Содержание
- 2. Cardiomegaly is a considerable enlargement of the heart from its dilatation and/or hypertrophy, accumulation of waste
- 3. COMMON SIGNS OF CARDIOMEGALY Enlargement of the heart Rhythm and conduction disturbances Physical findings: widened borders
- 4. MAIN CAUSES OF CARDIOMEGALY IHD: atherosclerotic cardiosclerosis, post-infarction cardiosclerosis, ischemic cardiomyopathy, cardiac aneurysm Arterial hypertension Heart
- 5. DIAGNOSIS OF CARDIOMEGALY Interviewing the patient to find out the main complaints: dyspnoea, fatigability, weakness, less
- 6. DIAGNOSIS OF CARDIOMEGALY History. We should specify: consequence of development of heart failure symptoms (left or
- 7. DIAGNOSIS OF CARDIOMEGALY PHYSICAL EXAMINATION: Inspection: cyanosis, acrocyanosis, paleness, ruddiness of cheeks, swollen veins in the
- 8. DIAGNOSIS OF CARDIOMEGALY PHYSICAL EXAMINATION: Percussion: wider vascular bundle, wider borders of heart dullness Auscultation: dull
- 9. DIAGNOSIS OF CARDIOMEGALY LABORATORY FINDINGS: CDC: diagnosis of anaemia, polycythemia (COPD, cyanotic congenital heart defects), leucocytosis
- 10. DIAGNOSIS OF CARDIOMEGALY INSTRUMENTAL INVESTIGATIONS: Chest X-ray (shape of the heart, enlargement of certain chambers, vessels):
- 11. DIAGNOSIS OF CARDIOMEGALY INSTRUMENTAL INVESTIGATIONS: Echocardiography is the most valuable non-invasive methods of diagnosis assesses thoroughly
- 12. MANAGEMENT OF PATIENTS WITH CARDIOMEGALY To confirm cardiomegaly (to determine enlargement of the chambers, dilation or
- 13. MANAGEMENT OF PATIENTS WITH CARDIOMEGALY ASSESSMENT OF FUNCTIONAL SIGNIFICANCE OF CARDIOMEGALY: Symptoms of dyspnoea, weakness, fatigability
