Содержание
- 2. Objectives Describe PCOS and associated pathophysiology Identify risk factors of and conditions related to PCOS Diagnose
- 3. Polycystic Ovary SYNDROME 1800s: polycystic ovaries “cystic oophoritis”; “sclerocystic” Stein & Leventhal (1953) Enlarged ovaries, hirsutism,
- 4. PCOS PCOS Collection of signs and symptoms May be difficult to diagnose Heterogeneous presentation Features change
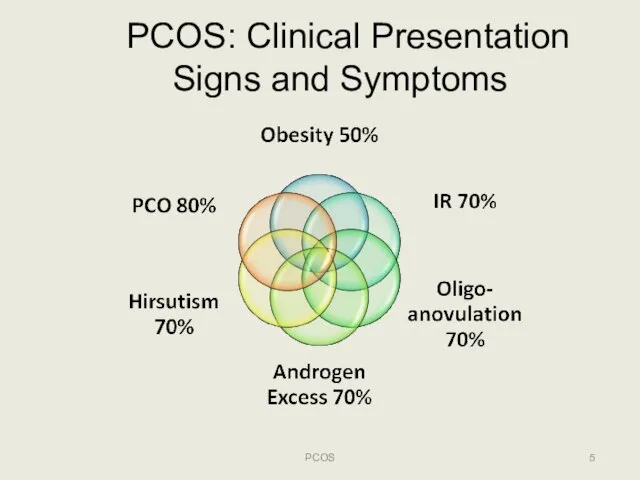
- 5. PCOS: Clinical Presentation Signs and Symptoms PCOS
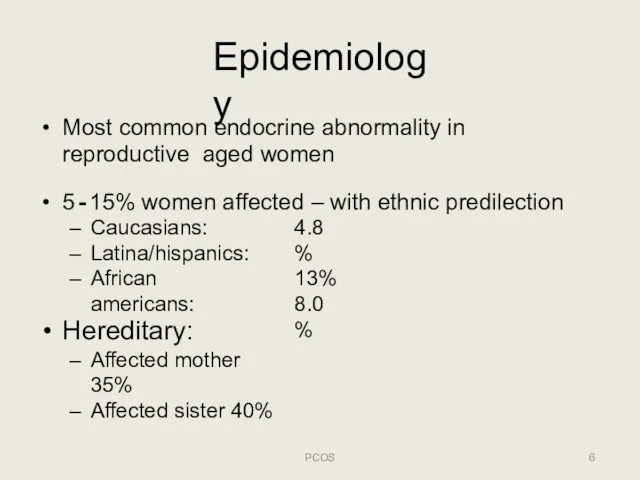
- 6. Epidemiology PCOS Most common endocrine abnormality in reproductive aged women 5‐15% women affected – with ethnic
- 7. Polycystic Ovary Syndrome (PCOS) ETIOLOGY & PATHOPHYSIOLOGY PCOS
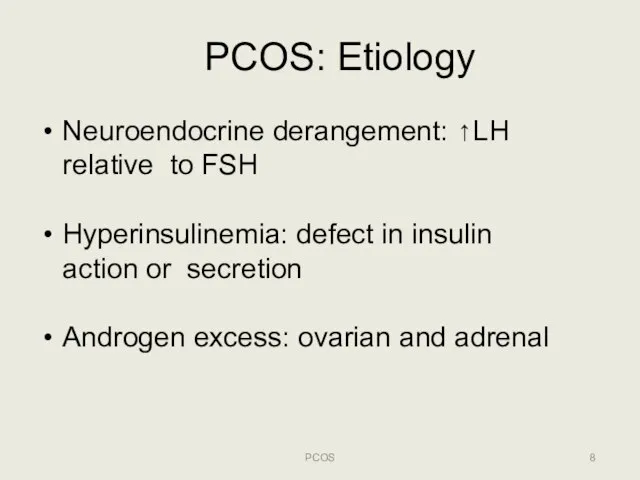
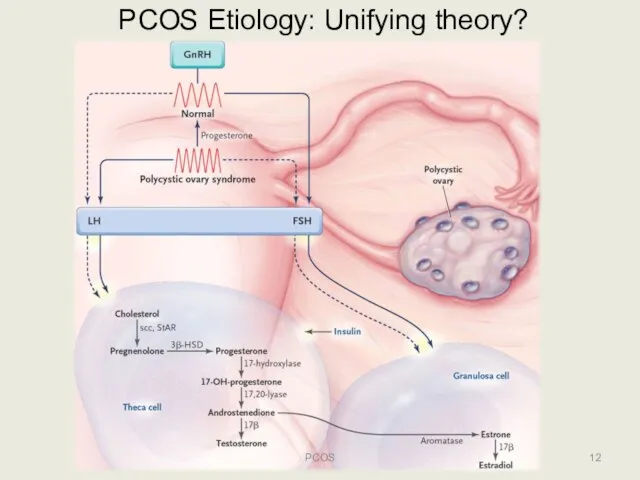
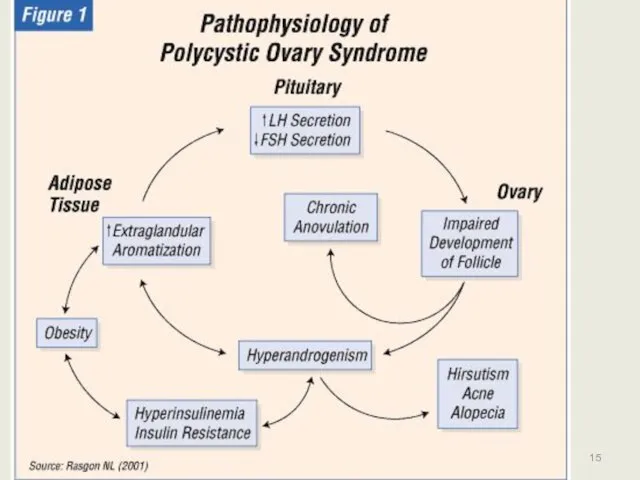
- 8. PCOS: Etiology PCOS Neuroendocrine derangement: ↑LH relative to FSH Hyperinsulinemia: defect in insulin action or secretion
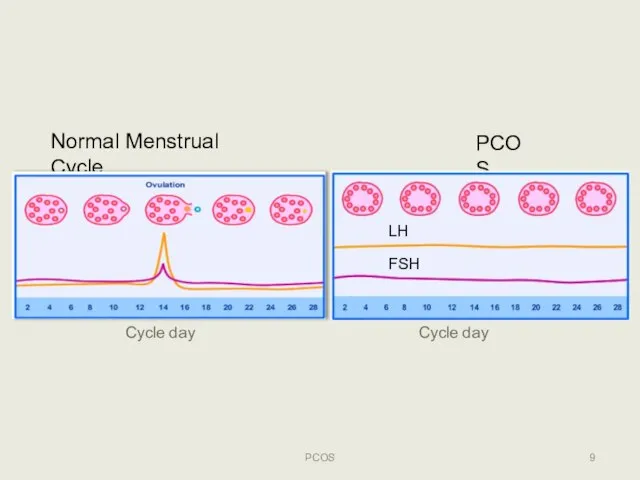
- 9. Normal Menstrual Cycle PCOS LH FSH PCOS Cycle day Cycle day
