Содержание
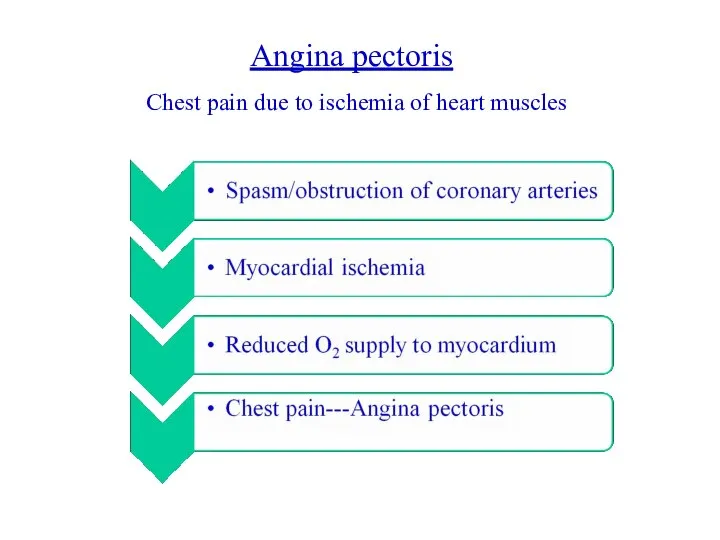
- 2. Angina pectoris Chest pain due to ischemia of heart muscles
- 3. Weak relationship between severity of pain and degree of oxygen supply- there can be severe pain
- 4. Stable angina: Also called “Effort Angina” Discomfort is precipitated by activity Minimal or no symptoms at
- 5. Unstable angina: Also called “Crescendo angina” Acute coronary syndrome in which angina worsens Occurs at rest
- 6. Microvascular angina: Also called Syndrome X Cause unknown Probably due to poor functioning of the small
- 7. Prinzmetal’s angina Prinzmetal’s angina is a variant form of angina with normal coronary vessels or minimal
- 8. Symptoms What is the cause of ischemia ? either ↑ oxygen demand or ↓ oxygen supply
- 9. Treatment: Aims: Relief of symptoms Slowing progression of the disease Reduction of future events like myocardial
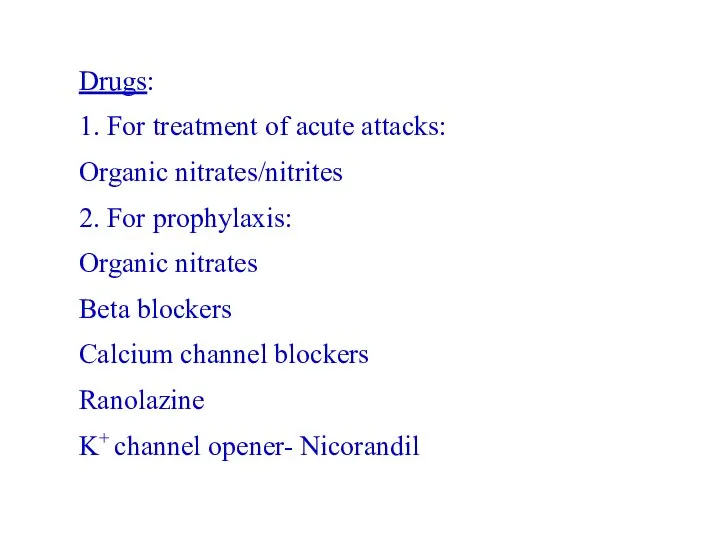
- 10. Drugs: 1. For treatment of acute attacks: Organic nitrates/nitrites 2. For prophylaxis: Organic nitrates Beta blockers
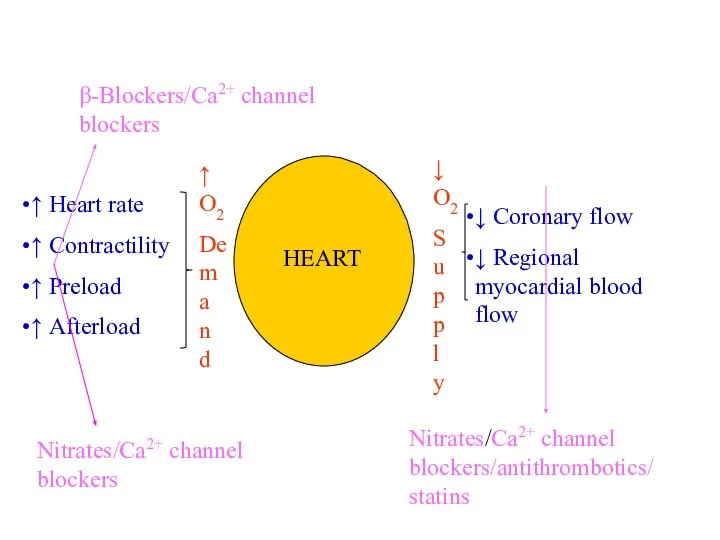
- 11. ↑ Heart rate ↑ Contractility ↑ Preload ↑ Afterload ↓ Coronary flow ↓ Regional myocardial blood
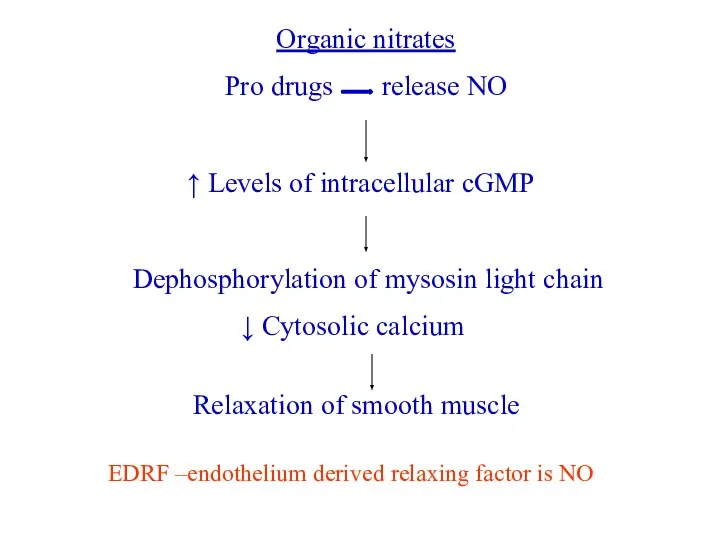
- 12. Organic nitrates Pro drugs release NO ↑ Levels of intracellular cGMP Dephosphorylation of mysosin light chain
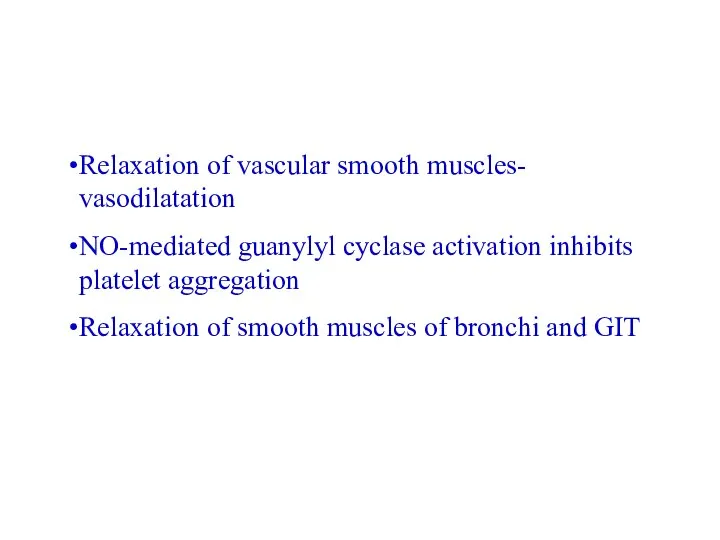