- 14. MANAGEMENT OF PATIENTS WITH CARDIOMEGALY PLANNING MANAGEMENT OF THE PATIENT: Prevention: changing lifestyle, treatment of hypertension,
- 15. CARDIOMYOPATHIES (CM) European Society of Cardiology (ESC), 2008 “Cardiomyopathies are structural and functional myocardial diseases in
- 16. CARDIOMYOPATHIES CM phenotypes HCM (hypertrophic CM) DCM (dilated CM) ARVD (arrhythmogenic right ventricular dysplasia) RCM (restrictive
- 17. ESC RECOMMENDATIONS (2008) All CM phenotypes are divided into: Familial (inherited, genetic) Non-identified genetic disorder A
- 18. Non-familial (acquired, non-genetic) Idiopathic A disease subgroup Toxic CM Endocrine CM Alimentary (nutritional) CM (thiamine or
- 19. HYPERTROPHIC CARDIOMYOPATHY Hypertrophic cardiomyopathy is defined by the presence of increased left ventricular (LV) wall thickness
- 20. HYPERTROPHIC CARDIOMYOPATHY 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy HCM is prevalently a
- 21. HYPERTROPHIC CARDIOMYOPATHY HCM is the main cause of sudden cardiac death (SCD) in the young, in
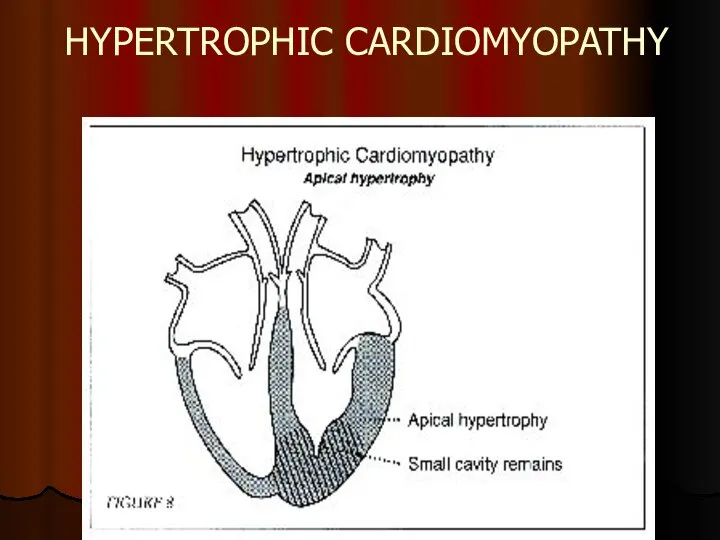
- 22. HYPERTROPHIC CARDIOMYOPATHY HCM is characterised by considerable (more than 15 mm) hypertrophy of myocardium of the
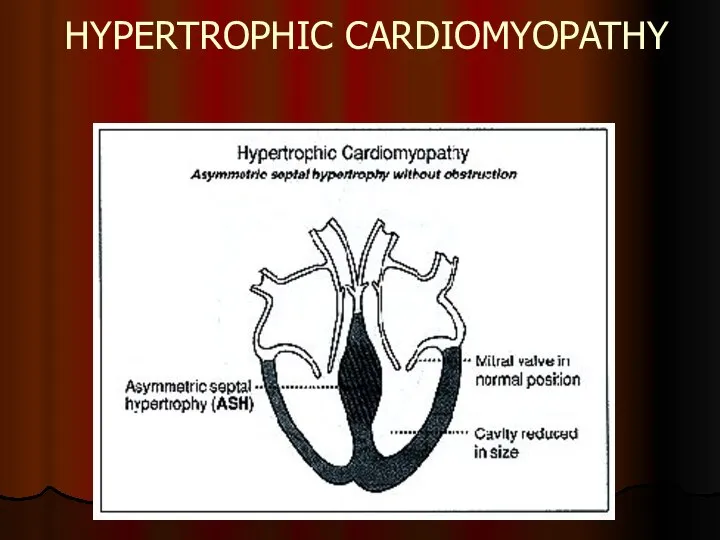
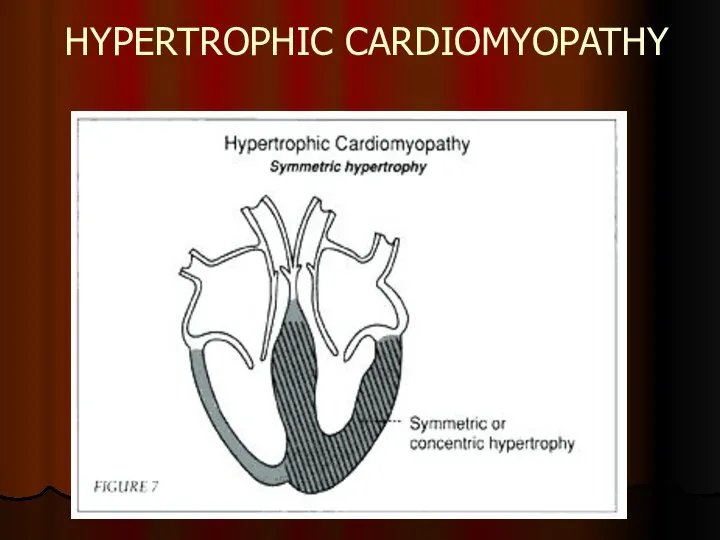
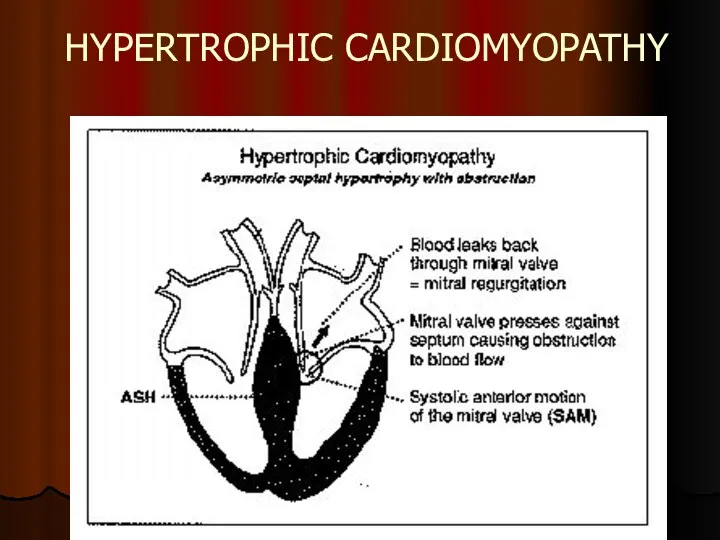
- 23. HYPERTROPHIC CARDIOMYOPATHY
- 24. HYPERTROPHIC CARDIOMYOPATHY
- 25. HYPERTROPHIC CARDIOMYOPATHY
- 26. HYPERTROPHIC CARDIOMYOPATHY
- 27. HYPERTROPHIC CARDIOMYOPATHY Pathogenesis of HCM includes 4 interrelated processes: Left ventricular outflow tract obstruction (LVOTO) Diastolic