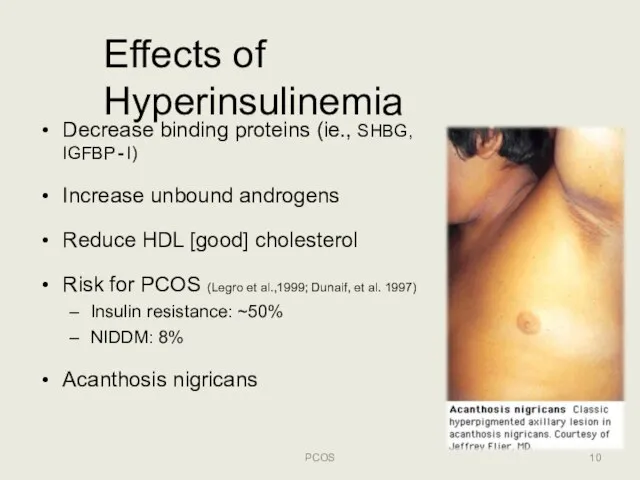
- 10. Effects of Hyperinsulinemia Decrease binding proteins (ie., SHBG, IGFBP‐I) Increase unbound androgens Reduce HDL [good] cholesterol
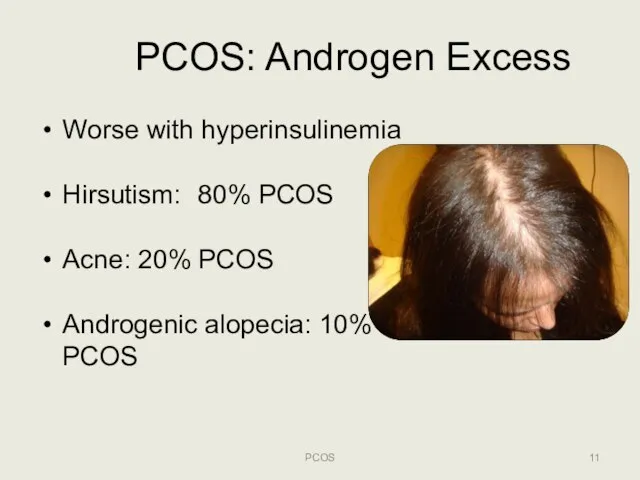
- 11. PCOS: Androgen Excess Worse with hyperinsulinemia Hirsutism: 80% PCOS Acne: 20% PCOS Androgenic alopecia: 10% PCOS
- 12. PCOS Etiology: Unifying theory? PCOS
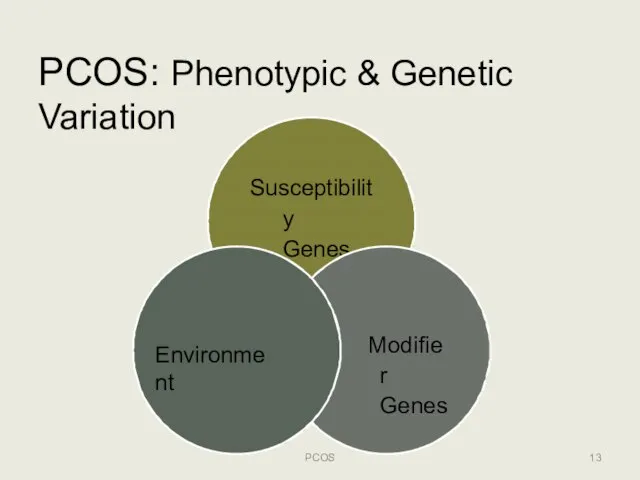
- 13. PCOS: Phenotypic & Genetic Variation Susceptibility Genes Modifier Genes Environment PCOS
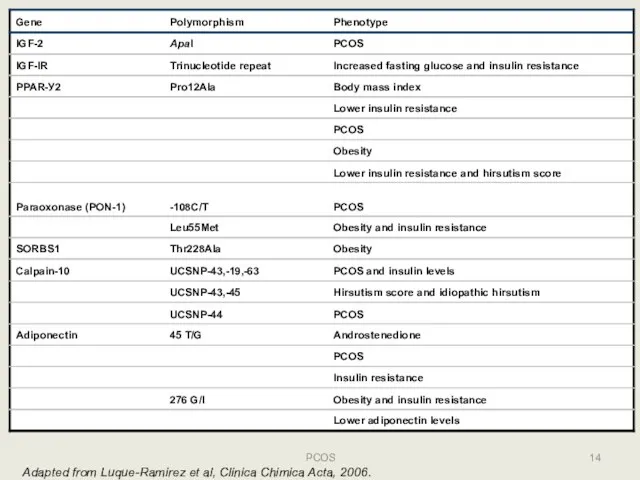
- 14. 14 PCOS Adapted from Luque-Ramirez et al, Clinica Chimica Acta, 2006.
- 15. PCOS 15
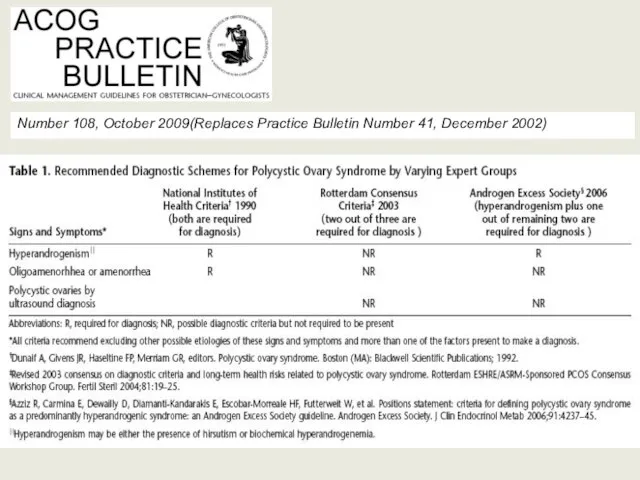
- 16. PCOS: Diagnostic Criteria PCOS NIH/NICHD: USA, 1990 ESHRE/ASRM: Rotterdam, 2004 Androgen Excess‐PCOS Intl Society: 2006
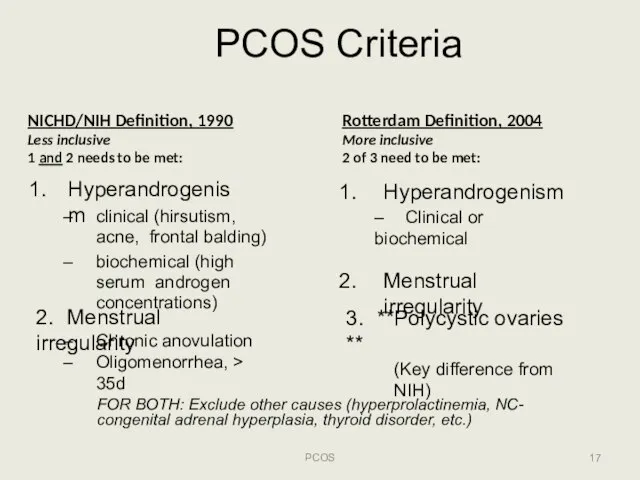
- 17. PCOS Criteria PCOS NICHD/NIH Definition, 1990 Less inclusive 1 and 2 needs to be met: Hyperandrogenism
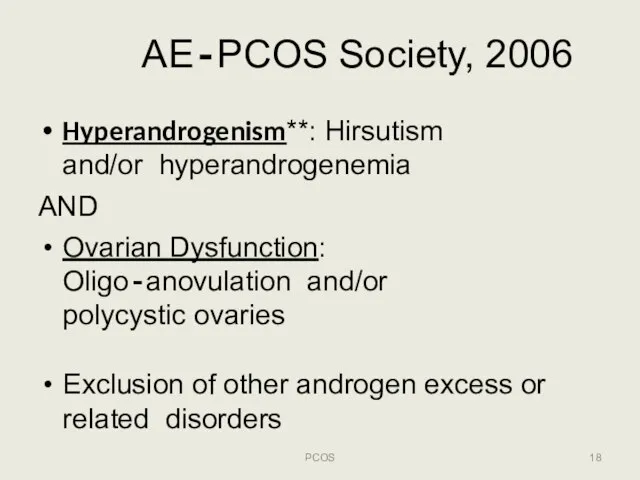
- 18. AE‐PCOS Society, 2006 PCOS Hyperandrogenism**: Hirsutism and/or hyperandrogenemia AND Ovarian Dysfunction: Oligo‐anovulation and/or polycystic ovaries Exclusion
