Содержание
- 2. Introduction Preoperative History and Physical IV’s and Premedication Commonly Used Medications Room Setup and Monitors Induction
- 3. Definitions Anesthesia - From the Greek meaning lack of sensation; particularly during surgical intervention.
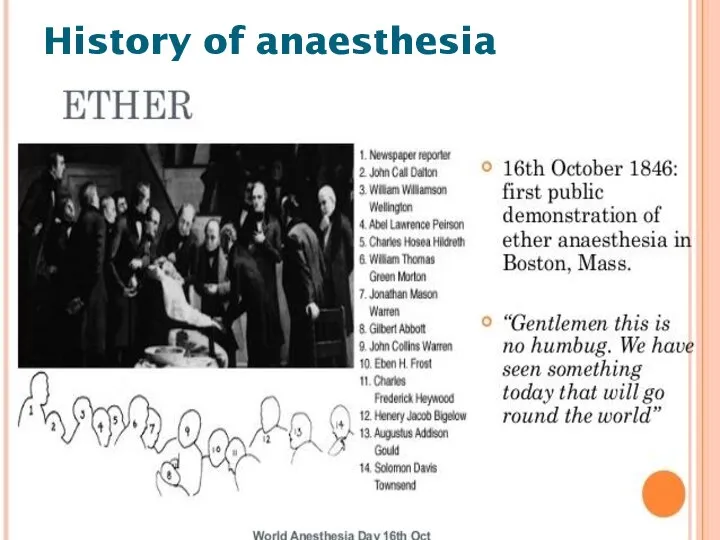
- 4. On October 16, 1846, in Boston, William T.G. Morton - the first publicized demonstration of general
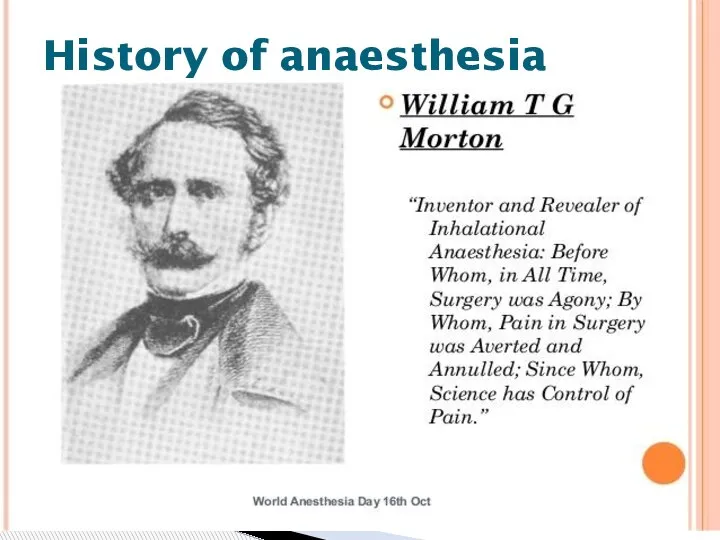
- 5. History of anaesthesia
- 6. History of anaesthesia
- 7. General anesthesia– a condition characterized by temporary shutting down consciousness pain sensitivity reflexes relaxation of skeletal
- 10. Reversible, drug-induced condition Amnesia & unconsciousness Analgesia Muscle relaxation Attenuation of autonomic responses to noxious stimulation
- 11. Anaesthesiology is the science of managing the life functions of the patients organism in time of
- 12. General Anesthesia Preoperative evaluation Intraoperative management Postoperative management
- 13. Physical Examination Physical exams of all systems. Airway assessment to determine the likelihood of difficult intubation
- 14. Unlike the standard internal medicine H&P, ours is much more focused, with specific attention being paid
- 15. • Elective: operation at a time to suit both patient and surgeon; for example hip replacement,
- 16. • Urgent: operation as soon as possible after resuscitation and within 24 h; for example intestinal
- 17. Of particular interest in the history portion of the evaluation are: Coronary Artery Disease Hypertension Asthma
- 18. Coronary Artery Disease What is the patient’s exercise tolerance? How well will his or her heart
- 19. Coronary Artery Disease What is the patient’s exercise tolerance? How well will his or her heart
- 20. Hypertension How well controlled is it? Intraoperative blood pressure management is affected by preoperative blood pressure