- 28. HYPERTROPHIC CARDIOMYOPATHY CLINICAL MANIFESTATION: Asymptomatic course in 25% cases Dyspnoea on exertion (90%), orthopnoea; Angina (70-80%);
- 29. HYPERTROPHIC CARDIOMYOPATHY ON EXAMINATION: intense, raised cardiac impulse shifted slightly to the left double, triple or
- 30. HYPERTROPHIC CARDIOMYOPATHY DIAGNOSIS: DNA-diagnosis using polymerase chain reaction (PSR) Genetic testing of relations in the first
- 31. HYPERTROPHIC CARDIOMYOPATHY
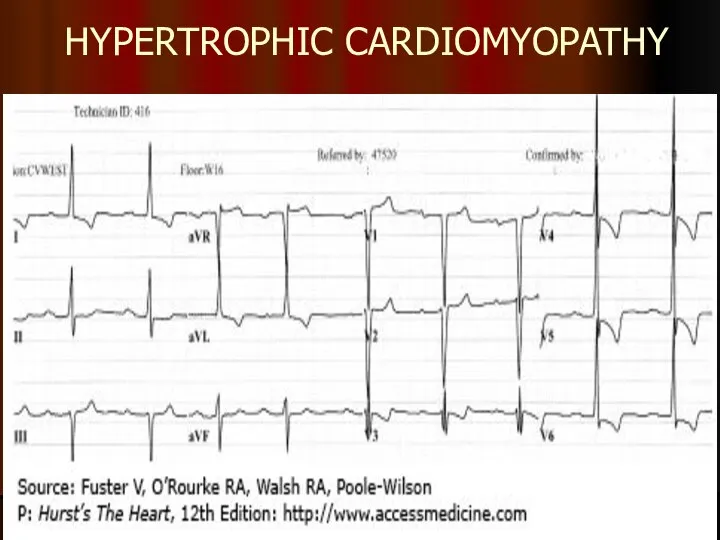
- 32. HYPERTROPHIC CARDIOMYOPATHY Left ventricular wall or IVS thickness >15 mm
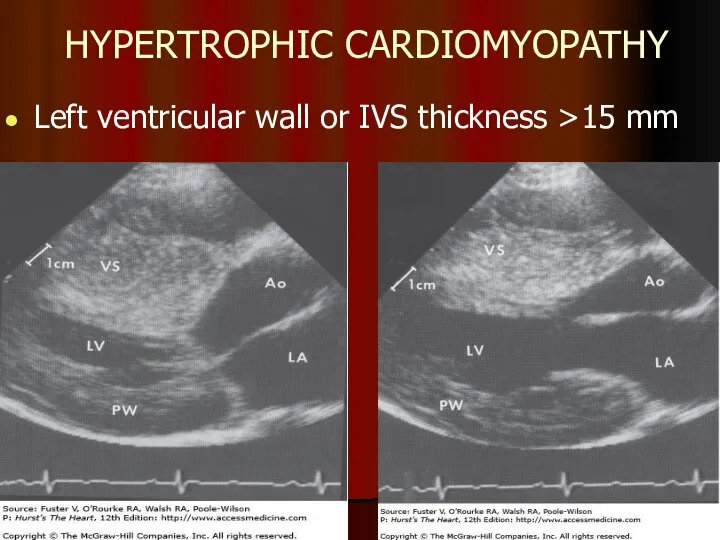
- 33. HYPERTROPHIC CARDIOMYOPATHY MEDICAL TREATMENT: ß-blockers Increase diastolic filling/relaxation of the LV Are first choice in obstructive
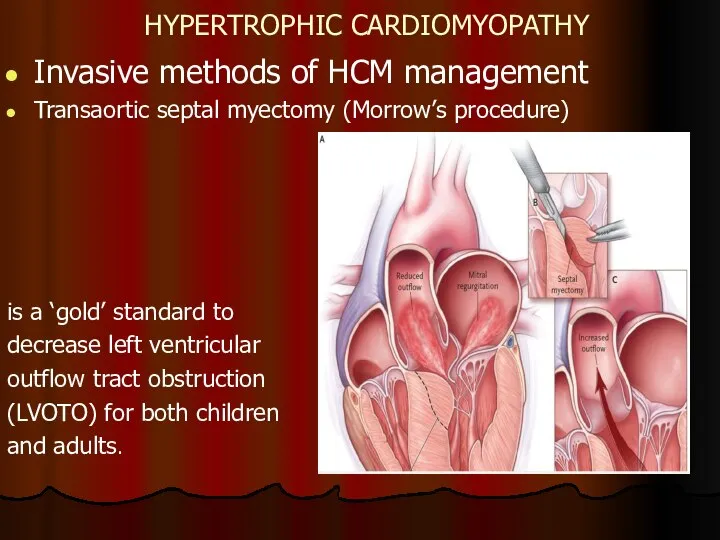
- 34. HYPERTROPHIC CARDIOMYOPATHY Invasive methods of HCM management Transaortic septal myectomy (Morrow’s procedure) is a ‘gold’ standard
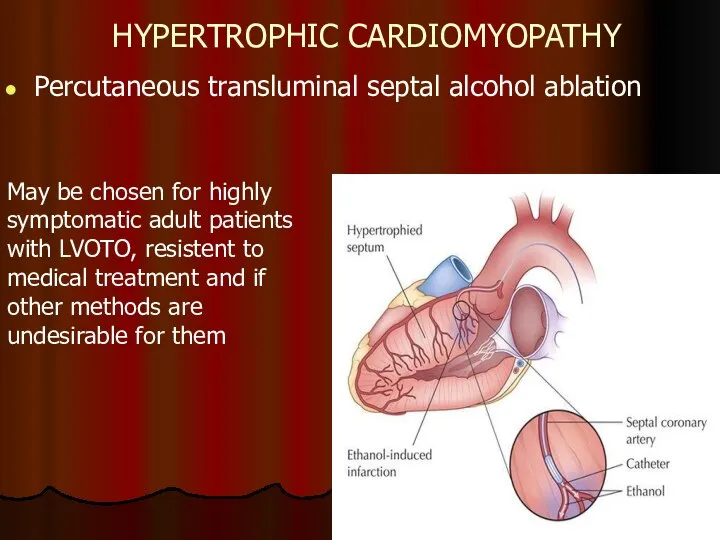
- 35. HYPERTROPHIC CARDIOMYOPATHY Percutaneous transluminal septal alcohol ablation May be chosen for highly symptomatic adult patients with
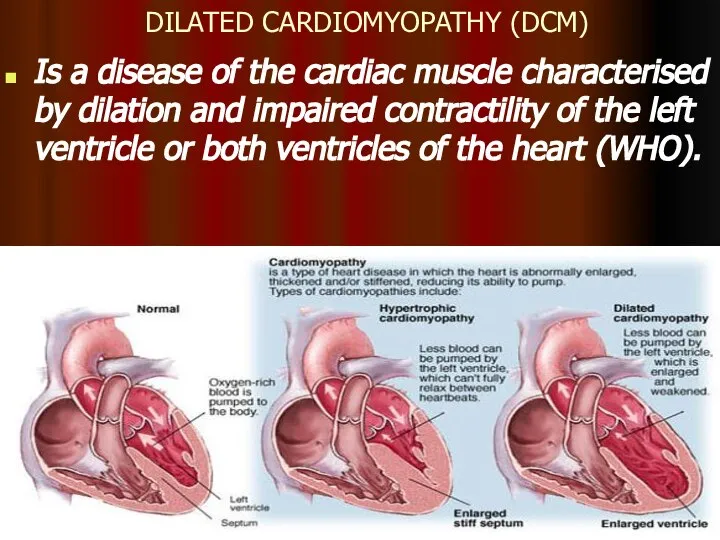
- 36. DILATED CARDIOMYOPATHY (DCM) Is a disease of the cardiac muscle characterised by dilation and impaired contractility
- 37. DILATED CARDIOMYOPATHY Dilated cardiomyopathy is responsible for 9% of all cases of heart failure. Incidence of
- 38. CLINICAL MANIFESTATIONS OF DCM Symptoms: palpitation, syncopes, weakness, dyspnoea, reduced exercise tolerance and sudden cardiac death.