- 19. Number 108, October 2009(Replaces Practice Bulletin Number 41, December 2002)
- 20. Polycystic Ovary Syndrome (PCOS) EVALUATION PCOS
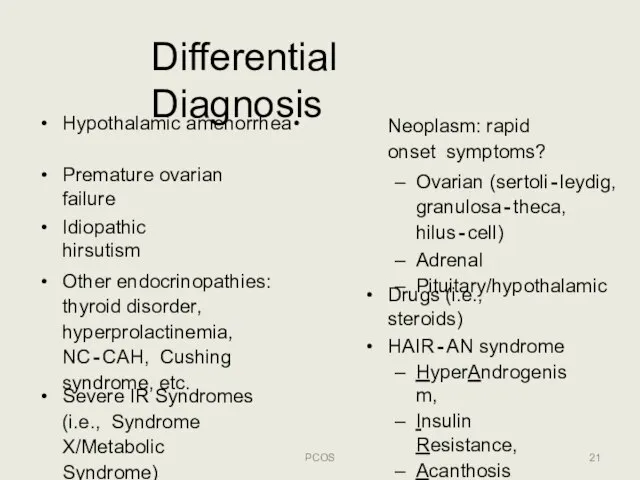
- 21. Differential Diagnosis PCOS Premature ovarian failure Idiopathic hirsutism Other endocrinopathies: thyroid disorder, hyperprolactinemia, NC‐CAH, Cushing syndrome,
- 22. PCOS: Menstrual Dysfunction PCOS 25‐30% of women with oligo‐anovulation have PCOS ≥35 day intervals or 2/3
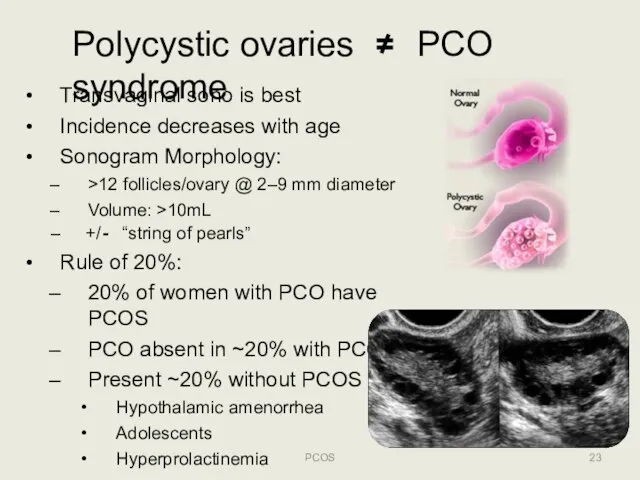
- 23. Polycystic ovaries ≠ PCO syndrome Transvaginal sono is best Incidence decreases with age Sonogram Morphology: >12
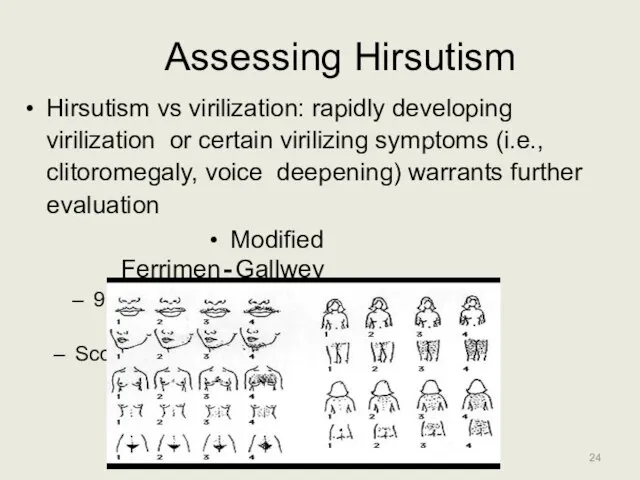
- 24. Assessing Hirsutism Hirsutism vs virilization: rapidly developing virilization or certain virilizing symptoms (i.e., clitoromegaly, voice deepening)
- 25. PCOS: Physical Exam PCOS Blood pressure Body mass index (kg/m2) >25 overweight >30 obese Waist circumference
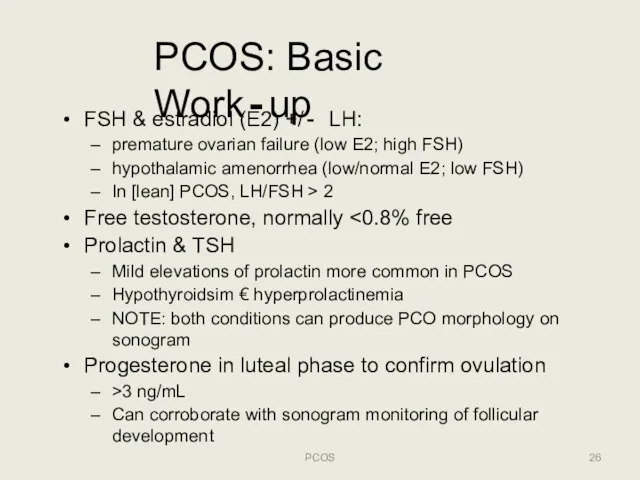
- 26. PCOS: Basic Work‐up PCOS FSH & estradiol (E2) +/‐ LH: premature ovarian failure (low E2; high