- 21. Asthma How well controlled is it? What triggers it? Many of the stressors of surgery as
- 22. Kidney or Liver disease Different anesthetic drugs have different modes of clearance and organ function can
- 23. Reflux Disease Present or not? Anesthetized and relaxed patients are prone to regurgitation and aspiration, particularly
- 24. Smoking Currently smoking? Airway and secretion management can become more difficult in smokers. Preoperative History and
- 25. Alcohol Consumption or Drug Abuse? Drinkers have an increased tolerance to many sedative drugs (conversely they
- 26. Diabetes Well controlled? The stress response to surgery and anesthesia can markedly increase blood glucose concentrations,
- 27. Medications Many medications interact with anesthetic agents, and some should be taken on the morning of
- 28. Allergies We routinely give narcotics and antibiotics perioperatively, and it is important to know the types
- 29. Family History There is a rare, but serious disorder known as malignant hyperthermia that affects susceptible
- 30. Anesthesia history Has the patient ever had anesthesia and surgery before? Did anything go wrong? Preoperative
- 31. Last Meal Whether the patient has an empty stomach or not impacts the choice of induction
- 32. All patients must have an assessment made of their airway, the aim being to try and
- 33. Finding any of these suggests that intubation may be more difficult. • limitation of mouth opening;
- 34. Also, any loose or missing teeth should be noted, as should cervical range of motion, mouth
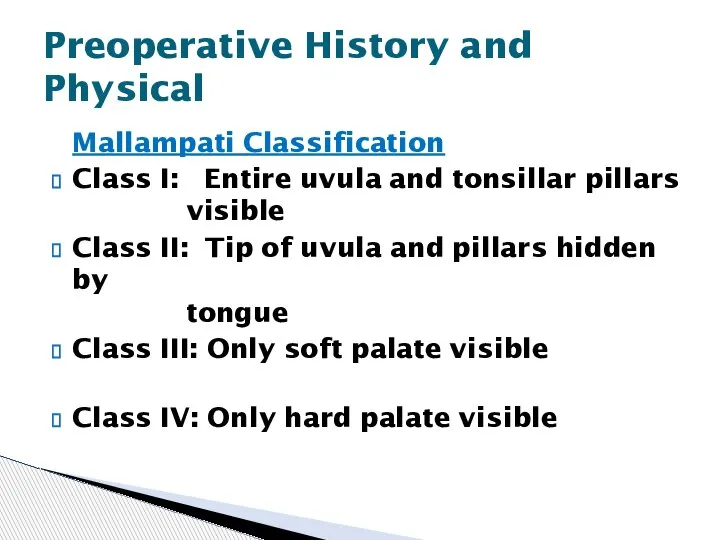
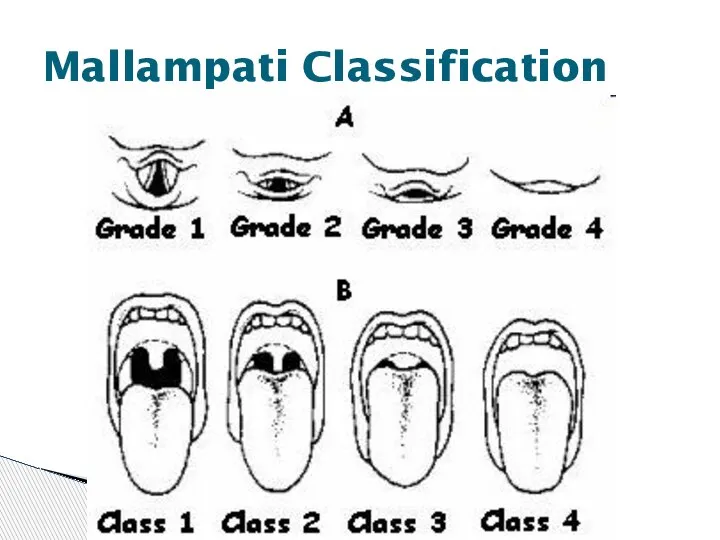
- 35. Mallampati Classification Class I: Entire uvula and tonsillar pillars visible Class II: Tip of uvula and
- 36. Mallampati Classification
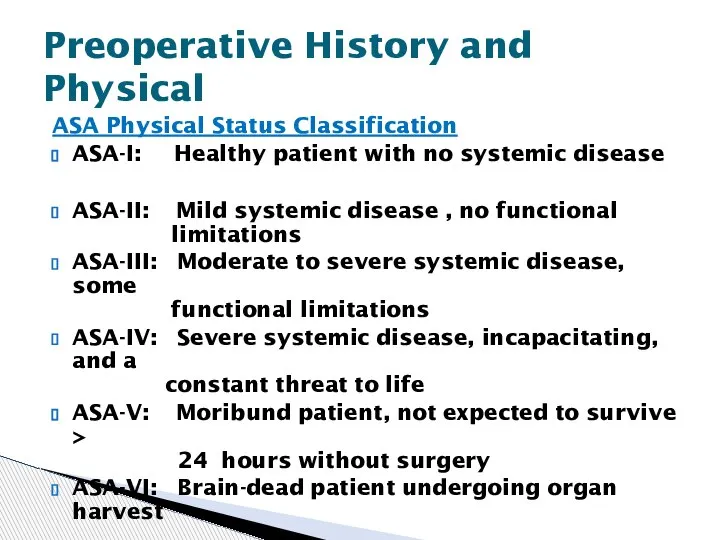
