Содержание
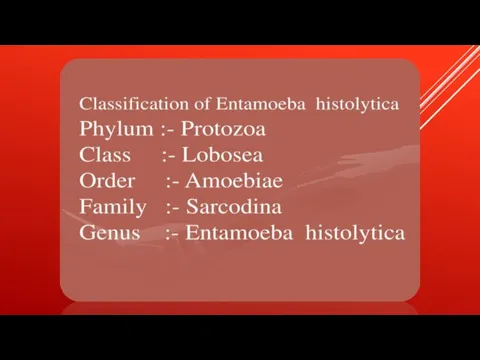
- 4. Anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and other primates causing amoebiasis,
- 7. It was thought that 10% of the world population was infected, but these figures predate the
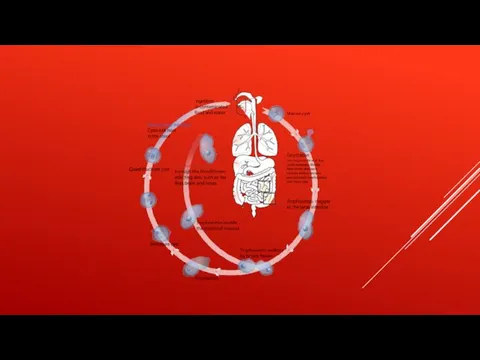
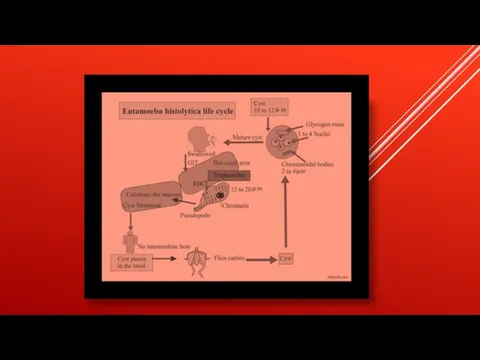
- 9. TRANSMISSION The active (trophozoite) stage exists only in the host and in fresh loose feces; cysts
- 11. The cysts are readily killed by heat and by freezing temperatures, and survive for only a
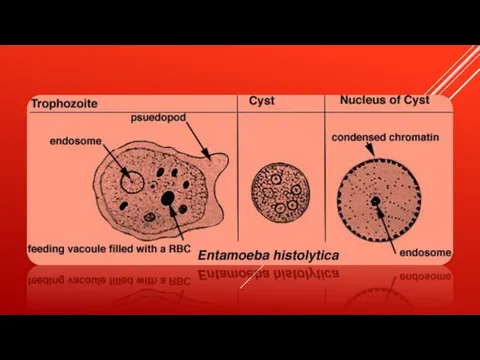
- 14. Symptoms can include fulminating dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain, and amoeboma. The amoeba
- 16. RISK FACTORS Poor sanitary conditions are known to increase the risk of contracting amebiasis E. histolytica.[8]
- 18. PATHOGEN INTERACTION E. histolytica may modulate the virulence of certain human viruses and is itself a
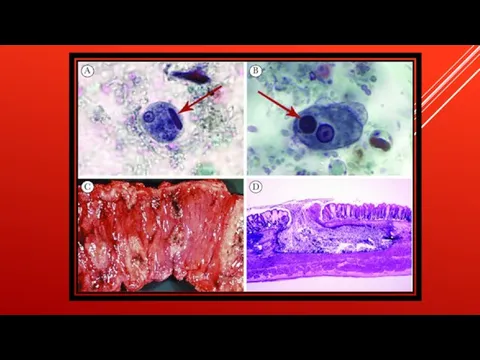
- 19. DIAGNOSIS Diagnosis is confirmed by microscopic examination for trophozoites or cysts in fresh or suitably preserved
- 21. Скачать презентацию
Слайд 4 Anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated
Anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated
![Anaerobic parasitic amoebozoan, part of the genus Entamoeba.[1] Predominantly infecting humans and](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/914432/slide-3.jpg)
to infect about 35-50 million people worldwide.[1] E. histolytica infection is estimated to kill more than 55,000 people each year
Слайд 7
It was thought that 10% of the world population was infected, but
It was thought that 10% of the world population was infected, but
these figures predate the recognition that at least 90% of these infections were due to a second species, E. dispar.[3] Mammals such as dogs and cats can become infected transiently, but are not thought to contribute significantly to transmission.
