Содержание
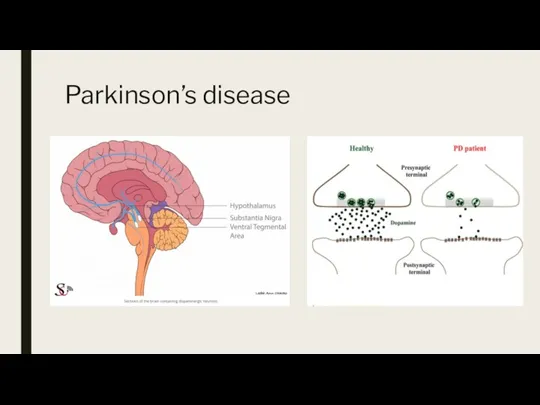
- 2. Parkinson’s disease
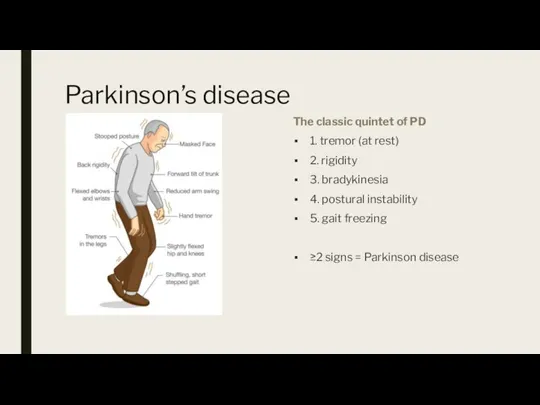
- 3. Parkinson’s disease The classic quintet of PD 1. tremor (at rest) 2. rigidity 3. bradykinesia 4.
- 4. Parkinson’s disease Pill-rolling Tremor of fingers and hand Cogwheel rigidity Moving arms passively toward body
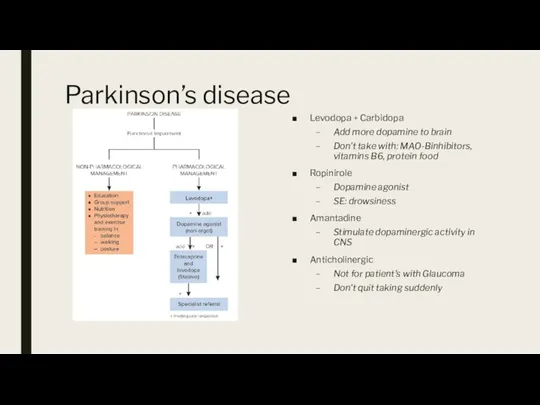
- 5. Parkinson’s disease Levodopa + Carbidopa Add more dopamine to brain Don’t take with: MAO-Binhibitors, vitamins B6,
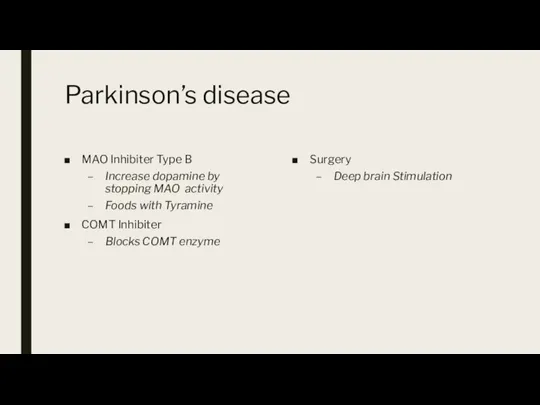
- 6. Parkinson’s disease MAO Inhibiter Type B Increase dopamine by stopping MAO activity Foods with Tyramine COMT
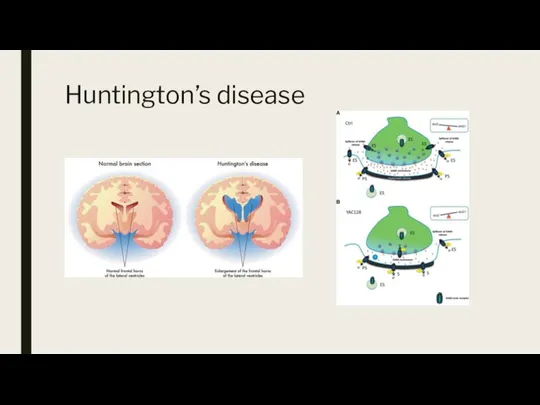
- 7. Huntington’s disease
- 8. Huntington’s disease Insidious onset and progression of chorea Onset most often between 35 and 55 years
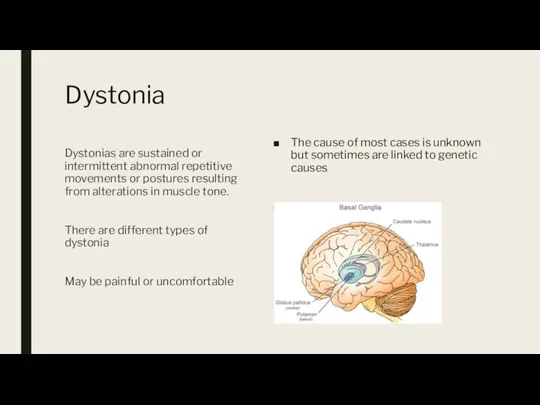
- 9. Dystonia The cause of most cases is unknown but sometimes are linked to genetic causes Disorder
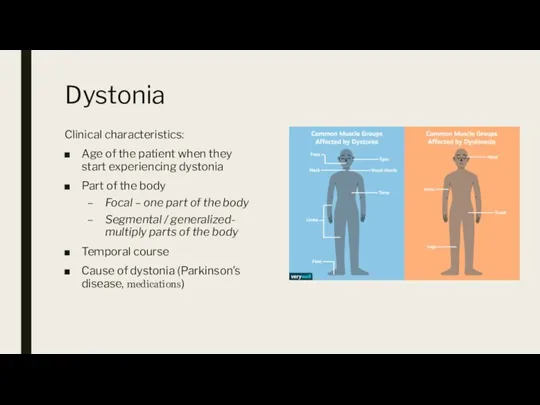
- 10. Dystonia Clinical characteristics: Age of the patient when they start experiencing dystonia Part of the body
- 11. Dystonia Management Medication Dopamine agents: levodopa Anticholinergics: trihexyphenidyl Benzodiazepines: clonazepam Muscle relaxants: baclofen Injectable biologics Botulinum
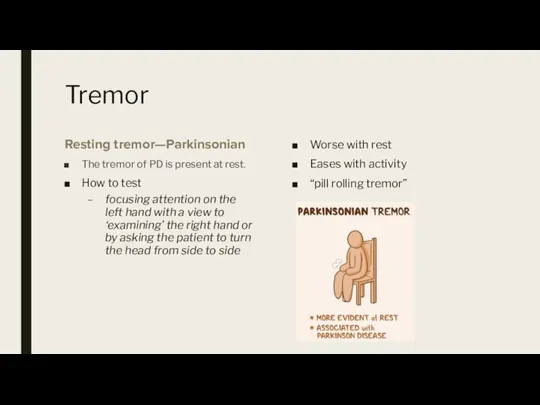