- 37. Finally, a physical status classification is assigned, based on the criteria of the American Society of
- 38. ASA Physical Status Classification ASA-I: Healthy patient with no systemic disease ASA-II: Mild systemic disease ,
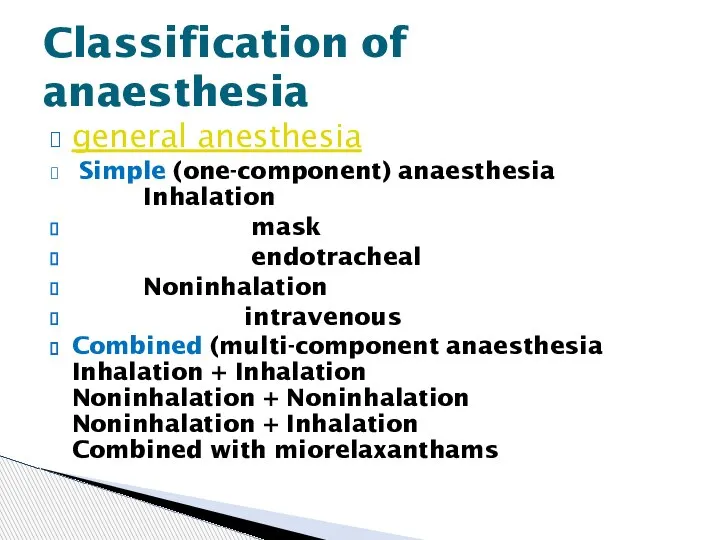
- 39. general anesthesia Simple (one-component) anaesthesia Inhalation mask endotracheal Noninhalation intravenous Combined (multi-component anaesthesia Inhalation + Inhalation
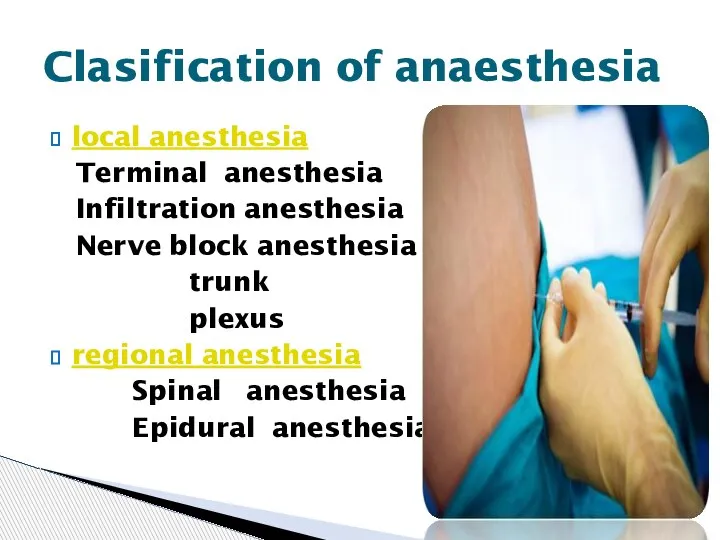
- 40. local anesthesia Terminal anesthesia Infiltration anesthesia Nerve block anesthesia trunk plexus regional anesthesia Spinal anesthesia Epidural
- 42. Every patient (with the exception of some children that can have their IV’s inserted following inhalation
- 43. Premedication refers to the administration of any drugs in the period before induction of anaesthesia. a
- 44. Many patients are understandably nervous preoperatively, and we often premedicate them, usually with a rapid acting
- 45. Before bringing the patient to the room, the anesthesia machine, ventilator, monitors, and cart must be
- 47. The monitors that we use on most patients include the pulse oximeter, blood pressure monitor, and
- 48. The anesthesia cart is set up to allow easy access to intubation equipment including endotracheal tubes,
- 49. Other preparations that can be done before the case focus on patient positioning and comfort, since
- 50. Four Phases Induction Maintenance Emergence Recovery General Anesthesia
- 51. Four Phases Induction Maintenance Emergence Recovery
- 52. You now have your sedated patient in the room with his IV and he’s comfortably lying
- 53. Stage I – Amnesia Stage II – Excitement Stage III – Surgical Intervention (4 planes) Stage
- 54. Stage I (stage of analgesia or disorientation): from beginning of induction of general anesthesia to loss
- 55. Stage III (stage of surgical anesthesia): from onset of automatic respiration to respiratory paralysis. It is