Слайд 9TRANSMISSION
The active (trophozoite) stage exists only in the host and in fresh
TRANSMISSION
The active (trophozoite) stage exists only in the host and in fresh
loose feces; cysts survive outside the host in water, in soils, and on foods, especially under moist conditions on the latter. The infection can occur when a person puts anything into their mouth that has touched the feces of a person who is infected with E. histolytica, swallows something, such as water or food, that is contaminated with E. histolytica, or swallows E. histolytica cysts (eggs) picked up from contaminated surfaces or fingers.
Слайд 11The cysts are readily killed by heat and by freezing temperatures, and
The cysts are readily killed by heat and by freezing temperatures, and
survive for only a few months outside of the host.[5] When cysts are swallowed they cause infections by excysting (releasing the trophozoite stage) in the digestive tract. The pathogenic nature of E. histolytica was first reported by Fedor A. Lösch in 1875,[1] but it was not given its Latin name until Fritz Schaudinn described it in 1903. E. histolytica, as its name suggests (histo–lytic = tissue destroying), is pathogenic; infection can be asymptomatic or can lead to amoebic dysentery or amoebic liver abscess.
Слайд 14Symptoms can include fulminating dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain,
Symptoms can include fulminating dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain,
and amoeboma. The amoeba can actually 'bore' into the intestinal wall, causing lesions and intestinal symptoms, and it may reach the blood stream. From there, it can reach different vital organs of the human body, usually the liver, but sometimes the lungs, brain, spleen, etc. A common outcome of this invasion of tissues is a liver abscess, which can be fatal if untreated. Ingested red blood cells are sometimes seen in the amoeba cell cytoplasm.
Слайд 16RISK FACTORS
Poor sanitary conditions are known to increase the risk of contracting
RISK FACTORS
Poor sanitary conditions are known to increase the risk of contracting
amebiasis E. histolytica.[8] In the United States, there is a much higher rate of amebiasis-related mortality in California and Texas, which might be caused by the proximity of those states to E. histolytica-endemic areas, such as Mexico, other parts of Latin America, and Asia.[9] E. histolytica is also recognized as an emerging sexually transmissible pathogen, especially in male homosexual relations, causing outbreaks in non-endemic regions.[10] As such, high-risk sex behaviour is also a potential source of infection.[11] Although it is unclear whether there is a causal link, studies indicate a higher chance of being infected with E. histolytica if one is also infected with HIV
Слайд 18PATHOGEN INTERACTION
E. histolytica may modulate the virulence of certain human viruses and is
PATHOGEN INTERACTION
E. histolytica may modulate the virulence of certain human viruses and is
itself a host for its own viruses.
For example, AIDS accentuates the damage and pathogenicity of E. histolytica.[13] On the other hand, cells infected with HIV are often consumed by E. histolytica. Infective HIV remains viable within the amoeba, although there has been no proof of human reinfection from amoeba carrying this virus.[23]
A burst of research on viruses of E. histolytica stems from a series of papers published by Diamond et al. from 1972 to 1979. In 1972, they hypothesized two separate polyhedral and filamentous viral strains within E. histolytica that caused cell lysis. Perhaps the most novel observation was that two kinds of viral strains existed, and that within one type of amoeba (strain HB-301) the polyhedral strain had no detrimental effect but led to cell lysis in another (strain HK-9). Although Mattern et al. attempted to explore the possibility that these protozoal viruses could function like bacteriophages, they found no significant changes in Entamoeba histolytica virulence when infected by viruses.