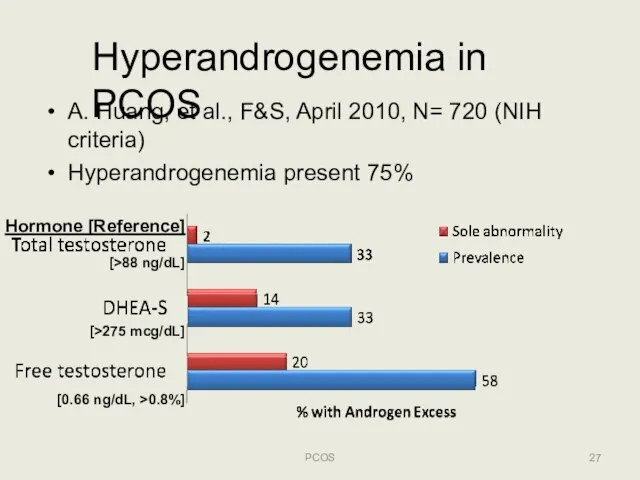
- 27. Hyperandrogenemia in PCOS A. Huang, et al., F&S, April 2010, N= 720 (NIH criteria) Hyperandrogenemia present
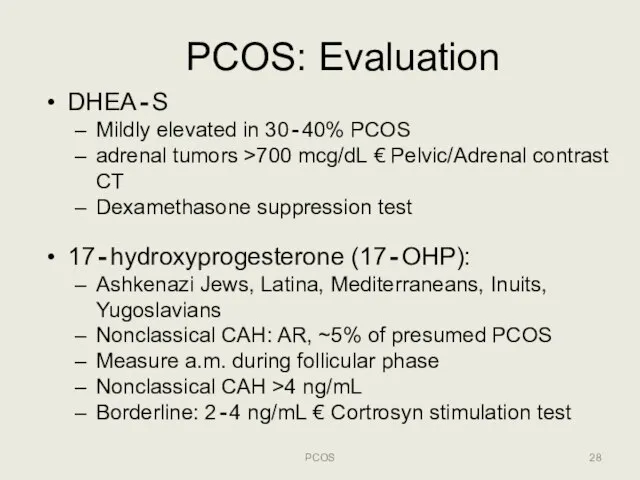
- 28. PCOS: Evaluation PCOS DHEA‐S Mildly elevated in 30‐40% PCOS adrenal tumors >700 mcg/dL € Pelvic/Adrenal contrast
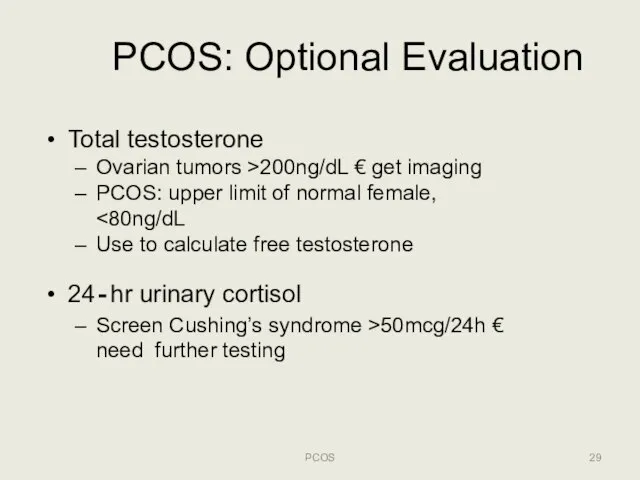
- 29. PCOS: Optional Evaluation PCOS Total testosterone Ovarian tumors >200ng/dL € get imaging PCOS: upper limit of
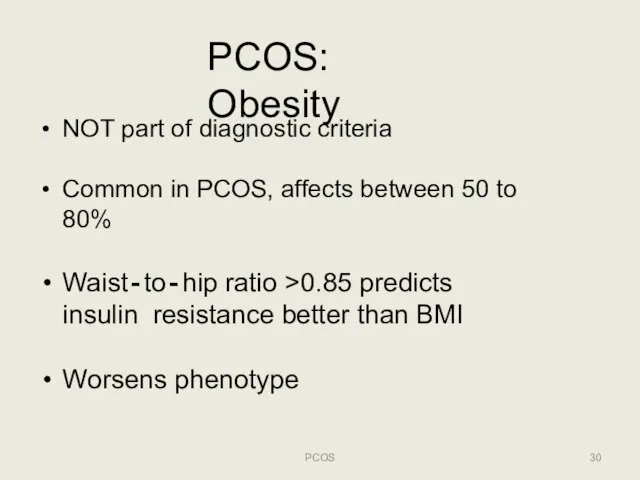
- 30. PCOS: Obesity PCOS NOT part of diagnostic criteria Common in PCOS, affects between 50 to 80%
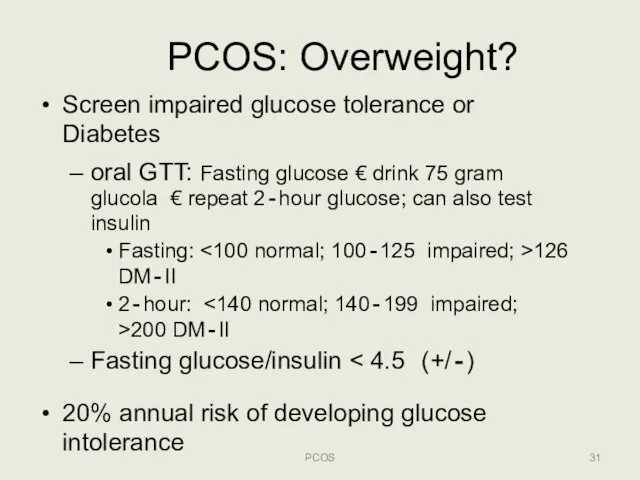
- 31. PCOS: Overweight? PCOS Screen impaired glucose tolerance or Diabetes oral GTT: Fasting glucose € drink 75
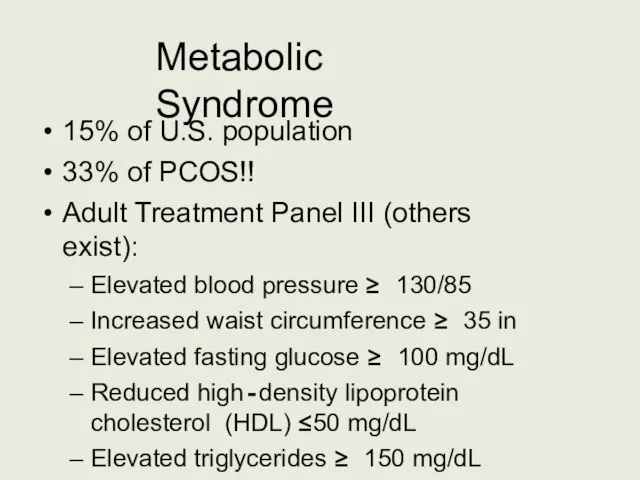
- 32. Metabolic Syndrome 15% of U.S. population 33% of PCOS!! Adult Treatment Panel III (others exist): Elevated
- 33. Polycystic Ovary Syndrome (PCOS) TREATMENT: GOAL SPECIFIC PCOS
- 34. PCOS: Goal Specific Therapy PCOS Screen and manage comorbidities Hirsutism/acne/hair loss Protect/monitor endometrium Ultrasound +/‐ endometrial