- 56. Plane II - from cessation of eyeball movements to beginning of paralysis of intercostal muscles. Laryngeal
- 57. Plane III - from beginning to completion of intercostal muscle paralysis. Diaphragmatic respiration persists but there
- 58. Plane IV - from complete intercostal paral ysis to diaphragmatic paralysis (apnea). Stage IV: from stoppage
- 59. The first part of induction of anesthesia should be preoxygenation with 100% oxygen delivered via a
- 60. Patients frequently become apneic after induction and you may have to assist ventilation. The most common
- 62. • Propofol Typical adult induction dose 1.5–2.5 mg/kg Popular and widely used drug associated with rapid
- 64. • Thiopental Sodium Typical adult induction dose 3–5 mg/kg (2.5% solution) The ‘gold-standard’ against which all
- 66. Ketamine Typical adult induction dose 0.5–2 mg/kg Useful for sedation with profound analgesia. Increases pulse rate
- 68. Ketamine
- 72. Assuming that you are now able to mask ventilate the patient, the next step is usually
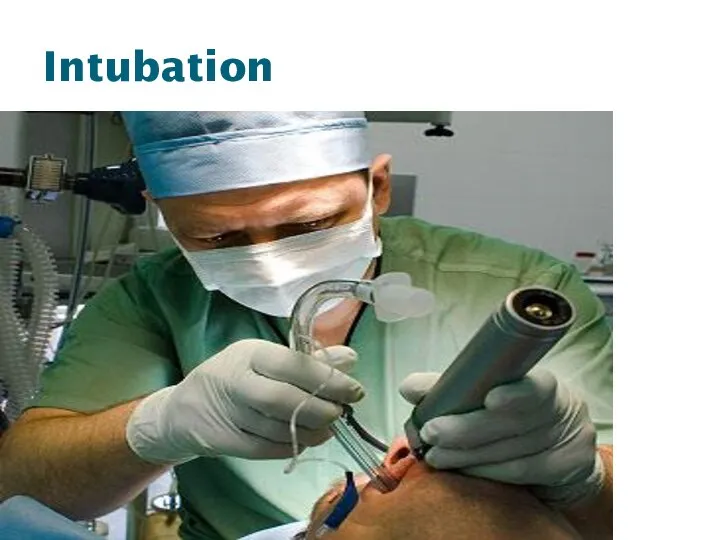
- 73. . Hold the laryngoscope in your left hand (whether you’re right or left handed) then open
- 74. Intubation
- 75. Careful and continues vigilance of vital sings and depth of anesthesia is the integral part of
- 76. It is important to keep track of the blood loss during the case and should be
- 77. It is also vital to pay attention to the case itself, since blood loss can occur
- 78. One can also prepare for potential post-operative problems during the case, by treating the patient intraoperatively
- 81. Volatile Anesthetics Halothane Pro: Cheap, Nonirritating so can be used for inhalation induction Con: Long time
- 83. Volatile Anesthetics Sevoflurane Pro: Nonirritating so can be used for inhalation induction, Extremely rapid onset/offset Con:
- 85. Volatile Anesthetics Isoflurane Pro: Cheap, Excellent renal, hepatic, coronary, and cerebral blood flow preservation Con: Long
- 86. Volatile Anesthetics Desflurane Pro: Extremely rapid onset/offset Con: Expensive, Stimulates catecholamine release, Possibly increases postoperative nausea
- 88. Nitrous Oxide Pro: Decreases volatile anesthetic requirement, Dirt cheap, Less myocardial depression than volatile agents Con:
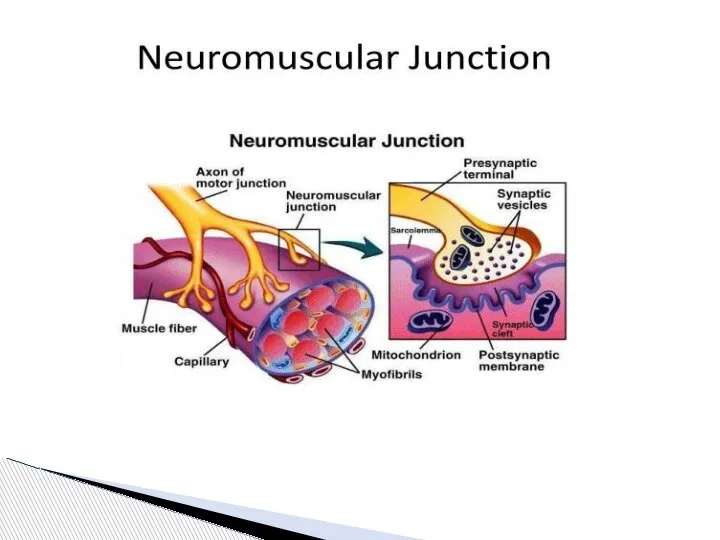
- 91. Muscle Relaxants Depolarizing Succinylcholine inhibits the postjunctional receptor and passively diffuses off the membrane, while circulating
- 92. Nondepolarizing Many different kinds, all ending in “onium” or “urium”. Each has different site of metabolism,
- 93. EMERGENCE FROM GENERAL ANESTHESIA 1. Reversal of muscle relaxation. 2. Turning off the inhalation agents and
- 94. First, the patient’s neuromuscular blockade must be re-assessed, and if necessary reversed and then rechecked with
- 95. . Once the patient is reversed, awake, suctioned, and extubated, care must be taken in transferring
- 96. The anesthesiologist’s job isn’t over once the patient leaves the operating room. Concerns that are directly
- 97. Other concerns include continuing awareness of the patient’s airway and level of consciousness, as well as
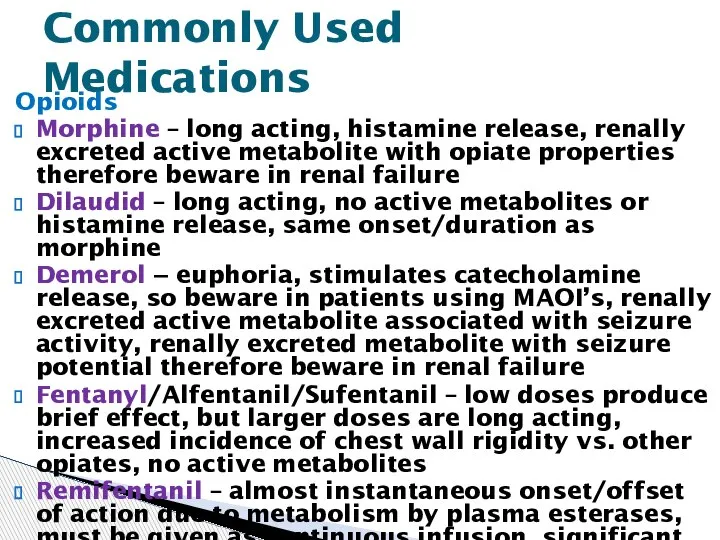
- 98. Opioids Morphine – long acting, histamine release, renally excreted active metabolite with opiate properties therefore beware
- 100. Скачать презентацию



 Записки судмедэксперта
Записки судмедэксперта Патология ЦНС у новорожденных
Патология ЦНС у новорожденных Гельминтозы. Пути заражения и меры профилактики
Гельминтозы. Пути заражения и меры профилактики I этап студенческой олимпиады по хирургии. Абдоминальная хирургия
I этап студенческой олимпиады по хирургии. Абдоминальная хирургия Разработка фито мази на основе лизоцима для комплексного лечения заболеваний пародонта in vitro