- 39. CLINICAL MANIFESTATIONS OF DCM Physical changes Inspection, palpation: Swollen, pulsating jugular veins Diffuse apical pulse shifted
- 40. DIAGNOSIS OF DCM ECG: no specific changes - Ventricular arrhythmia - Atrial fibrillation - Impaired contractility
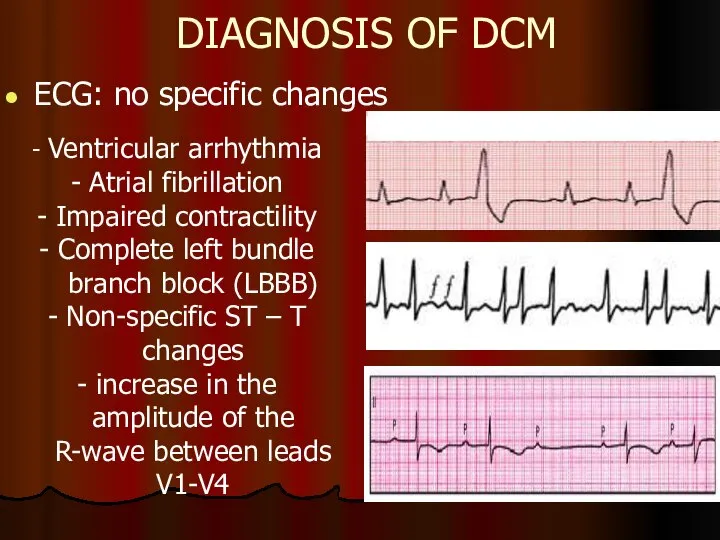
- 41. DIAGNOSIS OF DCM Cardiomegaly (cardiothoracic ratio > 50%) Pulmonary congestion
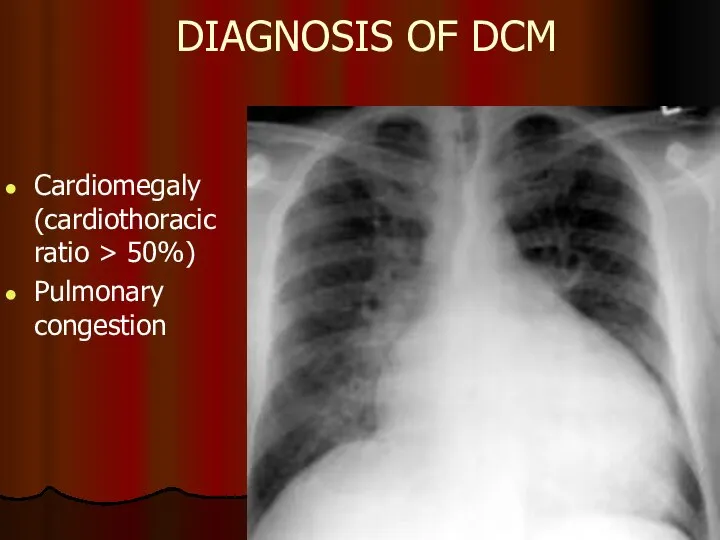
- 42. DIAGNOSIS OF DCM Dilation of heart cavities EF Sings of pulmonary hypertension Hypokinesis of walls No
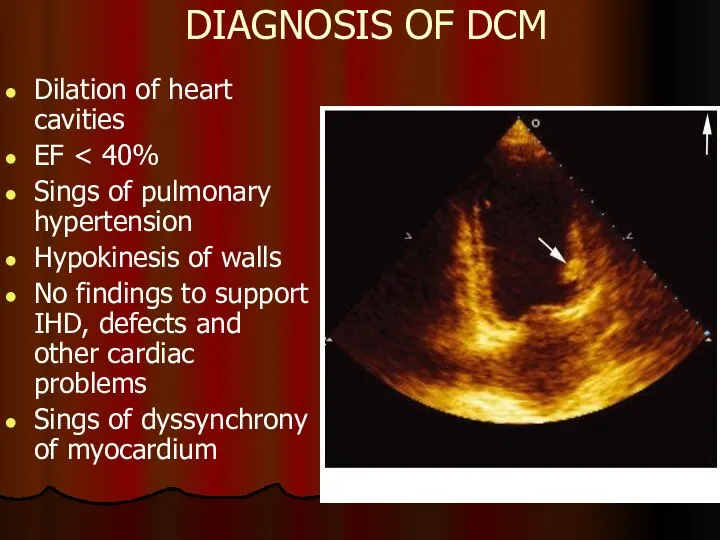
- 43. DIAGNOSIS OF DCM Radionuclide methods Can be used to assess the size of heart chambers, contractility
- 44. EXCLUSION CRITERIA FOR DCM Systemic arterial hypertension (> 160/100 mm Hg) Ischaemic heart diseases (50% coronary
- 45. MANAGEMENT OF DCM To exclude factors which may worsen dysfunction of myocardium Medical treatment: Management of
- 46. MYOCARDITIS Inflammatory impairment of the heart muscle due to influence (direct or indirect through immune mechanisms)
- 47. ETIOLOGY OF MYOCARDITIS Bacteria Rickettsiae and Spirochaete Viruses Protozoa Fungi Parasitic diseases Deficiencies (hypophosphataemia, hypomagnesemia, hypocalcaemia,
- 48. VIRAL INFECTION IN MYOCARDITIS Coxsackie of A and B groups, ЕСНО, A and B flu, herpes
- 49. MYOCARDITIS THE COURSE OF THE DISEASE Mild: mostly focal, without cavity dilation, systolic dysfunction, potentially dangerous