- 35. PCOS: Co‐morbidities! PCOS Insulin resistance, ~30% Type‐II DM, ~10% (3‐5x) Gestational diabetes (2.5x) Endometrial hyperplasia/ atypia/cancer
- 36. PCOS: Probable Links PCOS Coronary artery disease Dyslipidemia Hypertension Ovarian cancer (?) Miscarriage (?) Pregnancy induced
- 37. Prevention of CVD and DM PCOS Lifestyle: weightloss and exercise!! Metformin 1500‐2000 mg daily if documented
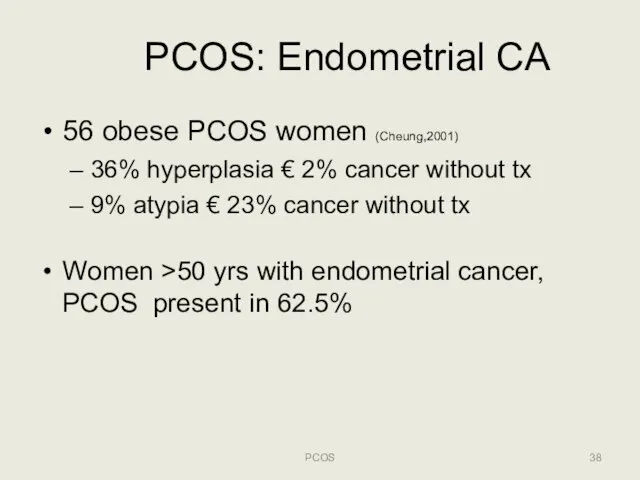
- 38. PCOS: Endometrial CA PCOS 56 obese PCOS women (Cheung,2001) 36% hyperplasia € 2% cancer without tx
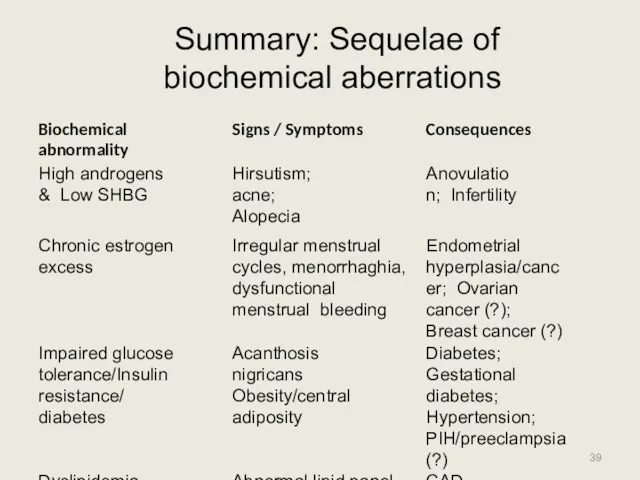
- 39. Summary: Sequelae of biochemical aberrations PCOS
- 40. Treatment of Hirsutism PCOS Multi‐step approach is most‐effective: Hair removal: wax, laser, eflornithine, etc. OCPs for
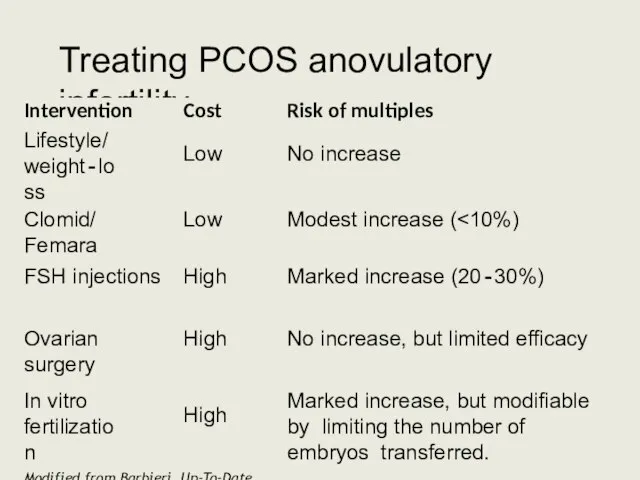
- 41. Treating PCOS anovulatory infertility PCOS
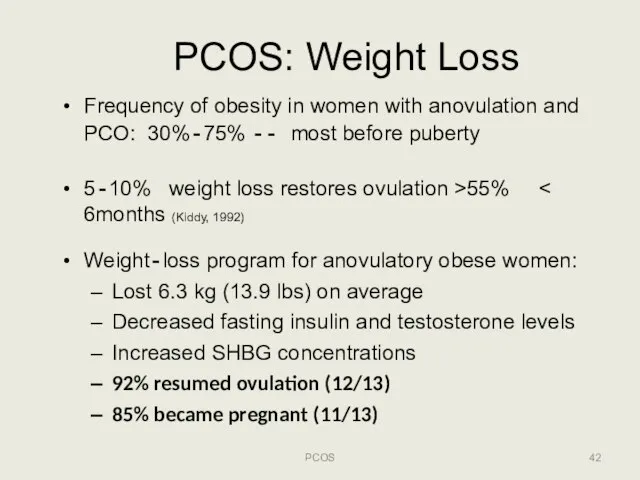
- 42. PCOS: Weight Loss PCOS Frequency of obesity in women with anovulation and PCO: 30%‐75% ‐‐ most
- 43. PCOS and Infertility: Metformin? PCOS Metformin (biguanide ): improves insulin resistance reduce hepatic glucose production &