- 13. Relaxation of vascular smooth muscles- vasodilatation NO-mediated guanylyl cyclase activation inhibits platelet aggregation Relaxation of smooth
- 14. L-Arginine NO NO Synthases Neurotransmission Vasomotor effects Immunomodulation Endogenous NO pathway nNOS eNOS iNOS
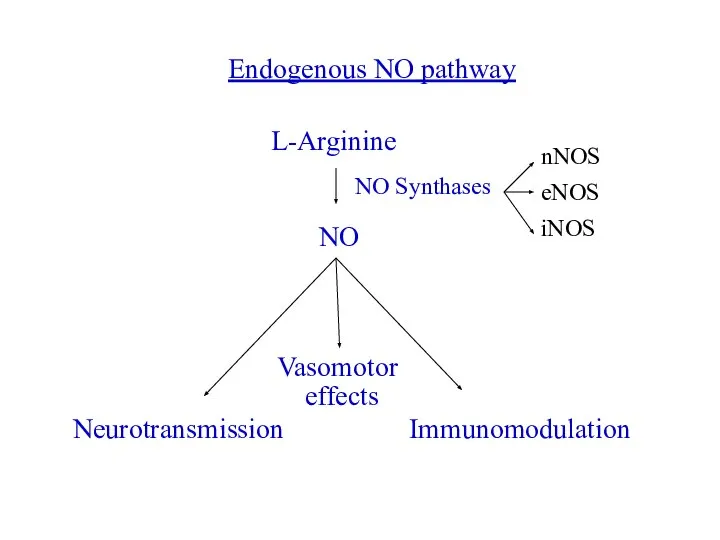
- 15. Three different forms of NO synthase are found in humans: 1. Neuronal NOS (nNOS or NOS1)-
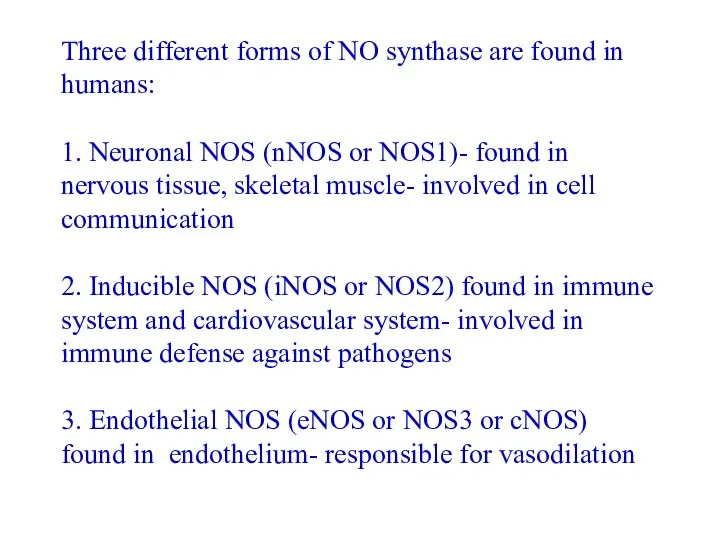
- 16. CVS Effects: Vasodilatation- low concentrations preferably dilate veins Venodilatation→ decreases venous return to heart Decreased chamber
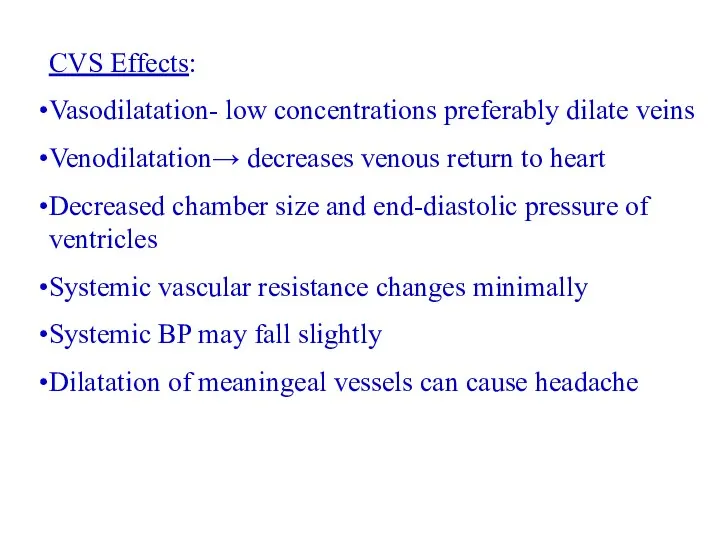
- 17. HR-unchanged or may increase slightly (reflex tachycardia) Cardiac output slightly reduced Even low doses can cause
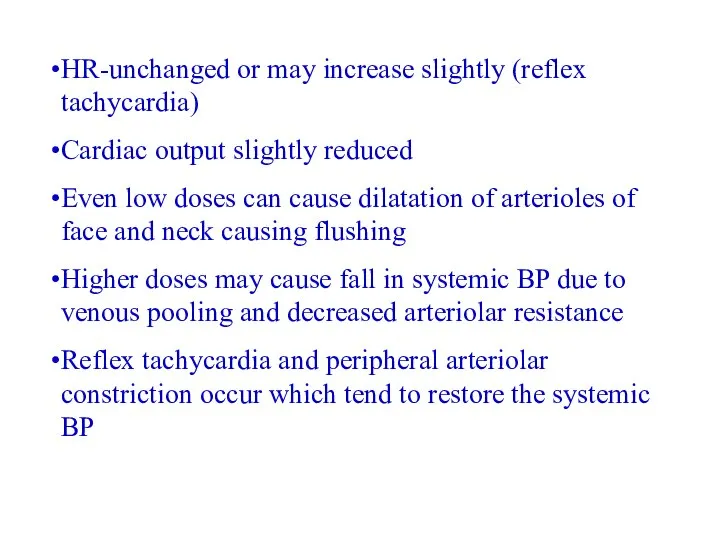
- 18. Coronary blood flow may initially increase transiently Subsequently, due to decreased BP, may decrease Nitrates have
- 19. Reduction in myocardial O2 consumption is caused by: Peripheral pooling of blood- reduced preload Arteriolar dilatation-
- 20. How myocardial O2 consumption can be determined? Double product: HR × systolic BP- approximate measure of
- 21. Pharmacokinetics: Orally ineffective because of high first pass metabolism Administered sublingually to avoid first pass matabolism
- 22. ADRs: Headache- may be severe May disappear after continued use or, Decrease dose Transient episodes of
