Содержание
- 2. ENDOCRINE PANCREAS
- 3. ENDOCRINE PANCREAS The pancreas consists of two functionally distinct components: The exocrine pancreas, which secretes digestive
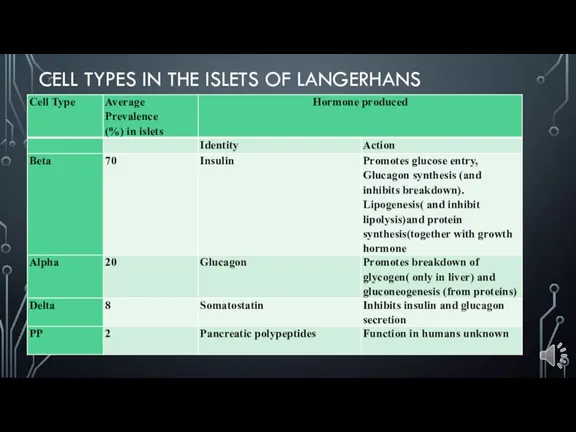
- 4. CELL TYPES IN THE ISLETS OF LANGERHANS
- 5. DIABETES MELLITUS Abnormal metabolic state characterised by glucose intolerance due to inadequate insulin action Type 1
- 6. Diagnosis is based on the clinical demonstration of glucose intolerance Insulin is unique, in that it
- 7. PATHOGENESIS The actions of insulin are all anabolic, that is, they promote the laying down of
- 8. In hyperglycaemia the renal threshold for glucose conservation is exceeded, so that there is osmotic diuresis
- 9. The combined result of severe ketosis, acidosis, hyperglycaemia, hyperosmolarity and electrolyte disturbance is to impair cerebral
- 10. CLASSIFICATION Type 1 (juvenile-onset, insulin-dependent diabetes) Typically presents in childhood. The patient usually shows the catabolic
- 11. Postmortem examination of the pancreas in patients who had recently developed type 1 diabetes but died
- 12. Autoimmune destruction. The majority of patients have circulatory antibodies to several different types of islet cell.
- 13. Type 2 (maturity-onset, non-insulin-dependent diabetes) is more common than type 1 and usually presents in middle
- 14. Type 2 (maturity-onset, non-insulin-dependent diabetes) Genetic factors clearly play an important part in the aetiology of
- 15. Secondary diabetes Hypersecretion of any of the hormones that tend to exert a hyperglycaemic effect may
- 16. COMPLICATIONS The commonest complications are seen in blood vessels. Atheroma, often ultimately severe and extensive, develops
- 17. TUMOURS Less common than pancreatic adenocarcinoma Present with endocrine effects and may be malignant Insulinoma: causes
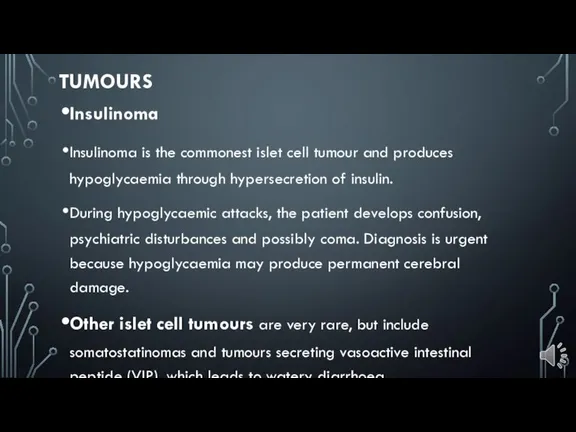
- 18. Insulinoma Insulinoma is the commonest islet cell tumour and produces hypoglycaemia through hypersecretion of insulin. During
- 19. Gastrinomas : Although gastrin is usually produced in the G-cells of the stomach, tumours of the
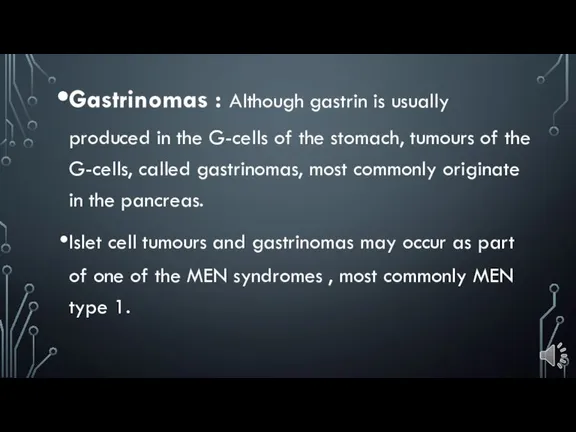
- 21. Скачать презентацию
 Жүктілікті анықтау
Жүктілікті анықтау Правильное питание в период беременности
Правильное питание в период беременности Интересные факты о здоровье