Разработка фито мази на основе лизоцима для комплексного лечения заболеваний пародонта in vitro Гласперленген залалсыздандыру
Гласперленген залалсыздандыру Первая медицинская помощь при травмах головы
Первая медицинская помощь при травмах головы Антибиотики (часть 2). Сульфаниламиды
Антибиотики (часть 2). Сульфаниламиды Патогенные коринебактерии
Патогенные коринебактерии Мышечная система у детей. (Лекция 6)
Мышечная система у детей. (Лекция 6) Правила здорового питания
Правила здорового питания Геогельминтозы. Эпидемиологическая характеристика геогельминтозов
Геогельминтозы. Эпидемиологическая характеристика геогельминтозов Сахарный диабет у детей
Сахарный диабет у детей Посттравматический остеомиелит
Посттравматический остеомиелит Фолатный цикл
Фолатный цикл Глаукомы. Клиника, диагностика, лечение, профилактика глауком
Глаукомы. Клиника, диагностика, лечение, профилактика глауком Healthy food. Rainbow Diet
Healthy food. Rainbow Diet Биоинформационное исследование молекулярно–генетических факторов ассоциации шизофрении и болезни Альцгеймера
Биоинформационное исследование молекулярно–генетических факторов ассоциации шизофрении и болезни Альцгеймера Реактивность организма
Реактивность организма Неспецифический язвенный колит. Разбор клинического случая
Неспецифический язвенный колит. Разбор клинического случая Lymphadenopathy. Лимфадениты
Lymphadenopathy. Лимфадениты Сердечно - легочная реанимация вне МО
Сердечно - легочная реанимация вне МО Қасаға буынының созылуы мен жыртылуы
Қасаға буынының созылуы мен жыртылуы Интернист. Digest интерниста
Интернист. Digest интерниста Лицевая дуга. Применение в работе врача-стоматолога
Лицевая дуга. Применение в работе врача-стоматолога Parameedik
Parameedik Инфекционные заболевания
Инфекционные заболевания Аналық жыныс жасушасы
Аналық жыныс жасушасы