Содержание
- 2. Medical Error is preventable adverse effect of medical care, whether or not it is evident or
- 3. Medical Errors Medical Errors represents a serious public health problem and pose a threat to patient
- 4. 2 Types of Human Errors Active Error- occur at the point of contact between a human
- 5. 2 Types of Human Errors Latent Errors- refer to less apparent failures of organization or design
- 6. How common are Medical Errors?
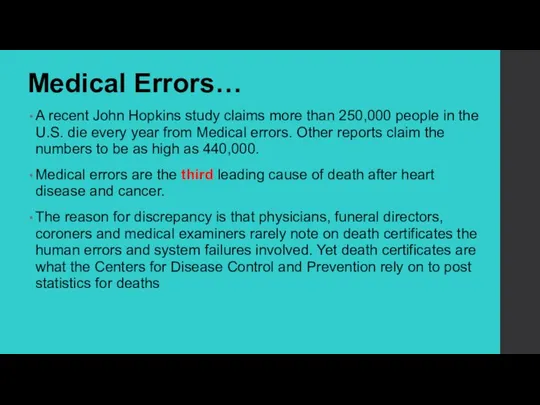
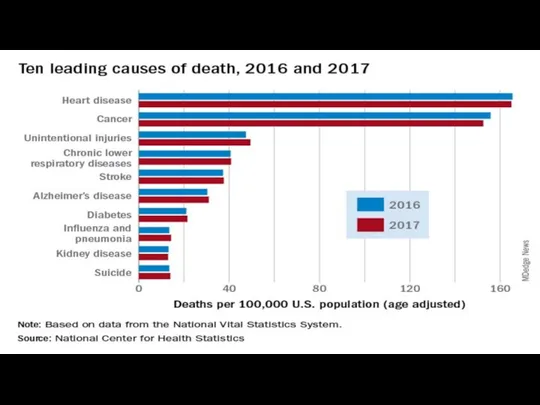
- 7. Medical Errors… A recent John Hopkins study claims more than 250,000 people in the U.S. die
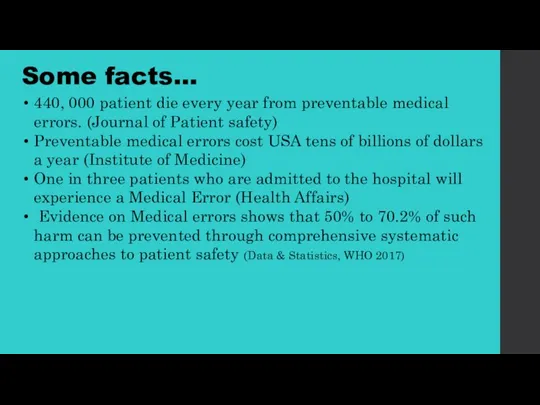
- 9. Some facts… 440, 000 patient die every year from preventable medical errors. (Journal of Patient safety)
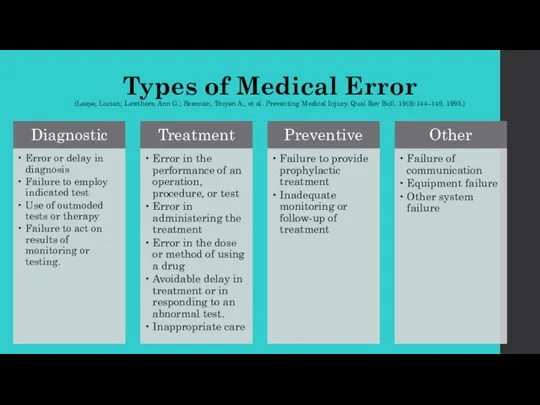
- 10. Types of Medical Error (Leape, Lucian; Lawthers, Ann G.; Brennan, Troyen A., et al. Preventing Medical
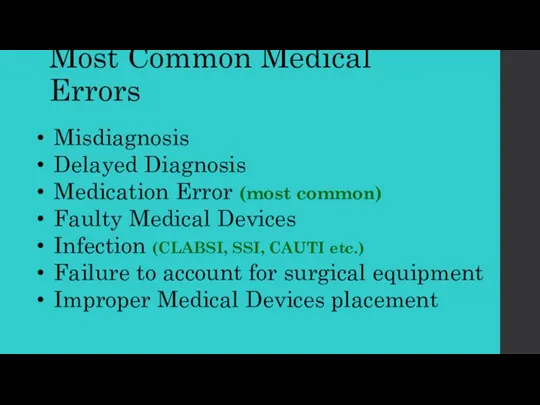
- 11. Most Common Medical Errors Misdiagnosis Delayed Diagnosis Medication Error (most common) Faulty Medical Devices Infection (CLABSI,
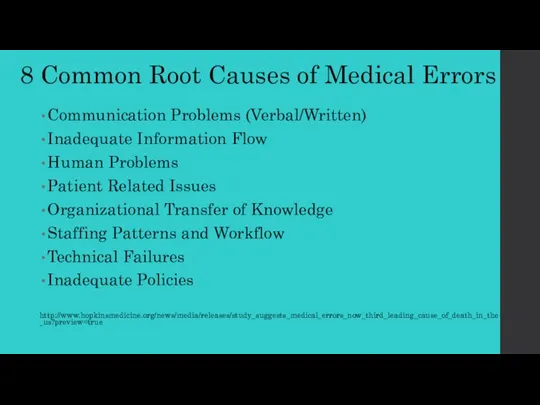
- 13. 8 Common Root Causes of Medical Errors Communication Problems (Verbal/Written) Inadequate Information Flow Human Problems Patient
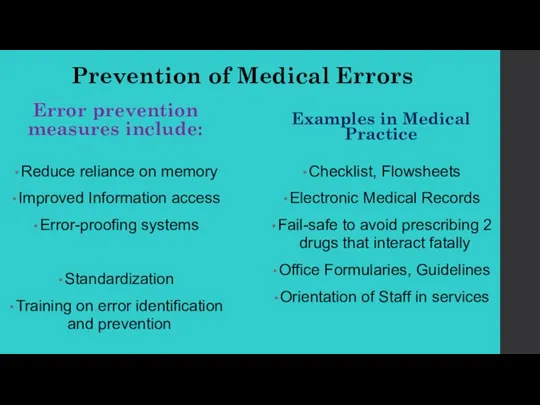
- 14. Prevention of Medical Errors Error prevention measures include: Reduce reliance on memory Improved Information access Error-proofing
- 15. MEDICAL ERROR REPORTING
- 16. All providers (nurses, pharmacists, and physicians) must accept the inherent issues in their roles as healthcare
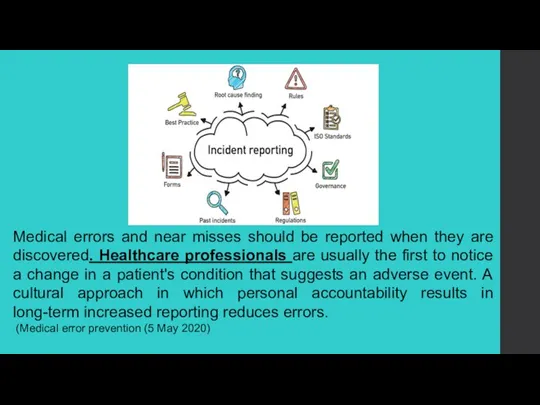