- 50. DIAGNOSIS OF MYOCARDITIS 1 CRITERIA OF INFLAMMATION, INFECTION: Fatigue, hyperthermia, accelerated ESR, leucocytosis, elevation of C-reactive
- 51. DIAGNOSIS OF MYOCARDITIS 2 CRITERIA OF MYOCARDIAL INVOLVEMENT: Clinical: cardialgia, heart palpitations, irregular heart work, HF
- 52. DIAGNOSIS OF MYOCARDITIS New York Heart Association (NYHA) History of infection confirmed clinically and biochemically or
- 53. MANAGEMENT OF MYOCARDITIS 1 Etiotropic treatment Antibacterial, antiviral, antiparasitic drugs 2 Pathogenic treatment Non-steroidal anti-inflammatory drugs
- 54. HF is a clinical syndrome characterized by typical symptoms (e.g. breathlessness, ankle swelling and fatigue) that
- 55. A state in which the heart cannot provide sufficient cardiac output to satisfy the metabolic needs
- 56. HF – is an imprecise term used to describe the pathological state that develops when the
- 57. CLASSIFICATION Heart failure can be classified in several ways 1 - Acute and chronic HF 2
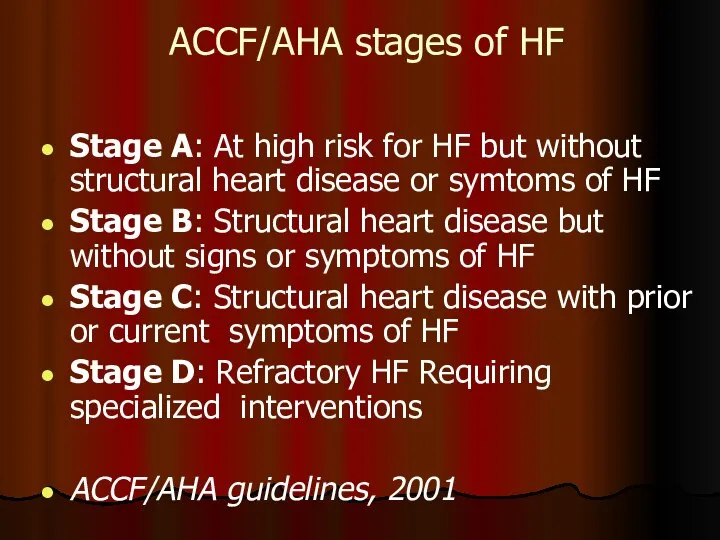
- 58. ACCF/AHA stages of HF Stage A: At high risk for HF but without structural heart disease
- 59. ESC Guidelines for diagnostic and treatment of acute and chronic HF (2016) Definition of heart failure
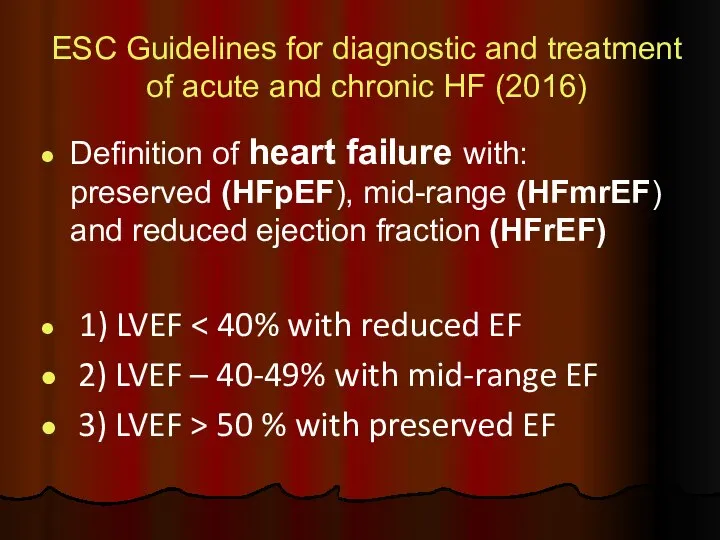
- 60. NEW YORK НЕАRT ASSOCIATION (NYHA) FUNCTIONAL CLASSIFICATION OF CHF I class. Patients with cardiac disease but
