Слайд 2Introduction
What is bronchial asthma?
Asthma is a long-term inflammatory disease of the airways of the lungs.[3] It is characterized by
variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms
Слайд 3Causes:
Asthma is caused by a combination of complex and incompletely understood environmental
and genetic interactions.
Environmental : allergens, pollens , air pollution & other chemicals.
Smoking
Chemical exposure(formaldehyde, pesticides)
Use of antibiotics in early life
Genetic
Слайд 4Signs and symptoms
Wheezing, shortness of breathing
Chest tightness
Cough
Sputum may produce
by lungs but its often hard to bring up.
Associate condition (GERD,Rhino sinusitis)
Слайд 5Pathophysiology
Asthma is the result of chronic inflammation of the conducting zone of the airways (most especially
the bronchi and bronchioles), which subsequently results in increased contractability of the surrounding smooth muscles.
This among other factors leads to bouts of narrowing of the airway and the classic symptoms of wheezing.
Typical changes in the airways include an increase in eosinophils and thickening of the lamina reticularis.
Слайд 6airways' smooth muscle may increase in size along with an increase in
the numbers of mucous glands.
cell types involved include: T lymphocytes, macrophages, and neutrophils.
may also be involvement of other components of the immune system including: cytokines, chemokines, histamine, and leukotrienesamong others.
Слайд 7Diagnosis
Spirometry
Asthma exacerbatio
-Near-fatal high PaCO2, or requiring mechanical ventilation, or both
-Life-threatening:Oxygen saturation < 92%
-Acute severe:Peak flow 33–50%, Respiratory rate ≥ 25 breaths per minute, Heart rate ≥ 110 beats per minute & Unable to complete sentences in one breath
Слайд 8Moderate :worsening symptomsPeak flow 50–80% best or predictedNo features of acute severe
asthma.
And also many induce asthma
-exercise induced
-occupational
-aspirin induced asthma
-alcohol induced asthma
-Non atopic asthma
Слайд 9Prevention
Stop tobacco smoking
Decrease air pollution
Chemical irritants- perfume should be
stop using.
Identify and avoid asthma triggers.
Get vaccinated for influenza and pneumonia.
Слайд 10Management
Prevention of antigen-antibody reaction:Antigen avoidance, hyposensitization
Neutralization of IgE (reaginic antibody):Omalizumab
Prevention of
the release of mediators: Mast cell stabilizers
Suppression of inflammation and bronchial hyper-reactivity: Corticosteroids
Antagonism of released mediators: Leukotriene antagonist, Antihistamines
Blockade of constrictor neurotransmitter:Anticholinergics
Слайд 11Directly acting bronchodilators: Methylxanthines
Bronchodilators:
1. β2-sympathomimetics (Salbutamol, Terbutaline etc)
2. Methylxanthines
(Theophylline, Aminophylline, )
3.Anticholinergics Tiotropium bromide)
Corticosteroids:
1. Systemic Corticosteroids (Hydrocortisone, Prednisolone)
2. Inhalational Corticosteroids (Beclomethasone, Budesonide, Fluticasone propionate, Flunisolide, Ciclesonide)
 Детские голоса
Детские голоса Гипотермия. Способы потери тепла
Гипотермия. Способы потери тепла Медицинская реабилитация при гипотонической болезни
Медицинская реабилитация при гипотонической болезни Основные клинические синдромы при заболеваниях мочевыделительной системы
Основные клинические синдромы при заболеваниях мочевыделительной системы Виды вирусов. Антивирусники
Виды вирусов. Антивирусники Мероприятия по предупреждению вредного воздействия профессиональных факторов на медицинский персонал
Мероприятия по предупреждению вредного воздействия профессиональных факторов на медицинский персонал Стенокардия Принцметала
Стенокардия Принцметала Неспецефический язвенный колит
Неспецефический язвенный колит Применение макромицетов в медицине
Применение макромицетов в медицине Ultrasound in medicine and biology
Ultrasound in medicine and biology Уход за больными с опухолями кожи, мягких тканей. Классификация рака кожи
Уход за больными с опухолями кожи, мягких тканей. Классификация рака кожи Хронической лимфоцитарный лейкоз
Хронической лимфоцитарный лейкоз Эпидемиологиялық ощақты зерттеу
Эпидемиологиялық ощақты зерттеу ВИЧ-инфекция
ВИЧ-инфекция Органосохраняющие операции при раке шейки матки и яичников. Показания и противопоказания. Технические особенности
Органосохраняющие операции при раке шейки матки и яичников. Показания и противопоказания. Технические особенности Вакцинация детей и взрослых против гриппа
Вакцинация детей и взрослых против гриппа Фотодело. Профилактика
Фотодело. Профилактика Физиологические роды
Физиологические роды Правила сбора мочи
Правила сбора мочи Ренгенологічна діагностика сечової системи
Ренгенологічна діагностика сечової системи Пульпит
Пульпит Нормативная, правовая база профилактической помощи (1) (1)
Нормативная, правовая база профилактической помощи (1) (1) Емізіктің жарақаттануы және лактостаз
Емізіктің жарақаттануы және лактостаз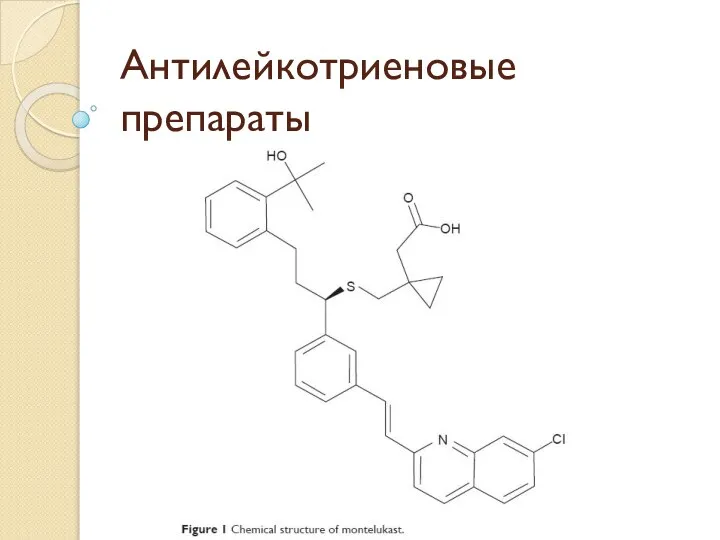 Антилейкотриеновые препараты
Антилейкотриеновые препараты Методы изучения и гигиеническая оценка комплексного действия метеофакоторов на организм
Методы изучения и гигиеническая оценка комплексного действия метеофакоторов на организм Как продлить жизнь человека
Как продлить жизнь человека Противовирусные средства
Противовирусные средства Методы исследования дисфункции желчевыводящих путей у детей
Методы исследования дисфункции желчевыводящих путей у детей