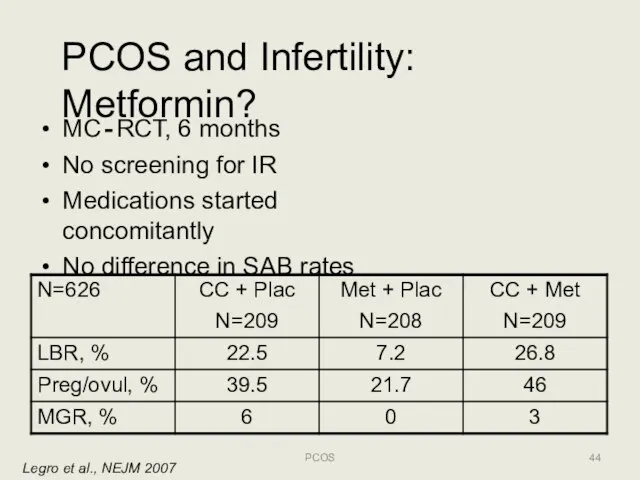
- 44. PCOS and Infertility: Metformin? Legro et al., NEJM 2007 MC‐RCT, 6 months No screening for IR
- 45. PCOS Fertility Options: Ovulation Induction (OI)/Superovulation (SO) Clomiphene Citrate: non‐steroidal weak estrogen related to diethystilbestrol, SERM
- 46. PCOS Fertility Options: OI/SO (2) Gonadotropins: HMG, FSH 60% live‐birth 12‐18 mo Need careful monitoring (follicle
- 47. PCOS Fertility Options: ART PCOS Assisted Reproductive Technologies (ie, IVF/ICSI) PROS Highly successful in PCOS: >60%
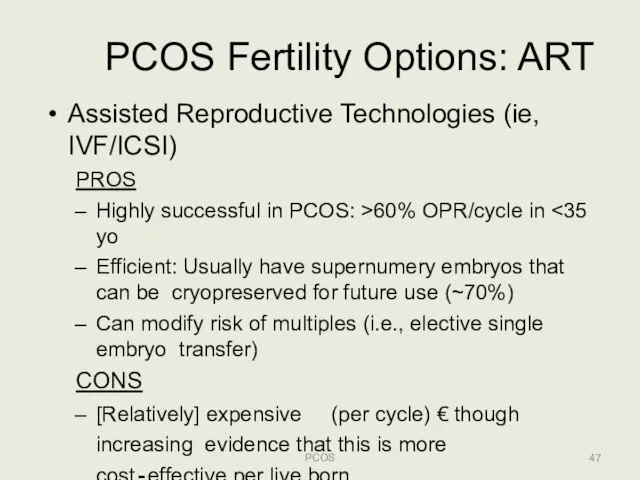
- 48. PCOS Fertility Options: Surgery PCOS Laparoscopic wedge resection or ovarian drilling PROS May avoid fertility treatment
- 49. PCOS: Pharmacotherapy summary PCOS
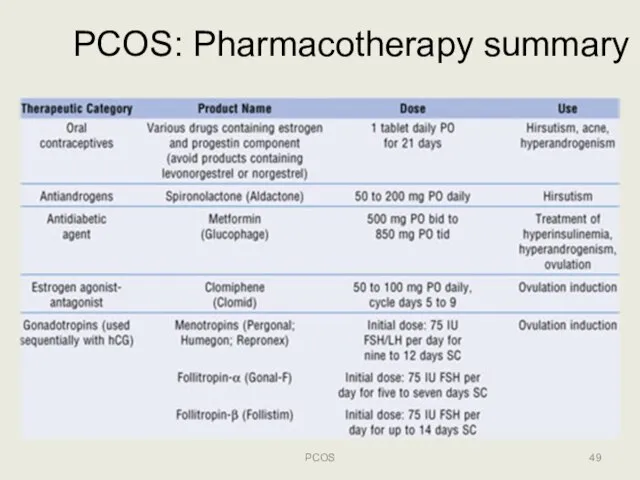
- 50. PCOS: Conclusions (1) PCOS Multifaceted condition with varying presentation No clearly accepted basis for diagnosis Significantly
- 52. Скачать презентацию

 Тракционная терапия
Тракционная терапия Пункция заднего свода влагалища (кульдоцентез)