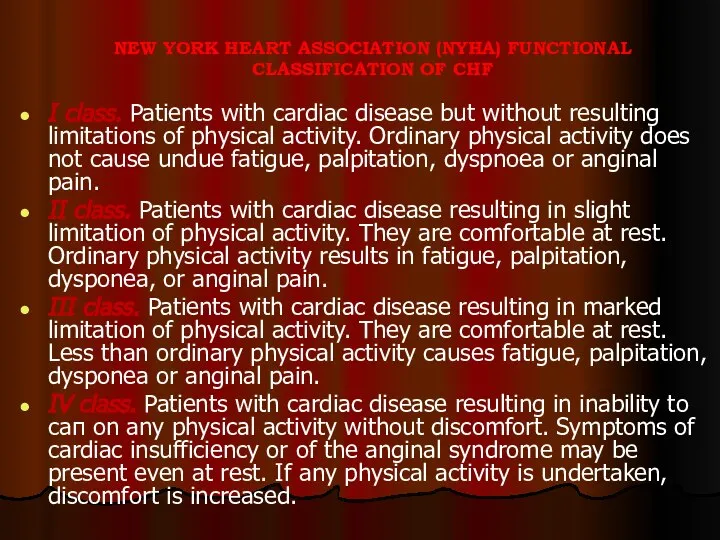
- 61. MANAGEMENT OF HEART FAILURE (HF) The main purposes: To reduce mortality !!! To relieve HF symptoms
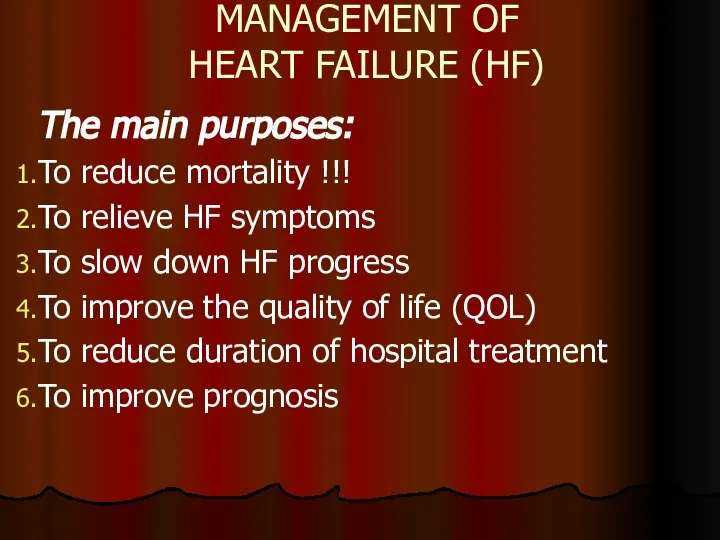
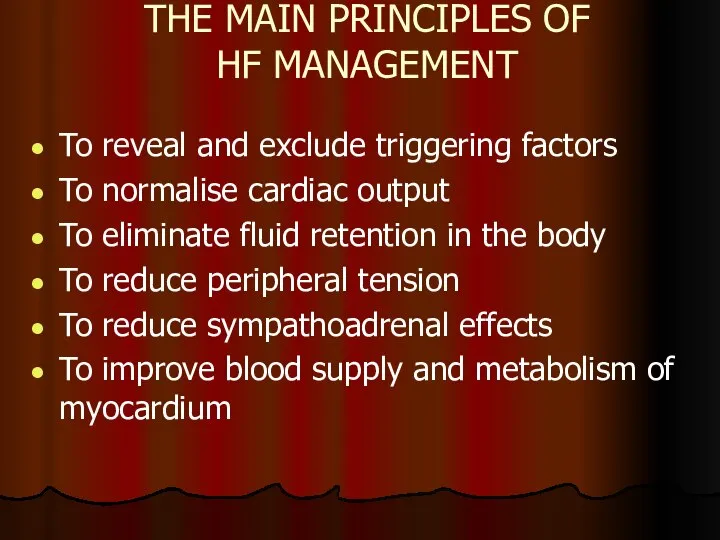
- 62. THE MAIN PRINCIPLES OF HF MANAGEMENT To reveal and exclude triggering factors To normalise cardiac output
- 63. METHODS OF HF MANAGEMENT Non-medical (changing lifestyle) Pharmacotherapy (ACE inhibitors or ARBs, beta-blockers, aldosterone antagonists, diuretics,
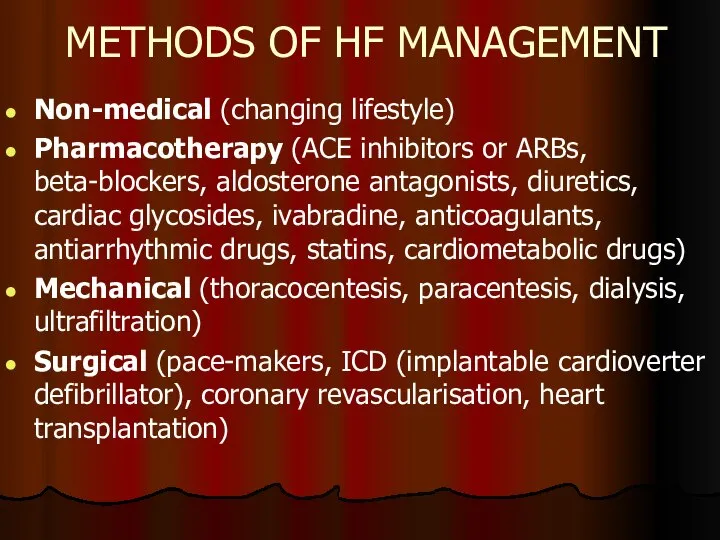
- 64. Pharmacotherapy for HF 1 DRUGS PROVED TO BE ABLE TO REDUCE MORBIDITY AND MORTALITY RATES IN
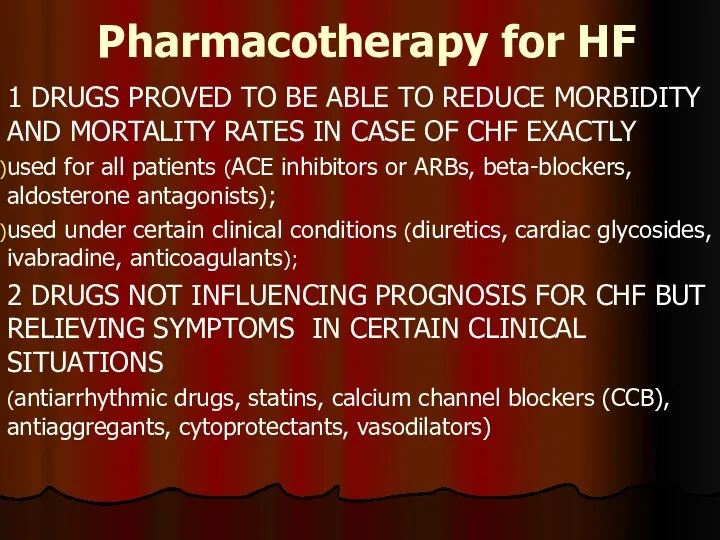
- 65. ACE inhibitors recommended by Russian Cardiology Society Enalapril 2,5×2 - 20×2 Captopril 6,25×3 - 50×3 Fosinopril
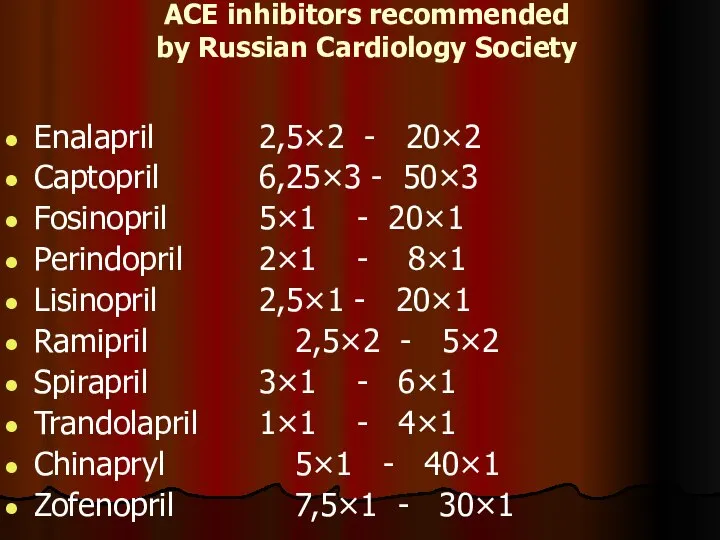
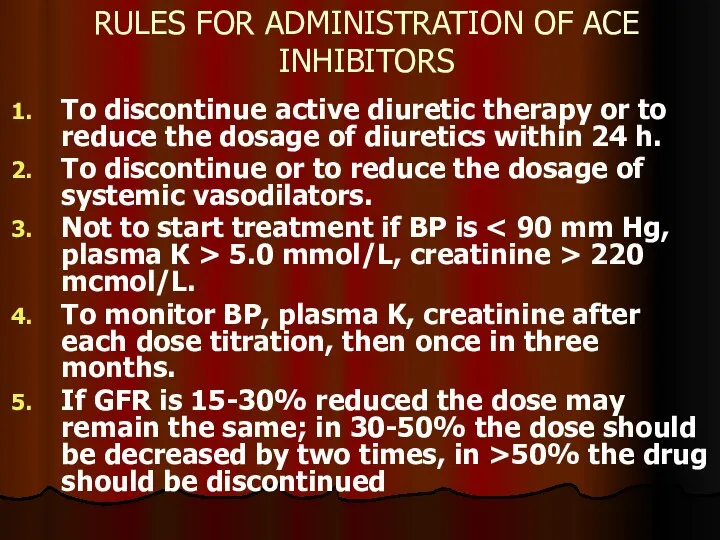
- 66. RULES FOR ADMINISTRATION OF ACE INHIBITORS To discontinue active diuretic therapy or to reduce the dosage
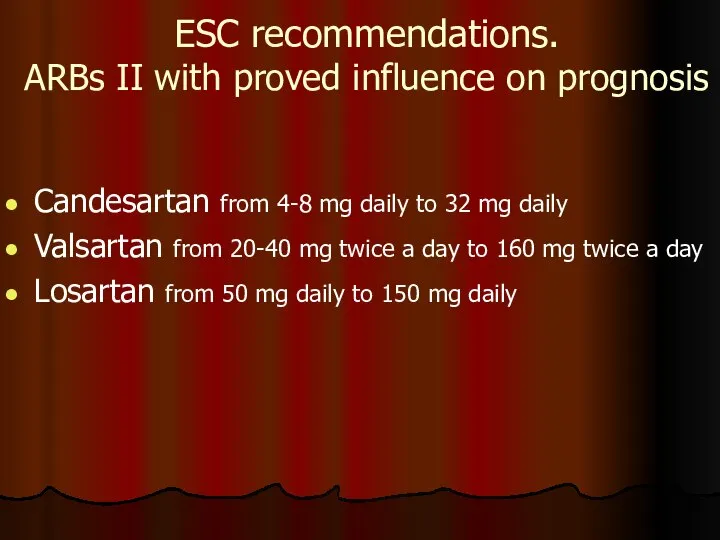
- 67. ESC recommendations. ARBs II with proved influence on prognosis Candesartan from 4-8 mg daily to 32
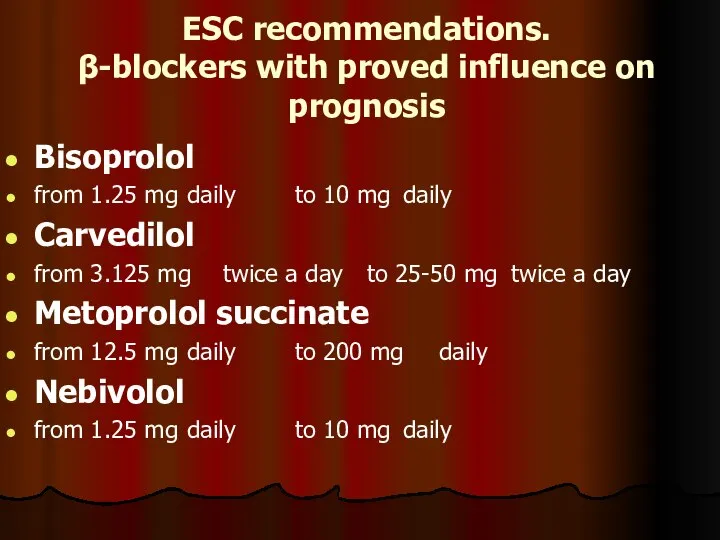
- 68. ESC recommendations. β-blockers with proved influence on prognosis Bisoprolol from 1.25 mg daily to 10 mg
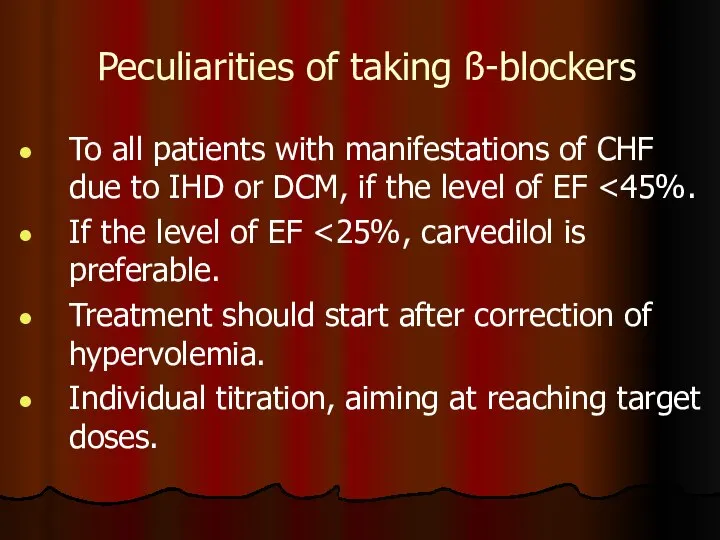
- 69. Peculiarities of taking ß-blockers To all patients with manifestations of CHF due to IHD or DCM,