- 17. Medical errors and near misses should be reported when they are discovered. Healthcare professionals are usually
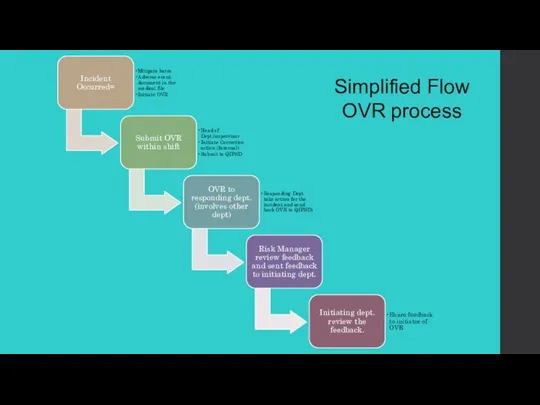
- 18. Simplified Flow OVR process
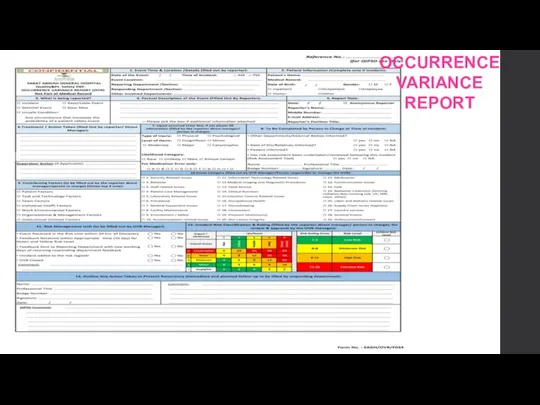
- 19. OCCURRENCE VARIANCE REPORT
- 20. We learn most from our painful mistakes. Mistakes can injure patients and land physicians in legal
- 21. In 1976, Dr. Jim Styner, an orthopedic surgeon, crashed his small plane into a cornfield in
- 22. Judy was 39 years old when she went to the hospital for a hysterectomy. After she
- 23. Sally and Ed looked forward to the birth of their first child. Sally's labor was long,
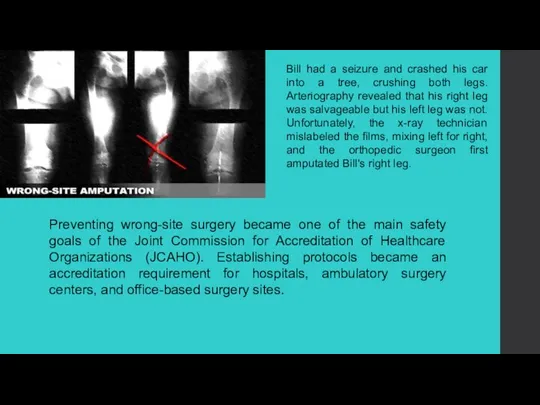
- 24. Preventing wrong-site surgery became one of the main safety goals of the Joint Commission for Accreditation
- 25. Tom was 12 years old when his appendix burst and he was taken to the local
- 26. As a young child, Betty had been given penicillin, turned blue, and was rushed to the
- 27. Linda wasn't doing well in her first trimester. The nausea and vomiting left her severely dehydrated
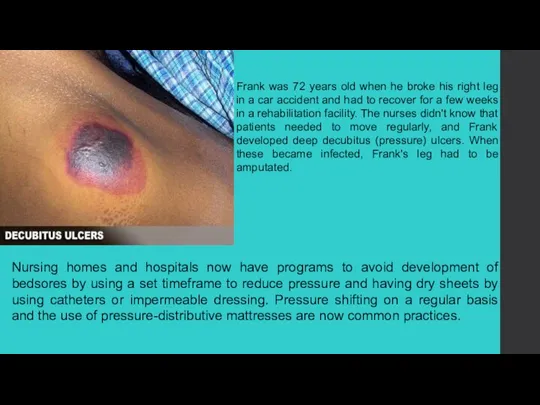
- 28. Frank was 72 years old when he broke his right leg in a car accident and
- 29. Lillian was 68 years old and weighed 250 lb when she underwent surgery to remove her
- 30. When Christy was 42 years old, her doctor discovered a large lump in her left breast.
- 32. Скачать презентацию
 Оценка функционального состояния сердечно-сосудистой системы
Оценка функционального состояния сердечно-сосудистой системы Лекция №11. Весы и взвешивание
Лекция №11. Весы и взвешивание Семейство Bacillaceae
Семейство Bacillaceae Галактоземия
Галактоземия Вторичный и третичный периоды сифилиса. 4 часть. Лекция 7