Пункция заднего свода влагалища (кульдоцентез) Трансторакальная эхокардиография
Трансторакальная эхокардиография Стрептококки
Стрептококки Сестринский процесс при пневмонии
Сестринский процесс при пневмонии Научно-практический календарь травматологии и ортопедии
Научно-практический календарь травматологии и ортопедии 10 факторов развития плоскостопия и нарушения осанки
10 факторов развития плоскостопия и нарушения осанки Приверженность АРВТ
Приверженность АРВТ Репродуктивное здоровье человека
Репродуктивное здоровье человека Анафилактический шок
Анафилактический шок Аллергия. Аллергические реакции
Аллергия. Аллергические реакции Сестринская деятельность при остром бронхите у детей
Сестринская деятельность при остром бронхите у детей Строение коркового и мозгового вещества почки
Строение коркового и мозгового вещества почки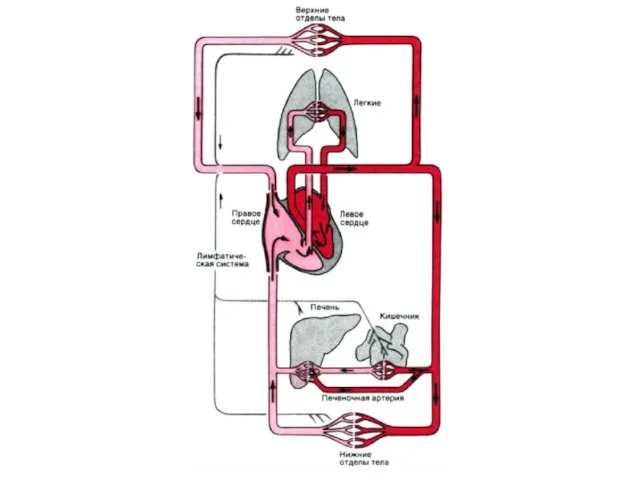 Кровообращение
Кровообращение Повреждения от острых предметов
Повреждения от острых предметов 15 хвилин про цукор
15 хвилин про цукор Осторожно, клещи!
Осторожно, клещи! Важнейшие открытия в медицине нового времени