- 12. Tremor Resting tremor—Parkinsonian The tremor of PD is present at rest. How to test focusing attention
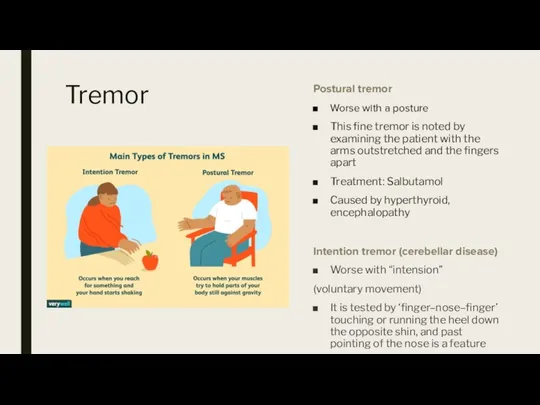
- 13. Tremor Postural tremor Worse with a posture This fine tremor is noted by examining the patient
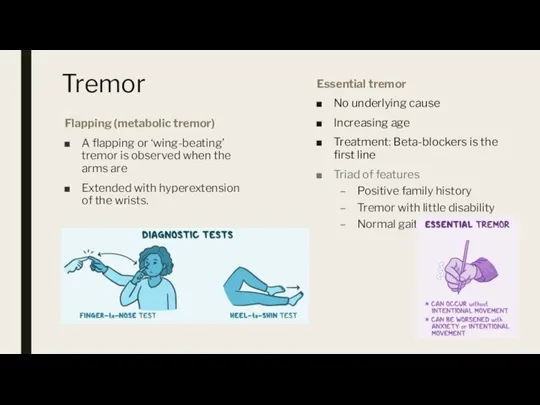
- 14. Tremor Flapping (metabolic tremor) A flapping or ‘wing-beating’ tremor is observed when the arms are Extended
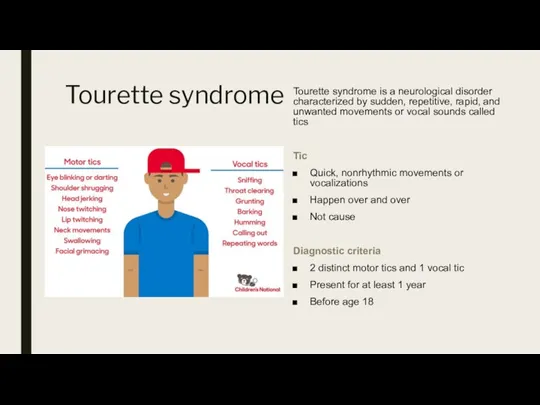
- 15. Tourette syndrome Tourette syndrome is a neurological disorder characterized by sudden, repetitive, rapid, and unwanted movements
- 16. Tourette syndrome Most severe Before puberty (10-12) During periods of anxiety, excitement, or exhaustion Management Therapy
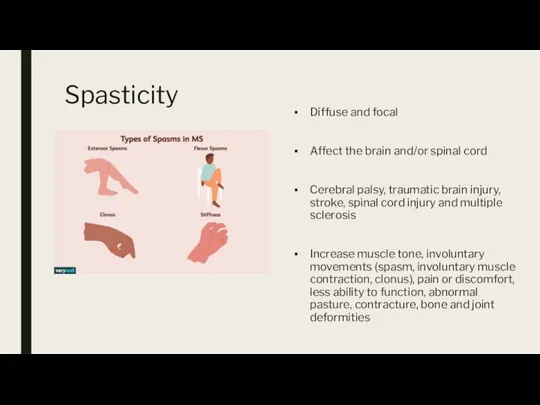
- 17. Spasticity Diffuse and focal Affect the brain and/or spinal cord Cerebral palsy, traumatic brain injury, stroke,
- 18. Spasticity Diagnosis: history, clinical, MRI Treatment Not require To stretch daily Centrally Acting Drugs Baclofen Alpha-2
- 19. Cerebellar syndrome Incoordination Walking Limb Speech Eves
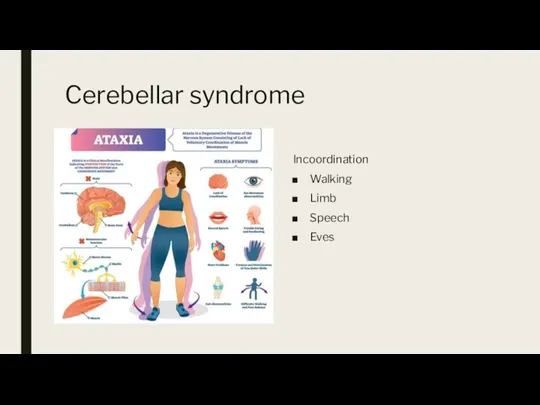
- 20. Wernickle encephalopathy and Korsacoff syndrome Is a brain disorder due to thiamine deficiency (vitamin B1) including
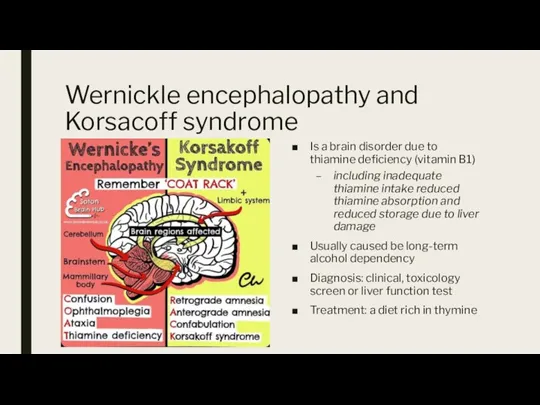