For example, AIDS accentuates the damage and pathogenicity of E. histolytica.[13] On the other hand, cells infected with HIV are often consumed by E. histolytica. Infective HIV remains viable within the amoeba, although there has been no proof of human reinfection from amoeba carrying this virus.[23]
A burst of research on viruses of E. histolytica stems from a series of papers published by Diamond et al. from 1972 to 1979. In 1972, they hypothesized two separate polyhedral and filamentous viral strains within E. histolytica that caused cell lysis. Perhaps the most novel observation was that two kinds of viral strains existed, and that within one type of amoeba (strain HB-301) the polyhedral strain had no detrimental effect but led to cell lysis in another (strain HK-9). Although Mattern et al. attempted to explore the possibility that these protozoal viruses could function like bacteriophages, they found no significant changes in Entamoeba histolytica virulence when infected by viruses.
Слайд 19DIAGNOSIS
Diagnosis is confirmed by microscopic examination for trophozoites or cysts in fresh
DIAGNOSIS
Diagnosis is confirmed by microscopic examination for trophozoites or cysts in fresh
or suitably preserved faecal specimens, smears of aspirates or scrapings obtained by proctoscopy, and aspirates of abscesses or other tissue specimen. A blood test is also available but is only recommended when a healthcare provider believes the infection may have spread beyond the intestine (gut) to some other organ of the body, such as the liver. However, this blood test may not be helpful in diagnosing current illness because the test can be positive if the patient has had amebiasis in the past, even if they are not infected at present.[26] Stool antigen detection and PCR are available for diagnosis, and are more sensitive and specific than microscopy.





 Переношенность
Переношенность Испаниядағы емдік туризм
Испаниядағы емдік туризм Культура питания
Культура питания Значение железа для организма. Лекарственные препараты, содержащие железо
Значение железа для организма. Лекарственные препараты, содержащие железо Неонатальные судороги
Неонатальные судороги Травмы половых органов у мужчин
Травмы половых органов у мужчин Гипоксия и нипероксия. (Лекция 13)
Гипоксия и нипероксия. (Лекция 13) Делирий. Диагностические критерии
Делирий. Диагностические критерии Диагностика рака шейки матки при беременности
Диагностика рака шейки матки при беременности Симптоматическая артериальная гипертензия
Симптоматическая артериальная гипертензия Миелин. Нарушение миелиновой оболочки
Миелин. Нарушение миелиновой оболочки Дефекты длинных трубчатых костей и их лечение
Дефекты длинных трубчатых костей и их лечение Формирование правильной осанки
Формирование правильной осанки Как продлить жизнь человека
Как продлить жизнь человека Mites and their manifestations
Mites and their manifestations Острый аппендицит
Острый аппендицит Мумификация. Варианты мумификации
Мумификация. Варианты мумификации Дистрофические заболевания слюнных желез
Дистрофические заболевания слюнных желез Физиология кожи
Физиология кожи Результаты оперативного лечения варикоцеле у мужчин
Результаты оперативного лечения варикоцеле у мужчин Внутренняя среда организма
Внутренняя среда организма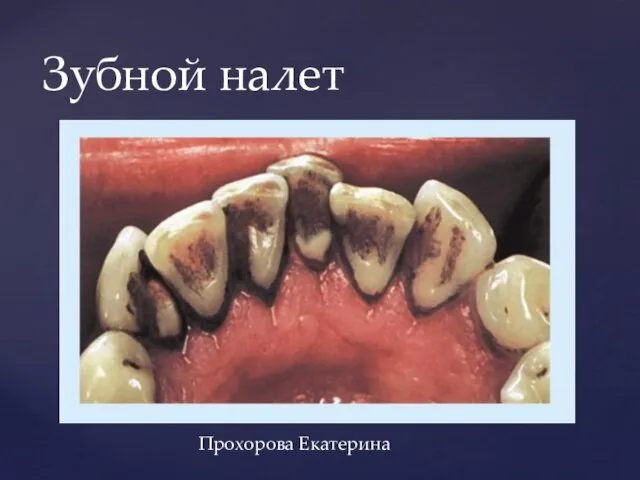 Зубной налет
Зубной налет Синдром встряхнутого ребенка
Синдром встряхнутого ребенка Этические комитеты: история создания, цели, задачи и их полномочия в России
Этические комитеты: история создания, цели, задачи и их полномочия в России Физиологическая беременность
Физиологическая беременность Неотложные состояния в урологии
Неотложные состояния в урологии Грибы в косметологии
Грибы в косметологии Сода в жизни человека
Сода в жизни человека