- 23. Administration of nitrates: Sublingual Oral: For prophylaxis, require high doses due to first pass metabolism, isosorbide
- 24. Transdermal nitrogycerine discs impregnated with nitroglycerine polymer- gradual absorption and 24 h plasma nitrate concentration Onset
- 25. Ca2+ antagonists: ↓ Ca2+ influx Negative iono and chronotropic effects Peripheral vasodilatation Used in variant angina
- 26. β-Blockers: Effective in reducing severity and frequency of exertional angina May worsen vasospastic angina- contraindicated Reduce
- 27. Ranolazine: Reserve agent for treatment of chronic, resistant angina Inhibits cardiac late Na+ current Effects the
- 29. Скачать презентацию
 Moderni ošetřovatelská praxe
Moderni ošetřovatelská praxe Школа здоровья для беременных. Занятие 2
Школа здоровья для беременных. Занятие 2 Иммунокоррекция больного при лечении туберкулёза
Иммунокоррекция больного при лечении туберкулёза КФ гипотензивных ЛС. Лекция № 2
КФ гипотензивных ЛС. Лекция № 2 Передний Инфаркт Миокарда
Передний Инфаркт Миокарда НИИ УРОНЕФРОЛОГИИ и РЕПРОДУКТИВНОГО ЗДОРОВЬЯ ЧЕЛОВЕКА. - презентация_
НИИ УРОНЕФРОЛОГИИ и РЕПРОДУКТИВНОГО ЗДОРОВЬЯ ЧЕЛОВЕКА. - презентация_ III А – топтың элементтері. Бор және алюминий
III А – топтың элементтері. Бор және алюминий doc480201671_646488054_botulizm
doc480201671_646488054_botulizm Общая характеристика антигенов
Общая характеристика антигенов Эписклеральное секторальное пломбирование