- 21. Spino-cerebellar ataxia Progressive neurodegenerative diseases of genetic origin Present of any age Progressive loss of coordination
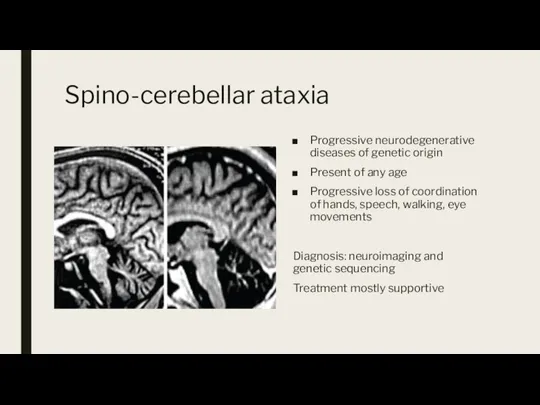
- 23. Скачать презентацию


 Клинико-эпидемиологическая характеристика дебюта рассеянного склероза в Рязанской области
Клинико-эпидемиологическая характеристика дебюта рассеянного склероза в Рязанской области Преемственность и комплексный подход в оказании психиатрической помощи. IV Муратовские научные чтения
Преемственность и комплексный подход в оказании психиатрической помощи. IV Муратовские научные чтения Переломы. Классификация травматизма
Переломы. Классификация травматизма Клиническая денситометрия
Клиническая денситометрия Электромагнитные поля в биомедицинской диагностике
Электромагнитные поля в биомедицинской диагностике Гемодинамика
Гемодинамика Концепция поддержки Herbalife Nutrition
Концепция поддержки Herbalife Nutrition Электрорентгенография, основы метода, области применения
Электрорентгенография, основы метода, области применения Утилизация медицинских отходов
Утилизация медицинских отходов Лучевая терапия история, современное состояние, физические основы
Лучевая терапия история, современное состояние, физические основы Гемокультивирование. Правила забора крови
Гемокультивирование. Правила забора крови 6
6 Жағдайлық есеп. Қызылша
Жағдайлық есеп. Қызылша Методики пункции суставов