Интересные факты о здоровье Привычки стройных людей
Привычки стройных людей Антибактериальная активность лекарственных растений в отношении антибиотикочувствительных и антибиотикоустойчивых бактерий
Антибактериальная активность лекарственных растений в отношении антибиотикочувствительных и антибиотикоустойчивых бактерий Наука, искусство и больные нервы. Искусство врачевания
Наука, искусство и больные нервы. Искусство врачевания Тимпаносклероз (ТСК)
Тимпаносклероз (ТСК) Экспресс-тестирование групп крови человека
Экспресс-тестирование групп крови человека Правила внутреннего трудового распорядка в аптеке
Правила внутреннего трудового распорядка в аптеке Уход за больными в связи с выполнением операции
Уход за больными в связи с выполнением операции Медицина (клиника академика Ройтберга)
Медицина (клиника академика Ройтберга) Медицинская лабораторная диагностика
Медицинская лабораторная диагностика Болезнь Гоше
Болезнь Гоше Сестринский уход при дисфункции кишечника. Лекция №9
Сестринский уход при дисфункции кишечника. Лекция №9 От незнания к донорству
От незнания к донорству Травма живота
Травма живота Модели сестринского ухода
Модели сестринского ухода Фитотерапия и физиотерапия. Аутизм в детском возрасте. Фитотерапия в педиатрии
Фитотерапия и физиотерапия. Аутизм в детском возрасте. Фитотерапия в педиатрии Новые возможности ранней диагностики острого инфаркта миокарда
Новые возможности ранней диагностики острого инфаркта миокарда Мониторинг здоровья обучающихся как средство развития образовательной среды школы
Мониторинг здоровья обучающихся как средство развития образовательной среды школы Клиника внутренних болезней
Клиника внутренних болезней Рак предстательной железы
Рак предстательной железы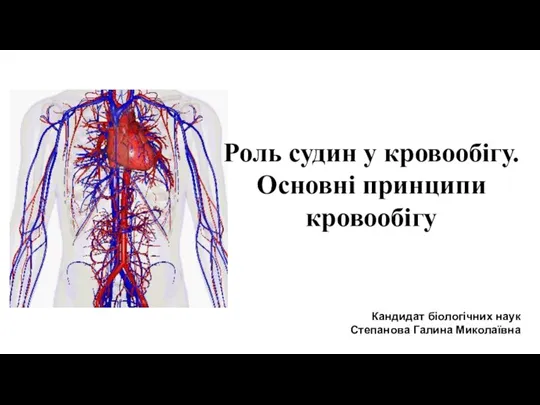 Роль судин у кровообігу. Основні принципи кровообігу
Роль судин у кровообігу. Основні принципи кровообігу Нарушения мозгового кровообращения
Нарушения мозгового кровообращения Амиодарон. Фармакологическая группа вещества Амиодарон
Амиодарон. Фармакологическая группа вещества Амиодарон Хр.болезнь почек 5 курс ДВ (1)
Хр.болезнь почек 5 курс ДВ (1) Методы исследования клеточных факторов неспецифической резистентности организма
Методы исследования клеточных факторов неспецифической резистентности организма Возбудимость и проводимость ЭКГ
Возбудимость и проводимость ЭКГ