Вторичный и третичный периоды сифилиса. 4 часть. Лекция 7 Астма
Астма Covid-19 что после …
Covid-19 что после … Обработка протеза
Обработка протеза Хорея Гентингтона (“пляска святого Витта”)
Хорея Гентингтона (“пляска святого Витта”) Первичная обработка проникающей раны грудной стенки
Первичная обработка проникающей раны грудной стенки Страшная плата за страшный миг радости
Страшная плата за страшный миг радости Профессиональная надежность работников и влияние здоровья на успешность работы
Профессиональная надежность работников и влияние здоровья на успешность работы Анестезиологический и операционный риск
Анестезиологический и операционный риск Терапия сахарного диабета 1 и 2 типа
Терапия сахарного диабета 1 и 2 типа Грипп. Признаки и лечение
Грипп. Признаки и лечение Внезапная смерть
Внезапная смерть Неотложные состояния в пульмонологии
Неотложные состояния в пульмонологии Морфофункциональная характеристика аппарата движения. Остеология. Скелет черепа
Морфофункциональная характеристика аппарата движения. Остеология. Скелет черепа День борьбы со СПИДом
День борьбы со СПИДом Сестринский уход при бронхиальной астме и её осложнениях
Сестринский уход при бронхиальной астме и её осложнениях Профилактика эпилепсии
Профилактика эпилепсии Mагний Хелат (Magnesium Complex)
Mагний Хелат (Magnesium Complex) Организация_офтальмологической_помощи
Организация_офтальмологической_помощи Пиометра. Диагностика
Пиометра. Диагностика Антибиотиктер микробтар мен
Антибиотиктер микробтар мен Психоаналептики. Антидепрессанты. Психостимуляторы. Ноотропы
Психоаналептики. Антидепрессанты. Психостимуляторы. Ноотропы Прием пациента в стационар. Лекция №1
Прием пациента в стационар. Лекция №1