- 70. ESC recommendations. Aldosterone antagonists Eplerenone from 25 mg daily to 50 mg daily Spironolactone from 25
- 71. ESC recommendations. Aldosterone antagonists Contraindicated: K level >5.0 mmol/L, creatinine >220 mcmol/L, While taking other sparing
- 72. IVABRADIN, a standard medication for CHF management Reviewing European recommendations on HF (2012): Ivabradin should be
- 73. Indications for administration of diuretics: To eliminate clinical symptoms of fluid retention. They contribute to better
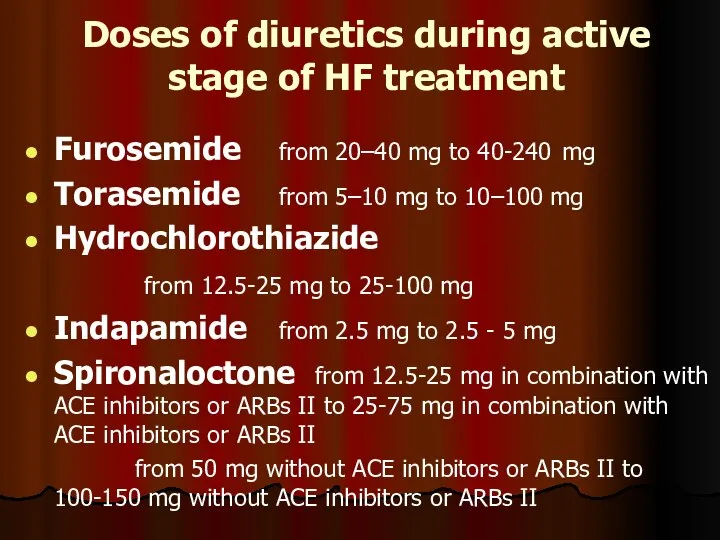
- 74. Doses of diuretics during active stage of HF treatment Furosemide from 20–40 mg to 40-240 mg
- 76. Скачать презентацию
 Риккетсиозы. Морфология и биологические свойства. Клиническая картина. Диагностика. Профилактика
Риккетсиозы. Морфология и биологические свойства. Клиническая картина. Диагностика. Профилактика Остеобластокластома
Остеобластокластома Нарушения метаболизма холестерина. Лекция 2
Нарушения метаболизма холестерина. Лекция 2 Психосоматические растройтсва
Психосоматические растройтсва Ведение критических пациентов – 20 правил Кирби
Ведение критических пациентов – 20 правил Кирби Исследование пользы дневного сна после нормального ночного сна
Исследование пользы дневного сна после нормального ночного сна Асцит в результате надпеченочного блока
Асцит в результате надпеченочного блока Развитие медицины в новое время. Акушерство, гинекология в XVII - начало XX века
