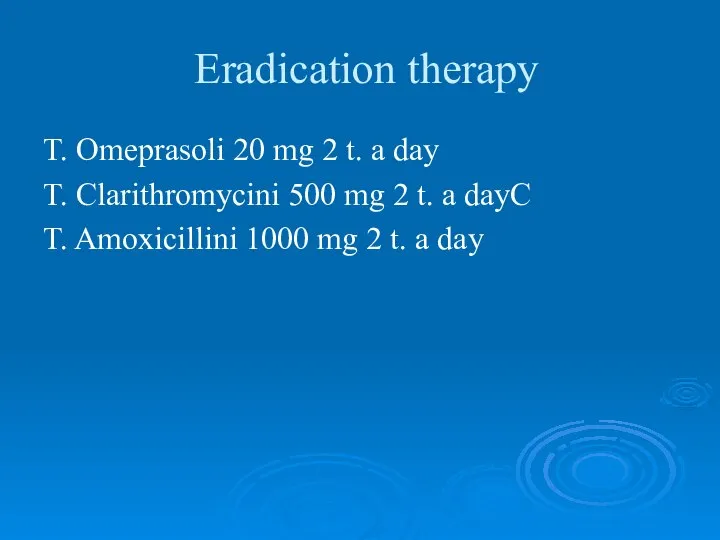
- 44. The basic means of patients' treatment of a developing dyskinetic variant is supposed to be prokinetic
- 45. The use of metodopramide (especially long-term one) may cause untoward and side effects in a great
- 46. European Motilium investigations in non-ulcerative dyspepsia treatment at doses of 5-20 mg 3-4 times a day
- 47. Итомед (Itomed) итоприда гидрохлорид 50 мг 3 раза в день side effects: -лейкопения, тромбоцитопения, гинекомастия, гиперпролактинемия;
- 48. Cyzapride (propulside, coordinacs) attracts much attention. This drug is quite effective in functional dyspepsia (in 60-90%>
- 50. Скачать презентацию
 Управление низкочастотным магнитным полем биохимическими процессами в биообъектах, содержащих магнитные наночастицы
Управление низкочастотным магнитным полем биохимическими процессами в биообъектах, содержащих магнитные наночастицы Влияние курения на организм
Влияние курения на организм Анатомічна термінологія
Анатомічна термінологія Хирургические методы лечения заболеваний пародонта: лоскутные операции и методы остеопластики дефектов альвеолярного отростка
Хирургические методы лечения заболеваний пародонта: лоскутные операции и методы остеопластики дефектов альвеолярного отростка Заболевание туберкулез
Заболевание туберкулез Расслоение аневризмы аорты. Клиника
Расслоение аневризмы аорты. Клиника Диффузные заболевания соединительной ткани
Диффузные заболевания соединительной ткани Дифтерия гортани – истинный круп
Дифтерия гортани – истинный круп Новые возможности ранней диагностики острого инфаркта миокарда
Новые возможности ранней диагностики острого инфаркта миокарда Объективный структурированный клинический экзамен – ОСКЭ
Объективный структурированный клинический экзамен – ОСКЭ Технологии социальной работы в сфере здравоохранения
Технологии социальной работы в сфере здравоохранения Иммунодефициты. Вторичные иммунодефициты
Иммунодефициты. Вторичные иммунодефициты Экстрагенитальные заболевания при беременности
Экстрагенитальные заболевания при беременности Osnovnye_i_vspomogatelnye_materialy
Osnovnye_i_vspomogatelnye_materialy Изоспорозы. Токсоплазмоз
Изоспорозы. Токсоплазмоз Foreign body removal techniques
Foreign body removal techniques Основные инфекционные болезни
Основные инфекционные болезни Патофизиология потерь жидкости
Патофизиология потерь жидкости Дифференциальная диагностика острых миокардитов с ревматическими поражениями сердца
Дифференциальная диагностика острых миокардитов с ревматическими поражениями сердца Клинический случай
Клинический случай Внутриаптечный контроль аптечной продукции
Внутриаптечный контроль аптечной продукции Эрозия зубов
Эрозия зубов Лабораторная диагностика ВИЧ и генитального герпеса
Лабораторная диагностика ВИЧ и генитального герпеса Профилактика неинфекционных заболеваний
Профилактика неинфекционных заболеваний Выделение. Строение и функция почек
Выделение. Строение и функция почек Гипертоническая болезнь
Гипертоническая болезнь Ларинготрахеит у детей
Ларинготрахеит у детей Возрастная физиология
Возрастная физиология