Методики пункции суставов Работая с пациентами пожилого и старческого возраста
Работая с пациентами пожилого и старческого возраста ВПС, протекающие с обогащением малого круга кровообращения. Лекция №3
ВПС, протекающие с обогащением малого круга кровообращения. Лекция №3 Мобильный ФАП. Мобильная дистанционная диагностика
Мобильный ФАП. Мобильная дистанционная диагностика Алыптасу кезеңіндегі (бозбалалық, бойжеткендік) негізгі проблемалар және оның шешу жолдары
Алыптасу кезеңіндегі (бозбалалық, бойжеткендік) негізгі проблемалар және оның шешу жолдары Особенности восприятия окружающего мира слабослышащими
Особенности восприятия окружающего мира слабослышащими Системные васкулиты
Системные васкулиты ВИЧ - инфекция
ВИЧ - инфекция Фармацевтикалық өндіріс орындарындағы еңбек қорғау ережелері мен негізгі қойылатын талаптар
Фармацевтикалық өндіріс орындарындағы еңбек қорғау ережелері мен негізгі қойылатын талаптар Массаж в стиле ДЗЕН
Массаж в стиле ДЗЕН Профзаболевания работников атомных электростанций
Профзаболевания работников атомных электростанций История педиатрии
История педиатрии Небезпечне меню
Небезпечне меню Современные способы лечения. Профилактика осложнений атеросклера нижних конечностей
Современные способы лечения. Профилактика осложнений атеросклера нижних конечностей Нарушение обмена витаминов
Нарушение обмена витаминов