Эписклеральное секторальное пломбирование Рак пищевода
Рак пищевода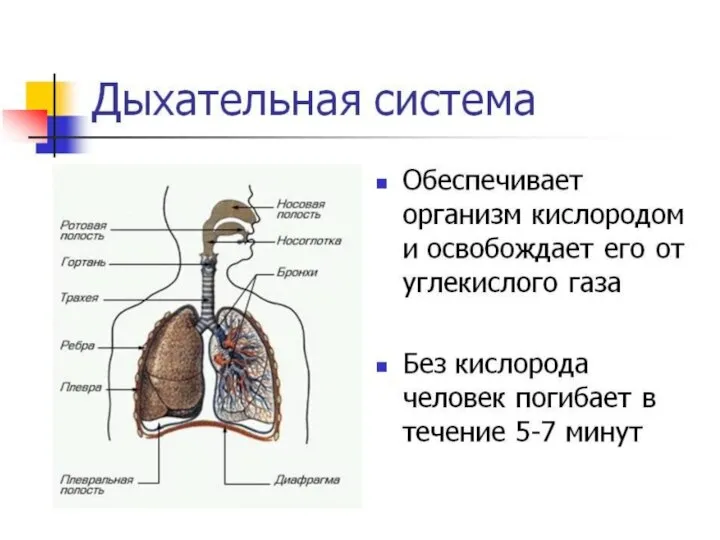 Дыхательная система
Дыхательная система 1328615
1328615 ABD politik sagli turizm
ABD politik sagli turizm Наш путь к протоколу лечения сепсиса
Наш путь к протоколу лечения сепсиса Пренатальная диагностика ВПР и тактика ведения беременности
Пренатальная диагностика ВПР и тактика ведения беременности Эмбриогенез нервной системы. Основные этапы
Эмбриогенез нервной системы. Основные этапы Эписклеральное радиальное пломбирование
Эписклеральное радиальное пломбирование Прионы и прионные заболевания
Прионы и прионные заболевания Ортопедическое лечение пациентки с частичным отсутствием зубов
Ортопедическое лечение пациентки с частичным отсутствием зубов Раны и раневой процесс
Раны и раневой процесс Актуальные вопросы критической ишемии нижних конечностей
Актуальные вопросы критической ишемии нижних конечностей Оспа. Открытие способа вакцинации
Оспа. Открытие способа вакцинации Анатомия центральной нервной системы
Анатомия центральной нервной системы Medical Level Up. Медицинский форум практических навыков в Крыму
Medical Level Up. Медицинский форум практических навыков в Крыму Врожденные пороки сердца. Острая ревматическая лихорадка
Врожденные пороки сердца. Острая ревматическая лихорадка Жабыспалы аурулар
Жабыспалы аурулар Наномедицина: от идеи до воплощения
Наномедицина: от идеи до воплощения