Развитие медицины в новое время. Акушерство, гинекология в XVII - начало XX века Запрещенный список 2018 года
Запрещенный список 2018 года Семейство Bacillaceae
Семейство Bacillaceae Дивертикулы пищевода
Дивертикулы пищевода Аборт как социально-медицинская проблема
Аборт как социально-медицинская проблема Уақытша сауыттар
Уақытша сауыттар Ультразвукова терапія
Ультразвукова терапія Способы остановки кровотечений
Способы остановки кровотечений Ситуационные задачи: ургентные
Ситуационные задачи: ургентные ЛЕКЦИЯ №1 диагностика
ЛЕКЦИЯ №1 диагностика Сосудистые расстройства и беременность
Сосудистые расстройства и беременность Treatment of toxoplasmosis in pregnancy
Treatment of toxoplasmosis in pregnancy Витамины, их полезные свойства
Витамины, их полезные свойства Эндокринная система
Эндокринная система Сап. Збудник
Сап. Збудник Пищеварение в желудке, кишечнике
Пищеварение в желудке, кишечнике Виды ущемления грыж
Виды ущемления грыж Стоп ВИЧ/СПИД. О проведении на территории Смоленской области мероприятий в рамках восьмой Всероссийской акции
Стоп ВИЧ/СПИД. О проведении на территории Смоленской области мероприятий в рамках восьмой Всероссийской акции Железодефицитная анемия при беременности
Железодефицитная анемия при беременности Флегмона. Классификация
Флегмона. Классификация Судебно-медицинское учение о повреждениях
Судебно-медицинское учение о повреждениях