Важнейшие открытия в медицине нового времени Сахарный диабет у детей
Сахарный диабет у детей Сестринский процесс при раке желудка
Сестринский процесс при раке желудка Состояние адаптационного резерва сердечно-сосудистой системы у детей, проживающих на экологически неблагополучных территориях
Состояние адаптационного резерва сердечно-сосудистой системы у детей, проживающих на экологически неблагополучных территориях Кровотечения
Кровотечения Влияние грудного вскармливания на развитие детей
Влияние грудного вскармливания на развитие детей Синдром Ламберта-Итона
Синдром Ламберта-Итона Қант диабеті(ҚД) ІІ типі қосарланған созылмалы жүрек жетіспеушілгі (СЖЖ) бар науқастарға стандартты емнің әсері
Қант диабеті(ҚД) ІІ типі қосарланған созылмалы жүрек жетіспеушілгі (СЖЖ) бар науқастарға стандартты емнің әсері Синхронизация колебаний в связанных осцилляторах ФитцХью-Нагумо в ходе эпилептического приступа
Синхронизация колебаний в связанных осцилляторах ФитцХью-Нагумо в ходе эпилептического приступа Medical concern of a shoulder pain
Medical concern of a shoulder pain Грипп и вакцинопрофилактика
Грипп и вакцинопрофилактика